Abstract
Xylazine is a nonopioid veterinary anesthetic and sedative that is increasingly detected in the illicit drug supply in the United States. Data indicate a striking prevalence of xylazine among opioid-involved overdose deaths.
The emergence of xylazine in the illicit drug supply poses many unknowns and potential risks for people who use drugs. The public health system needs to respond by increasing testing to determine the prevalence of xylazine, identifying its potential toxicity at various exposure levels, and taking mitigating action to prevent harms.
Currently, there is little testing capable of identifying xylazine in drug supplies, which limits the possibility of public health intervention, implementation of harm reduction strategies, or development of novel treatment strategies. (Am J Public Health. 2022;112(8):1212–1216. https://doi.org/10.2105/AJPH.2022.306881)
Xylazine is a veterinary pharmaceutical that is rapidly disseminating across the unregulated drug supply in the United States. It is not commonly tested for in clinical settings or forensic testing labs and can be deadly.1,2 As recently as 2018, xylazine was rarely seen in the US drug markets, but it is now a common additive to substances like fentanyl, heroin, and cocaine. Most concerning is its increasing involvement in drug overdose deaths.3
Xylazine is a nonopioid anesthetic and sedative approved by the US Food and Drug Administration for use in veterinary medicine but not for use in humans.4 It is an α-2 adrenergic receptor agonist that has a chemical structure similar to dexmedetomidine, a paralytic, and clonidine, an antihypertensive, as well as phenothiazines and tricyclic antidepressants.4,5 In humans, α-2 agonist medications similar to xylazine are often used as adjunctive medications in anesthesia to reduce the requirement for general anesthesia.6 The effects of xylazine are primarily actuated in the central nervous system (CNS) via the locus coeruleus, which then causes sedation, analgesia, and muscle relaxation.5 These actions appear to be mediated by xylazine inhibiting the release of norepinephrine in the CNS, leading to decreased excitatory action.7
The effects of xylazine that may contribute to overdose risk in humans include CNS depression, hypotension, bradycardia, and respiratory depression.8 When combined with opioids, xylazine increases the potential for fatal respiratory depression. Although the opioid reversal agent naloxone plays a critical role in responding to any overdose with possible opioid involvement, it does not reverse the effects of xylazine. Furthermore, there is no specific reversal agent for xylazine approved for use in humans, although the α-2 adrenergic antagonist tolazoline has been described as a xylazine reversal agent in veterinary medicine.9 Consequently, people who ingest xylazine may need acute medical care, including mechanical ventilation.8 Without timely and widespread testing for xylazine, clinicians are underprepared to recognize and respond to the medical needs of people exposed to it.
In this article, we describe current trends of xylazine in the US drug supply highlighting state-level data from Connecticut, identify clinical concerns, and present recommendations for addressing xylazine contamination moving forward.
CURRENT TRENDS IN DRUG SUPPLY
Xylazine was first reported as a frequently encountered drug contaminant in Puerto Rico in 2001.10 Since then, reports from Pennsylvania, Connecticut, and other areas of the United States have arisen.3,11,12 Starting in 2019, xylazine first presented in toxicology reports of opioid overdose fatalities in Connecticut.13 Over the last 2 years, xylazine has more than doubled in prevalence among fatal opioid overdoses in Connecticut,14 with similar increases reported in Philadelphia, Pennsylvania,3 implying widespread and underrecognized adulteration of the illicit drug supply. Besides being used as an adulterant, xylazine is sought out by some individuals for its effects when combined with other substances, in part leading to its increased prevalence.
Xylazine is rapidly increasing in prevalence among various illicit substances, primarily in combination with fentanyl, but is also found in samples containing cocaine, heroin, and other substances.15 The effects of xylazine are thought to enhance, prolong, or modify the effects of heroin and fentanyl, and recent mixed methodologies including ethnographic data note that people use xylazine to extend the “legs” (duration of opioid effect) of fentanyl.16 In 2014, it was believed to be more accessible and easier to acquire than substances such as fentanyl because xylazine is not classified as a controlled substance.8 Furthermore, xylazine may serve as a bulking agent that can be used by street-level distributers to extend the supply of their other drug products.11,17
In Puerto Rico, xylazine has been used for almost 2 decades. Despite long-time knowledge that xylazine has been used as an adulterant of other substances, little has been done in terms of prevention, surveillance, and education regarding this substance. In the United States, xylazine is currently emerging as a significant component of the drug supply and appears to be regional. Current data show that in 2019 only 2% of all drug overdose deaths contained xylazine, but the majority of cases (67%) were in the northeastern United States.12 However, this regional distribution could reflect the uneven availability of toxicology testing for xylazine, with variability across counties and states, rather than the true distribution of xylazine, which may be more widespread.
STATEWIDE DATA FROM CONNECTICUT
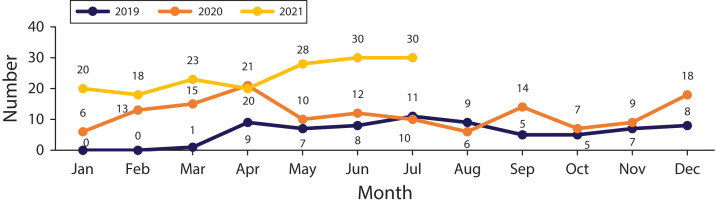
All suspected overdoses in the state of Connecticut are investigated through the Office of the Chief Medical Examiner, and toxicology testing is standardized statewide; xylazine testing commenced in 2013 for all suspected accidental drug intoxication deaths.13 Monthly and annually, the Connecticut Department of Public Health releases an update on fatal drug overdoses. The department’s August 2021 monthly report showed rising rates of xylazine-involved overdose deaths since they started tracking in 2019 (Figure 1).14 In 2019, the first report of xylazine among opioid-involved overdose deaths in Connecticut identified 71 deaths containing xylazine and fentanyl. In 2020, 141 overdose deaths involving xylazine and fentanyl were reported, and in the first 30 weeks of 2021 there were 172 overdose deaths involving xylazine and fentanyl. In August 2021, data from the report indicated that xylazine prevalence among fatal opioid overdoses was rapidly increasing.14 The US Centers for Disease Control and Prevention (CDC) reported that between 2019 and July 2020, Connecticut saw unintentional drug overdose deaths with a lethal combination of fentanyl and xylazine increase from 5.8% to 11.4% of cases.11
FIGURE 1—
Number of Xylazine-Involved Overdose Deaths, by Month: Connecticut, 2019–2021
Source. Adapted from the Connecticut Department of Public Health.14
NATIONAL DATA
National data are similar to the trends seen in Connecticut, with evidence of increased prevalence of xylazine in the US drug supply. In 2019, the CDC released a report indicating that xylazine had been identified in postmortem toxicology samples from drug overdose deaths in 25 of the 38 states that were examined.12 Prevalence of xylazine-involved overdose deaths has risen over the past year, with states including Connecticut, Massachusetts, and Pennsylvania reporting substantial increases in the number of cases identified from postmortem toxicology testing over the past 1 to 2 years.3,11,18 The CDC also reported that xylazine was identified in over 3800 national toxicological surveillance samples reported from 2015 through December 2020, with progressive increases each year, culminating in 1492 reports in 2020.12
DATA LIMITATIONS
Reported increases in prevalence of xylazine-involved overdose deaths significantly underestimate true prevalence because of wide variation in how cause of death is reported and how postmortem samples are tested within and across states.1 Causes of death are classified according to International Classification of Diseases, 10th Revision (ICD-10) classifications, many of which do not specify the substance involved (e.g., “other opioid,” “other narcotic,” or “drug overdose”). Thus, even if the involved substance is known, it is not captured via current overdose death reporting systems. Although the National Association of Medical Examiners recommends listing all involved substances on death certificates, this recommendation is not universally adopted in standard practice.1 Furthermore, xylazine involvement is likely being undercounted among overdose deaths because testing only occurs at the request of the medical examiner and not in routine practice.8
CLINICAL CONCERNS
The clinical effects of acute xylazine toxicity in humans are not well defined but generally include significant respiratory depression, bradycardia, hypotension, and decreased consciousness.8 There are no specific reversal agents for xylazine toxicity approved for use in humans, and supportive measures such as mechanical ventilation, fluid resuscitation, blood pressure management, and heart rate monitoring may be indicated.8
Another important clinical concern is unique skin lesions associated with chronic xylazine injection, typically appearing as abscesses or ulcerations predominantly on the extremities.19 Multiple associations have been made between xylazine and severe skin ulcerations based on observational studies.19,20 Although a link has not yet been definitively established, it is important to recognize these severe skin lesions as potentially xylazine related to effectively address the underlying cause and recommend cessation of xylazine injection, both intentional and unintentional. Of note, these ulcerations are not specifically localized to the sites of injection but can occur diffusely.10
RECOMMENDATIONS
The rising prevalence of xylazine in the drug supply is a concerning trend that may be altering the risk profile of substance use, changing use patterns, and affecting treatment response for individuals with suspected overdose events. To further understand the impact of xylazine on the drug supply and on drug users, additional testing, research, education, and harm reduction measures are needed.
Testing
Despite postmortem testing showing xylazine involvement in an increasing number of overdose deaths, there remains minimal screening, surveillance, or monitoring for xylazine among people who use drugs, or of the drug supply itself. There is great need for improved surveillance to develop a better understanding of the current drug supply. This information is crucial for an appropriate and directed public health response and for first responders and clinicians making medical decisions related to xylazine-involved drug overdoses and associated complications.
Despite there being high-quality, detailed data from Connecticut, Philadelphia, and a few other areas in the Northeast United States, overall, there is a dearth of surveillance testing and therefore a scarcity of information on the prevalence of xylazine, both nationally and in most localities. All cases of suspected drug overdose should include xylazine testing; however, current xylazine testing requires a comprehensive toxicology screen via gas chromatography–mass spectrometry, which is a timely and costly barrier to widespread screening. A rapid xylazine screening test needs to be developed and disseminated to allow for point-of-care testing for clinical and individual use. In fact, point-of-care drug checking services using Fourier transform infrared spectroscopy have identified xylazine in the drug supply.21 Given the growing presence of xylazine in drug overdose deaths, test kit developers should consider creating xylazine test strips, similar to fentanyl test strips (rapid antigen testing for use on urine samples), to allow for rapid detection of xylazine in settings utilizing drug checking technologies to identify components of unregulated substances prior to use.
Research
Research is critical to better understanding the national distribution of xylazine in the drug supply, the physiological effects of xylazine in humans at various exposure levels, and the combined effects of xylazine and other commonly used drugs (e.g., fentanyl, heroin, cocaine, amphetamines). One important area of clinical research is determining any causal relationship between xylazine and skin ulcerations and ways to treat and prevent these dangerous complications. The safety and effectiveness of tolazoline as a reversal agent for xylazine-related sedation in humans should also be investigated. More qualitative research, including ethnography, is critical to understanding how people are managing xylazine’s risks, adapting their use patterns, and avoiding the substance or seeking it out, and to knowing the drug’s relative availability and cost on the street and its embodied effects.
Patient and Clinician Education
Education about the presence of xylazine in the drug supply is important for both patients and clinicians. First-line medical staff and responders—including emergency medical technicians, paramedics, emergency medicine clinicians, and people who use drugs—need to be aware of its rising prevalence as well as what to do in cases of suspected xylazine-involved overdose. In addition to continuing the use of naloxone for all overdoses with potential opioid involvement, all first responders should consider xylazine as a contributor when response to naloxone administration is inadequate, and be prepared to provide hemodynamic support for xylazine-induced hypotension. Testing for xylazine should be performed, if available, and those with confirmed or suspected xylazine exposure should be evaluated for skin ulcerations. Importantly, testing the drug supply, and informing people who use drugs of identified contaminants, provides them the opportunity to modify their behaviors and incorporate harm reduction strategies.
Harm Reduction
Because there are currently no specific interventions for xylazine, it is important to continue to recommend and implement universal harm reduction measures as the prevalence of xylazine increases around the country. Harm reduction strategies and education on xylazine should be given to all individuals who use drugs. These harm reduction interventions include the following:
• Never use drugs alone. If using alone, individuals should take advantage of resources such as the Never Use Alone hotline (1-800-484-3731).22
• Always have and know how to use naloxone if using unregulated substances. Always administer naloxone in response to any suspected overdose, including suspected xylazine, to reverse any possible opioid involvement.
• Start low and go slow: use a small test sample first to ensure that potency and effects are what is expected. Give ample time between dosing. Stagger use if using with others, so that 1 person can administer naloxone if necessary.
• Use from the same supplier if possible.
• Adopt safe injection practices (sterile syringes, clean skin with alcohol swab, don’t lick needles, don’t share or reuse needles).
• Seek medical care for unusual abscesses.
• Always contact emergency services in the event of drug overdose. Naloxone will not reverse the effects of xylazine.
CONCLUSION
The emergence of xylazine in the US drug supply represents a growing threat to people who use drugs. Coupled with the rise of high-potency synthetic opioids, such as fentanyl and its analogs, xylazine is a new potential risk in an ongoing overdose crisis. Initial steps to addressing this threat must include expanded xylazine testing, patient and clinician education on its risks, and promotion of harm reduction strategies to prevent further morbidity and mortality.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This work did not involve human participants and was institutional review board exempt.
REFERENCES
- 1.Slavova S, O’Brien DB, Creppage K, et al. Drug overdose deaths: let’s get specific. Public Health Rep. 2015;130(4):339–342. doi: 10.1177/003335491513000411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spoerke DG, Hall AH, Grimes MJ, Honea BN, Rumack BH. Human overdose with the veterinary tranquilizer xylazine. Am J Emerg Med. 1986;4(3):222–224. doi: 10.1016/0735-6757(86)90070-7. [DOI] [PubMed] [Google Scholar]
- 3.Johnson J, Pizzicato L, Johnson C, Viner K. Increasing presence of xylazine in heroin and/or fentanyl deaths, Philadelphia, Pennsylvania, 2010–2019. Inj Prev. 2021;27(4):395–398. doi: 10.1136/injuryprev-2020-043968. [DOI] [PubMed] [Google Scholar]
- 4.Drug Enforcement Administration. 2021. https://www.deadiversion.usdoj.gov/drug_chem_info/Xylazine.pdf
- 5.Hoffmann U, Meister CM, Golle K, Zschiesche M. Severe intoxication with the veterinary tranquilizer xylazine in humans. J Anal Toxicol. 2001;25(4):245–249. doi: 10.1093/jat/25.4.245. [DOI] [PubMed] [Google Scholar]
- 6.Giovannitti JA, Thoms SM, Crawford JJ. Alpha-2 adrenergic receptor agonists: a review of current clinical applications. Anesth Prog. 2015;62(1):31–39. doi: 10.2344/0003-3006-62.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinclair MD. A review of the physiological effects of α2-agonists related to the clinical use of medetomidine in small animal practice. Can Vet J. 2003;44(11):885–897. [PMC free article] [PubMed] [Google Scholar]
- 8.Ruiz-Colón K, Chavez-Arias C, Díaz-Alcalá JE, Martínez MA. Xylazine intoxication in humans and its importance as an emerging adulterant in abused drugs: a comprehensive review of the literature. Forensic Sci Int. 2014;240:1–8. doi: 10.1016/j.forsciint.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Agricultural Marketing Service, US Dept of Agriculture; Xylazine, tolazoline. 2022. https://www.ams.usda.gov/rules-regulations/organic/national-list
- 10.Torruella RA. Xylazine (veterinary sedative) use in Puerto Rico. Subst Abuse Treat Prev Policy. 2011;6(1):7. doi: 10.1186/1747-597X-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thangada S, Clinton HA, Ali S, et al. Notes from the field: xylazine, a veterinary tranquilizer, identified as an emerging novel substance in drug overdose deaths—Connecticut, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70(37):1303–1304. doi: 10.15585/mmwr.mm7037a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kariisa M, Patel P, Smith H, Bitting J. Notes from the field: xylazine detection and involvement in drug overdose deaths—United States, 2019. MMWR Morb Mortal Wkly Rep. 2021;70(37):1300–1302. doi: 10.15585/mmwr.mm7037a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nunez J, DeJoseph ME, Gill JR. Xylazine, a veterinary tranquilizer, detected in 42 accidental fentanyl intoxication deaths. Am J Forensic Med Pathol. 2021;42(1):9–11. doi: 10.1097/PAF.0000000000000622. [DOI] [PubMed] [Google Scholar]
- 14.Connecticut Dept of Public Health. Drug Overdose Monthly Report. 2021. https://portal.ct.gov/-/media/DPH/Injury-Prevention/Opioid-Overdose-Data/Monthly-Death-Reports/August-2021-_2020-and-2019-Drug-Overdose-Deaths-Monthly-Report_CT_-9-13-2021_Final.pdf.
- 15.Evans A, Krause M, Leach S, Levitas M, Nguyen L, Short LC. Analysis of drug residue in needle-exchange syringes in Washington, DC. Forensic Sci Int. 2021;329:111083. doi: 10.1016/j.forsciint.2021.111083. [DOI] [PubMed] [Google Scholar]
- 16.Friedman J, Montero F, Bourgois P, et al. Xylazine spreads across the US: a growing component of the increasingly synthetic and polysubstance overdose crisis. Drug Alcohol Depend. 2022;233:109380. doi: 10.1016/j.drugalcdep.2022.109380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Busardò FP, Pichini S, Pacifici R, Karch SB. The never-ending public health issue of adulterants in abused drugs. J Anal Toxicol. 2016;40(7):561–562. doi: 10.1093/jat/bkw051. [DOI] [PubMed] [Google Scholar]
- 18.Maryland Poison Center. 2019. https://www.mdpoison.com/media/SOP/mdpoisoncom/ToxTidbits/2019/Jan%202019%20ToxTidbits.pdf
- 19.Reyes JC, Negrón JL, Colón HM, et al. The emerging of xylazine as a new drug of abuse and its health consequences among drug users in Puerto Rico. J Urban Health. 2012;89(3):519–526. doi: 10.1007/s11524-011-9662-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodríguez N, Vidot JV, Panelli J, Colón H, Ritchie B, Yamamura Y. GC-MS confirmation of xylazine (Rompun), a veterinary sedative, in exchanged needles. Drug Alcohol Depend. 2008;96(3):290–293. doi: 10.1016/j.drugalcdep.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tobias S, Shapiro AM, Wu H, Ti L. Xylazine identified in the unregulated drug supply in British Columbia, Canada. Can J Addict. 2020;11(3):28–32. doi: 10.1097/CXA.0000000000000089. [DOI] [Google Scholar]
- 22.Never Use Alone. Meeting people where they are, on the other end of the line, one human connection at a time. Available at: https://neverusealone.com2021