Abstract
Objective:
The coronavirus disease (COVID-19) pandemic has presented unique challenges to pediatric emergency medicine (PEM) departments. The purpose of this study was to identify these challenges and ascertain how centers overcame barriers in creating solutions to continue to provide high-quality care and keep their workforce safe during the early pandemic.
Methods:
This is a qualitative study based on semi-structured interviews with physicians in leadership positions who have disaster or emergency management experience. Participants were identified through purposive sampling. Interviews were recorded and transcribed electronically. Themes and codes were extracted from the transcripts by 2 independent coders. Constant comparison analysis was performed until thematic saturation was achieved. Member-checking was completed to ensure trustworthiness.
Results:
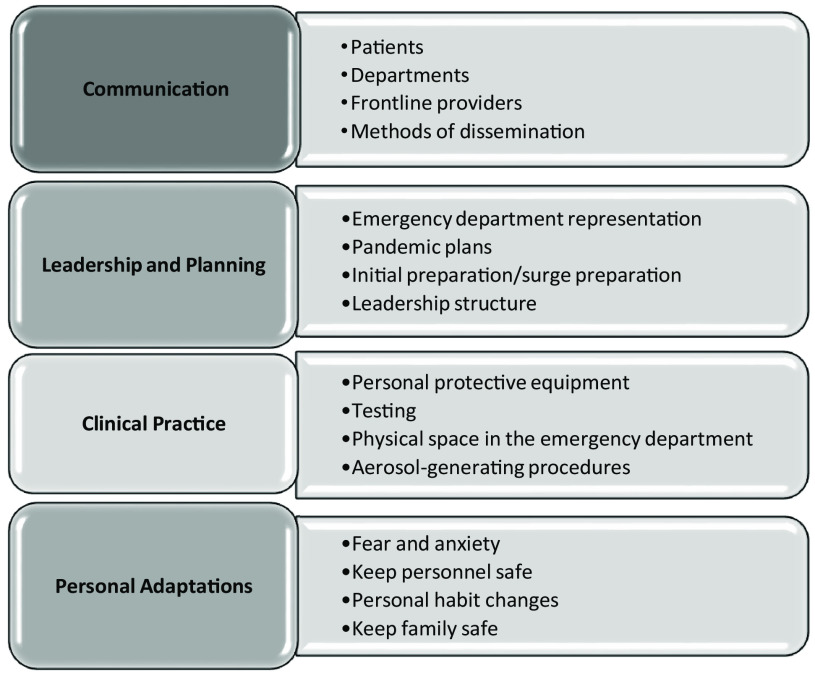
Fourteen PEM-trained physicians participated in this study. Communication, leadership and planning, clinical practice, and personal adaptations were the principal themes identified. Recommendations elicited include improving communication strategies; increasing emergency department (ED) representation within hospital-wide incident command; preparing for a surge and accepting adult patients; personal protective equipment supply and usage; developing testing strategies; and adaptations individuals made to their practice to keep themselves and their families safe.
Conclusions:
By sharing COVID-19 experiences and offering solutions to commonly encountered problems, pediatric EDs may be better prepared for future pandemics.
Keywords: COVID-19, disaster management, pediatric emergency medicine, qualitative
In December 2019, the coronavirus disease (COVID-19) epidemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was beginning in Wuhan City, China. By March 2020, COVID-19 was declared a pandemic by the World Health Organization. 1 As of July 27, 2021, there have been over 194 000 000 cases and nearly 5 000 000 deaths due to COVID-19. 2,3 With thousands of new cases daily, information has been constantly changing as researchers and the larger medical community attempt to better understand this pandemic and disseminate knowledge to the world.
To address the severe knowledge gaps that exist with COVID-19, many emergency departments (EDs) looked to their past experiences with pandemics such as the 2014 Ebola outbreak, the 2009 H1N1 influenza pandemic, and the 2003 SARS outbreak. Given variable and constantly changing practice standards, many institutions were forced to work through operational challenges on their own. Researchers in other countries hit particularly hard in the early months of the pandemic graciously shared lessons learned with the medical community. 4–6 However, these do not always translate to the experiences here in the United States, particularly at pediatric hospitals.
Pediatric emergency departments (PEDs) have faced their own set of challenges that may not reflect the experiences of EDs that primarily care for adults. For example, PEDs initially saw a precipitous decline in the number of arrivals, at the same time seeing the acuity of those patients rise. 7,8 Clinical and social complications, such as multisystem inflammatory syndrome in children (MIS-C) and child neglect, continue to challenge pediatric emergency medicine (PEM) providers throughout this pandemic. 9
As PEDs plan a way forward, we must seek to understand the unique experiences and lessons learned throughout this pandemic. This study aimed to identify the early challenges and barriers that institutions have faced as the pandemic has evolved. The primary objective was to report on the drivers that interfere with the ability to provide high-quality medical care during a pandemic and to report on how institutions overcame those forces. The secondary objective was to identify areas of improvement for health care systems to consider when preparing for anticipated surges within this and the next pandemic.
Methods
Content analysis of social media postings, opinion pieces, and a PEM email distribution list identified COVID-19-related themes discussed by PEM physicians. These themes, as they related to the current COVID-19 pandemic, served as a framework, and guided the creation of semi-structured interview questions.
Participants, all PEM physicians, were identified using a purposive sample. The participants were working as frontline providers during the COVID-19 pandemic. Participants were identified using the researchers’ professional contacts at other institutions and are members of a network of disaster management leaders at PEDs around the United States. Participants were contacted via email and asked to participate. Willing participants were assigned a unique ID and asked to fill out a demographic survey prior to the interview. No personally identifiable data were collected. Consent was implied with survey completion. Participants could opt out anytime during the study. Survey data were securely stored using REDCap 10 data capture tools hosted at Texas Children’s Hospital. IRB approval was obtained.
Interviews were conducted and audio-recorded using Zoom video conferencing software. They were auto-transcribed using Otter.ai (Los Altos, California) voice-to-text transcribing software, and transcription errors were corrected to create the raw data.
Given that these were semi-structured interviews, interviewers were provided a guide with suggested questions and topics with unscripted questions utilized to elicit further experiences and thoughts.
Two independent coders (TT, EMS) analyzed the raw data to summarize topics and form descriptions of interview answers to allow for investigator triangulation. Thematic saturation in the semi-structured interviewers was achieved when no new themes emerged in successive interview transcripts. The two coders developed mutually agreed-upon definitions for each code and established examples of each code to ensure reliability and trustworthiness. These members discussed the qualitative findings and developed themes from the codes. A third member of the research team (ND) was available to review any disagreements in coding so that team consensus could be reached. Memos of coding decisions were kept for consistency as analysis progressed. Member checking was performed to review themes and to check for accuracy and completeness of the findings. This thematic approach is a widely utilized process in the analysis of qualitative data 11 and was used in our study to identify a conceptual framework of themes related to disaster management during the pandemic.
Results
Participants
A total of 14 PEM fellowship-trained physicians from academic centers with rotating fellows and residents participated. More than half were women with the median years of experience after fellowship being 15 years. Half held leadership roles within their institution, almost all were part of their institution’s disaster or emergency management department, and the majority had received specialized disaster management training (Table 1). Member checking was accomplished using a Zoom focus group of 4 participants.
Table 1.
Participant and institution demographics
| Descriptor | Response categories | Number (%) (N = 14) |
|---|---|---|
| Sex | Female | 9 (64.3%) |
| Male | 5 (35.7%) | |
| Race | White | 9 (64.3%) |
| Black or African American | 1 (7.1%) | |
| Asian | 4 (28.6%) | |
| Years of experience post fellowship a | Median (range) in years | 15 (5–30) |
| Residency specialty | Pediatrics | 14 (100%) |
| Fellowship specialty | Pediatric emergency medicine | 14 (100%) |
| Global health | 1 (7.1%) | |
| Received specialized disaster management training | Yes | 11 (78.6%) |
| No | 3 (21.4%) | |
| Disaster management team member b | Yes | 13 (92.9%) |
| No | 1 (7.1%) | |
| Disaster management role | Director | 10 (71.4%) |
| ED representative | 3 (21.4%) | |
| None | 1 (7.1%) | |
| Other leadership positions identified | Chief of clinical operations | 1 (7.1%) |
| Chief of quality, medicine | 1 (7.1%) | |
| Trauma medical director | 1 (7.1%) | |
| Chief of emergency medicine | 2 (14.3%) | |
| PEM fellowship director | 1 (7.1%) | |
| Director of risk management | 1 (7.1%) | |
| None | 7 (50%) | |
| Geographic location of institution where employed c | Northeast | 5 (35.7%) |
| Midwest | 5 (35.7%) | |
| South | 1 (7.1%) | |
| West | 3 (21.4%) | |
| Annual census d | 20 001–45 000 | 5 (35.7%) |
| 45 001–80 000 | 5 (35.7%) | |
| > 80 001 | 4 (28.6%) | |
| Type of clinical setting | Academic | 14 (100%) |
| Shared space with adult ED | Yes | 1 (7.1%) |
| No | 13 (92.9%) | |
| Learners in the ED | Residents | 14 (100%) |
| Fellows | 14 (100%) | |
| Medical students | 14 (100%) | |
| Department leadership e | Pediatrics | 12 (85.7%) |
| Emergency medicine | 2 (14.3%) |
ED, emergency department; PEM, pediatric emergency medicine.
Number of years practicing following the conclusion of fellowship training.
Disaster management and emergency preparedness are used interchangeably.
Northeast (ME, NH, MA, RI, CT, VT, NY, PA, NJ, DE, MD), Midwest (OH, MI, IN, IL, MO, IA, WI, KS, NE, SD, ND, MN), South (WV, DC, VA, KY, TN, NC, SC, GA, FL, AL, MS, LA, AR, OK, TX), West (NM, CO, WY, MT, ID, UT, AZ, NV, CA, OR, WA, AK, HI).
Estimated annual census of emergency departments prior to the COVID-19 pandemic.
Divisions of pediatric emergency medicine under the leadership of either the department of pediatrics or emergency medicine.
Themes
Many used the semi-structured interviews as an opportunity to share their frustrations, and what did and did not work well. Four primary themes emerged from these interviews: communication, leadership and planning, clinical practice, and personal adaptations (Figure 1). The following are the summarized themes with select quotes that highlight the codes elicited from the interviews (Table 2). Solutions and recommendations to these challenges mentioned by participants are summarized in Table 3.
Figure 1.
Themes and codes identified from semi-structured interviews.
Table 2.
Identified themes from interviews with example quotations to demonstrate underlying codes
| Theme | Code | Example quotation |
|---|---|---|
| Communication | ||
| Patients | “… So I think it’s hard on the kids to have us walk in with these. Even if it’s just a gown and gloves and face mask. We look pretty ridiculous…I think we’ve lost some of that kind of humanity side of being pediatricians where you now just look like a little space monster walking in.” | |
| “I feel now that there is a barrier between myself and my patients that hadn’t existed before. And there’s just something about the masks and the goggles, and the gown, and all of that, that that sets up a barrier…a small example is having to walk in the room and ask the parents to put on a mask, you know, so you become the mask police and it’s set us up for negative interaction.” | ||
| Departments | “I think everyone got the same information, but I think where we ran into some difficulties was that our physicians are employed by the university. The nurses and everybody else are also employed by our health care facility.” | |
| “The COVID leader from the ED team would communicate with ED staff, and kind of filter out or filter through all the different messages that were coming out and making sure everything was synced, because in the beginning, there was just an overload of information coming from multiple different resources…So one of our jobs we identified within the first month was to filter through that information and summarize it for everybody.” | ||
| Frontline providers | “…because we try to keep the door closed, there is minimal communication in and out of the rooms. This was much harder. So we actually set up iPads and were able to create Zoom conference for each of our resuscitation rooms so that the outside teams could listen in.” | |
| “Also, with our resuscitation rooms now being completely empty we have the role called the gatekeeper, and they stand by the door, and they help with communication, but they also help with getting the right people in, but they’re also making sure that not everybody goes in. So they’re exactly the kind of a gatekeeper role.” | ||
| Methods of dissemination | “…we have these huddles first, we’re having them daily, like every morning, there’d be a little huddle in the command center. And all information was supposed to come through there and, you know, be checked by the team and then disseminated out once we thought we had the right information, especially when it was changing so frequently, like with what’s aerosolized and what PPE do you use, and what is our visitor policy…We would then incorporate whatever new things had changed in the last five hours since information was changing so fast into the twice daily ER board huddles with physicians, nurses, techs, etc.” | |
| “I think our communication could always tune it up a little bit. You know, finding new ways to reach people, global emails are fascinating, but nobody reads the global emails. I would definitely do the town halls again. I think it’s important to be transparent.” | ||
| Leadership and planning | ||
| ED representation | “…we really needed to have representation, because it was clear that the infection prevention people didn’t necessarily have the perspective or the appreciation for the frontline worker. And a lot of it was kind of almost like a clinics approach or inpatient approach to COVID, which is much different.” | |
| “I was the incident commander for the ED. And so I had two associates, a nurse and a physician who would virtually communicate with me while I was in the actual incident command for the hospital. So I was the liaison officer to the ED in a way. And so that was really helpful.” | ||
| Pandemic plans | “I was hoping that H1N1 and all that stuff we learned from that would help. And it doesn’t because it’s a different disease. Totally different.” | |
| “There’s a Bio-Response Team hospital wide that was set up to prepare for Ebola. We were one of the few centers in the US that would accept Ebola patients. So that infrastructure was there, and we’ve kind of pivoted to COVID and COVID prep.” | ||
| Initial and surge preparation | “I think after any type of event, you always think, Oh, I wish we just spent a little more time with X, Y, or Z. Like we spent so much time trying to figure out how we set up stupid surge tents, which we never used, maybe we’ll use someday. But we should have already had that as a plan. Like, we should have had a type of surge tent plan for any type of aerosolized disease anyway. And we didn’t.” | |
| “I usually did one pediatric and one OB, tabletop, and we would just, we would just run it for, you know, half hour with our incident command staff, just to sort of run the whole thing. And it was interesting, because, you know, a lot of it was done virtually…this was done to test new protocols.” | ||
| Leadership structure | “We had too big a group at the beginning, we narrowed it way down to about maybe eight people after a while, and that helped get decisions made.” | |
| “We’re changing up how we do training for incident command going forward because we found that sometimes roles would start muddling together and planning an operation would kind of start squishing together in that way.” | ||
| Finances and taking adult patients | “We definitely cut shifts back and you know, I’m sure like everywhere like there’s zero raises this year. There’s no bonuses, there’s no travel money, there’s no CME money, there’s none of that. There’s no extra money anywhere when there’s no hiring. So they did cuts like that, but we didn’t have to take a salary cut.” | |
| “So we have a plan in place that we would take people up to the age of I think 30. Our surgeons are on board to do things like appendectomies and cholecystectomies, and I think ortho might be on board to do simple ortho stuff, you know, we’re obviously not going to take sick COVID people, though we did take a 42 year old on ECMO in the ICU, which was insane” | ||
| Supply chain | “Supply chain had already planned for a lot of this in the sense that once they knew this was coming, they started looking to see who are my other suppliers besides all the suppliers from China…How can we get here? How can we go collaborate with the distillers to get our hand sanitizer?” | |
| “We had one of those calculators and a dashboard in the command center where you see the number of ventilators, PPE, number of N95s a week, it was constant inventory control and constant management.” | ||
| Clinical practice | ||
| Personal protective equipment | “I mean, very early on, there were recommendations that said, maybe masks weren’t even helpful, like this was coming from I think it was the CDC, which is really interesting to think about the history of all this. So are masks really helpful? Or should they just be used by people who have preexisting condition conditions or immunocompromised and this kind of thing? You know, and then you have, what sort of masks should we be using? You know, and then it felt like a switch kind of flipped.” | |
| “It’s been clear that a lot of the recommendations I’m talking about now even at the national level, has been based more on less science and more on issues like supply chain and availability” | ||
| “So just the very concept of wearing an N95 for multiple patients, you know, that’s hard to justify from a medical perspective, and for both the provider and also for all those patients. And yet, you know, the thought of every provider switching out their mask in between every patient that wasn’t tenable, either.” | ||
| “We had a robust and highly safe repurposing process. You doffed your N95, you packed it, you put it in a room, it was taken and went through a chemical cleaning, and brought back to you was labeled with your name.” | ||
| “We developed a guide, you know, we follow the guidelines from the university and then basically posted them on every door, going into each exam room on how to put on your PPE and take it off, where to store it, and then the reuse guidelines. And then we would have like PPE champions who would kind of go around just watching people as they don and doff and help them.” | ||
| Testing | “We never developed our own in-house test. We’ve been using Abbott. That limited us. And initially we had to work through the State and County Department of Public Health to get our testing like everyone did.” | |
| “We’ve had some rapid tests that we’ve had to dole out very carefully, rapid antigen and rapid PCR that we use for behavioral health and emergency surgery, but we’ve only got like an average of like, 4 per day.” | ||
| “April is when we started having in-house testing, but again, it was very limited, really the main limitation was the reagent. And so we you could do in-house testing, but it was only for those that were high risk or PUI.” | ||
| “Our biggest success honestly, was that drive thru site that we established within five days…” | ||
| “Once we had more testing availability, we actually started being a little bit more liberal. So, we test for kind of softer symptoms just to get a better idea of the actual prevalence rate in the community. So even if you had just kind of vague symptoms sometimes, we were testing or if you had a symptomatic contact.” | ||
| Physical space in the ED | “And so instead we’re going to split the ED into two different areas and the symptomatic over here asymptomatic kids over here. And so that was sort of the approach that we took.” | |
| “So, we bifurcated folks from the beginning at our visitor desk and asked them questions. Then we put a divider in our waiting room. So, there was one side that was the PUI side and one side that was not; so orthopedic injuries, that sort of stuff. But eventually, we came to the realization that almost everyone who lives in this community could be a PUI even if you didn’t have symptoms. So, the curtain, the divider, eventually went away.” | ||
| Aerosol-generating procedures | “… early on there was no consistent document that described the way aerosol-generating procedures affected spread. Well, whose information do we use? Do we just use our own expert opinion on that? Because then what if one person of those 20 experts says the air contrast enema is an aerosolized procedure. Well, then we have to have everybody in radiology wearing N95s and hazmat suits to do an air contrast enema.” | |
| “We actually were able to change air flow over for a lot of our other rooms. So, facilities, I call them down had them change over the flow of the air. So, it’s not negative pressure, but there is at least a negative flow in like, thankfully, our EDs filter out so it doesn’t go anywhere else.” | ||
| Personal adaptations | ||
| Fear and anxiety | “I think from a leadership perspective, it was difficult trying to figure out how do you help address those fears, in that minor number of people, but if you didn’t address it, their fear and anxiety spread to everyone else that we’re working with. And so, trying to figure out how you contain that, I think was a struggle.” | |
| “So, people have just sort of settled in. And I think, you know, once people started seeing the experience elsewhere, I think that people started feeling a little bit better about the protection they had.” | ||
| “…there was also the reverse, where there were people who were like, you know what, we got this, and they were willing to step in and be on the front lines. And I think more than the panic, we had more people who wanted to step up and figure out how to solve and engage in solutions rather than problems.” | ||
| “…the initial response when the anxiety was so high was to have that reassurance. I remember there’s a couple people that came up to me. I led a huddle and I said, look, you know, I don’t know what’s going to happen, but everybody’s going to be okay. You know, like, we just need to put out that message, we don’t know, but we’re going to support each other, and we’re going to be okay, and that actually, people came up to me later and said, that was really helpful for them to hear just because, you know, everything was changing so much.” | ||
| Keeping personnel safe | “And then there are definitely some who took it a little less seriously, who would, you know, sit with their goggles off or mask partly down on the chin, or you know, the shared computer space. And so there have been multiple discussions about no eating and drinking around the computers and keeping your mask and goggles on the whole time.” | |
| “I feel a great deal of confidence that if we had to deal with another Ebola event, that we’re not going to have to do a lot of training for people because everyone’s just so used to putting stuff on nowadays.” | ||
| “We have not had a single positive faculty member or fellow…we’ve had maybe only three hospital transmissions, but they’ve all been from employee to employee, not patient. Yeah. So, we’ve done well…” | ||
| Personal habit changes | “I don’t think that I have ever taken the time to look at my infection control practices as much as I have to the point of how often do I clean my stethoscope? When do I click the keyboards at the beginning of my shift? How often do I wear gloves? I mean, yeah, no, I don’t like wearing gloves. I kind of like the touch of people. And so even that has been different. So, it’s, I think it’s my infection control practices. And I probably should be doing it all the time in an ER, but I just haven’t done it.” | |
| “And so maybe I’m making judgments from the doorway, you know, looking through the glass door, and looking at the patient that way, or relying on my residents and fellows who have been in the room, you know, to give me updates.” | ||
Table 3.
Commonly discussed challenges based on identified themes and ways participants addressed these challenges
| Theme | Challenge | Recommendations |
|---|---|---|
| Communication | ||
| Reaching a large department with updates | • Shift huddles with entire ED staff to share new updates • Town hall meetings with leadership • Bidirectional communication between leadership and frontline • Leaders and administrators be physically present in ED to answer questions early in a pandemic |
|
| Keeping information consistent | • Establish public information officer role early • Establish education group to review CDC updates • Information should only come from incident command |
|
| Large numbers of emails and rapidly changing processes | • Limit use of email to one update email per day • Highlight the newest process revisions within emails • Create internal websites for staff to reference • Create short videos from leadership highlighting new changes |
|
| Traumas and resuscitations | • “Gatekeeper” makes sure the right people are in the resuscitation and help communicate with consultants • Everyone wears a role tag over their PPE • Use iPads for video conference resuscitations so that outside teams could listen |
|
| Leadership and planning | ||
| ED representation within leadership | • Identify ED COVID leader to be on daily command center calls • ED COVID leadership team responsible to summarizing updates |
|
| Pandemic plans and adjusting to new outbreaks | • Create a containment unit • Know your supply chain and have backup vendors • Regularly update emergency operation plans |
|
| Initial preparation | • Use hospital-wide “emergency” drills to test plans and communication structure • Reach out to colleagues in other countries or across the US experiencing the pandemic • Open command center early • Have a surge plan ready even if you do not need it |
|
| Setting up leadership structure | • Establish collaboration across the local health care system • Keep roles consistent and train individuals on how to perform duties in incident command • Regularly update business continuity plans • Know who your leaders are for different groups and involve them early • Have multiple people trained in the same role and rotate them through incident command |
|
| Adjusting to patient volumes and adult patients | • Have plan to care for adults in emergency operations plan • If no surge, repurpose surge areas for testing and screening purposes • Utilize telehealth to consult on pediatric patients at other EDs |
|
| Managing supply chain | • Use predictive modeling and dashboards to track PPE and other supply • Foster relationships with new vendors or other health care institutions to share supplies • Invest in multiple forms of protection, that is, PAPRs and N95s |
|
| Clinical practice | ||
| Aerosol-generating procedures | • Even if room is not negative pressure, try to change flow to “negative air flow” • Practice airway simulations • Consider PAPR hoods for all intubations |
|
| Testing | • Establish “drive-thru” and community testing sites • Create in-house testing capabilities early • Do not wait on test results before admitting patients • Have access to multiple testing modalities in case you run out of supplies for one, you have the other |
|
| Cohorting patients | • Perform triage in the room if able • Understand asymptomatic patients may have infection and cohorting patients based on symptoms may not be necessary • Treat everyone like a PUI |
|
| PPE | • “PPE spotters” to ensure staff are properly donning and doffing • Post videos online that review proper donning and doffing techniques • Offer “refresher” training on proper PPE usage during prolonged pandemics • Have multiple methods for repurposing N95s • Early on, institute mandatory masking and eye protection for staff to limit in-hospital spread |
|
| Personal adaptations | ||
| Addressing fear and anxiety | • Be transparent about supplies, testing, protection, and plans to keep staff safe • Make leaders available to address questions • Offer reassurance and lead by example |
|
| Keeping personnel safe and healthy | • Safety monitors to ensure proper PPE use • Remind consultants coming to ED to wear proper PPE • Provide support hotline to staff for information about testing, child care, mental health, and other needs |
|
| Personal changes | • Use room phones to update patients and families • Use monitors in room so one can check up on vitals from doorway • Rely on resident and fellow evaluations to limit contact • Avoid excess clothing, and change scrubs before going home |
|
Communication
Early in the pandemic, multiple participants remarked they “don’t spend as much time as I used to (with patients) because getting in and out of the room is challenging with all the gear I have to wear.” This makes building rapport difficult, especially when the children think “we look like monsters sometimes coming in these rooms.” Additionally, the personal protective equipment (PPE) makes hearing difficult, not only for the provider, but also for the patient and their family. These communication challenges make ED visits “not as a personal experience as it used to be.”
With ever-changing recommendations, participants identified difficulties reaching providers within their division about new processes, whether related to PPE, testing, or return-to-work guidelines, to name a few examples. One participant remarked, “We have over ninety plus practitioners plus over 200 nurses, and all these rotating residents. How do you communicate all the changes when they change so fast?” Emails were viewed as a necessary means of information dissemination, but institutions and leaders “had to figure out what’s the cadence of sending those things (emails) out. If you send 3 of them and someone doesn’t get a chance to look at them daily, they’re flooded.” To address the overwhelming number of emails, several institutions incorporated town hall meetings with leadership, shift huddles, and designating an ED point person to consolidate the information coming from incident command (IC). Internal websites were created for providers to reference changes.
Traumas and resuscitations that require closed-loop communication, precision with medications and orders, and multiple people working in concert, posed new communication challenges. With the extra layers of PPE, “no one can hear the team leader very well.” Resuscitation teams limited their numbers to prevent potential exposures to an entire department, and as a result have “gone to virtual or partly virtual resuscitations with a limited team in the room.” To address this issue of limited personnel, institutions have incorporated radios or tablets; in some centers, a new role, the “gatekeeper,” was created to communicate with those outside the trauma or resuscitation bay.
Leadership and Planning
As frontline providers, participants stressed the importance of ED representation within IC. One participant put it plainly: “Taking the IC side, I mean, the hospital leadership view, they had to deal with like, the entire hospital. Right, not just the ED but the ED is like a unique organism. So, I think it was hard for them to see what the needs were in the ED when they didn’t have ED representation on the hospital leadership team.” To address this challenge with ED representation at the hospital leadership level, it is key to “identify a group of people interested in pandemic and disaster preparedness” and develop a “leadership COVID team within the ED…” These leaders “would communicate with ED staff, and kind of filter out or filter through all the different messages that were coming out and making sure everything was synced,” which ensures bidirectional communication with IC.
As COVID-19 cases increased, institutions initially prepared by looking to their past experiences with pandemics. At some institutions, these plans were helpful in terms of “PPE readiness,” developing a “command center,” and deploying “bio response teams.” However, as several mentioned, past experiences did not apply or help with the response to COVID-19 because simply “it’s a different disease.”
For most, planning for COVID-19 began as early as January 2020. Some institutions “started discussing strategies in late January, and, started doing simulations toward the end of February.” Others began to prepare for a surge: “We knew pretty early on, or we had heard earlier on, there were not many pediatric cases. But, you know, again, we just didn’t know at that time, so we were ready for a pediatric surge.” Alternative care sites (ACS) to receive the anticipated surge were built at some institutions only to discover that at least, prior to any variant-led surges, space was not a limiting factor. “In the first, I’d say three, four months of the pandemic, we had five COVID positive kids. And so, we had the tent set up, and I don’t regret doing it…But we definitely didn’t use it like we thought we would.” Several institutions chose to wait before setting up ACS based on experiences elsewhere: “The initial indication of that was from the New York experience. As we know, the adult hospitals got hit hard. Early in the pandemic, pediatric hospitals were relatively spared. And we had no reason to think then that our experience would be any different.”
As the pandemic progressed, participants reflected on challenges working across health care systems. Several mentioned challenges collaborating with other hospitals: “But even regionally, every hospital was kind of building its own fort. And there was very little collaboration with one another.” Even within their own institution, participants expressed frustration working with other departments. “It was harder to get people on board, to not think of themselves as needing special privileges…” To address these challenges, participants recalled methods to improve command structure and leadership within their institution. This included establishing a centralized command quickly and using “the information officer to keep things consistent,” opening command to physicians and “allowing physicians to have a voice,” and establishing collaboration across health care systems because it can “result in innovations.”
Additionally, the early COVID-19 pandemic had other unintentional consequences, especially when it came to hospital finances and patient volumes. Initially, many institutions began to cut cost as “they saw numbers go down and elective surgeries being shut off.” For them, the easiest thing to do was “furlough nurse practitioners” and “cut shifts back.” To relieve the overstressed nearby adult hospitals, pediatric centers also began admitting adult patients or accepting their pediatric patients to free up more space for adults. Instead of preparing for a surge, centers “created plans to care for adults.”
Managing the supply chain became the focus of many leaders within their institutions’ command structure to ensure adequate amounts of PPE, ventilators, and testing materials. Institutions that created real-time “dashboards” and “calculators” could keep constant inventory control. Collaborating with other industries such as liquor distillers ensured some institutions had enough hand sanitizer.
Clinical Practice
Aerosol-generating procedures (AGP) created their own set of challenges as institutions looked to contain the infectious droplets created. Part of the struggle was defining AGPs and how these procedures “affected spread.” In response, institutions with the capabilities moved these procedures into “negative pressure rooms”; in 1 instance, the entire ED was able to change the air flow in the rooms to negative flow. Others enforced mandatory use of powered air purifying respirators (PAPR) in resuscitation rooms or during intubations.
Before in-house testing was commonplace, “tests were controlled by the CDC or through public health…and every potential patient had to be run by public health before we would be allowed to test.” ED providers were also frustrated by inpatient units refusing patients until results returned: “We tell people that they don’t have to do that, that it is ok to admit at least an asymptomatic patient to the floor pending a result.” Operating rooms and inpatient psychiatric units also demanded test results before accepting patients, so institutions employed rapid tests that would provide results within 1 hour. Several institutions were able to deploy “drive-thru testing” and any patient who visited the ED could get tested once the supply was secured. Three-dimensional printing was able to create swabs that were in short supply nationwide. Overall, participants thought liberalizing testing was a necessity in addressing the pandemic.
To limit the spread between infected persons and other patients, some institutions divided their EDs between cohorts: COVID PUIs (patient under investigation) and the non-PUIs. Cohorting required rooms and pods to be redesignated “COVID assessment areas” and equipment was removed to prevent contamination. Many participants expressed that dividing patients was unnecessary as they “came to the realization that almost everyone who lives in the community could be a PUI even if you didn’t have symptoms.” To address the asymptomatic PUI, institutions adopted practices such as “triage in the room” to limit exposure of non-infected patients. Institutions that built ACSs re-purposed areas for screening.
PPE posed unique challenges as recommendations changed frequently. N95 face masks were especially difficult to obtain early in the pandemic, so several institutions chose to reserve their use based on the prevalence of COVID-19 in their community. One participant said, “We only have a seven-day supply of N95s, do you want to use them up? Now? When the incidence is so low, the prevalence of it in the community is so low, or do you want to use the N95s when the prevalence is higher, and you really do need the N95?” To address supply chain issues with N95 masks early on, some institutions developed sterilization procedures involving “hydrogen peroxide vaporization” or “UV light sterilization” to render N95s safe for reuse. To ensure staff was wearing the appropriate PPE correctly, some employed strategies such as “PPE spotters” to ensure staff was properly donning and doffing PPE while in the ED. As individuals became more proficient at wearing PPE, institutions could link videos to proper donning and doffing technique on their website for review. PPE guides were posted on patients’ doors to instruct providers on what PPE was required for that patient.
Personal Adaptions
Early on, individuals did not feel safe coming to work and participants discussed challenges with addressing the fear COVID-19 struck in the entire ED staff. One individual said, “…there was irrational fear, even with the degree of reassurance that we tried to provide, it seemed like there were those individuals who, during normal times, are very rational people who then became very hard to convince that it’s safe to be at work.” At an institution where a team member became ill due to COVID-19, fear was an even bigger challenge to address: “We actually had one of my division members in mid-March, at the beginning of this, who actually got very, very severe COVID. That impacted our division significantly… And he didn’t have any reasons to be so sick, just unlucky. That made all of us a little more cautious.” To address this fear and anxiety throughout the ED, participants reiterated the importance of communication, setting an example for others to follow, involving all staff in shift huddles, being flexible with scheduling and securing, or at the least planning for a robust PPE supply.
In addition to securing adequate PPE, leaders discussed challenges keeping their colleagues and workforce safe throughout the pandemic. Even within departments, there were personnel who at times “took it a little less seriously” than others and would do things such as “sit with their goggles off and mask partly down their chin” or share workstations meant for 1 individual to use. “Burnout” was mentioned by several participants as providers were constantly dealing with changes to PPE, testing, and management of COVID-19 patients and people were “feeling the stress of this long process.” “Safety monitors” were useful in ensuring that individuals followed regulations. To keep exposure at a minimum, non-clinical staff such as registration or research staff utilized in-room phones and tablets to interact with families. Employees were tested frequently, and institutions “moved away from in-person screening of every employee” to using cellular phone applications. By employing these methods, nearly every participant mentioned they had very little spread within their workforce.
All participants discussed changes they made to their routine at work or when coming home to keep themselves and their families safe. Most participants reflected that perhaps they did not wear adequate PPE for patient encounters prior to COVID-19. Many mentioned “changing in the garage” and “showering before seeing family” as ways to protect one’s family from exposure to the virus. Wardrobes have changed as “everyone has ditched the white jacket,” and even providers who used to dress professionally are now wearing scrubs. To limit their exposures and preserve PPE, several mentioned they “make judgements from the doorway” or “rely… on residents and fellows who have been in the room” to re-evaluate patients.
Discussion
Since late 2019, the world has been at war with COVID-19, 12 and EDs have continued to be the first line of defense for many health care systems where they serve as the primary access points for many patients. 13,14 Despite initial drops in overall pediatric patient volumes and low mortality, as of August 16, 2021, COVID-19 has affected more than 4 000 000 children nationwide, with numbers increasing daily due to new variants that are changing the landscape of COVID-19. 7,15–19 PEDs’ experience with COVID-19 has forced many leaders to re-evaluate their pandemic planning and approach to disease outbreaks. We set out to understand those issues faced by PEDs due to the early COVID-19 pandemic and provide possible solutions to improve the emergency response.
As emails were flooding mail servers, the way we communicated early during COVID-19 highlighted challenges with reaching large, multi-disciplinary departments. While interdepartmental communication was challenging, so was speaking with patients and colleagues during traumas and resuscitations. In a national survey of 25 PEDs, mass email messaging was utilized by 96% of the institutions during the COVID-19 pandemic. 20 Email is a quick and easy communication modality that can be utilized to update departments and reiterate important information that is rapidly evolving. 21,22 However, as our participants discussed and as mentioned in previous studies, the number of emails received per day can be overwhelming. 23 By limiting the number of emails sent and highlighting the most important changes within the text of the emails, important updates are better received. In addition to adjusting the number of emails, our participants echoed the utility of virtual town hall meetings with leaders, shift huddles, internal web pages, and opening divisional meetings to non-physician staff. 22,24 For traumas and resuscitations, participants recommended using technology and team members to communicate with consultants, pharmacists, and other team members outside of the trauma bay. Tablets with video conferencing capability, baby monitors and 2-way radios, secure network cell phones, and white boards are all ways to enhance communication during the care of these complex patients during a pandemic. 25–27
Disease outbreaks and other public health emergencies highlight the necessity of strong hospital and departmental leadership, as well as having a flexible plan for addressing the emergency. The top-down leadership approach during a pandemic or other disaster is often not well-received by ED physicians who wish to participate. 14 As mentioned by participants and described by others sharing their institution’s experience with COVID-19, developing multi-disciplinary ED leadership teams not only helps improve communication, but also can be useful in surge planning, improving collaboration with other institutions, streamlining logistics, and setting up IC structure within the ED. 21–23 Additionally, by being physically present in the PED, leaders are able to better understand the workforce’s concerns and provide reassurance to address those concerns. 18 Following the 2009 H1N1 outbreak, the Institute of Medicine developed the crisis standards of care, emphasizing the importance of early preparation and management of resources during a disaster to maximize patient care and minimize harm. 20,28 This framework for disaster preparedness was discussed by several of the participants and was evident in discussions around ACSs, re-deploying staff to care for adults, 9,26,29–32 keeping plans up-to-date, and knowing the supply chain. While it is challenging to predict the need, having those ACSs available and knowing how to re-purpose them is invaluable to an institution’s pandemic preparation. 23
Much has evolved in our clinical approach to COVID-19 regarding PPE, testing, triaging patients, AGPs, and airway management. Aggressive, early PPE practices were almost universally recommended by participants as droplet and enhanced precaution (addition of N95 mask or respirator) guidelines were refined, as was using negative pressure or negative flow rooms for AGPs and using video laryngoscopes for intubations. 20,33,34 PPE champions and interpersonal accountability for properly wearing and disposing of PPE helped ensure that staff were donning and doffing correctly, as well as helping mitigate supply shortages. 20,21,33 As testing capabilities improved and institutions developed their own in-house testing, it became evident that we could not test everyone without running out of supply. 23 While it is crucial to have widespread testing available for the community during a pandemic, testing those deemed “high-risk” based on symptoms, risk factors, or those being admitted to the hospital or going to the operating room should be given priority within the PED. 20,21 While some participants discussed eventually moving away from cohorting patients in favor of treating everyone like a PUI, having the capability to physically separate PUIs from the rest of the patient population is crucial to infection control during a pandemic. The wide array of symptoms observed in pediatric patients, including not only respiratory but also gastrointestinal, musculoskeletal, and cardiovascular symptoms, persuaded many centers to treat everyone like a PUI and institute universal PPE procedures for all patients. 26,35–37
During a pandemic or other public health disaster, health care workers routinely put themselves in danger as they are filled with a sense of duty to assist. This lack of regard for personal safety does not extend to the fear health care workers have of transmitting illnesses to their families or to other patients. 14,38 Recommendations for protecting the PED workforce, especially those with higher risk of severe disease go beyond adequate PPE supplies and include introducing new strategies to appropriately minimize interactions with potentially infected patients. 21 By using phones in patient rooms to provide updates, coordinating with trainees and nurses to do exams together, and having cardiac monitors visible from the doorway, PED providers can limit their exposure. Participants took this further and recommended having changes of clothes available and showers at the hospital for providers to use before going home. By being transparent about PPE supply, providing child care and mental health resources, and allowing personnel to get tested when they desire, leadership will boost confidence in the workforce and help alleviate some of the stress and anxiety felt during a prolonged pandemic. 18,39
Our study is not without its limitations. Two independent coders were used in the evaluation of the qualitative data, which may have introduced bias. However, utilizing a third coder to resolve discrepancies allowed for investigator triangulation and ensured trustworthiness. Furthermore, member checking was performed to confirm consistency and dependability of the findings. Despite only 14 PEM providers participating in this study, thematic saturation was reached. This relatively small number may not be generalizable across all PEDs. However, we were able to capture responses from institutions of varying sizes and geographic locations. Additionally, we only spoke with PEM physicians with disaster management experience who may have different perspectives than junior physicians or leaders who work at institutions that primarily care for adults and limits generalizability.
As the Delta variant of COVID-19 is spreading and future disease outbreaks are likely to occur, by collectively sharing our biggest challenges we faced as pediatric emergency centers and providing recommendations to overcoming those challenges, we may be better prepared for the next disaster.
Author contributions
All authors contributed to study design, development of data collection tools, data analysis, and manuscript writing and editing. Thomas Tanner was the primary data collector. Thomas Tanner and Esther Sampayo coded the data, and Nichole Davis was the tie breaker should there be a discrepancy. Erin Endom and Nichole Davis participated in member checking session with Thomas Tanner and Esther Sampayo.
Funding statement
Presented at American Academy of Pediatrics national conference on October 7, 2022.
References
- 1. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. Geneva, Switzerland: WHO; 2020.
- 2. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71-76. doi: 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533-534. doi: 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schwartz J, King CC, Yen MY. Protecting health care workers during the COVID-19 coronavirus outbreak—lessons from Taiwan’s SARS response. Clin Infect Dis. 2020;71(15):858-860. doi: 10.1093/cid/ciaa255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Z, Liu S, Xiang M, et al. Protecting healthcare personnel from 2019-nCoV infection risks: lessons and suggestions. Front Med. 2020; 14(2):229-231. doi: 10.1007/s11684-020-0765-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang K, Liu WL, Locatis C, Ackerman M. Mobile videoconferencing apps for telemedicine. Telemed J E Health. 2016;22(1):56-62. doi: 10.1089/tmj.2015.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Isba R, Edge R, Auerbach M, et al. COVID-19: transatlantic declines in pediatric emergency admissions. Pediatr Emerg Care . 2020. 36(11):551-553. doi: 10.1097/PEC.0000000000002260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization—a concerning trend. BMC Pediatr. 2020;20(1):427. doi: 10.1186/s12887-020-02303-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Walker DM, Tolentino VR. COVID-19: the impact on pediatric emergency care. Pediatr Emerg Med Pract. 2020;17(Suppl 6-1):1-27. [PubMed] [Google Scholar]
- 10. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ayub EM, Sampayo EM, Shah MI, Doughty CB. Prehospital providers’ perceptions on providing patient and family centered care. Prehosp Emerg Care. 2017;21(2):233-241. doi: 10.1080/10903127.2016.1241326 [DOI] [PubMed] [Google Scholar]
- 12. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Venkat A, Asher SL, Wolf L, et al. Ethical issues in the response to Ebola virus disease in United States emergency departments: a position paper of the American College of Emergency Physicians, the Emergency Nurses Association, and the Society for Academic Emergency Medicine. Acad Emerg Med. 2015;22(5):605-615. doi: 10.1111/acem.12642 [DOI] [PubMed] [Google Scholar]
- 14. Markwell A, Mitchell R, Wright AL, Brown AF. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: can lessons from Ebola virus disease be applied to the COVID-19 pandemic? Emerg Med Australas. 2020;32(3):520-524. doi: 10.1111/1742-6723.13514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Team CC-R. Coronavirus disease 2019 in children—United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):422-426. doi: 10.15585/mmwr.mm6914e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sisk B, Cull W, Harris JM, et al. National trends of cases of COVID-19 in children based on US State Health Department data. Pediatrics. 2020;146(6):e2020027425. doi: 10.1542/peds.2020-027425 [DOI] [PubMed] [Google Scholar]
- 17. DeLaroche AM, Rodean J, Aronson PL, et al. Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics. 2021;147(4):e2020039628. doi: 10.1542/peds.2020-039628. [DOI] [PubMed] [Google Scholar]
- 18. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133-2134. doi: 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- 19. Cull B, Harris M. Children and COVID-19: state data report. American Academy of Pediatrics. Published August, 12, 2021. Accessed August 16, 2021. https://downloads.aap.org/AAP/PDF/AAP%20and%20CHA%20-%20Children%20and%20COVID-19%20State%20Data%20Report%208.12%20FINAL.pdf
- 20. Auerbach MA, Abulebda K, Bona AM, et al. A national US survey of pediatric emergency department coronavirus pandemic preparedness. Pediatr Emerg Care. 2021;37(1):48-53. doi: 10.1097/PEC.0000000000002307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jain S, Fahlgren R, Giovanni J, Dowd MD. Pediatric emergency department challenges and response to COVID-19. Pediatr Ann. 2021;50(4):e172-e177. doi: 10.3928/19382359-20210318-01 [DOI] [PubMed] [Google Scholar]
- 22. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308-310. doi: 10.12788/jhm.3435 [DOI] [PubMed] [Google Scholar]
- 23. Hartford EA, Keilman A, Yoshida H, et al. Pediatric emergency department responses to COVID-19: transitioning from surge preparation to regional support. Disaster Med Public Health Prep. 2021;15(1):e22-e28. doi: 10.1017/dmp.2020.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Diskin C, Orkin J, Agarwal T, et al. The secondary consequences of the COVID-19 pandemic in hospital pediatrics. Hosp Pediatr. 2021;11(2):208-212. doi: 10.1542/hpeds.2020-002477 [DOI] [PubMed] [Google Scholar]
- 25. Turer RW, Jones I, Rosenbloom ST, et al. Electronic personal protective equipment: a strategy to protect emergency department providers in the age of COVID-19. J Am Med Inform Assoc. 2020;27(6):967-971. doi: 10.1093/jamia/ocaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Beno S, Ross C, Principi T. Coronavirus disease 2019 in the pediatric emergency department: unique considerations in preparation and response. Curr Opin Pediatr. 2021;33(3):269-274. doi: 10.1097/MOP.0000000000001010 [DOI] [PubMed] [Google Scholar]
- 27. Dharamsi A, Hayman K, Yi S, et al. Enhancing departmental preparedness for COVID-19 using rapid-cycle in-situ simulation. J Hosp Infect. 2020;105(4):604-607. doi: 10.1016/j.jhin.2020.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations; Institute of Medicine. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington (DC): National Academies Press (US); 2012. PMID: 24830057. [PubMed]
- 29. Bressan S, Buonsenso D, Farrugia R, et al. Preparedness and response to pediatric COVID-19 in European emergency departments: a survey of the REPEM and PERUKI networks. Ann Emerg Med. 2020;76(6):788-800. doi: 10.1016/j.annemergmed.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Walker DM, Tolentino VR. COVID-19: the effects on the practice of pediatric emergency medicine. Pediatr Emerg Med Pract. 2020;17(Suppl 6-3):1-15. [PubMed] [Google Scholar]
- 31. Hu NY, Castillo J, Flores-Sanchez P, et al. Perspectives on pediatric redeployment during COVID-19 from an emergency department in New York City. Pediatr Emerg Care. 2020;36(9):e541-e542. doi: 10.1097/PEC.0000000000002206 [DOI] [PubMed] [Google Scholar]
- 32. Levine DA, Fraymovich S, Platt SL. Where have all the children gone? Pediatric perspectives on COVID-19 in New York City. Ann Emerg Med. 2020;76(1):109-110. doi: 10.1016/j.annemergmed.2020.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Morgan RW, Kienzle M, Sen AI, et al. Pediatric resuscitation practices during the coronavirus disease 2019 pandemic. Pediatr Crit Care Med. 2020;21(9):e651-e660. doi: 10.1097/PCC.0000000000002512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tan RMR, Ong GY, Chong SL, et al. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37(5):252-254. doi: 10.1136/emermed-2020-209634 [DOI] [PubMed] [Google Scholar]
- 35. Parri N, Lenge M, Cantoni B, et al. COVID-19 in 17 Italian pediatric emergency departments. Pediatrics . 2020;146(6):e20201235. doi: 10.1542/peds.2020-1235 [DOI] [PubMed] [Google Scholar]
- 36. Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088-1095. doi: 10.1111/apa.15270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yasuhara J, Kuno T, Takagi H, Sumitomo N. Clinical characteristics of COVID-19 in children: a systematic review. Pediatr Pulmonol. 2020;55(10):2565-2575. doi: 10.1002/ppul.24991 [DOI] [PubMed] [Google Scholar]
- 38. He K, Stolarski A, Whang E, Kristo G. Addressing general surgery residents’ concerns in the early phase of the COVID-19 pandemic. J Surg Educ. 2020;77(4):735-738. doi: 10.1016/j.jsurg.2020.04.003 [DOI] [PMC free article] [PubMed]
- 39. Siddle J, Tolleson-Rinehart S, Brice J. Survey of emergency department staff on disaster preparedness and training for Ebola virus disease. Am J Disaster Med. 2016;11(1):5-18. doi: 10.5055/ajdm.2016.0220 [DOI] [PubMed] [Google Scholar]