Abstract
Background:
The COVID-19 pandemic has highlighted the role of personal support workers (PSWs) in health care, as well as their work conditions. Our study aimed to understand the characteristics of the PSW workforce, their work conditions and their job security, as well as to explore the health of PSWs and the impact of precarious employment on their health.
Methods:
Our community-based participatory action research focused on PSWs in the Greater Toronto Area. We administered an online, cross-sectional survey between June and December 2020 using respondent-driven sampling. Data on sociodemographics, employment precarity, worker empowerment and health status were collected. We assessed the association between precarious employment and health using multivariable logistic regression models.
Results:
We contacted 739 PSWs, and 664 consented to participate. Overall, 658 (99.1%) completed at least part of the survey. Using data adjusted for our sampling approach, the participants were predominantly Black (76.5%, 95% confidence interval [CI] 68.2%–84.9%), women (90.1%, 95% CI 85.1%–95.1%) and born outside of Canada (97.4%, 95% CI 94.9%–99.9%). Most worked in home care (43.9%, 95% CI 35.2%–52.5%) or long-term care (34.5%, 95% CI 27.4%–42.0%). Although most participants had at least some postsecondary education (unadjusted proportion = 83.4%, n = 529), more than half were considered low income (55.1%, 95% CI 46.3%–63.9%). Most participants were precariously employed (86.5%, 95% CI 80.7%–92.4%) and lacked paid sick days (89.5%, 95% CI 85.8%–93.3%) or extended health benefits (74.1%, 95% CI 66.8%–81.4%). Nearly half of the participants described their health as less than very good (46.7%, 95% CI 37.9%–55.5%). Employment precarity was significantly associated with higher risk of depression (odds ratio 1.02, 95% CI 1.01–1.03).
Interpretation:
Despite being key members of health care teams, most PSWs were precariously employed with low wages that keep them in poverty; the poor work conditions they faced could be detrimental to their physical and mental health. Equitable strategies are needed to provide decent work conditions for PSWs and to improve their health.
Jobs in health care have traditionally been secure.1 Over the past 30 years, however, disparities in pay and work conditions have grown between registered professionals (e.g., physicians, nurses) and other staff in health care whose jobs are part-time, temporary, on contract and not unionized (e.g., housekeeping, clerical, security). One particularly disadvantaged group are personal support workers (PSWs), also called health care aides, patient care assistants, home support workers or home care attendants.2,3 Personal support workers help older individuals and people with disabilities with their activities of daily living in their own home or in institutions. 4 Aging populations in Canada and a move to discharge people quickly from acute care to the community have driven up the demand for PSWs, who now represent about 10% of all health workers.5–8
Despite their important role within health care systems in Canada, PSWs continue to face the risk of precarious employment, which is associated with adverse health and psychosocial conditions.6 In Ontario, PSWs are not formally regulated by statutory bodies.6 They work for both public and private employers, typically as casual, nonpermanent employees.9 According to a 2020 staffing study by the Ministry of Long-Term Care, the average wage of PSWs ranged from $17.30/hr in home and community care to $25.01/hr in municipally owned long-term care facilities.10 Those working in home care typically received lower pay than those working in long-term care or in hospitals.11 The absence of a central PSW registry in Ontario, combined with the geographically dispersed nature of PSW work locations, makes PSWs difficult to reach for research.6 The limited evidence points to low rates of unionization and relatively higher safety risks compared with other health care professionals.3,12,13
Given the growing concerns around precarious employment among PSWs, the study team initiated EMPOWER (Employment and Precarious Work in Toronto’s Health Sector: Evaluation and Research Project), with the overarching purpose of improving the work conditions for PSWs. The planning of this initiative coincided with the COVID-19 pandemic, which further highlighted the crucial role of PSWs in health systems as they cared for older adults in congregate settings, where the worst outbreaks and highest number of deaths occurred. Although data are limited, among health workers, PSWs were some of the most likely to be infected and die from COVID-19.14,15
As part of EMPOWER, this study aimed at generating evidence on the PSW workforce, centring around 2 objectives. First, we sought to create a sociodemographic profile of the PSW workforce, their work conditions and job security, focusing on key aspects of PSW employment conditions that could be improved through policy change. Our second objective was to explore the perceived health of PSWs, particularly in relation to their work and the impact of precarious work on their health outcomes. We hypothesized that higher levels of job precarity would be associated with worse health.
Methods
Study design and setting
We conducted this cross-sectional survey study from June 2020 to December 2020, and engaged PSWs working in the Greater Toronto Area (GTA), the largest metropolitan area in Canada, with a combined population of 5.9 million.16 No estimates exist of the total number of PSWs in the GTA or its municipalities, but it is estimated that 90 000–100 000 PSWs work in the province of Ontario (population 14.5 million).4,17
We followed the principles of community-based participatory action research by engaging PSW partners in all aspects of the project and employing a shared decision-making model throughout planning processes.18 We formed an advisory committee consisting of 8 PSWs who met regularly from March 2020 to May 2021. Advisors shared their experiences to inform the study design, survey development, pilot testing, recruitment strategy and interpretation of the data. Advisors also presented preliminary results to community organizations. Concurrently, advisors received training on their employment rights, research methods and advocacy engagement. A modest honorarium was provided to compensate advisors for their time.
Reporting of our findings was guided by the Strengthening the Reporting of Observational Studies in Epidemiology for Respondent-Driven Sampling Studies (STROBE-RDS) and the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) reporting guidelines.19,20
Participants and recruitment
Participants were 18 years of age or older and had worked as a PSW in the Toronto area within the previous year. Given the lack of standardized educational requirements for PSWs, the participants were able to self-identify as a PSW during recruitment, and research staff asked about their work setting as a proxy to verify their PSW status. We included participants who were unemployed at the time of the survey to reduce selection bias, as PSWs are frequently between jobs, given employment precarity, job stress or injuries.
We used respondent-driven sampling (RDS), a network-based sampling method that begins with a small convenience sample (known as “seeds”) and that incentivizes respondents to participate in the survey and refer their peers.21 Similar to snowball sampling, this design allows for data collection from hard-to-reach populations, such as PSWs who have no regulatory body or central registry, and who often have multiple workplaces and limited availability given work and family obligations. The advantage of RDS is its ability to produce asymptotically unbiased estimates of population parameters by accounting for the respondent’s network size and their recruitment pattern.21
We identified seeds that would reflect the diversity of the PSW population in Toronto in terms of gender, age, race and work setting (Appendix 1, Section 1, available at www.cmajopen.ca/content/10/2/E527/suppl/DC1). Seeds were recruited through recommendations from the advisory committee, through emails distributed by partner organizations and through online advertisements on social media and job search platforms (Appendix 1, Section 2). Initially, we selected 10 seeds, and added another 16 seeds later to increase recruitment. Two seeds did not initiate the survey and were subsequently removed from further analysis. There was no explicit time limit for recruitment, but we informed participants that data collection would be completed by December 2020.
Data sources and collection
We collected data on sociodemographic characteristics, employment precarity, worker empowerment and health status using an online survey (Appendix 1, Section 3). Where available, we selected instruments that had been validated or administered to populations in Canada to allow for comparison with existing evidence. The survey was developed in an iterative manner, whereby the advisory members tested different survey versions and provided input on the relevance of questions to current issues, clarity of the questions and the general user experience of the online survey. The survey was composed of 75 questions and took about 20 minutes to complete.
The survey used participants’ full name, phone number and email address to prevent an individual from participating more than once. Participants received a Can$20 honorarium for completing the survey and were asked to recruit up to 3 peers for an additional honorarium of Can$10 per successful referral. To track the recruitment chains, PSWs interested in participating in the survey had to provide the full names of their referees. We also assigned unique identification numbers to the eligible participants, which were linked to the relevant participant information in a master log that was stored in a secured and private network (managed by St. Michael’s Hospital) and was accessible only to authorized research team members.
Public health restrictions prevented in-person meetings during the COVID-19 pandemic, and all communications with participants, including obtainment of consent, occurred through phone or email. The consent form contained information on the investigators, project funder, study background and purpose, anticipated time to complete the survey, reimbursement, confidentiality and privacy, potential harms and benefits, ethics approval and study contact. Most participants were able to complete the survey independently through an online survey software (Qualtrics), accessible via a unique link assigned to each participant. To avoid duplicate entries from the same participant, the survey link became inaccessible once the survey was completed. A small number of participants without reliable access to the Internet had the survey administered over the phone.
Variables
Sociodemographic data included age, gender identity, racial background, birth location, level of education, current student status and housing status. Low-income status was inferred using the 2018 Canadian low-income cut-off for urban areas, which considers household size.22 We also collected information about financial assistance received from government sources and included 5 items from the Income Stress Index.23,24 Specifically, these items address how participants’ employment insecurity affects large spending decisions, how they keep up with bills and debts, their concerns about maintaining their current standard of living and if they recently experienced income reductions.23,24
We evaluated precarious employment using the Employment Precarity Index, which contains 12 questions around employment types (e.g., casual, part-time or full-time), income and job stability, work schedule, paid sick days, benefits and fear of reprisal for raising labour concerns with an employer.25 We assessed worker empowerment with a 5-item subscale from the Occupational Health and Safety Vulnerability Measure.26 Additional questions on labour experience included current employment status, membership in a union, workplace discrimination, work-related injuries and whether they reported the injuries to the Workplace Safety and Insurance Board (WSIB), a government-mandated, employer-funded insurance system that provides compensation to workers for work-related injury or illness.
Health-related variables included risk of depression (specifically depressed mood and anhedonia), measured by the Patient Health Questionnaire-2 (PHQ-2),27 and perception of general health (categorized into “poor–good” and “very good–excellent”) and life satisfaction (categorized into “satisfied” and “dissatisfied”) from the Canadian Community Health Survey. 28 Other health-related questions asked about the amount of stress in participants’ lives and at work, as well as the perceived impact of their employment on their mental health.
Sample size
We initially estimated a target sample size of 474 participants, based on an RDS design effect of 1.5. We selected this design effect by projecting that the proportion of participants reporting poor general health would be 50%, with a 95% confidence interval (CI) ranging from 45% to 55%. Since the typical design effect used in RDS is 2, we increased the target sample size to 600 participants in anticipation of variance inflation arising from the nonrandom sample, while still maintaining feasibility.29,30 Larger deviation of the RDS variance from the simple random sample variance would be reflected in a larger 95% CI than initially expected.
Statistical analysis
Item-specific missing data for each variable was less than 8%, and we used available case analysis. We calculated proportion estimates with a 95% CI for all variables using the RDS package (version 0.9.2) in R statistical software (version 4.0.2) with RDS-II estimators. These estimators assigned a weight to each participant based on their sampling probability, as estimated using reported network size, thus requiring connectedness among the population of interest. Individuals who were more connected to other PSWs received a lower weight than those who were less connected. The survey measured the network size of each participant by asking “How many friends do you know who work as a PSW in the Greater Toronto Area, whom you have communicated with regularly in the past year (in-person/online/by texts)?” Through consultation with the advisory committee, we estimated an average network size of 15 to 25 PSW peers in the Toronto area. We conducted posthoc sensitivity analyses to assess the stability of the point estimates when recruits from 2 seeds with the largest recruitment waves were removed.
Number of years as a PSW, number of paid sick days, number of paid hours per week and number of missed workdays because of work-related sickness or injury were the only continuous variables collected in the survey. Except for the number of years as a PSW, we categorized the continuous variables to facilitate RDS point and interval estimations. Number of paid hours per week was categorized into full-time (≥ 30 h) or part-time hours (< 30 h). Number of missed workdays and paid sick days were categorized based on the same 5-day interval, corresponding to half of the 10 days proposed by the advisory members and experts as the adequate amount of paid sick days for PSWs.31
We assessed the association between work precarity level and health outcomes using multivariable logistic regression models. Perceived general health and risk of depression (as measured by PHQ-2) served as the main outcome variables in the first and second models, respectively. We controlled for age, gender, education level, low-income status and work setting in both models. Listwise deletion was implemented to address missing values in each model, yielding a total sample size of 585 and 568 participants for the first and second models, respectively. We made a posthoc decision to revert the precarity index back into a numerical variable (range 0–100), as most participants were found to be precariously employed. Odds ratios greater than 1 were interpreted as poorer reported general health (model 1) or higher risk of depression (model 2). We chose unweighted models to minimize risk of bias and type I error, which have been shown to occur in RDS-weighted regression models.32
Ethics approval
This study was reviewed and approved by the St. Michael’s Hospital Research Ethics Board (no. 18-103), Toronto.
Results
Of the 739 participants who were sent a consent form and a survey link, 664 participants opened the survey links, resulting in an 89.9% recruitment rate. Among those recruited, 658 participants submitted the survey and had their responses recorded, which amounts to a 99.1% completion rate. A total of 634 participants were included in the RDS analysis after removing the seeds (n = 24). The RDS recruitment network and waves propagating from each seed are presented in Appendix 1, Section 4.
Participant demographic characteristics are described in Table 1. The survey respondents were predominantly racialized (n = 572, 90.2%), women (90.1%, 95% CI 85.1%–95.1%) and born outside of Canada (97.4%, 95% CI 94.9%–99.9%). Most participants identified as Black (76.5%, 95% CI 68.2%–84.9%) and were between the ages of 30 and 49 years old. The participants were highly educated (47.4% had at least a college degree, 95% CI 39.0%–55.9%), but more than half belonged to a low-income household (55.1%, 95% CI 46.3%–63.9%) and only 10.7% were homeowners (95% CI 4.8%–16.5%).
Table 1:
Characteristics of survey participants
| Characteristic | Unweighted no. of participants n = 634 |
Unadjusted estimate, % | RDS-II adjusted estimate,* % (95% CI)† |
|---|---|---|---|
| Racial and ethnic background | |||
| Black | 425 | 67.0 | 76.5 (68.2–84.9) |
| East Asian | 32 | 5.0 | 3.7 (1.4–5.9) |
| South Asian | 19 | 3.0 | 1.9 (0.1–3.0) |
| Southeast Asian | 70 | 11.0 | 10.5 (5.6–15.4) |
| White | 16 | 2.5 | 3.7 (0.0–9.0) |
| Mixed or other racial categories | 26 | 4.1 | 3.7 (0.0–9.3) |
| Missing | 46 | 7.3 | |
| Gender identity | |||
| Female | 528 | 83.3 | 90.1 (85.1–95.1) |
| Male | 57 | 9.0 | 9.6 (4.6–14.5) |
| Other | 3 | 0.5 | 0.3 (0.0–0.8) |
| Missing | 46 | 7.3 | |
| Born in Canada | |||
| No | 576 | 90.9 | 97.4 (94.9–99.9) |
| Yes | 11 | 1.7 | 2.6 (0.1–5.1) |
| Missing | 47 | 7.4 | |
| Age category, yr | |||
| 18–29 | 52 | 8.2 | 10.4 (4.7–16.1) |
| 30–39 | 174 | 27.4 | 32.1 (23.8–40.3) |
| 40–49 | 247 | 39.0 | 38.3 (30.6–46.1) |
| ≥ 50 | 115 | 18.1 | 19.2 (10.6–27.7) |
| Missing | 46 | 7.3 | |
| Educational attainment | |||
| Some grade school | 7 | 1.1 | 1.6 (0.0–7.2) |
| Some high school | 6 | 0.9 | 1.0 (0.0–2.7) |
| High school degree | 45 | 7.1 | 8.7 (4.4–13.1) |
| Some college or university | 241 | 38.0 | 41.2 (32.3–50.0) |
| College degree, university degree or postgraduate degree | 288 | 45.4 | 47.4 (39.0–55.9) |
| Missing | 47 | 7.4 | |
| Current student status | |||
| Not a student | 512 | 80.8 | 78.9 (72.4–85.5) |
| Student | 113 | 17.8 | 21.1 (14.5–27.6) |
| Missing | 9 | 1.4 | |
| Income level | |||
| Income below LICO | 328 | 51.7 | 55.1 (46.3–63.9) |
| Income above LICO | 259 | 40.9 | 44.9 (36.1–53.7) |
| Missing | 47 | 7.4 | |
| Housing status | |||
| Living in a temporary shelter run by an agency | 3 | 0.5 | 0.4 (0.0–1.3) |
| Living in an institution (e.g., group home, long-term care, correctional facility) | 1 | 0.2 | 0.1 (0.0–0.2) |
| Living in own home | 70 | 11.0 | 10.7 (4.8–16.5) |
| Renting a home | 487 | 76.8 | 82.1 (73.8–90.4) |
| Staying with friends or family | 27 | 4.3 | 6.7 (0.0–13.5) |
| Missing | 46 | 7.3 | |
| Main setting worked as PSW in the previous year | |||
| Home care in the community | 258 | 40.7 | 43.9 (35.2–52.5) |
| Long-term care | 211 | 33.3 | 34.5 (27.0–42.0) |
| Other (e.g., hospitals, shelters, group homes, rehabilitation centres) | 126 | 19.9 | 21.6 (12.2–31.1) |
| Missing | 39 | 6.2 | |
| Current employment status | |||
| Employed | 569 | 89.8 | 89.0 (82.7–95.3) |
| Unemployed | 57 | 9.0 | 11.0 (4.7–17.3) |
| Missing | 8 | 1.3 | |
| Currently working as PSW | |||
| Not working as PSW | 25 | 3.9 | 5.3 (0.0–10.9) |
| Working as PSW | 599 | 94.5 | 94.7 (89.1–100.0) |
| Missing | 10 | 1.6 | |
Note: CI = confidence interval, LICO = low-income cut-off, PSW = personal support worker, RDS = respondent-driven sampling.
Missing data were not included in the distribution of percent estimates.
Negative CI values were truncated at 0.
In terms of work experience, participants had worked as a PSW for an average of 4.4 (standard deviation 4.9) years. They worked in various settings, with most working in home care in the community (43.9%, 95% CI 35.2%–52.5%) or long-term care (34.5%, 95% CI 27.0%–42.0%). At the time of the survey, 11.0% (95% CI 4.7%–17.3%) were unemployed and 5.3% (95% CI 0.0%–10.9%) were not working as a PSW. These demographic characteristics are also presented elsewhere.33
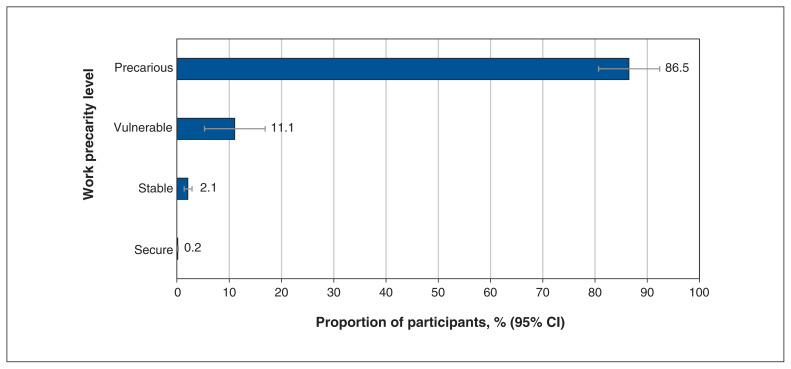
Overall, 86.5% (95% CI 80.7%–92.4%) of the participants were precariously employed (Figure 1). For example, 49.3% (95% CI 40.9%–57.8%) mainly worked part-time hours and 65.3% (95% CI 57.4%–73.1%) were in nonpermanent contract positions (Table 2). More than half also reported absence of union membership (53.8%, 95% CI 45.7%–61.9%) and lack of benefits from employers, such as paid sick days (89.5%, 95% CI 85.8%–93.3%), retirement plans (67.2%, 95% CI 59.5%–74.8%) and extended health benefits (74.1%, 95% CI 66.8%–81.4%). Other indicators of precarious employment included irregular scheduling (68.1%, 95% CI 60.2%–75.9%) and risk of reprisal for raising a health and safety concern (43.5%, 95% CI 34.8%–52.1%).
Figure 1:
Work precarity level based on the Employment Precarity Index. Note: CI = confidence interval.
Table 2:
Work conditions of survey participants
| Characteristic | Unweighted no. of participants n = 634 |
Unadjusted estimate, % | RDS-II adjusted estimate,* % (95% CI)† |
|---|---|---|---|
| Average no. of paid work hours per week in the previous year | |||
| < 30 | 282 | 44.5 | 49.3 (40.9–57.8) |
| ≥ 30 | 318 | 50.2 | 50.7 (42.2–59.1) |
| Missing | 34 | 5.4 | |
| Main employment type in the previous year‡ | |||
| Casual or on contract (part-time or full-time) or self-employed | 399 | 62.9 | 65.3 (57.4–73.1) |
| Permanent part-time or full-time | 225 | 35.5 | 34.7 (26.9–42.6) |
| Missing | 10 | 1.6 | |
| Union membership | |||
| No | 314 | 49.5 | 53.8 (45.7–61.9) |
| Yes | 310 | 48.9 | 46.2 (38.1–54.3) |
| Missing | 10 | 1.6 | |
| Paid sick days‡ | |||
| No | 547 | 86.3 | 89.5 (85.8–93.3) |
| Yes | 76 | 12.0 | 10.5 (6.7–14.2) |
| Missing | 11 | 1.7 | |
| No. of paid sick days received (among those with paid sick days, n = 76) | |||
| 0–5 | 14 | 18.4 | 18.9 (0.0–40.2) |
| 6–10 | 31 | 40.8 | 35.2 (14.5–56.0) |
| ≥ 10 | 28 | 36.8 | 45.8 (23.2–68.5) |
| Missing | 3 | 4.0 | |
| Retirement income plan from employer‡ | |||
| No | 386 | 60.9 | 67.2 (59.5–74.8) |
| Yes | 226 | 35.7 | 32.8 (25.2–40.5) |
| Missing | 22 | 3.5 | |
| Other employment benefits from employer (e.g., dental, medications)‡ | |||
| No | 438 | 69.1 | 74.1 (66.8–81.4) |
| Yes | 176 | 27.8 | 25.9 (18.6–33.2) |
| Missing | 20 | 3.2 | |
| Financial assistance received from government§ | |||
| Housing | 73 | 11.5 | 13.5 (6.6–20.5) |
| Child care | 155 | 24.5 | 26.2 (18.7–33.7) |
| Recreation | 27 | 4.3 | 4.7 (1.5–8) |
| Food allowances | 54 | 8.5 | 7.9 (5.1–10.7) |
| Dental | 71 | 11.2 | 10.7 (5.1–16.2) |
| Vision | 39 | 6.2 | 5.2 (3.0–7.4) |
| Prescription drugs | 77 | 12.2 | 11.4 (7.6–15.2) |
| Assistive living devices | 5 | 0.8 | 0.9 (0.0–2) |
| Transit passes | 28 | 4.4 | 4.8 (2.0–7.6) |
| Student grants | 26 | 4.1 | 5.6 (2.4–8.8) |
| Electricity grants | 69 | 10.9 | 11.5 (7.2–15.7) |
| Disability supports | 10 | 1.6 | 2.8 (0.6–5.1) |
| Other | 23 | 3.6 | 2.8 (1.4–4.2) |
| Frequency of knowing work schedule 1 week in advance‡ | |||
| Half the time, some of the time or never | 194 | 30.6 | 31.9 (24.1–39.8) |
| All the time or most of the time | 413 | 65.1 | 68.1 (60.2–75.9) |
| Missing | 27 | 4.3 | |
| Perceived likelihood of reprisal for raising health and safety or employment rights concern to employer‡ | |||
| Not likely or not likely at all | 353 | 55.7 | 56.5 (47.9–65.2) |
| Somewhat likely, likely or very likely | 261 | 41.2 | 43.5 (34.8–52.1) |
| Missing | 20 | 3.2 | |
| Work-related injuries or sickness in the previous year | |||
| No | 430 | 67.8 | 74.5 (68.3–80.7) |
| Yes | 177 | 27.9 | 25.5 (19.3–31.7) |
| Missing | 27 | 4.3 | |
| No. of working days missed (among those with work-related injuries or sickness, n = 177) | |||
| 0–5 | 79 | 44.6 | 46.2 (31.0–61.4) |
| 6–10 | 28 | 15.8 | 16.3 (7.8–24.8) |
| ≥ 10 | 50 | 28.3 | 37.5 (22.7–52.3) |
| Missing | 20 | 11.3 | |
| WSIB claim filed (among those with work-related injuries or sickness, n = 177) | |||
| No | 136 | 76.8 | 81.2 (73.6–88.8) |
| Yes | 41 | 23.2 | 18.8 (11.2–26.4) |
| Worker’s empowerment to participate in injury and illness prevention | |||
| Empowered | 89 | 14.0 | 12.1 (6.0–18.2) |
| Not empowered | 545 | 86.0 | 87.9 (81.8–94.0) |
| Experience with discrimination based on given variable§ | |||
| Race or ethnicity | 137 | 21.6 | 21.4 (16.3–26.5) |
| Gender | 11 | 1.7 | 1.8 (0–3.6) |
| Age | 24 | 3.8 | 4 (2–6.1) |
| Sexual orientation | 2 | 0.3 | 0.6 (0–1.5) |
| Disability | 5 | 0.8 | 0.7 (0–1.6) |
| Immigration status | 63 | 9.9 | 9.9 (4.0–15.7) |
| Other | 50 | 7.9 | 8.2 (3.8–12.5) |
Note: CI = confidence interval, RDS = respondent-driven sampling, WSIB = Workplace Safety and Insurance Board.
Missing data were not included in the distribution of percent estimates.
Negative CI values were truncated at 0.
Measure from the Employment Precarity Index.
Participants were able to select multiple options. Therefore, each category of assistance or discrimination elicited a binary response (i.e., received a particular assistance or not; discriminated against for a particular reason or not) and the sum of positive responses across the different categories exceeded the total number of participants (n = 634).
About a quarter of the participants reported work-related sickness or injury (25.5%, 95% CI 19.3%–31.7%), which resulted in loss of work hours (i.e., 78 participants or 44.1% missed more than 5 work days). Among those who were sick or injured (n = 177), about one-fifth (18.8%, 95% CI 11.2%–26.4%) filed a claim to the WSIB. Furthermore, 87.9% (95% CI 81.8%–94.0%) felt unempowered to participate in safety and injury prevention, and 35.4% (95% CI 27.8%–43.0%) experienced some form of discrimination, mainly perceived to be based on their race or ethnicity (21.4%, 95% CI 16.3%–26.5%) (Table 2).
Most participants reported that their employment situation negatively affected their large spending decisions (80.8%, 95% CI 74.3%–87.2%) and made them concerned about their ability to meet their debt obligations (73.9%, 95% CI 67.7%–80.0%) and to maintain their current standard of living (67.1%, 95% CI 60.0%–74.2%). Some also reported a decrease in their personal income compared with the previous year (40.7%, 95% CI 31.8%–49.5%), which left 14.1% (95% CI 6.2%–21.9%) of the participants struggling to keep up with their current bills and other financial commitments.
Table 3 presents the health outcomes of the participants. About half (53.3%, 95% CI 44.5%–62.1%) described their general health as very good or excellent, and more than a quarter (28.2%, 95% CI 20.7%–35.8%) expressed dissatisfaction with their lives. Some participants found most days to be stressful (26.8%, 95% CI 19.1%–34.6%) and had a weak sense of belonging to the community (28.0%, 95% CI 19.0%–34.6%). When assessed with the PHQ-2 scale (Appendix 1, Section 3), 21.0% of participants (95% CI 14.0%–28.0%) were likely to have some form of depressive disorder. Work was also found to negatively affect the mental health of the participants (16.8%, 95% CI 8.9%–24.8%) and their relationships with their family and friends (28.8%, 95% CI 20.7%–36.8%). For example, some participants were often angered by their work (10.1%, 95% CI 4.0%–16.3%) or found their work stressful (32.7%, 95% CI 24.1%–41.3%).
Table 3:
Health outcomes of survey participants
| Characteristic | Unweighted no. of participants n = 634 |
Unadjusted estimate, % | RDS-II adjusted estimate,* % (95% CI) |
|---|---|---|---|
| Perceived general health | |||
| Poor, fair or good | 278 | 43.9 | 46.7 (37.9–55.5) |
| Very good or excellent | 323 | 51.0 | 53.3 (44.5–62.1) |
| Missing | 33 | 5.2 | |
| Life satisfaction | |||
| Dissatisfied | 168 | 26.5 | 28.2 (20.7–35.8) |
| Satisfied | 433 | 68.3 | 71.8 (64.2–79.3) |
| Missing | 33 | 5.2 | |
| Amount of stress in most days | |||
| Not at all stressful, not very stressful or a bit stressful | 434 | 68.5 | 73.2 (65.4–80.9) |
| Quite a bit stressful or extremely stressful | 166 | 26.2 | 26.8 (19.1–34.6) |
| Missing | 34 | 5.4 | |
| Sense of belonging in the community | |||
| Somewhat strong or strong | 452 | 71.3 | 72.0 (63.0–81.0) |
| Somewhat weak or very weak | 146 | 23.0 | 28.0 (19.0–37.0) |
| Missing | 36 | 5.7 | |
| Risk for depression (PHQ-2 scale) | |||
| Likely | 136 | 21.5 | 21.0 (14.0–28.0) |
| Unlikely | 456 | 71.9 | 79.0 (72.0–86.0) |
| Missing | 42 | 6.6 | |
| Frequency of work negatively affecting mental health | |||
| Always or usually | 98 | 15.5 | 16.8 (8.9–24.8) |
| Occasionally, rarely or never | 503 | 79.3 | 83.2 (75.2–91.1) |
| Missing | 33 | 5.2 | |
| Perceived impact of work on relationships | |||
| Always or usually | 193 | 30.4 | 28.8 (20.7–36.8) |
| Occasionally, rarely or never | 406 | 64.0 | 71.2 (63.2–79.3) |
| Missing | 35 | 5.5 | |
| Frequency of getting angry, owing to work | |||
| Always or usually | 59 | 9.3 | 10.1 (4.0–16.3) |
| Occasionally, rarely or never | 543 | 85.7 | 89.9 (83.7–96.0) |
| Missing | 32 | 5.1 | |
| Amount of stress at work | |||
| Not at all stressful, not very stressful or a bit stressful | 402 | 63.4 | 67.3 (58.7–75.9) |
| Quite a bit stressful or extremely stressful | 200 | 31.6 | 32.7 (24.1–41.3) |
| Missing | 32 | 5.1 | |
Note: CI = confidence interval, PHQ-2 = Patient Health Questionnaire-2, RDS = respondent-driven sampling.
Missing data were not included in the distribution of percent estimates.
Using regression models, we found that increased work precarity was significantly associated with higher risk of depression, but not associated with perceived general health. Specifically, for every unit increase in the precarity score, the odds of exhibiting risk for depression increased by 2% (odds ratio [OR] 1.02, 95% CI 1.01–1.03). Older PSWs (i.e., aged ≥ 50 yr) were also more likely to report poor general health (OR 2.78, 95% CI 1.41–5.60) compared with those aged 18–29 years. Finally, posthoc sensitivity analysis showed that the proportion estimates for reported general health were reasonably stable after we removed the recruits from the 2 seeds with the largest recruitment sizes (Appendix 1, Section 5).
Interpretation
In this study, we investigated the work conditions and health of PSWs in the GTA using RDS to engage this hard-to-reach population. We found substantial evidence of precarious and dangerous work conditions. Compared with the general population in Ontario (28.5%),23 86.5% of PSWs reported being precariously employed, as highlighted by high frequency of casualized and nonpermanent employment, widespread lack of benefits and paid sick days, and socioeconomic vulnerability, including low income.
Our findings fit with existing evidence that points to the growing disparity in working conditions within the health care sector, where PSWs typically have the lowest pay and greatest employment precarity.5,6,11,34–36 Personal support workers also tend to be female and racialized, and are more likely to be immigrants.37 Similar to the findings of Neysmith and colleagues,38 we found high levels of racial discrimination in the workplace and a lack of formal supports to address workplace safety and security concerns, such as labour unions.
Given recent calls for deinstitutionalizing care or providing more care in the home and community,39 the shift toward relying on low-wage earners with unstable work is a troubling trend.40 Future research should explore potential policy solutions, such as mandating a minimum number of paid sick days, raising wages to reduce poverty, providing incentives to employers to provide more full-time positions, enforcing existing labour laws that protect PSWs from reprisals if they raise concerns about health and safety, and developing an independent system to track and address racial discrimination.
Our findings underscore the poor health outcomes of PSWs. About 53% of the PSW participants perceived their health to be very good or excellent, which is lower than the overall proportion for Canadians (61.2% in 2019).41 Although more than 90% of Canadians were satisfied or very satisfied with their lives, only 72% of the PSW participants reported similar levels of satisfaction.42 More than 20% of the PSWs were also likely to be depressed, significantly exceeding the prevalence of major depressive episodes among Canadians (5.4%–11.7%); however, this proportion is consistent with evidence of mental health burden among health care workers, particularly during the COVID-19 pandemic.43–45 Poor work conditions, including exposure to injury, communicable diseases, violence, time pressure and mental stress, have a negative impact on the health of PSWs.12,13,46–49 Similarly, we found that some PSWs found their work to negatively influence their mental well-being and their personal relationships. Given reports of understaffing in long-term care during the COVID-19 pandemic,50 improving work conditions could minimize absence owing to work-related sickness or injury and help retain PSWs.
During the COVID-19 pandemic, PSWs were more likely to contract COVID-19 than physicians and nurses.51 Therefore, health inequity across occupations within the health care sector should be evaluated in future studies. Unmanageable workload, burnout and job stress have also repeatedly been shown to result in poor quality of care provided by health care workers.49,52,53 Subsequent studies could therefore consider evaluating the impact of job precarity among PSWs on the health outcomes of their clients. Assessing the characteristics of PSW workplaces that display poor quality of care, such as infectious disease outbreaks, could help identify key areas to address in quality improvement programming.
Limitations
A key limitation of our study is the lack of an adequate sampling frame, since PSWs in Ontario are not registered in a centralized registry. To overcome this limitation, we employed an RDS approach that used information about the recruitment chains and the connectivity of the participants to produce asymptotically unbiased estimates. This method allowed us to sample a hard-to-reach population, such as PSWs during the COVID-19 pandemic who worked long hours and could not be approached directly in their work locations because of public health restrictions. Despite the advantages of RDS, the convenience sampling of the seeds may result in a sample that is not representative of the PSW population in Ontario. Our study also focused on PSWs living in and around the GTA, which further reduced generalizability to other jurisdictions given differences in population characteristics, labour policies and demand for PSWs. Furthermore, RDS estimators have a relatively high degree of variability and rely on untestable assumptions, such as sampling with replacement.30
Other limitations include absence of rigorous measures to verify participant occupations, potential recall bias and inaccurate reporting, and the use of English in a long survey, which might hinder the participation of nonfluent individuals who might be subjected to different working conditions than those who are fluent in English. Nonetheless, the community-based approach helped with targeting issues pertinent to the PSW community and with the collection of data during the COVID-19 pandemic, when work conditions have been a particularly important factor in the spread of infection.15
Conclusion
The PSW workforce in the GTA is mainly made up of racialized and immigrant women. Personal support workers had low income and precarious employment, which included widespread absence of permanent and full-time positions, inconsistent work hours and schedules, lack of paid sick days and other extended benefits, and limited membership in labour unions. Uncertainty about their current employment situation also made them concerned about their ability to meet their financial obligations. Collectively, these poor working conditions negatively affected the well-being and mental health of PSWs. Equitable strategies are needed to provide decent work conditions for PSWs and to improve their health.
Supplementary Material
Acknowledgements
The authors appreciate the time and advice of the personal support workers who make up the advisory committee, assisting our planning, implementation and knowledge translation processes.
Footnotes
Competing interests: Andrew D. Pinto reports funding from the Canadian Institutes for Health Research (CIHR), the Government of Ontario, PSI Foundation, Maytree Foundation, Atkinson Foundation, St. Michael’s Hospital Foundation, Ontario SPOR Support Unit, the Canadian Institute for Health Information and the Public Health Agency of Canada. He also reports honoraria for presentations at the University of Toronto, McMaster University, University of Ghent, the North American Primary Care Research Group and Toronto Metropolitan University. He serves on the scientific advisory board of the Alliance for Healthier Communities, the Pan-Canadian Advisory Panel on a Framework for a Prescription Drug List organized by Canadian Agency for Drugs and Technologies in Health and the CIHR Institute Advisory Board for the Institute of Population and Public Health. He receives salary support from St. Michael’s Hospital and the University of Toronto, is the CIHR Applied Public Health Chair and is a scientific advisor to Mutuo Health Solutions. Ayu Hapsari reports an honorarium from Toronto Metropolitan University. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Andrew D. Pinto contributed to the overall conception and design of the work. All authors assisted with refining the research questions and plans for data collection, as well as the survey development. Ayu Pinky Hapsari recruited the participants and administered the surveys. Christopher Meaney conducted the analysis. All authors contributed to data interpretation. Andrew D. Pinto drafted the manuscript and all the authors revised it critically for important intellectual content. All authors provided their approval of the version to be published and agreed to be accountable for the work.
Funding: This research was funded by the George Cedric Metcalf Charitable Foundation. Andrew D. Pinto is supported as a clinician scientist by the Department of Family and Community Medicine (University of Toronto), the Department of Family and Community Medicine (St. Michael’s Hospital) and the Li Ka Shing Knowledge Institute (St. Michael’s Hospital). He is also supported by a fellowship from the Physicians’ Services Incorporated Foundation and as the Associate Director for Clinical Research at the University of Toronto Practice-Based Research Network (UTOPIAN). Funders did not have any involvement in the collection, analysis and interpretation of data, nor did they have any involvement in the writing of the report and in the decision to submit.
Data sharing: Data from this study are held in a secure network at St. Michael’s Hospital. Data are accessible only to the study team members named in the protocol who have been approved by the hospital’s research ethics board.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/2/E527/suppl/DC1.
References
- 1.Canada’s health care providers. Ottawa: Canadian Institute for Health Information; [accessed 2021 Feb. 4]. pp. 1–112. Available: https://secure.cihi.ca/free_products/hctenglish.pdf. [Google Scholar]
- 2.Sims-Gould J, Byrne K, Craven C, et al. Why I became a home support worker: Recruitment in the home health sector. Home Health Care Serv Q. 2010;29:171–94. doi: 10.1080/01621424.2010.534047. [DOI] [PubMed] [Google Scholar]
- 3.Zeytinoglu IU, Denton M, Brookman C, et al. Health and safety matters! Associations between organizational practices and personal support workers’ life and work stress in Ontario, Canada. BMC Health Serv Res. 2017;17:427. doi: 10.1186/s12913-017-2355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly C, Bourgeault IL. The personal support worker program standard in Ontario: An alternative to self-regulation? Healthc Policy. 2015;11:20–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Colombo F, Llena-Nozal A, Mercier J, et al. Help wanted? Providing and paying for long-term care. OECD Health Policy Studies. Paris (France): Organisation for Economic Co-operation and Development (OECD); 2011. [accessed 2021 Feb. 2]. Available: https://www.oecd-ilibrary.org/social-issues-migration-health/help-wanted_9789264097759-en. [Google Scholar]
- 6.Zagrodney K, Saks M. Personal support workers in Canada: The new precariat? Healthc Policy. 2017;13:31–9. doi: 10.12927/hcpol.2017.25324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 and the employment of health care workers. Ottawa: Statistics Canada; [accessed 2022 Feb. 9]. modified 2020 June 19. Available https://www150.statcan.gc.ca/n1/pub/89-28-0001/2018001/article/00019-eng.htm. [Google Scholar]
- 8.Job prospects: personal support worker — home support in Canada. Government of Canada Job Bank; [accessed 2022 Feb. 9]. modified 2022 Feb. 9. Available: https://www.on.jobbank.gc.ca/marketreport/outlook-occupation/24584/ca. [Google Scholar]
- 9.Zeytinoglu IU, Denton M, Davies S, et al. Casualized employment and turnover intention: home care workers in Ontario, Canada. Health Policy. 2009;91:258–68. doi: 10.1016/j.healthpol.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Long-term care staffing study. Toronto: Ontario Ministry of Long-Term Care; 2020. [accessed 2022 Jan. 13]. Available: https://www.ontario.ca/page/long-term-care-staffing-study. [Google Scholar]
- 11.Lilly MB. Medical versus social work-places: constructing and compensating the personal support worker across health care settings in Ontario, Canada. Gend Place Cult. 2008;15:285–99. [Google Scholar]
- 12.Hignett S, Otter ME, Keen C. Safety risks associated with physical interactions between patients and caregivers during treatment and care delivery in home care settings: a systematic review. Int J Nurs Stud. 2016;59:1–14. doi: 10.1016/j.ijnurstu.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Daly T, Banerjee A, Armstrong P, et al. Lifting the “violence veil”: examining working conditions in long-term care facilities using iterative mixed methods. Can J Aging. 2011;30:271–84. doi: 10.1017/S071498081100016X. [DOI] [PubMed] [Google Scholar]
- 14.Maness SB, Merrell L, Thompson EL, et al. Social determinants of health and health disparities: COVID-19 exposures and mortality among African American people in the United States. Public Health Rep. 2021;136:18–22. doi: 10.1177/0033354920969169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Upshaw TL, Brown C, Smith R, et al. Social determinants of COVID-19 incidence and outcomes: a rapid review. PLoS One. 2021;16:e0248336. doi: 10.1371/journal.pone.0248336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Focus on Geography Series, 2016 Census: Toronto, (CMA): Ontario Data products, 2016 Census. Ottawa: Statistics Canada; [accessed 2021 May 25]. modified 2019 July 18. Cat no 98-404-X2016001. Available: https://www12.statcan.gc.ca/census-recensement/2016/as-sa/fogs-spg/Facts-cma-eng.cfm?LANG=eng&GK=CMA&GC=535&TOPIC=1. [Google Scholar]
- 17.Saari M, Patterson E, Kelly S, et al. The evolving role of the personal support worker in home care in Ontario, Canada. Health Soc Care Community. 2018;26:240–9. doi: 10.1111/hsc.12514. [DOI] [PubMed] [Google Scholar]
- 18.Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 19.White RG, Hakim AJ, Salganik MJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology for respondent-driven sampling studies: “STROBE-RDS” statement. J Clin Epidemiol. 2015;68:1463–71. doi: 10.1016/j.jclinepi.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl. 2002;49:11–34. [Google Scholar]
- 22.Table 11-10-0241-01: Low income cut-offs (LICOs) before and after tax by community size and family size, in current dollars. Ottawa: Statistics Canada; [accessed 2021 May 11]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1110024101. [Google Scholar]
- 23.Lewchuck W, Laflèche M, Procyk S, et al. The precarity penalty: the impacts of employment precarity on individuals households and communities — and what to do about it Poverty & Employment Precarity in Southern Ontario. McMaster University Social Sciences and United Way Toronto. 2015. [accessed 2018 Oct 18]. Available https://pepsouwt.files.wordpress.com/2012/12/precarity-penalty-report_final-hires_trimmed.pdf.
- 24.Lewchuk W, Laflèche M, Procyk S, et al. Poverty and Employment Precarity in Southern Ontario (PEPSO) [survey] 2014. [accessed 2021 Dec. 6]. pp. 15–7. Available: https://www.economics.mcmaster.ca/pepso/documents/final-pepso-survey-2014.pdf.
- 25.Manual for constructing the PEPSO Employment Precarity Index. Hamilton (ON): Poverty and Employment Precarity in Southern Ontario (PEPSO); 2016. [accessed 2018 Oct 20]. Available: https://pepso.ca/documents/manual-for-precarity-index-2016-06-21-final.pdf. [Google Scholar]
- 26.OHS. Vulnarability Measure. Toronto: Institute for Work and Health; 2016. [accessed 2021 Jan. 20]. Available: http://www.iwh.on.ca/ohs-vulnerability-measure. [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JBW. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 28.Canadian Community Health Survey (CCHS) — 2019. Ottawa: Statistics Canada; [accessed 2020 May 8]. modified 2019 Dec 30. Available: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&a=1&&lang=en&Item_Id=1207185. [Google Scholar]
- 29.Salganik MJ. Variance estimation, design effects, and sample size calculations for respondent-driven sampling. J Urban Health. 2006;83(Suppl):i98–112. doi: 10.1007/s11524-006-9106-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Léon L, Des Jarlais D, Jauffret-Roustide M, et al. Update on respondent-driven sampling: theory and practical considerations for studies of persons who inject drugs. Methodol Innov. 2016;9:1–9. [Google Scholar]
- 31.Fraser J. Bill30510 paid sick days for Ontario Workers Act. Toronto: Legislative Assembly of Ontario; 2021. [accessed 2021 Dec. 21]. Available: https://www.ola.org/en/legislative-business/bills/parliament-42/session-1/bill-305. [Google Scholar]
- 32.Avery L, Rotondi N, McKnight C, et al. Unweighted regression models perform better than weighted regression techniques for respondent-driven sampling data: results from a simulation study. BMC Med Res Methodol. 2019;19:202. doi: 10.1186/s12874-019-0842-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hapsari AP, Ho JW, Meaney C, et al. The working conditions for personal support workers in the Greater Toronto Area during the COVID-19 pandemic: a mixed-methods study. Can J Public Health. 2022 doi: 10.17269/s41997-022-00643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van den Tooren M, de Jonge J. Managing job stress in nursing: What kind of resources do we need? J Adv Nurs. 2008;63:75–84. doi: 10.1111/j.1365-2648.2008.04657.x. [DOI] [PubMed] [Google Scholar]
- 35.Willemse BM, de Jonge J, Smit D, et al. The moderating role of decision authority and coworker-and supervisor support on the impact of job demands in nursing homes: a cross-sectional study. Int J Nurs Stud. 2012;49:822–33. doi: 10.1016/j.ijnurstu.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Wilkinson S. How nurses can cope with stress and avoid burnout. Emerg Nurse. 2014;22:27–31. doi: 10.7748/en.22.7.27.e1354. [DOI] [PubMed] [Google Scholar]
- 37.Ontario personal support workers in home and community care: CRNCC/PSNO survey results. Toronto: Canadian Research Network for Care in the Community; [accessed 2020 Feb. 8]. Available: https://www.ryerson.ca/content/dam/crncc/knowledge/infocus/factsheets/InFocus-OntarioPSWsinHomeandCommunityCare.pdf. [Google Scholar]
- 38.Neysmith SM, Aronson J. Working conditions in home care: negotiating race and class boundaries in gendered work. Int J Health Serv. 1997;27:479–99. doi: 10.2190/3YHC-7ET5-5022-8F6L. [DOI] [PubMed] [Google Scholar]
- 39.Common Statement 2017a common statement of principles on shared health priorities. Ottawa: Health Canada; [accessed 2021 Feb. 4]. Available: https://www.canada.ca/content/dam/hc-sc/documents/corporate/transparency_229055456/health-agreements/principles-shared-health-priorities.pdf. [Google Scholar]
- 40.Denton M, Brookman C, Zeytinoglu I, et al. Task shifting in the provision of home and social care in Ontario, Canada: implications for quality of care. Health Soc Care Community. 2015;23:485–92. doi: 10.1111/hsc.12168. [DOI] [PubMed] [Google Scholar]
- 41.Table 13-10-0096-02: Perceived health, by age group. Ottawa: Statistics Canada; [accessed 2021 Jan. 20]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009602. [Google Scholar]
- 42.Table 13-10-0096-05: Life satisfaction, satisfied or very satisfied, by age group. Ottawa: Statistics Canada; [accessed 2021 Jan. 20]. Available https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009605. [Google Scholar]
- 43.Dobson KG, Vigod SN, Mustard C, et al. Trends in the prevalence of depression and anxiety disorders among Canadian working-age adults between 2000 and 2016. Health Rep. 2020;31:12–23. doi: 10.25318/82-003-x202001200002-eng. [DOI] [PubMed] [Google Scholar]
- 44.Wilbiks JMP, Best LA, Law MA, et al. Evaluating the mental health and well-being of Canadian healthcare workers during the COVID-19 outbreak. Healthc Manage Forum. 2021;34:205–10. doi: 10.1177/08404704211021109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Overview: impacts of COVID-19 on health care workers. Ottawa: Canadian Institute for Health Information; 2021. [accessed 2021 Dec. 13]. Available: https://www.cihi.ca/en/health-workforce-in-canada-highlights-of-the-impact-of-covid-19/overview-impacts-of-covid-19-on. [Google Scholar]
- 46.Armstrong P, Armstrong H, Banerjee A, et al. Structural violence in long-term residential care. [accessed 2018 June 15];Womens Health Urban Life. 2011 10:111–29. Available http://www.diva-portal.org/smash/get/diva2:433372/FULLTEXT01.pdf. [Google Scholar]
- 47.Aström S, Bucht G, Eisemann M, et al. Incidence of violence towards staff caring for the elderly. Scand J Caring Sci. 2002;16:66–72. doi: 10.1046/j.1471-6712.2002.00052.x. [DOI] [PubMed] [Google Scholar]
- 48.Delp L, Wallace SP, Geiger-Brown J, et al. Job stress and job satisfaction: home care workers in a consumer-directed model of care. Health Serv Res. 2010;45:922–40. doi: 10.1111/j.1475-6773.2010.01112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruotsalainen S, Jantunen S, Sinervo T. Which factors are related to Finnish home care workers’ job satisfaction, stress, psychological distress and perceived quality of care?: a mixed method study. BMC Health Serv Res. 2020;20:896. doi: 10.1186/s12913-020-05733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marrocco FN, Coke A, Kitts J. Ontario’s Long-Term Care COVID-19 Commission: final report. Toronto: Ontario’s Long-Term Care COVID-19 Commission; 2021. [accessed 2021 Aug. 16]. Available: http://www.ltccommission-commissionsld.ca/report/pdf/20210623_LTCC_AODA_EN.pdf. [Google Scholar]
- 51.COVID-19 cases and deaths in health care workers in Canada. Ottawa: Canadian Institute for Health Information; 2021. [accessed 2021 Dec. 13]. Available: https://www.cihi.ca/en/covid-19-cases-and-deaths-in-health-care-workers-in-canada. [Google Scholar]
- 52.van den Hombergh P, Künzi B, Elwyn G, et al. High workload and job stress are associated with lower practice performance in general practice: an observational study in 239 general practices in the Netherlands. BMC Health Serv Res. 2009;9:118. doi: 10.1186/1472-6963-9-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Klein J, Frie KG, Blum K, et al. Psychosocial stress at work and perceived quality of care among clinicians in surgery. BMC Health Serv Res. 2011;11:109. doi: 10.1186/1472-6963-11-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.