Abstract
Objectives. To describe which industries have the highest burden of COVID-19 outbreaks in California.
Methods. We assigned US census industry codes to COVID-19 outbreaks reported to the California Department of Public Health (CDPH) from January 1, 2020, to August 31, 2021, and determined numbers of outbreaks, numbers of outbreak-associated cases, and outbreak incidence levels by industry. We determined characteristics of outbreak-associated cases using individual case data linked to COVID-19 outbreaks.
Results. Local health departments reported 19 893 COVID-19 outbreaks and 300 379 outbreak-associated cases to CDPH. The most outbreaks (47.8%) and outbreak-associated cases (54.8%) occurred in the health care and social assistance sector, where outbreak incidence levels were highest in skilled nursing facilities and residential care facilities (1306 and 544 outbreaks per 1000 establishments, respectively). High proportions of outbreaks also occurred in the retail trade (8.6%) and manufacturing (7.9%) sectors. Demographics of outbreak-associated cases varied across industries.
Conclusions. Certain California industries, particularly in the health care, manufacturing, and retail sectors, have experienced a high burden of COVID-19 outbreaks during the pandemic.
Public Health Implications. Tracking COVID-19 outbreaks by industry may help target prevention efforts, including workforce vaccination. (Am J Public Health. 2022;112(8):1180–1190. https://doi.org/10.2105/AJPH.2022.306862)
Work-related exposures and risk factors play an important role in COVID-19 disease transmission. Workers in certain industries, such as health care, agriculture, manufacturing, and transportation, have been found to be at increased risk for COVID-19 infection and mortality.1–3 In addition, overrepresentation of certain racial and ethnic groups in higher risk occupations and industries may contribute to the disproportionate burden of COVID-19 morbidity and mortality experienced by those groups.2,4
COVID-19 outbreak data can provide additional information about which workers may be at higher risk for exposure and infection. Although COVID-19 outbreaks have been well documented in certain industries, including health care, corrections, and meat processing,5–8 less information is available about outbreaks in other types of potentially high-risk workplaces, and limited comprehensive information is available about which types of workplaces have been most affected by COVID-19 outbreaks. This type of information could help direct prevention efforts such as workplace-specific guidance, nonpharmaceutical interventions, and workplace- or industry-targeted vaccination campaigns.
In California, home to both the largest population and the highest total number of COVID-19 cases of any US state,9 employer reporting of workplace COVID-19 outbreaks is mandated under a state law that became effective January 1, 2021. The law also requires the California Department of Public Health (CDPH) to publicly report numbers of outbreaks and outbreak-associated cases by industry.10 Using these statewide data on COVID-19 outbreaks, as well as outbreak data reported by local health departments in 2020, we sought to describe which industries have experienced the highest burden of COVID-19 outbreaks during the pandemic. We also sought to describe temporal trends in COVID-19 outbreaks and characterize demographics of outbreak-associated cases.
METHODS
We analyzed all confirmed COVID-19 outbreaks reported to CDPH as of September 27, 2021, in which onset occurred between January 1, 2020, and August 31, 2021.
Outbreak Definitions and Reporting
Outbreak definitions vary by setting. In non–health care workplaces, CDPH defines an outbreak as 3 or more probable or confirmed COVID-19 cases within a 14-day period among people who are epidemiologically linked in the setting, are from different households, and are not identified as close contacts of each other in any other case investigation.11 Separate definitions apply to health care workplaces; for example, in long-term care facilities, an outbreak is defined as 1 or more facility-acquired cases in a resident.12
Potential outbreaks are reported to local health departments (LHDs) by employers or facilities; LHDs may also identify outbreaks via individual case investigations and contact tracing. During 2020, requirements for employers to report outbreaks to LHDs varied by type of workplace and jurisdiction. Since January 1, 2021, however, California law has required non–health care employers to report to their LHD when they identify 3 or more cases of COVID-19 among workers in a workplace within a 14-day period; separate reporting requirements apply to health care facilities.
Once notified by an employer, LHDs investigate to determine whether the reported cases constitute an outbreak according to the specified CDPH outbreak definitions. LHDs then report confirmed outbreaks to CDPH via established electronic reporting systems, as required by existing California regulations.13
Outbreak reports also include numbers of associated cases. Outbreak-associated cases may include workers as well as nonworkers present at the worksite, such as residents or patients in congregate residential or health care settings or students in educational settings. LHDs are asked to link patient records for outbreak-associated cases to outbreak reports in electronic reporting systems, although not all LHDs consistently do so. For outbreak-linked cases for which data were available, we analyzed demographic variables such as sex, age, and race/ethnicity. Because nonworker cases cannot be reliably distinguished from worker cases on the basis of information submitted by LHDs, we analyzed these demographic variables across all outbreak-associated cases reported to CDPH, including cases among both workers and nonworkers.
Industry Assignments and Incidence Calculations
A CDPH team trained in industry coding reviewed available information for individual outbreaks reported to CDPH, including location name, address, and LHD outbreak descriptions, and assigned each outbreak a 2012 US census 4-digit industry code.14 Each individual industry is also part of a larger industry sector (e.g., hospitals are an individual industry that is part of the health care and social assistance sector). Total numbers of reported outbreaks and outbreak-associated cases were calculated for each individual industry as well as each industry sector. Outbreak incidence by sector and individual industry was calculated by dividing numbers of reported outbreaks by numbers of establishments in each industry or sector. If a single facility reported more than 1 outbreak during the study period, each outbreak was counted separately (i.e., a single facility could be responsible for more than 1 outbreak in the data set).
Numbers of establishments were obtained from the California Employment Development Department’s Quarterly Census of Employment and Wages and were calculated as the average numbers of establishments from the first through fourth quarters of 2020; 6-digit North American Industrial Classification System codes used by the Employment Development Department to classify establishments were crosswalked to US census industry codes. For a limited number of US census industry codes (0590, 0690, 1290, 2990, 3290, 3875, 3980, 4590, and 5590), no North American Industrial Classification System code is available that crosswalks directly to the specific 2012 US census industry code; these industries were therefore excluded from outbreak incidence calculations. (A total of 120 outbreaks and 1476 outbreak-associated cases occurred in these excluded industries. Among them, the “not specified food industries” category [census code 1290] included the most reported outbreaks [56] and outbreak-associated cases [1017].)
We also ranked industries according to their prevention indexes. The prevention index is a tool that can be used, alongside other considerations, to prioritize occupational health and safety interventions. As described elsewhere, we calculated prevention indexes by ranking industries according to outbreak count and outbreak incidence and dividing the sum of the count and incidence ranks by 2; this produced a prevention index for each industry, with lower prevention indexes corresponding to a higher priority for intervention.15 We rank ordered individual industries by prevention index values (with rank 1 as the highest priority).
RESULTS
Local health departments reported to CDPH 19 893 COVID-19 outbreaks and 300 379 outbreak-associated cases in which onset occurred between January 1, 2020, and August 31, 2021; this corresponded to an incidence of 12.2 outbreaks per 1000 establishments. An additional 489 outbreaks were reported to CDPH but were excluded because of insufficient information to assign an industry code (281) or because they occurred in homeless encampments, a nonoccupational setting (208). Outbreak-associated cases represented 7.0% of COVID-19 cases reported in California during this period.
A total of 9513 outbreaks (47.8%) and 164 659 outbreak-associated cases (54.8%) were reported in the health care and social assistance sector (Table 1). Other sectors with high percentages of outbreaks included retail trade (8.6%), manufacturing (7.9%), and accommodation and food services (7.3%). The sector with the highest overall incidence of reported outbreaks (78.1 outbreaks per 1000 establishments) was public administration, which includes correctional facilities and public safety establishments such as police and fire services.
TABLE 1—
COVID-19 Outbreaks and Outbreak-Associated Cases, by Industry Sector: California, January 2020–August 2021
| Industry Sectora | No. of Reported Outbreaks (%) | No. of Outbreak-Associated Cases (%) | Mean No. of Outbreak-Associated Cases per Outbreak | Outbreak Incidence (per 1000 Establishments) |
| Health care and social assistance | 9 513 (47.8) | 164 659 (54.8) | 17.3 | 14.8 |
| Retail trade | 1 706 (8.6) | 16 201 (5.4) | 9.5 | 15.9 |
| Manufacturing | 1 576 (7.9) | 22 570 (7.5) | 14.3 | 35.7 |
| Accommodation and food services | 1 461 (7.3) | 9 423 (3.1) | 6.4 | 16.4 |
| Educational services | 1 224 (6.2) | 10 333 (3.4) | 8.4 | 35.1 |
| Public administration | 954 (4.8) | 41 218 (13.7) | 43.2 | 78.1 |
| Transportation and warehousing | 689 (3.5) | 13 356 (4.4) | 19.4 | 21.7 |
| Construction | 499 (2.5) | 3 874 (1.3) | 7.8 | 5.7 |
| Other services, except public administration | 447 (2.2) | 3 451 (1.1) | 7.7 | 4.5 |
| Wholesale trade | 305 (1.5) | 3 463 (1.2) | 11.4 | 4.7 |
| Professional, scientific, and technical services | 263 (1.3) | 1 598 (0.5) | 6.1 | 1.6 |
| Real estate and rental and leasing | 256 (1.3) | 1 751 (0.6) | 6.8 | 4.2 |
| Administrative and support and waste management services | 218 (1.1) | 1 553 (0.5) | 7.1 | 3.8 |
| Agriculture, forestry, fishing, and hunting | 215 (1.1) | 2 679 (0.9) | 12.5 | 13.3 |
| Finance and insurance | 187 (0.9) | 1 109 (0.4) | 5.9 | 3.5 |
| Arts, entertainment, and recreation | 176 (0.9) | 1 744 (0.6) | 9.9 | 5.8 |
| Utilities | 85 (0.4) | 450 (0.1) | 5.3 | 52.4 |
| Information | 69 (0.3) | 470 (0.2) | 6.8 | 2.3 |
| Management of companies and enterprises | 31 (0.2) | 313 (0.1) | 10.1 | 6.5 |
| Mining, quarrying, and oil and gas extraction | 15 (0.1) | 88 (0.0) | 5.9 | 19.1 |
| Military | 4 (0.0) | 76 (0.0) | 19.0 | 25.3 |
| Total | 19 893 | 300 379 | 15.1 | 12.2 |
Industry sectors are listed in descending order of number of reported outbreaks.
Among individual industries in the health care and social assistance sector (Table 2), percentages and outbreak incidence values were highest in residential care facilities (22.8% of all outbreaks; 544 outbreaks per 1000 establishments), skilled nursing facilities (13.0%; 1306 per 1000), community food and housing and emergency services, including homeless shelters (3.3%; 425 per 1000), and hospitals (2.9%; 409 per 1000). Among individual retail industries, outbreak percentages were highest in grocery stores (2.5% of all outbreaks; 47 per 1000) and department and discount stores (1.3%; 272 per 1000). Restaurants, part of the accommodation and food services sector, had the third-highest percentage of outbreaks of any individual industry (6.5%; 16 per 1000).
TABLE 2—
COVID-19 Outbreaks and Outbreak-Associated Cases in the 25 Industries With the Highest Numbers of Outbreaks: California, January 2020–August 2021
| Industry | US Census Industry Code | No. of Reported Outbreaksa | No. of Outbreak- Associated Cases | No. of Industry Establishmentsb | Outbreak Incidence (per 1000 Establishments) | Prevention Index Rankingc |
| Residential care facilities, except skilled nursing facilities | 8290 | 4 518 | 52 410 | 8 300 | 544.4 | 2 |
| Skilled nursing facilities | 8270 | 2 585 | 91 120 | 1 979 | 1 306.4 | 1 |
| Restaurants and other food services | 8680 | 1 291 | 7 821 | 78 935 | 16.4 | 32 |
| Elementary and secondary schools | 7860 | 963 | 6 137 | 16 086 | 59.9 | 9 |
| Justice, public order, and safety activities | 9470 | 696 | 39 166 | 3 357 | 207.3 | 5 |
| Community food and housing and emergency services | 8380 | 654 | 5 508 | 1 538 | 425.0 | 3 |
| Hospitals | 8190 | 581 | 8 486 | 1 422 | 408.6 | 4 |
| Grocery stores | 4970 | 501 | 3 772 | 10 782 | 46.5 | 18 |
| Construction | 0770 | 499 | 3 874 | 87 451 | 5.7 | 61 |
| Child day care services | 8470 | 474 | 2 604 | 8 789 | 53.9 | 16 |
| Warehousing and storage | 6390 | 327 | 7 828 | 2 308 | 141.7 | 7 |
| Automobile dealers | 4670 | 267 | 2 342 | 3 452 | 77.3 | 8 |
| Department stores and discount stores | 5380 | 266 | 2 834 | 978 | 272.0 | 6 |
| Outpatient care centers | 8090 | 262 | 1 583 | 5 949 | 44.0 | 20 |
| Real estate | 7070 | 222 | 1 570 | 54 104 | 4.1 | 71 |
| Colleges, universities, and professional schools, including junior colleges | 7870 | 217 | 3 858 | 4 999 | 43.4 | 25 |
| Individual and family services | 8370 | 215 | 1 691 | 531 624 | 0.4 | 124 |
| Religious organizations | 9160 | 193 | 1 611 | 3 087 | 62.5 | 15 |
| Building material and supplies dealers | 4870 | 179 | 1 813 | 4 030 | 44.4 | 21 |
| Crop production | 0170 | 169 | 2 126 | 8 568 | 19.7 | 36 |
| Traveler accommodation | 8660 | 141 | 1 322 | 6 399 | 22.0 | 33 |
| Miscellaneous general merchandise stores | 5390 | 135 | 2 482 | 2 949 | 45.8 | 24 |
| Other amusement, gambling, and recreation industries | 8590 | 135 | 929 | 9 283 | 14.5 | 43 |
| Medical equipment and supplies manufacturing | 3960 | 127 | 1 487 | 1 811 | 70.1 | 14 |
| Bus service and urban transit | 6180 | 118 | 891 | 1 503 | 78.5 | 10 |
Note. The 25 industries shown here represented 79.1% of all outbreaks and 85.0% of all outbreak-associated cases.
If a single facility reported more than 1 outbreak during the study period, each outbreak was counted separately (i.e., a single facility might be responsible for more than 1 outbreak in the data set).
Data on numbers of establishments by industry were obtained from the California Employment Development Department Quarterly Census of Employment and Wages and calculated as the average number of establishments from the first through the fourth quarter of 2020.
Prevention indexes were calculated as the average of the count rank and the incidence rank; the numbers shown here represent prevention index rankings among all individual industries. A lower numeric prevention index ranking indicates an industry with a higher priority for intervention.
Seventy-three percent of outbreaks involved 10 or fewer associated cases; the median was 5 cases per outbreak (interquartile range = 3–11). Although most outbreaks were small, 389 (2%) involved more than 100 associated cases. Larger outbreaks were observed in certain congregate living settings where cases occurred among workers as well as residents, as evidenced by higher mean numbers of outbreak-associated cases in those settings. Examples include the justice, public order, and safety activities industry, which includes correctional facilities (mean of 56.3 cases per outbreak), and skilled nursing facilities (35.3 cases per outbreak). Mean numbers of cases per outbreak were also high in certain manufacturing industries such as ship and boat building (55.7 cases per outbreak), cut and sew apparel manufacturing (33.0 cases per outbreak), and animal slaughtering and processing (32.5 cases per outbreak).
The 5 industries with the highest prevention index rankings were skilled nursing facilities, residential care facilities, community food and housing and emergency services, hospitals, and justice, public order, and safety activities (Table 2). Several manufacturing industries not included in Table 2 because of lower total numbers of outbreaks had high prevention index rankings as a result of their higher outbreak incidence levels; these industries included animal slaughtering and processing (182 per 1000; prevention index rank = 11), aerospace products and parts manufacturing (555 per 1000; rank = 12), fruit and vegetable preserving and specialty food manufacturing (134 per 1000; rank = 13), and seafood and other miscellaneous foods manufacturing (70 per 1000; rank = 17).
Case-level information was available for 162 207 (54.0%) outbreak-associated cases. The availability of case-level data varied across industry sectors and was lowest in the information (32.6%), wholesale trade (32.9%), and construction (34.8%) sectors and highest in the public administration sector (82.4%).
Among outbreak-associated cases with available information, 84 653 of 159 351 (53.1%) cases occurred among men and 82 523 of 162 104 (50.9%) among individuals 18 to 49 years of age (Table A, available as a supplement to the online version of this article at http://www.ajph.org). Race/ethnicity information was missing for 24.8% of cases with available case-level data and 59.4% of cases overall. Among cases with available information, the distribution by race and ethnicity varied across industry sectors (Table 3; Figure A, available as a supplement to the online version of this article at http://www.ajph.org); for example, Latino people were most highly represented in the agriculture sector (84.2% of cases), whereas Asian people were most highly represented in the real estate sector (16.6%) and Black people in the public administration sector (13.2%).
TABLE 3—
Race/Ethnicity of Individuals With Outbreak-Associated COVID-19 Cases, by Industry Sector: California, January 2020–August 2021
| Industry Sector | Latino, No. (%) | White, No. (%) | Asian, No. (%) | Black, No. (%) | Other,a No. (%) | Unknown, No. (%) |
| Health care and social assistance (n = 85 766) | 16 066 (18.7) | 27 158 (31.7) | 9 477 (11.0) | 5 389 (6.3) | 8 643 (10.1) | 19 033 (22.2) |
| Public administration (n = 33 954) | 7 868 (23.2) | 4 627 (13.6) | 545 (1.6) | 2 274 (6.7) | 1 830 (5.4) | 16 810 (49.5) |
| Manufacturing (n = 8 228) | 4 339 (52.7) | 973 (11.8) | 1 063 (12.9) | 153 (1.9) | 793 (9.6) | 907 (11.0) |
| Retail trade (n = 7 491) | 3 587 (47.9) | 1 707 (22.8) | 476 (6.4) | 242 (3.2) | 787 (10.5) | 692 (9.2) |
| Educational services (n = 5 303) | 1 598 (30.1) | 2 029 (38.3) | 261 (4.9) | 236 (4.5) | 575 (10.8) | 604 (11.4) |
| Transportation and warehousing (n = 5 203) | 2 505 (48.1) | 784 (15.1) | 421 (8.1) | 336 (6.5) | 606 (11.6) | 551 (10.6) |
| Accommodation and food services (n = 5 008) | 2 469 (49.3) | 1 275 (25.5) | 247 (4.9) | 147 (2.9) | 439 (8.8) | 431 (8.6) |
| Other services, except public administration (n = 2 390) | 919 (38.5) | 762 (31.9) | 214 (9.0) | 53 (2.2) | 232 (9.7) | 210 (8.8) |
| Agriculture, forestry, fishing, and hunting (n = 1 521) | 1 134 (74.6) | 88 (5.8) | 36 (2.4) | 4 (0.3) | 85 (5.6) | 174 (11.4) |
| Construction (n = 1 349) | 687 (50.9) | 350 (25.9) | 33 (2.4) | 26 (1.9) | 113 (8.4) | 140 (10.4) |
| Arts, entertainment, and recreation (n = 1 333) | 580 (43.5) | 376 (28.2) | 98 (7.4) | 33 (2.5) | 142 (10.7) | 104 (7.8) |
| Wholesale trade (n = 1 141) | 684 (59.9) | 156 (13.7) | 43 (3.8) | 14 (1.2) | 120 (10.5) | 124 (10.9) |
| Administrative and support and waste management services (n = 844) | 532 (63.0) | 101 (12.0) | 34 (4.0) | 34 (4.0) | 68 (8.1) | 75 (8.9) |
| Real estate and rental and leasing (n = 792) | 298 (37.6) | 179 (22.6) | 118 (14.9) | 60 (7.6) | 56 (7.1) | 81 (10.2) |
| Professional, scientific, and technical services (n = 739) | 257 (34.8) | 226 (30.6) | 79 (10.7) | 17 (2.3) | 72 (9.7) | 88 (11.9) |
| Finance and insurance (n = 514) | 196 (38.1) | 137 (26.7) | 30 (5.8) | 12 (2.3) | 59 (11.5) | 80 (15.6) |
| Utilities (n = 245) | 90 (36.7) | 76 (31.0) | 4 (1.6) | 12 (4.9) | 31 (12.7) | 32 (13.1) |
| Information (n = 153) | 80 (52.3) | 31 (20.3) | 13 (8.5) | 7 (4.6) | 14 (9.2) | 8 (5.2) |
| Management of companies and enterprises (n = 137) | 71 (51.8) | 23 (16.8) | 8 (5.8) | 3 (2.2) | 12 (8.8) | 20 (14.6) |
| Military (n = 60) | 8 (13.3) | 9 (15.0) | 1 (1.7) | 1 (1.7) | 1 (1.7) | 40 (66.7) |
| Mining, quarrying, and oil and gas extraction (n = 36) | 15 (41.7) | 11 (30.6) | 0 (0.0) | 0 (0.0) | 1 (2.8) | 9 (25.0) |
Note. Information is shown for all outbreak-associated cases for which case-level data were available (54% of cases); the percentage of cases with case-level data available varied by sector. See Figure A for data visualization.
Includes Native Hawaiian and other Pacific Islander, American Indian/Alaska Native, other, and multirace.
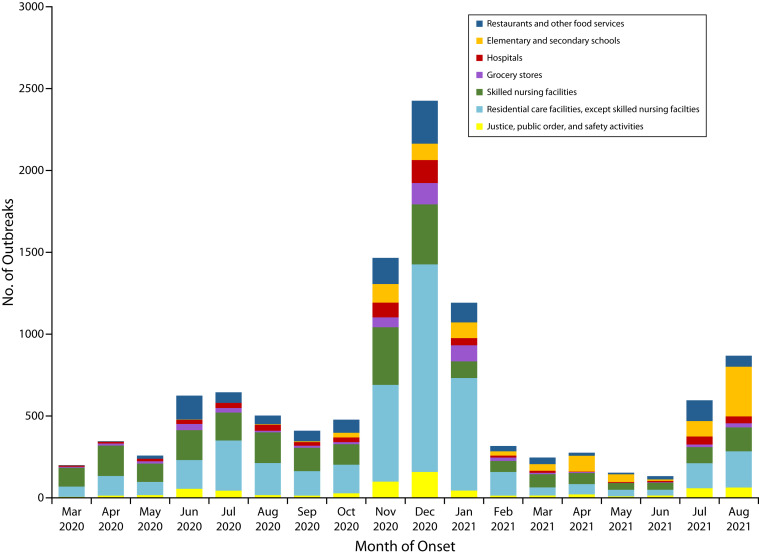
The largest numbers of reported outbreaks occurred during November 2020 to January 2021, coinciding with California’s winter 2020–2021 COVID-19 surge; the highest monthly number (21.0% of all outbreaks) was reported in December 2020. Outside of the winter surge, the highest numbers of monthly outbreaks during the study period were seen in July and August 2021 (5.7% and 6.9% of all outbreaks, respectively), coinciding with an increase in overall COVID-19 cases associated with the Delta variant.
During most months, the highest numbers of outbreaks were reported in residential care facilities and skilled nursing facilities; however, reported outbreaks were highest in elementary and secondary schools in April (34.8%) and May (30.5%) 2021 and in August 2021 (34.9%) (Figure 1; Table B, available as a supplement to the online version of this article at http://www.ajph.org). Overall, the percentage of outbreaks reported in the health care and social assistance sector decreased in 2021 (40.5%) relative to 2020 (52.0%); the percentages of outbreaks remained stable in most other sectors with the exception of educational services, which increased from 2.9% of reported outbreaks in 2020 to 11.8% in 2021 (Table C, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
COVID-19 Outbreaks in Top Industries Over Time: California, March 2020–August 2021
Note. Shown are the 7 industries with the highest total numbers of outbreaks. See Table B (available as a supplement to the online version of this article at https://www.ajph.org) for the data underlying this figure. Data for January and February 2020 are excluded because of low numbers of outbreaks (9 reported outbreaks with onset in January and 4 reported outbreaks in February).
DISCUSSION
We identified nearly 20 000 COVID-19 outbreaks reported in California from the beginning of the pandemic through August 2021. These outbreaks occurred across industry sectors, with the most outbreaks and outbreak-associated cases reported in the health care and social assistance sector, which includes residential care facilities and skilled nursing facilities. These known high-risk settings have been the focus of significant public health interventions during the COVID-19 pandemic, including setting-specific guidance and consultation, an emphasis on personal protective equipment and other protective measures, and early prioritization for vaccination.
However, our study also highlights additional industries with high counts and a high incidence of COVID-19 outbreaks such as restaurants and retail and manufacturing industries, where employees continued to report to work during the pandemic and had public-facing roles or worked in close proximity to others. Although these industries may have received less attention, their elevated burden of COVID-19 outbreaks merits intervention, including development of industry-specific strategies for outbreak prevention and response; specific outreach to workers and labor unions, employers and trade associations, and local health departments in areas where these industries are concentrated; and targeted vaccination campaigns.
Residential care facilities, skilled nursing facilities, and correctional facilities ranked highly in terms of both outbreak counts and incidence in California and require ongoing public health attention and intervention. These settings are known to involve a high risk of COVID-19 outbreaks owing to their vulnerable resident populations, frequent close contact between residents and staff, movement of residents and staff between facilities, and other factors.16 These are also congregate settings where nonworkers are present and often account for a significant proportion of cases. Although high outbreak case counts in these settings may therefore overestimate COVID-19 incidence rates among workers, they nonetheless likely result in an increased occupational risk of COVID-19 exposure. Health care facilities have also been subject to outbreak reporting mandates since early in the pandemic and have lower thresholds in terms of the number of cases required to be considered an outbreak; both of these factors may have led to increased numbers of reported outbreaks in these settings relative to others.
In addition to the known high-risk settings just discussed, we also identified other industries with high proportions of reported outbreaks. Given that prevention strategies are likely to differ across industries, such industries may require both additional prevention efforts and additional investigation of which interventions may be most effective in those specific settings. One such industry is the restaurant industry, which had the third-highest outbreak count of any individual industry. This corresponded to a relatively low outbreak incidence, likely as a result of the high number of establishments in this industry, but the large number of workers and workplaces potentially affected nonetheless warrant prioritization. In addition, many restaurants were closed for in-person dining in California during portions of the pandemic, which may have contributed to lower outbreak rates. As restaurants reopen, workers remain vulnerable to COVID-19 exposure from coworkers as well as from members of the public.
Several additional industries and sectors had high outbreak counts and incidence levels. The manufacturing and retail trade sectors each represented around 8% of all outbreaks reported to CDPH. These sectors have also been identified as high risk in other jurisdictions; in reports from Utah, Wisconsin, and Los Angeles, both manufacturing and retail ranked highly in numbers of COVID-19 outbreaks among non–health care, noncongregate settings during portions of 2020.4,17,18 Within the retail trade sector in California, several individual industries had high outbreak counts, incidence levels, and prevention index rankings, including grocery stores, department and discount stores, and automobile dealers, all workplaces where employees are likely to come into close, frequent contact with other employees as well as with members of the public.
Within the manufacturing sector, fewer individual industries ranked highly in outbreak counts, likely because of smaller industry sizes, but many had high outbreak incidence levels and prevention index rankings. Examples include several food processing industries such as animal slaughtering and processing, fruit and vegetable preserving, and seafood manufacturing, which have been documented settings of large COVID-19 outbreaks in numerous jurisdictions.8,19 High outbreak incidence levels were also seen in some nonfood manufacturing industries, in particular the aerospace manufacturing industry, which had the third-highest outbreak incidence of any individual industry.
Unlike workers in retail industries, workers in manufacturing industries are typically not public facing; most of these workers did, however, continue to report to work throughout the pandemic, typically in high-density workplaces where the risk of exposure to other workers with COVID-19 may be higher. Another industry with similar risk factors is the warehousing and storage industry, which had high outbreak counts, incidence levels, and prevention index rankings.
Outbreak-associated cases reported to CDPH represented 7% of COVID-19 cases in California; this finding was comparable to the percentage of cases associated with outbreaks in a Seattle report (5%) but lower than the percentage identified as outbreak associated in Utah (12%) and Wisconsin (18%).4,18,20 The true number of outbreak-associated cases is likely higher than the number reported to CDPH, as not all cases associated with an outbreak are identified as such and additional cases identified after the initial outbreak report are not consistently reported to CDPH.
Some demographic groups—in particular, communities of color and those of lower socioeconomic status—have been disproportionately affected by the COVID-19 pandemic, and the overrepresentation of these groups in certain essential industries and occupations may play a role in these disparities.21,22 In Utah, for example, Hispanic and non-White individuals represent 24% of the state’s workforce but were found to make up 73% of workplace outbreak-associated cases.4 In our outbreak data, the distribution of outbreak-associated cases among racial and ethnic groups was similar to the overall distribution of the state’s population; however, there were variations in the distribution of outbreak-associated cases by race and ethnicity across industry sectors.
For instance, in several sectors with high numbers of outbreaks, including manufacturing, retail, accommodation and food services, and transportation and warehousing, more than 50% of outbreak-associated cases with race/ethnicity information available involved Latino individuals. Given that Latino people have been disproportionately represented among COVID-19 cases and fatalities in California,21,23 these findings highlight occupational factors and enhanced workplace protections as a potential avenue for addressing disparities.
These demographic trends in our outbreak-associated case data should, however, be interpreted with caution. Race and ethnicity information was missing or unknown for nearly 60% of cases, and the amount of missing data varied across industry sectors. In addition, outbreak-associated cases included workers as well as nonworkers, so the demographic trends described here may not represent demographic trends among workers, particularly in certain settings with larger numbers of nonworkers present such as health care, correctional, and educational settings. Nonetheless, our findings as well as those of earlier reports indicate that public health interventions should continue to target industries with high proportions of workers from disproportionately affected groups and should be culturally and linguistically appropriate and informed by worker demographics. In addition, efforts should be made to improve collection and reporting of key demographic variables in outbreak data.
Numbers of reported outbreaks over time over time largely paralleled overall trends in COVID-19 cases in California, with the highest numbers of outbreaks seen during California’s winter 2020–2021 COVID-19 surge and a July and August 2021 increase in outbreaks alongside an overall increase in cases associated with the Delta variant. For the most part, the distribution of COVID-19 outbreaks across industries remained stable over time. One exception was elementary and secondary schools, which experienced few outbreaks in the early months of the pandemic, when they remained largely closed, but were responsible for a larger proportion of outbreaks during periods of 2021 when many California schools reopened for in-person learning.
Limitations
This report is subject to several additional limitations. Although a statewide requirement for non–health care employers to report outbreaks to LHDs has been in place since January 1, 2021, prior to that reporting requirements differed by local jurisdiction and by type of setting, which may have led to differential reporting across settings. The proportion of outbreaks reported in non–health care settings relative to health care settings increased from 2020 to 2021, which might suggest an increase in reporting following implementation of the statewide requirement; however, the proportions of outbreaks reported in most individual non–health care sectors, with the exception of educational services, remained relatively stable in 2020 and 2021. This year-to-year comparison should also be interpreted in the context of other changes over time; for example, closures in schools and other non–health care settings in 2020 and earlier availability of vaccination in health care and congregate settings may have led to fewer outbreaks in those settings relative to others.
In addition, although employers are required by law to report COVID-19 outbreaks, some may be unaware of or noncompliant with this requirement, which would lead to underestimation of outbreak incidence; it is also possible that consistency in reporting differs across industries. Furthermore, work arrangements in certain industries—for instance, industries with mobile or temporary workforces such as transportation or agriculture—might be less conducive to outbreak identification, which could lead to outbreak underreporting in those industries. CDPH outbreak data also rely on reports received from LHDs, and these local departments may have had limited resources to report outbreaks. Such limitations may have led to underestimated outbreak counts and incidence levels, particularly during COVID-19 surges.
We assigned industry codes on the basis of available information submitted by LHDs; misclassification may have occurred as a result of missing or inaccurate information. In addition, although many of the outbreaks included in our analysis occurred in settings where workers were present, some may have been nonoccupational; we were unable to distinguish workers from nonworkers in our outbreak data. This limitation precluded calculation of outbreak-associated case incidence levels among workers; because our outbreak incidence estimates did not account for numbers of workers per establishment, they may overestimate or underestimate the relative impact of workplace COVID-19 outbreaks on workers in industries with particularly large or small establishment sizes. Although prevention indexes incorporate data on burden of disease as well as disease risk, they do so with limited precision and should be used in the context of additional information and tools to prioritize interventions.
Finally, although outbreaks in our data set were classified by industry, we were unable to analyze COVID-19 incidence according to worker occupation. It is possible that increased risk of COVID-19 among certain occupational groups was not captured in our industry-based analysis.
Public Health Implications
Individual case investigations and contact tracing have formed the backbone of the response to COVID-19 in the United States but may not represent the most timely or complete methods for identifying COVID-19 workplace outbreaks, as workplace information is not always collected during individual case investigations and mechanisms may not exist for linking individual cases identified in the same workplace.20 Furthermore, during the current phase of the pandemic, as public health departments transition away from universal case investigation and contact tracing,24 employer reporting of workplace outbreaks can provide a mechanism for health departments to continue to identify higher-risk settings and target interventions.
An outbreak reporting mandate such as California’s may help ensure that such reporting happens more consistently and enable more systematic tracking of where COVID-19 outbreaks are taking place. The resulting outbreak data can be used to categorize outbreaks by industry, as we have done in this report, and identify settings with high numbers and incidence levels of outbreaks and outbreak-associated cases. The use of outbreak data to direct prevention efforts, including workforce vaccination, can play an important role in the ongoing effort to combat the COVID-19 pandemic and in planning for future pandemic responses to protect the workers who are most at risk.
ACKNOWLEDGMENTS
This work was supported by the California Department of Public Health. Kathryn Gibb, Andrea Rodriguez, and Jessie Wong were supported by Centers for Disease Control and Prevention (CDC) Cooperative Agreement for Emergency Response: Public Health Crisis Response (6 NU90TP922071-01-05) and the Epidemiology and Laboratory Capacity for Infectious Disease cooperative agreement (6 NU50CK000539). Matt Frederick and Elena Chan were supported through a cooperative agreement with the CDC National Institute for Occupational Safety and Health (U60-OH-008468-16).
We acknowledge members of the California Department of Public Health COVID-19 Response Team who contributed to outbreak data preparation, as well as local employers and health department staff in California who contributed COVID-19 outbreak data.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the views or opinions of the California Department of Public Health or the California Health and Human Services Agency.
CONFLICTS OF INTEREST
The authors do not report any conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study was determined by the California Health and Human Services Committee for the Protection of Human Subjects to be public health practice as opposed to research and was exempt from institutional review board review.
See also Hawkins, p. 1081.
REFERENCES
- 1.Chen Y-H, Glymour M, Riley A, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through November 2020. PLoS One. 2021;16(6):e0252454. doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63(9):817–820. doi: 10.1002/ajim.23145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mutambudzi M, Niedzwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2021;78(5):307–314. doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bui DP, McCaffrey K, Friedrichs M, et al. Racial and ethnic disparities among COVID-19 cases in workplace outbreaks by industry sector—Utah, March 6–June 5, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(33):1133–1138. doi: 10.15585/mmwr.mm6933e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanchez GV, Biedron C, Fink LR, et al. Initial and repeated point prevalence surveys to inform SARS-CoV-2 infection prevention in 26 skilled nursing facilities—Detroit, Michigan, March–May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):882–886. doi: 10.15585/mmwr.mm6927e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace M, Hagan L, Curran KG, et al. COVID-19 in correctional and detention facilities—United States, February–April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):587–590. doi: 10.15585/mmwr.mm6919e1. [DOI] [PubMed] [Google Scholar]
- 8.Waltenburg M, Rose C, Victoroff T, et al. Coronavirus disease among workers in food processing, food manufacturing, and agriculture workplaces. Emerg Infect Dis. 2021;27(1):243–249. doi: 10.3201/eid2701.203821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. 2021. https://covid.cdc.gov/covid-data-tracker/#trends
- 10.California Legislature. Assembly Bill. 2021. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200AB685
- 11.California Department of Public Health. 2021. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/OutbreakDefinitionandReportingGuidance.aspx
- 12. California Department of Public Health. 2021;20-75.1 https://www.cdph.ca.gov/Programs/CHCQ/LCP/Pages/AFL-20-75.aspx [Google Scholar]
- 13.California Code of Regulations. 2021. https://www.law.cornell.edu/regulations/california/17-CCR-Sec-2502 [PubMed]
- 14.US Census Bureau. 2012 industry code list. Available at. 2021. https://www2.census.gov/programs-surveys/demo/guidance/industry-occupation/census-2012-final-code-list.xls
- 15.Bonauto D, Silverstein B, Adams D, Foley M. Prioritizing industries for occupational injury and illness prevention and research, Washington State workers’ compensation claims, 1999–2003. J Occup Environ Med. 2006;48(8):840–851. doi: 10.1097/01.jom.0000225062.88285.b3. [DOI] [PubMed] [Google Scholar]
- 16.McMichael TM, Clark S, Pogosjans S, et al. COVID-19 in a long-term care facility—King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Contreras Z, Ngo V, Pulido M, et al. Industry sectors highly affected by worksite outbreaks of coronavirus disease, Los Angeles County, California, USA, March 19–September 30, 2020. Emerg Infect Dis. 2021;27(7):1769–1775. doi: 10.3201/eid2707.210425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pray IW, Kocharian A, Mason J, Westergaard R, Meiman J. Trends in outbreak-associated cases of COVID-19—Wisconsin, March–November 2020. MMWR Morb Mortal Wkly Rep. 2021;70(4):114–117. doi: 10.15585/mmwr.mm7004a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Porter KA, Ramaswamy M, Koloski T, Castrodale L, McLaughlin J. COVID-19 among workers in the seafood processing industry: implications for prevention measures—Alaska, March–October 2020. MMWR Morb Mortal Wkly Rep. 2021;70(17):622–626. doi: 10.15585/mmwr.mm7017a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonwitt J, Deya RW, Currie DW, et al. COVID-19 surveillance and investigations in workplaces—Seattle & King County, Washington, June 15–November 15, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(25):916–921. doi: 10.15585/mmwr.mm7025a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia E, Eckel SP, Chen Z, Li K, Gilliland FD. COVID-19 mortality in California based on death certificates: disproportionate impacts across racial/ethnic groups and nativity. Ann Epidemiol. 2021;58:69–75. doi: 10.1016/j.annepidem.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess deaths associated with COVID-19, by age and race and ethnicity—United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1522–1527. doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.California Department of Public Health. 2021. https://covid19.ca.gov/state-dashboard/#ethnicity-gender-age
- 24.Council of State and Territorial Epidemiologists. Public health agencies transitioning away from universal case investigation and contact tracing for individual cases of COVID-19. 2021. https://www.naccho.org/blog/articles/joint-statement-public-health-agencies-transitioning-away-from-universal-case-investigation-and-contact-tracing-for-individual-cases-of-covid-19