Abstract
Reversible splenial injury syndrome (RESLES) is a rare clinicoradiological entity that defines a reversible lesion in the splenium of the callosum in magnetic resonance imaging.
RESLES may be of infectious iatrogenic or metabolic origin. We report 2 cases of drug induced RESLES in our training.
The presence of an isolated lesion of the corpus callosum in a context of polymedication by psychotropic drugs and the regression in less than 4 weeks suggests a toxic origin, in particular medicinal.
The pathophysiology of these reversibles lesions of the splenium of callosum is not very clear, most often it is a phenomenon of vasogenic edema that is evoked, the clinical symptoms are very varied and nonspecific, and the prognosis is generally good in the absence of underlying disorder.
Keywords: Splenial, Reversible, MRI
Introduction
Reversible splenial injury syndrome (RESES) is a rare clinicoradiological entity that defines a reversible lesion in the splenium of the corpus callosum in magnetic resonance imaging (MRI) [1].
The availability of increasingly sophisticated MRI sequences has led to a better definition of this entity, whichappears to be of favorable prognosis [2].
RESLES has many etiologies. These can include metabolic disorders, demyelinating diseases, infectious diseases, and also toxic causes [3].
Here we describe 2 patients with RESLES and conduct a systematic literature search to define the syndrome, its possible pathophysiological mechanisms, its clinical and especially radiological presentation, its etiologies, and prognosis [1].
Patients and observations
Case 1
The first case is a man aged 26 years old who has been treated for resistant Schizophrenia for 10 years and has been prescribed multiple medications. He has also developed recent unusual behavioral disorders. While doing a neurological examination, no infectious signs were detected. The autoimmunity test was negative.
To explain more, there were no fluid and electrolyte disorders or inflammatory syndrome, and the lumbar puncture (LP) was negative. This motivated the performance of a brain MRI (T1, T2 spin echo and gradient echo sequences, FLAIR, diffusion with ADC mapping, T1 sequences after injection of Gadolinium) which showed a single lesion of the Splenium of the corpus callosum, rounded, well limited, in isosignal T1, in hypersignal T2 and FLAIR, in hypersignal diffusion with ADC drop, not enhancing after injection of Gadolinium (Fig. 1).
Fig. 1.
Initial cerebral MRI: axial T2 FLAIR, diffusion, and ADC: a rounded well-limited single lesion of the splenium of the corpus callosum, hyperintense on T2 Flair and diffusion with ADC restriction. Complete disappearance of the lesion on MRI control after one month.
Psychiatric therapy involved stopping the treatment. The evolution was marked by the improvement of the clinical symptomatology and by the total disappearance of the lesion on the MRI control carried out after 1 month.
Case 2
The second case is a man aged 18 years old with no previous health related issues. He was admitted to the neurology department for a behavioral disorder. The neurological examination was without particularities. LP test returned negative. Blood tests for toxins revealed the presence of Benzodiazepines. The patient benefited from a brain MRI with weighted sequences T1, T2, FLAIR, diffusion with ADC mapping, T2*. After that, He got injected with a 3DT1 Gadolinium injection and Axial T1 sequences which showed a single rounded signal anomaly of the Splenium of the Corpus Callosum in hypersignal T2, hypersignal diffusion with low ADC, unchanged after Gadolinium injection (Fig. 2). The evolution was positive with a total disappearance of the splenium lesion on MRI control performed after one month.
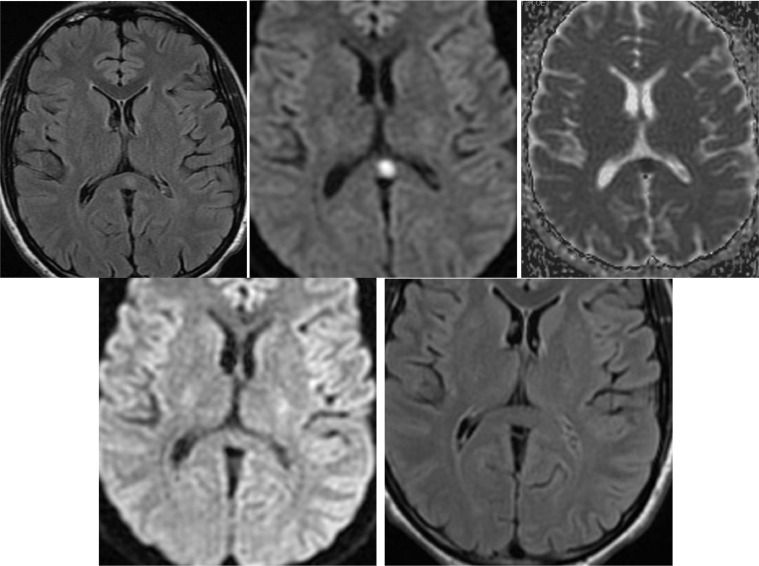
Fig. 2.
Initial cerebral MRI: axial T2, diffusion and ADC: single signal abnormality of the splenium of the corpus callosum, hyperintense on T2 and diffusion with ADC restriction. Control brain MRI after 1 month: a complete disappearance of the corpus callosum splenium's lesion.
Discussion
RESLES is a clinical condition involving transient lesions in the splenium of the corpus callosum. It was first reported by Kim and colleagues in 1999, describing a group of Epilepsy concomitant lesions of the splenium of the corpus callosum due to the anti-epileptic medication [4].
The accurate frequency of this syndrome is difficult to determine, probably underestimated, as the majority of patients do not undergo an MRI. Also, it has been estimated that it occurs in 0.7% of patients diagnosed with an epilepsy that is resistant to treatment [2].
The pathophysiology of these reversible splenium lesions of the corpus callosum is not very clear given the diversity of etiologies. It is possible that several mechanisms are responsible [3]; such as intramyelinic edema, hyponatremia, oxidative stress, autoimmune processes, inflammation, cytotoxic edema characterized by swelling of neurons, and glial cells with a reduction in extracellular space and vasogenic edema [4].
The RESLES predilection is unclear, but may be related to its relative lack of adrenergic tone, making it more exposed to hypoxic vasodilation and autoregulatory dysfunction [2].
The clinical symptoms of RESLES are unspecified and diverse, but the neurological symptoms are the most frequent. Cognitive impairment, seizures, behavioral changes, insomnia, confusion, acute urinary retention, delirium, motor deterioration, neck pain, coma, shaking, ataxia, and dysarthria. The clinical symptoms of RESLES are unspecified and diverse, but the neurological symptoms are the most frequent. Cognitive impairment, seizures, behavioral changes, insomnia, confusion, acute urinary retention, delirium, motor deterioration, neck pain, coma, shaking, ataxia, dysarthria, etc., may be experienced. Other general clinical symptoms such as headache, digestive disorders, or fever may precede or accompany this syndrome [4].
On the basis of MRI, the lesion of the corpus callosum can acquire 2 forms: a small central round or oval lesion that is isolated or extended to the anterior part of the corpus callosum and the adjacent white substance. It appears in hypersignal, T2, FLAIR, and diffusion. The quantization of ADC values has shown at the acute stage of RESLES a restriction of diffusion. On T1-weighted sequences, the lesion is in an iso- or discrete T1 hyposignal without enhancement after injection of contrast agent [4].
In about 2 weeks, the most typical MRI feature that can be noticed is a reversible restricted diffusion with either a complete disappearance of the lesion or a clear decrease without atrophy [4].
The etiologies of RESLES are very diverse and can be of infectious, metabolic, toxic, and medicinal origin [4].
The first patient has an isolated lesion of the corpus callosum in a context of polymedication by psychotropic drugs while the second patient has benzodiazepines in the blood in a context of apyrexia. Also, there is a regression in less than 4 weeks after the stopping of the treatment. This makes us conclude that the origin is drug-induced.
The medical coverage is based on treatment of the causative agent.
The recovery is positive as there is a complete disappearance of the neurological symptoms after 1 month. However, it can be negative for the patients accompanied with a loss of consciousness [4].
Conclusion
RESLES is identified by a reversible lesion in the splenium of the corpus callosum on MRI. It has variable etiologies and an excellent prognosis if it is treated quickly as it is an uncommon one.
Authors’ contribution
All authors contributed to the completion of this work.
Patient consent
The patient's parents agreed with a written informed consent to anonymously publish their boys medical informations.
Footnotes
Competing Interests: All authors declare no conflict of interest.
References
- 1.Dong et Cong, Reversible splenial lesion syndrome associated with acute mycoplasma pneumoniae‑associated encephalitis. A report of four cases and literature review, Department of Neurology, Shengjing Hospital of China Medical University, Shenyang, Liaoning, P.R. China Received October 18, 2017; Accepted June 8, 2018 [DOI] [PMC free article] [PubMed]
- 2.Garcia-Monco J.C., Cortina I.E., Ferreira E., Martínez A., Ruiz L., Cabrera A., et al. Reversible splenial lesion syndrome (RESLES) Neuroimaging. 2011;21:e1–e14. doi: 10.1111/j.1552-6569.2008.00279.x. [DOI] [PubMed] [Google Scholar]
- 3.Debien V., Dalmas M.C., Taquet M.C., Maire C., Weibel S., Dietemann J.L., et al. Le syndrome de lésion réversible du corps calleux (RESLES) Rev Méd Intern. 2015;36(Supplement 2):A195–A196. [Google Scholar]
- 4.Tetsuka S. Reversible lesion in the splenium of the corpus callosum. Brain Behav. 2019;9:e01440. doi: 10.1002/brb3.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]