Abstract
Background:
Compared with general anesthesia, spinal anesthesia has many benefits for patients undergoing total hip (THA) or total knee (TKA) arthroplasty, but few studies have explored rates of morbidity and mortality. We aimed to compare perioperative outcomes by anesthetic type for patients undergoing THA or TKA for osteoarthritis.
Methods:
We identified patients who underwent primary THA or TKA from the affiliated institute’s database. We calculated inpatient, 30-day, 60-day and 90-day mortality rates, as well as 90-day perioperative complications, readmissions and length of stay (LOS). We compared outcomes between groups using logistic regression and propensity-adjusted multivariate analysis.
Results:
We included 6100 (52.2%) patients undergoing THA and 5580 (47.8%) undergoing TKA. We found no differences by anesthetic type in mortality rates up to 90 days after surgery. Patients under spinal anesthesia were less likely to need a blood transfusion (THA odds ratio [OR] 0.75, 95% confidence interval [CI] 0.60 to 0.92; TKA OR 0.52, 95% CI 0.40 to 0.67) and were more likely to be discharged home among those who underwent TKA (OR 1.61, 95% CI 1.30 to 2.00). Patients who received spinal anesthesia for THA had a longer LOS (0.28 d, 95% CI 0.17 to 0.39), and patients who received spinal anesthesia for TKA had a shorter LOS than those who received general anesthesia (−0.34 d, 95% CI −0.51 to −0.18). Anesthetic type was not associated with any difference in adverse events.
Conclusion:
These findings may inform decisions on anesthetic type for total joint arthroplasty, especially for rapid discharge protocols. Further research is needed to understand postoperative pain and functional outcomes between anesthetic types.
Abstract
Contexte:
Comparée à l’anesthésie générale, la rachianesthésie présente de nombreux avantages pour les patients subissant une arthroplastie totale de la hanche (ATH) ou du genou (ATG), mais peu d’études se sont intéressées aux taux de morbidité et de mortalité. Nous avons cherché à comparer les résultats périopératoires par type d’anesthésie pour les patients subissant une ATH ou une ATG en raison de l’arthrose.
Méthodes:
Nous avons identifié des patients ayant subi une ATH ou une ATG primaire dans la base de données de l’institut affilié. Nous avons calculé les taux de mortalité des patients hospitalisés, à 30, 60 et 90 jours, ainsi que les complications périopératoires à 90 jours, les réadmissions et la durée de séjour. Nous avons comparé les résultats des différents groupes au moyen d’une analyse de régression logistique et d’une analyse multivariée adaptée au score de propension.
Résultats:
Notre étude comprenait 6100 (52,2 %) patients soumis à une ATH et 5580 (47,8 %) patients soumis à une ATG. Nous n’avons trouvé aucune différence dans les taux de mortalité en fonction du type d’anesthésie jusqu’à 90 jours après l’intervention. Les patients ayant subi la rachianesthésie étaient moins sujets à nécessiter une transfusion sanguine (ATH : rapport des cotes [RC] de 0,75, intervalle de confiance [IC] de 95 % 0,60 à 0,92; ATG : RC de 0,52, IC de 95 % 0,40 à 0,67) et plus sujets à obtenir leur sortie de l’hôpital parmi le groupe des ATG (RC de 1,61, IC de 95 % 1,30 à 2,00). Les patients ayant reçu la rachianesthésie pour l’ATH avaient un séjour de plus longue durée (0,28 j, IC de 95 %, 0,17 à 0,39) et les patients ayant reçu la rachianesthésie pour l’ATG avaient eu un séjour plus court que les patients ayant subi une anesthésie générale (−0,34 j, IC de 95 %, −0,51 à −0,18). Le type d’anesthésie n’était pas associé à une différence dans les événements indésirables.
Conclusion:
Ces résultats peuvent éclairer les décisions sur le type d’anesthésie à privilégier pour les arthroplasties totales, en particulier pour les protocoles de sortie rapide. D’autres recherches sont nécessaires pour comprendre la douleur postopératoire et les résultats fonctionnels propres aux différents types d’anesthésie.
The growing demand and rising costs for total joint arthroplasty (TJA) carries an important economic burden to health care systems.1 A sizeable proportion of the overall costs for TJA is attributed to patient postoperative length of stay (LOS).2 To mitigate costs, there has been a recent push toward rapid-recovery and fast-track clinical pathways that aim to shorten postoperative LOS. These endeavours have ignited a new interest in assessing if a specific type of anesthetic could shorten LOS while offering an equivalent safety profile.
Despite numerous studies suggesting benefits of spinal anesthesia over general anesthesia for patients undergoing TJA, general anesthesia is still commonly used.3 The reported advantages of spinal anesthesia include fewer blood transfusions, lower rates of thromboembolic events and fewer surgical site infections.4–14 Unfortunately, many of these studies do not report on rates of morbidity and mortality beyond 30 days after surgery, which may undermine results as some complications attributable to surgery can occur up to 90 days later.
The purpose of this study is to expand current knowledge on 30-day perioperative mortality and identify any differences in inpatient, 60-day and 90-day mortality, as well as 90-day perioperative outcomes, between patients who received spinal or general anesthesia at the time of their TJA. Our null hypothesis was that anesthesia type would not be associated with increased mortality at any time point, but that there would be fewer perioperative complications with spinal anesthesia than with general anesthesia.
Methods
Study population
We conducted a retrospective, population-based assessment using prospectively collected patient-level data, extracted from the provincial administrative data repositories that were available to the Alberta Bone and Joint Health Institute, Calgary, Alberta. The institute contains patient data from all hospitals across the province in a country with publicly funded health care. We used the Reporting of Studies Conducted Using Observational Routinely Collected Data (RECORD) guidelines in reporting this study.15
We searched the institute’s repositories to identify all patients who underwent an elective, primary, unilateral total hip arthroplasty (THA) or total knee arthroplasty (TKA) for osteoarthritis between December 2009 and December 2019, excluding those performed in the context of acute fractures, revision surgery, rheumatoid arthritis or osteonecrosis. We also excluded procedures for other secondary types of osteoarthritis such as posttraumatic or inflammatory osteoarthritis, or osteoarthritis resulting from dysplasia. This was achieved by using the Canadian Classification of Health Interventions codes 1VA53LAPN and 1VA53LLPN for THA, and 1VG53LAPN and 1VG53LAPP for TKA, and their variations. We excluded patients who received any form of anesthesia other than general or spinal, and patients who received a revision arthroplasty, bilateral joint arthroplasty, unicompartmental knee replacement or resurfacing hip arthroplasty.
We collected patient characteristics, including age, sex, body mass index, score on the American Society of Anesthesiologists (ASA) physical status classification system and baseline comorbidities. The ASA score is a validated measure of perioperative mortality and immediate postoperative morbidity.16,17 The affiliated institute’s Arthroplasty Pre-Surgery Risk Factors methodology identifies the presence of patient-related risk factors (comorbidities) by screening preadmission comorbidities in the Discharge Abstract Database and in the Canadian Institute for Health Information (CIHI) Population Grouper data within the 5 years before the arthroplasty event. Population Grouper data are extracted from provincial administrative data sources to identify the presence of 226 discrete health conditions, which are aggregated into 16 health profile categories, 10 of which were of interest for this study, namely cancer, cardiac illness, chronic hepatic conditions, chronic pulmonary conditions, chronic renal conditions, dementia, diabetes with complications, previous stroke, obesity and moderate or severe mental health disorders.
Outcomes
The primary objective of this study was to compare in-hospital, 30-day, 60-day and 90-day mortality rates between cohorts, defined as all-cause deaths that occurred after surgery. This was determined using the provincial patient registry, which captures all provincial deaths.
The secondary objectives were to compare need for blood transfusion; discharge destination; 30-, 60- and 90-day readmission rates; deep surgical site infection; acute LOS; and postoperative complications. Postoperative complications included myocardial infarction, pneumonia, gastrointestinal bleed, ileus, bleeding, delirium, acute renal failure and urinary tract infection. Discharge destination identified if a patient was discharged home with or without support services (e.g., home care assistance), or if they were discharged to an inpatient rehabilitation or a long-term care facility. We determined diagnosis of a deep surgical site infection based on the criteria outlined by the Centre for Disease Control and the National Healthcare Safety Network.18 We calculated acute LOS in days from admission to discharge from the hospital where the surgery took place.
Surgeries were performed in accordance with each surgeon’s preferred surgical approach. All patients received a dose of tranexamic acid and antibiotics as per hospital protocol. All patients were admitted postoperatively as fast-track pathways had not yet been implemented in the province.
Statistical analysis
We performed all statistical analyses using R version 4.0.2 and R Studio using the ggplot2, survival, ranger, ggfortify, survminer, dplyr, glm2 and oddsratio packages. Results were reported separately for patients who received a THA and those who received a TKA.
We summarized continuous variables as means with standard deviations and categorical variables as percentages. We used the χ2 and Fisher exact tests to test for significance in the comparison of categorical outcomes between matched cohorts. We used the Student t test to test for significance in the comparison of continuous values.
We matched patients using the propensity score technique to control for selection bias and baseline patient characteristics. We matched all patients 1-to-1 by type of anesthetic used based on age, sex, body mass index, type of joint replacement (THA or TKA), ASA physical status and baseline comorbidities. We used multiple logistic regression to compare the odds of a perioperative complication between anesthetic type for matched cohorts, adjusted for age, sex, BMI and ASA score. We used multiple linear regression to compare the acute LOS between matched cohorts, also adjusted for the aforementioned variables.
Ethics approval
This study was approved by the University of Calgary’s Conjoint Health Research Ethics Board. Given the secondary access to deidentified data, this study received a waiver of consent.
Results
After exclusions, 42 874 patients were eligible for analysis: 17 727 (41.3%) who underwent THA (n = 3050 with general anesthesia, n = 14 677 with spinal anesthesia) and 25 147 (58.6%) who underwent TKA (n = 2790 with general anesthesia, n = 22 357 with spinal anesthesia). Ninety-three surgeons were responsible for these surgeries, for an average of 461 patients per surgeon.
After excluding patients with missing data for some of the characteristics, measures or outcomes, a total of 11 680 patients were included in the study; 6100 (52.2%) patients underwent THA and 5580 (47.8%) underwent TKA. To control for selection bias between treatment groups, we calculated propensity scores for each patient on the basis of the aforementioned variables and preoperative comorbidities. The model successfully reduced selection bias by eliminating significant differences in preoperative variables. Patient demographic characteristics and preoperative comorbidities are presented in Table 1 and Table 2. We did not observe any significant differences between the THA and TKA groups after matching.
Table 1.
Characteristics of the matched cohort of patients who underwent total hip arthroplasty*
| Characteristic | No. (%) of patients† | p value‡ | |
|---|---|---|---|
| Spinal anesthesia n = 3050 |
General anesthesia n = 3050 |
||
| Sex | > 0.99 | ||
| Male | 1314 (43.1) | 1313 (43) | |
| Female | 1736 (56.9) | 1737 (57) | |
| Age, yr, mean ± SD | 63.7 ± 11.9 | 63.6 ± 12.2 | 0.75 |
| BMI, mean ± SD | 29.8 ± 5.9 | 29.8 ± 6.1 | 0.97 |
| ASA score | > 0.99 | ||
| 1 or 2 | 2235 (73.3) | 2236 (73.3) | |
| 3 or 4 | 815 (26.7) | 814 (26.7) | |
| Medical comorbidities§ | |||
| Cancer | 436 (14.3) | 446 (14.6) | 0.74 |
| Cardiac illness | 659 (21.6) | 665 (21.8) | 0.88 |
| Chronic hepatic conditions | 50 (1.6) | 51 (1.7) | > 0.99 |
| Chronic pulmonary conditions | 319 (10.5) | 324 (10.6) | 0.87 |
| Chronic renal conditions | 91 (3) | 99 (3.2) | 0.61 |
| Dementia | 26 (0.9) | 26 (0.9) | > 0.99 |
| Diabetes with complications | 364 (11.9) | 366 (12.0) | 0.97 |
| Previous stroke | 33 (1.1) | 34 (1.1) | > 0.99 |
| Obesity | 442 (14.5) | 456 (15) | 0.64 |
| Moderate or severe mental health disorders | 138 (4.5) | 138 (4.5) | > 0.99 |
ASA = American Society of Anesthesiologists, BMI = body mass index, SD = standard deviation.
14 677 records of patients with spinal anesthesia were extracted and were matched with 3050 records of patients with general anesthesia on age, sex, BMI, ASA Score and baseline comorbidities using the propensity score matching technique.
Unless indicated otherwise.
Propensity scores were used to control for selection bias between the spinal and general anesthesia groups, and propensity-adjusted p values (from χ2 test for categorical variables and Student t test for continuous variables) for preoperative patient characteristics are reported. The model successfully reduced selection bias by eliminating significant differences in preoperative variables (the adjusted p value was > 0.05 for all).
Chronic pulmonary conditions include congenital disorder of the respiratory system, chronic obstructive pulmonary disease, pulmonary hypertension, respiratory failure, cystic fibrosis, tuberculosis and other chronic lung disease. Moderate or severe mental health disorders include delusional disorder (including schizophrenia), bipolar or manic mood disorder, eating disorder, intellectual disorder or delay, and mental disorder resulting from brain injury or other illness.
Table 2.
Characteristics of the matched cohort of patients who underwent total knee arthroplasty*
| Characteristic | No. (%) of patients† | p value‡ | |
|---|---|---|---|
| Spinal anesthesia n = 2790 |
General anesthesia n = 2790 |
||
| Sex | > 0.99 | ||
| Male | 1009 (36.2) | 1009 (36.2) | |
| Female | 1781 (63.8) | 1,781 (63.8) | |
| Age, yr, mean ± SD | 66.2 ± 9.3 | 66.2 ± 9.5 | 0.84 |
| BMI, mean ± SD | 33.4 ± 6.4 | 33.3 ± 6.6 | 0.78 |
| ASA score | 0.98 | ||
| 1 or 2 | 1845 (66.1) | 1847 (66.2) | |
| 3 or 4 | 945 (33.9) | 943 (33.8) | |
| Medical comorbidities§ | |||
| Cancer | 361 (12.9) | 362 (13) | > 0.99 |
| Cardiac illness | 771 (27.6) | 779 (27.9) | 0.83 |
| Chronic hepatic conditions | 47 (1.7) | 47 (1.7) | > 0.99 |
| Chronic pulmonary conditions | 284 (10.2) | 291 (10.4) | 0.79 |
| Chronic renal conditions | 89 (3.2) | 91 (3.3) | 0.94 |
| Dementia | 30 (1.1) | 32 (1.1) | 0.90 |
| Diabetes with complications | 595 (21.3) | 605 (21.7) | > 0.99 |
| Previous stroke | 48 (1.7) | 48 (1.7) | > 0.99 |
| Obesity | 783 (28.1) | 783 (28.1) | > 0.99 |
| Moderate or severe mental health disorders | 131 (4.7) | 131 (4.7) | > 0.99 |
ASA = American Society of Anesthesiologists, BMI = body mass index, SD = standard deviation.
22 357 records of patients with spinal anesthesia were extracted and matched with 2790 records of patients with general anesthesia on age, sex, BMI, ASA Score and baseline comorbidities using the propensity score matching technique.
Unless indicated otherwise.
Propensity scores were used to control for selection bias between the spinal and general anesthesia groups, and propensity-adjusted p values (from χ2 test for categorical variables and by Student t test for continuous variables) for preoperative patient characteristics are reported. The model successfully reduced selection bias by eliminating significant differences in preoperative variables (the adjusted p value was > 0.05 for all).
Chronic pulmonary conditions include congenital disorder of the respiratory system, chronic obstructive pulmonary disease, pulmonary hypertension, respiratory failure, cystic fibrosis, tuberculosis and other chronic lung disease.
Moderate or severe mental health disorders include delusional disorder (including schizophrenia), bipolar or manic mood disorder, eating disorder, intellectual disorder or delay, and mental disorder resulting from brain injury or other illness.
Primary outcome
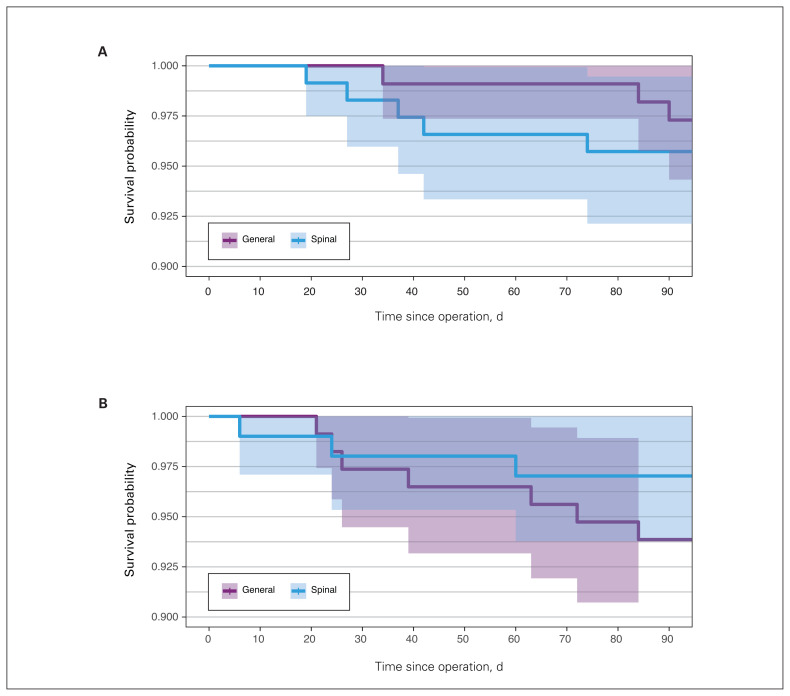
No statistically significant difference was found in the overall prevalence of inpatient, 30-day, 60-day and 90-day mortality (Table 3). For the THA cohort, anesthetic type was not associated with increased inpatient mortality (odds ratio [OR] 0.95, 95% confidence interval [CI] 0.00 to 110.59), 30-day mortality (OR 1.45, 95% CI 0.95 to 2.44), 60-day mortality (OR 1.30, 95% CI 1.12 to 1.52) or 90-day mortality (OR 1.08, 95% CI 1.05 to 1.12). Similar results were found for patients who received a TKA: inpatient mortality (OR 0.68, 95% CI 0.02 to 3.63), 30-day mortality (OR 0.92, 95% CI 0.90 to 0.95), 60-day mortality (OR 0.92, 95% CI 0.90 to 0.95) and 90-day mortality (OR 0.85, 95% CI 0.83 to 0.87). Figure 1 shows the estimates of survival probability within 90 days after surgery, grouped by anesthetic type.
Table 3.
Adjusted primary outcomes of matched cohort of patients who underwent total joint arthroplasty*
| Outcome | Total hip arthroplasty | Total knee arthroplasty | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| No. (%) of patients with spinal anesthesia n = 3050 |
No. (%) of patients with general anesthesia n = 3050 |
OR spinal v. general anesthesia (95% CI) | No. (%) of patients with spinal anesthesia n = 2790 |
No. (%) of patients with general anesthesia n = 2790 |
OR spinal v. general anesthesia (95% CI) | |
| Inpatient mortality | 0 (0.0) | 0 (0.0) | 0.95 (0.00 to 110.59) | 0 (0.0) | 1 (0.0) | 0.68 (0.02 to 3.63) |
|
| ||||||
| 30-day mortality | 2 (0.1) | 0 (0.0) | 1.45 (0.95 to 2.44) | 2 (0.1) | 4 (0.1) | 0.92 (0.90 to 0.95) |
|
| ||||||
| 60-day mortality | 4 (0.1) | 1 (0.0) | 1.30 (1.12 to 1.52) | 3 (0.1) | 5 (0.2) | 0.92 (0.90 to 0.95) |
|
| ||||||
| 90-day mortality | 5 (0.2) | 3 (0.1) | 1.08 (1.05 to 1.12) | 3 (0.1) | 7 (0.2) | 0.85 (0.83 to 0.87) |
|
| ||||||
CI = confidence interval, OR = odds ratio.
Adjusted for age, sex, body mass index, American Society of Anesthesiologists score and baseline comorbidities (including diabetes, cardiac illness, pulmonary condition, cancer, stroke, renal dysfunction, hepatic dysfunction, obesity, dementia and mental illness) using multiple logistic regression.
Fig. 1.
Estimates of survival probability within 90 days after (A) total hip arthroplasty or (B) total knee arthroplasty, grouped by anesthesia type (general or spinal). The shading represents the 95% confidence interval.
Secondary outcome
Adjusted secondary outcomes are shown in Table 4. The most notable differences were that patients who received spinal anesthesia needed fewer blood transfusions regardless of procedure performed (THA 5.5% v. 7.2%, OR 0.75, 95% CI 0.60 to 0.92; TKA 3.7% v. 6.8%, OR 0.52, 95% CI 0.40 to 0.67). For patients who underwent TKA, those who received spinal anesthesia were more likely to be discharged home rather than a rehabilitation facility (OR 1.61, 95% CI 1.30 to 2.00). We did not observe a statistical difference in the rate of readmission between patients who received spinal or general anesthesia. There was also no difference in the risk of developing a deep surgical site infection within 90 days for patients in either cohort.
Table 4.
Adjusted secondary outcomes of matched cohort of patients who underwent total joint arthroplasty*
| Measure | Total hip arthroplasty | Total knee arthroplasty | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| No. (%) of patients with spinal anesthesia n = 3050 |
No. (%) of patients with general anesthesia n = 3050 |
OR spinal v. general anesthesia (95% CI) | No. (%) of patients with spinal anesthesia n = 2790 |
No. (%) of patients with general anesthesia n = 2790 |
OR spinal v. general anesthesia (95% CI) | |
| Blood transfusion | 168 (5.5) | 220 (7.2) | 0.75 (0.60 to 0.92) | 102 (3.7) | 189 (6.8) | 0.52 (0.40 to 0.67) |
|
| ||||||
| Discharge home | 2794 (91.6) | 2777 (91.0) | 1.07 (0.88 to 1.30) | 2626 (94.1) | 2543 (91.2) | 1.61 (1.30 to 2.00) |
|
| ||||||
| 30-day readmission | 50 (1.6) | 58 (1.9) | 0.87 (0.59 to 1.28) | 64 (2.3) | 63 (2.3) | 1.03 (0.72 to 1.47) |
|
| ||||||
| 60-day readmission | 74 (2.4) | 84 (2.8) | 0.89 (0.64 to 1.22) | 94 (3.4) | 99 (3.6) | 0.96 (0.72 to 1.28) |
|
| ||||||
| 90-day readmission | 97 (3.2) | 120 (3.9) | 0.81 (0.61 to 1.06) | 130 (4.7) | 137 (4.9) | 0.95 (0.74 to 1.23) |
|
| ||||||
| Deep infection | 13 (0.4) | 10 (0.3) | 1.05 (0.99 to 1.13) | 9 (0.3) | 9 (0.3) | 1.00 (0.92 to 1.09) |
CI = confidence interval, OR = odds ratio.
Adjusted for age, sex, body mass index, American Society of Anesthesiologists score and baseline comorbidities (including diabetes, cardiac illness, pulmonary condition, cancer, stroke, renal dysfunction, hepatic dysfunction, obesity, dementia and mental illness).
Interestingly, there was an inverse impact on LOS for those who received spinal anesthesia for their THA compared with those who underwent a TKA (Table 5). Patients who received spinal anesthesia for a THA were found to have a longer LOS than those who received general anesthesia (mean difference 0.28, 95% CI 0.17 to 0.39), whereas, patients who received spinal anesthesia for a TKA were found to have a shorter LOS than those who received general anesthesia (−0.34, 95% CI −0.51 to −0.18).
Table 5.
Adjusted mean length of acute hospital stay of matched cohort of patients who underwent total joint arthroplasty*
| Cohort | Length of stay, d, mean ± SD | Mean difference (95% CI) | |
|---|---|---|---|
| Spinal anesthesia | General anesthesia | ||
| Total hip arthroplasty | 3.33 ± 2.13 | 3.05 ± 2.35 | 0.28 (0.17 to 0.39) |
| Total knee arthroplasty | 3.43 ± 2.08 | 3.78 ± 4.07 | −0.34 (−0.51 to −0.18) |
CI = confidence interval, SD = standard deviation.
Adjusted for age, gender, body mass index, American Society of Anesthesiologists score and comorbidities (including diabetes, cardiac illness, pulmonary condition, cancer, stroke, renal dysfunction, hepatic dysfunction, obesity, dementia and mental illness) using multiple linear regression.
Lastly, anesthetic type did not influence risk of postoperative complications in either cohorts (Table 6).
Table 6.
Postoperative complications of matched cohort of patients who underwent total joint arthroplasty
| Characteristic | Total hip arthroplasty | Total knee arthroplasty | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| No. (%) of patients with spinal anesthesia n = 3050 |
No. (%) of patients with general anesthesia n = 3050 |
OR spinal v. general anesthesia (95% CI) | No. (%) of patients with spinal anesthesia n = 2790 |
No. (%) of patients with general anesthesia n = 2790 |
OR spinal v. general anesthesia (95% CI) | |
| Myocardial infarction | 5 (0.16) | 3 (0.1) | 1.08 (1.07 to 1.08) | 1 (0.04) | 7 (0.25) | 0.55 (0.27 to 0.96) |
|
| ||||||
| Pneumonia | 0 (0) | 1 (0.03) | 0.65 (0.02 to 3.44) | 4 (0.14) | 7 (0.25) | 0.84 (0.74 to 0.93) |
|
| ||||||
| Gastrointestinal bleed | 3 (0.10) | 1 (0.03) | 1.59 (0.53 to 8.68) | 1 (0.04) | 2 (0.07) | 0.82 (0.04 to 8.03) |
|
| ||||||
| Ileus | 12 (0.39) | 6 (0.2) | 1.29 (1.25 to 1.34) | 9 (0.32) | 8 (0.29) | 1.07 (0.93 to 1.23) |
|
| ||||||
| Bleeding* | 16 (0.52) | 24 (0.79) | 0.89 (0.86 to 0.91) | 20 (0.72) | 22 (0.79) | 0.96 (0.90 to 1.02) |
|
| ||||||
| Delirium | 11 (0.36) | 14 (0.46) | 0.98 (0.97 to 0.98) | 14 (0.50) | 8 (0.29) | 1.10 (1.07 to 1.13) |
|
| ||||||
| Acute kidney injury | 3 (0.10) | 2 (0.07) | 1.07 (1.03 to 1.12) | 2 (0.07) | 6 (0.22) | 0.86 (0.85 to 0.87) |
CI = confidence interval, OR = odds ratio.
Bleeding, defined as any of the following codes from the International Classification of Diseases, 10th edition: D500 — anemia due to blood loss; D62 — acute anemia; D683 — hemorrhagic disorders due to anticoagulants; D69 — other hemorrhagic conditions; G361 — hemorrhagic leukoencephalitis; H113 — conjunctival hemorrhage; H356 — retinal hemorrhage; H431 — vitreous hemorrhage; H450 — vitreous hemorrhage; I60 — hemorrhage; I61 — hemorrhage; I62 — hemorrhage; J942 — hemothorax; J9500 — hemorrhage from tracheostomy stoma; K5520 —angiodysplasia; K625 — hemorrhage of anus and rectum; K661 — hemoperitoneum; M250 — haemarthrosis; R04 — hemorrhage from respiratory passages; R31 — hematuria; R58 — hemorrhage, NEC; R823 — hemoglubinuria; S064 — epidural hemorrhage;T810 — hemorrhage and hematoma, NEC.
Discussion
We sought to expand current knowledge on 30-day mortality rates and perioperative outcomes and identify differences in inpatient, 60-day and 90-day postoperative mortality rates and morbidity between patients managed with spinal or general anesthesia at the time of their arthroplasty. The current investigation used data collected from an affiliated institute, a large, independent, not-for-profit institute that prospectively collects data of patients who have undergone elective TJA. Both THA and TKA have previously been shown to be associated with short-term increase in mortality.29–31
Given the relatively low event and complication rates, specifically deaths, large sample sizes are required to achieve adequate statistical power. In addition, analyzing this research question with a large randomized controlled trial would be financially unfeasible. Therefore, one method to analyze mortality and reach adequate statistical power is by using a large observational study design. We chose a retrospective cohort study from prospectively gathered data to address our primary objective.
Our findings are consistent with those of previous studies.5,9–11,14 Perlas and colleagues5 were the first to report a strong association between anesthetic technique and 30-day mortality in arthroplasty. In their single-centre cohort study of 2135 matched pairs, they found a mortality rate of 0.19% (n = 4) for those who received spinal anesthesia and 0.8% (n = 17) for those who received general anesthesia. Since then, a large observational study has reported similar findings.30 Hunt and colleagues30 determined anesthetic type to be a modifiable clinical variable to reduce mortality (n = 0.019) in 409 096 THA procedures. However, they did not find a similar association in patients after TKA.31 These studies report cumulative rates of mortality of 0.20% and 0.29% after TKA and THA, respectively.
Three large American studies, using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, have reported increased perioperative complications in patients managed with general anesthesia at the time of surgery.4,10,11 Our findings are consistent with these studies and other smaller studies,9,14 suggesting that patients who receive spinal anesthesia for a THA require fewer blood transfusions. However, we did not observe any difference in rates of readmission or deep surgical site infection. On the other hand, patients who received spinal anesthesia for a TKA also required fewer blood transfusions, but were also found to be more likely to be discharged home. This has been supported by other studies.9,14,32 The association between transfusion risk and use of general anesthesia during THA has been described previously.32 The sympathetic blockade achieved with spinal anesthesia lowers mean arterial blood pressure and peripheral venous pressure, thus reducing the bleeding.33
The rising demand for TJA is concerning, given the growing economic burden these surgeries have on health care systems.34 In addition, these surgeries are forecasted to increase during the next 20 years.35,36 A sizeable proportion of overall cost of TJA is attributed to the postoperative LOS. To mitigate these costs, there has been a recent push toward rapid-recovery and fast-track clinical pathways. The impact of anesthetic type on hospital LOS after TJA continues to be poorly understood and a topic for debate.11,37–39 A recent randomized controlled trial looked at recovery times after TJA in patients receiving spinal or general anesthesia.39 General anesthesia resulted in slightly shorter LOS (26 h v. 30 h, p = 0.004) and better orthostatic function. During fast-track arthroplasty pathways, general anesthesia may enable faster ambulation with less dizziness, but may compromise postoperative pain control. In the present study, we found an interesting difference between patients who received spinal anesthesia for THA or for TKA. Patients in the THA cohort who received spinal anesthesia required a longer LOS than those who received general anesthesia. This likely reflects the ability of patients to ambulate sooner after surgery. However, the same is not true in the TKA cohort. Patients who received spinal anesthesia at the time of surgery were found to require a shorter LOS. Although only speculative, this may reflect the better ability of spinal anesthesia to control pain. We believe that patients have more pain after a TKA than a THA, especially without a nerve block. A spinal anesthetic may provide the necessary pain control to allow patients to be discharged earlier after a TKA. Unfortunately, our databases do not collect data on use of peripheral nerve block during TJA. Therefore, we do not know if there are any significant differences in use of peripheral blocks between group cohorts.
A strength of this study is that we asssessed morbidity and mortality with both a THA and a TKA cohort from the same database, while successfully matching patients using the propensity score technique. We were able to extend data acquisition time up to 90 days postsurgery. Some complications, such as deep vein thrombosis and pulmonary embolism must be monitored for longer, as virtually all venous thromboembolism attributable to surgery can occur up to 90 days after the procedure.
Limitations
The limitations of our study are those characteristic of the use of large administrative databases. Additional study limitations include patient care factors that were not analyzed but may differ between patients receiving general or spinal anesthesia, including narcotic use, use of peripheral nerve blocks and procedure complexity — factors that may affect anesthetic choice and perioperative outcomes. As previously stated, the decision to use general or spinal anesthesia in our study reflected the anesthesiologists’ judgment and practice rather than predetermined guidelines. Given our method of data capture, we were unable to identify patients who had a failed spinal anesthetic and converted to general anesthesia. It is unclear whether there are any effects of this conversion on reported results, as no study has addressed this. Finally, we used the ASA grade as an indicator of medical frailty for matching; however, this ultimately does not provide a complete picture of the patient’s medical status. The ASA grade has recognized limitations in terms of interobserver variability, but is a validated measure of perioperative mortality and immediate postoperative morbidity, thus lending value in creating 2 similar cohorts.18 Despite these shortcomings, the affiliated institute’s database is one of the largest institutes that prospectively collects and analyzes data for measuring outcomes against international benchmarks using carefully selected data elements and key performance indicators. This database further allowed us to report 90-day perioperative complications, which was a shortcoming of previous studies.
Conclusion
Our study shows that receiving general anesthesia during a TJA has no significant difference on mortality, but may be associated with an increased need for blood transfusion. Our results also suggest anesthetic type does not influence the risk of perioperative medical complications. However, spinal anesthesia was associated with longer LOS after THA but shorter LOS after TKA, compared with patients who received general anesthesia. Future randomized trials are necessary to further elucidate the importance of anesthetic type during TJA to optimize patient care and postoperative outcomes.
Footnotes
An abstract of this work was presented at the 2019 Canadian Orthopedic Association meeting.
Competing interest: Rajrishi Sharma reports consulting fees from Depuy Synthes, Zimmer Biomet, Stryker and OSI. No other competing interests were declared.
Contributors: David Halpenny, Saboura Mahdavi and Rajrishi Sharma conceived and designed the study. Jonathan Bourget-Murray and Sophie Piroozfar analyzed and interpreted the data. Jonathan Bourget-Murray, David Halpenny and Rajrishi Sharma drafted the manuscript. All of the authors revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This study was supported by the Departments of Anesthesiology, University of Calgary, Calgary, Alta. The funding body had no role in study design, data analysis and interpretation, or in writing the manuscript.
References
- 1.Lovett-Carter D, Sayeed Z, Abaab L, et al. Impact of outpatient total joint replacement on postoperative outcomes. Orthop Clin North Am 2018;49:35–44. [DOI] [PubMed] [Google Scholar]
- 2.Sutton JC, III, Antoniou J, Epure LM, et al. Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. J Bone Joint Surg Am 2016;98:1419–28. [DOI] [PubMed] [Google Scholar]
- 3.Memtsoudis SG, Sun X, Chiu Y-L, et al. Perioperative comparative effectiveness of anesthetic technique in orthopedic patients. Anesthesiology 2013;118:1046–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belmont PJ, Jr, Goodman GP, Waterman BR, et al. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am 2014;96:20–6. [DOI] [PubMed] [Google Scholar]
- 5.Perlas A, Chan VWS, Beattie S. Anesthesia technique and mortality after total hip or knee arthroplasty: a retrospective, propensity score–matched cohort study. Anesthesiology 2016;125:724–31. [DOI] [PubMed] [Google Scholar]
- 6.Stundner O, Chiu Y-L, Sun X, et al. Comparative perioperative outcomes associated with neuraxial versus general anesthesia for simultaneous bilateral total knee arthroplasty. Reg Anesth Pain Med 2012;37:638–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mauermann WJ, Shilling AM, Zuo Z. A comparison of neuraxial block versus general anesthesia for elective total hip replacement: a meta-analysis. Anesth Analg 2006;103:1018–25. [DOI] [PubMed] [Google Scholar]
- 8.Chang C-C, Lin H-C, Lin H-W, et al. Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study. Anesthesiology 2010;113:279–84. [DOI] [PubMed] [Google Scholar]
- 9.Park YB, Chae WS, Park SH, et al. Comparison of short-term complications of general and spinal anesthesia for primary unilateral total knee arthroplasty. Knee Surg Relat Res 2017; 29:96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pugely AJ, Martin CT, Gao Y, et al. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am 2013; 95:193–9. [DOI] [PubMed] [Google Scholar]
- 11.Basques BA, Toy JO, Bohl DD, et al. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am 2015;97:455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis FM, Laurenson VG, Gillespie WJ, et al. Deep vein thrombosis after total hip replacement. A comparison between spinal and general anaesthesia. J Bone Joint Surg Br 1989;71:181–5. [DOI] [PubMed] [Google Scholar]
- 13.Rashiq S, Finegan BA. The effect of spinal anesthesia on blood transfusion rate in total joint arthroplasty. Can J Surg 2006; 49:391–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Maurer SG, Chen AL, Hiebert R, et al. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop 2007;36:E101–6. [PubMed] [Google Scholar]
- 15.Benchimol EI, Smeeth L, Guttmann A, et al. RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA 1961;178:261–6. [DOI] [PubMed] [Google Scholar]
- 17.Sankar A, Johnson SR, Beattie WS, et al. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth 2014;113:424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Healthcare Safety Network. CDC/NHSN surveillance definitions for specific types of infections. Atlanta: Centers for Disease Control and Prevention; 2022. Available: https://www.cdc.gov/nhsn/PDFs/pscManual/17pscNosInfDef_current.pdf (accessed 2020 May 7). [Google Scholar]
- 29.Parry MC, Smith AJ, Blom AW. Early death following primary total knee arthroplasty. J Bone Joint Surg Am 2011;93:948–53. [DOI] [PubMed] [Google Scholar]
- 30.Hunt LP, Ben-Shlomo Y, Clark EM, et al. National Joint Registry for England, Wales and Northern Ireland. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 2013;382:1097–104. [DOI] [PubMed] [Google Scholar]
- 31.Hunt LP, Ben-Shlomo Y, Clark EM, et al. National Joint Registry for England and Wales. 45-day mortality after 467,779 knee replacements for osteoarthritis from the National Joint Registry for England and Wales: an observational study. Lancet 2014;384:1429–36. [DOI] [PubMed] [Google Scholar]
- 32.Rashiq S, Finegan BA. The effect of spinal anesthesia on blood transfusion rate in total joint arthroplasty. Can J Surg 2006;49:391–6. [PMC free article] [PubMed] [Google Scholar]
- 33.Modig J, Karlström G. Intra- and post-operative blood loss and haemodynamics in total hip replacement when performed under lumbar epidural versus general anaesthesia. Eur J Anaesthesiol 1987;4:345–55. [PubMed] [Google Scholar]
- 34.Mesko NW, Bachmann KR, Kovacevic D, et al. Thirty-day readmission following total hip and knee arthroplasty: a preliminary single institution predictive model. J Arthroplasty 2014;29:1532–8. [DOI] [PubMed] [Google Scholar]
- 35.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780–5. [DOI] [PubMed] [Google Scholar]
- 36.Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 2005;87:1487–97. [DOI] [PubMed] [Google Scholar]
- 37.Bozic KJ, Beringer D. Economic considerations in minimally invasive total joint arthroplasty. Clin Orthop Relat Res 2007;(463):20–5. [DOI] [PubMed] [Google Scholar]
- 38.Johnson RL, Kopp SL, Burkle CM, et al. Neuraxial vs general anaesthesia for total hip and total knee arthroplasty: a systematic review of comparative effectiveness research. Br J Anaesth 2016;116:163–76. [DOI] [PubMed] [Google Scholar]
- 39.Harsten A, Kehlet H, Toksvig-Larsen S. Recovery after total intravenous general anaesthesia or spinal anaesthesia for total knee arthroplasty: a randomized trial. Br J Anaesth 2013;111:391–9. [DOI] [PubMed] [Google Scholar]