Abstract
Members of the Klebsiella pneumoniae species complex frequently colonize the gut and colonization is associated with subsequent infection. To identify genes associated with progression from colonization to infection, we undertook a case-control comparative genomics study. Concordant cases (N = 85), where colonizing and invasive isolates were identical strain types, were matched to asymptomatically colonizing controls (N = 160). Thirty-seven genes are associated with infection, 27 of which remain significant following adjustment for patient variables and bacterial phylogeny. Infection-associated genes are not previously characterized virulence factors, but instead a diverse group of stress resistance, regulatory and antibiotic resistance genes, despite careful adjustment for antibiotic exposure. Many genes are plasmid borne, and for some, the relationship with infection is mediated by gut dominance. Five genes were validated in a geographically-independent cohort of colonized patients. This study identifies several genes reproducibly associated with progression to infection in patients colonized by diverse Klebsiella.
Subject terms: Bacterial genetics, Pathogens, Bacterial genomics, Comparative genomics
Patient variables, such as comorbidities, partially explain which patients will progress to Klebsiella infection, with colonization of the gut acting as a reservoir. Little is known, however, regarding Klebsiella genes that may increase risk of disease in colonized individuals. Here, authors conduct a comparative genomics study to identify genes associated with progression from colonisation to infection.
Introduction
The Klebsiella pneumoniae species complex (hereby referred to as Klebsiella) is comprised of several species capable of causing severe infections, including bacteremia, pneumonia, and urinary tract infection (UTI). The member species are K. pneumoniae, K. variicola, K. quasipneumoniae, K. quasivariicola sp. nov.1, and K. africana2, which are genetically distinct but often clinically indistinguishable (reviewed in3). Klebsiella infections are a serious public health concern because they are a leading cause of healthcare-associated infections4, can harbor multiple antimicrobial resistance (AMR) determinants, and can be hypervirulent. Antimicrobial resistant Klebsiella complicate disease treatment, leading to high mortality and healthcare costs whereas hypervirulent Klebsiella cause unique clinical manifestations such as pyogenic liver abscess and meningitis3,5,6. Klebsiella colonization is the primary risk factor for disease7,8, where the gut acts as a reservoir for disease-causing Klebsiella strains7,9. Patient variables, including comorbidities and baseline laboratory values, partially explain which patients will progress to infection10. Furthermore, the high relative abundance of Klebsiella colonizing the gut is associated with an increased risk of infection in colonized patients11. For hypervirulent Klebsiella, the genes associated with their unique presentations have been well-defined by molecular epidemiology and experimental studies (reviewed in12); however, little is known about the Klebsiella genes contained by non-hypervirulent strains, including multi-drug resistant (MDR) strains, that increase the risk of disease in colonized patients more broadly. Given that most infections are caused by non-hypervirulent strains13, more data concerning the genetic determinants of infection are necessary for predicting, diagnosing, and experimentally evaluating these strains.
In general, the ability of bacteria to progress from colonization to infection is dependent on the immune status of the host, environmental and iatrogenic exposures such as antimicrobials, and the virulence potential of the strain. Known Klebsiella virulence determinants are found in both the core genome, which are ~1700 genes present in >95% of all sequenced strains, and the accessory genome, which are genes that vary among sequenced strains14. The overall Klebsiella accessory genome is currently estimated to include >100,000 unique genes3. With an average of >5000 genes per genome, thousands of genes vary between strains. The size of the Klebsiella accessory genome provides a unique opportunity to perform comparative genomics studies to understand pathogenesis. Comparative genomics approaches are used to understand hospital outbreaks15,16, identify in-host adaptation17, and infer conserved virulence determinants or pathways. The latter approach has been used to interrogate the pathogenicity of numerous bacterial pathogens, such as Pseudomonas aeruginosa18, Streptococcus pneumoniae19, Escherichia coli20, and invasive non-typhoidal Salmonella enterica spp.21. Previously, we used a comparative genomics approach to identify Klebsiella factors associated with infection in a small, hospital-wide cohort of Klebsiella-colonized patients22. Two infection-associated factors identified in this study, the psicose utilization locus and ter operon, were experimentally validated and characterized22,23, confirming the value of this approach for understanding Klebsiella pathogenesis.
The strong association between gut colonization and Klebsiella disease indicates a potential point of intervention to prevent infection in the most at-risk patients, such as those in intensive care and hematology/oncology units. If patients with risk factors for infection are colonized by high-risk Klebsiella isolates, early detection and intervention may prevent disease. The development of these approaches is likely to be critical as therapeutic options become limited due to rising antimicrobial resistance. We previously performed a large cohort study of Klebsiella-colonized patients in the intensive care and hematology/oncology units and identified patient variables associated with subsequent infection10. Additionally, we identified an association between gut dominance by Klebsiella and infection, even after adjustment for the patient variables11. Here, we aimed to rigorously identify Klebsiella genes that are associated with disease in colonized patients through whole-genome sequencing (WGS) in a nested case-control study from a cohort of over 1900 colonized patients. This approach differed from other comparative genomics studies in that it focused on concordant infections (e.g., same colonizing and infecting isolate) after infection, directly compared cases of infection to well-matched controls from the same patient population and incorporated careful adjustment with patient variables associated with infection. Through this approach, we identified 27 genes associated with infection in colonized patients. We identified which genes may act through gut dominance, and determined that many genes were found on large, conjugative plasmids. Finally, we demonstrate that five of these genes are associated with infection in a geographically-independent cohort of intensive care patients colonized with Klebsiella.
Results
Selection of Klebsiella for WGS and description of the case-control study
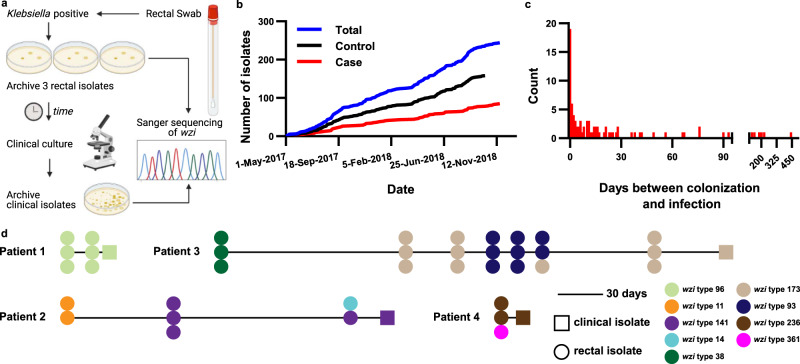
A nested case-control study was performed using a cohort of 1978 Klebsiella colonized, intensive care, and hematology/oncology patients at a single academic medical center in Michigan, USA10. Over the course of this study patient rectal swabs were screened for the presence of Klebsiella. If a patient was colonized with Klebsiella, up to three rectal isolates were banked, and the patient was enrolled in the study. Subsequent rectal swab isolates and clinical culture Klebsiella isolates (blood, respiratory, urinary, and other) were also banked (Fig. 1a). Cases of infection were considered for inclusion based on chart review using strict clinical definitions10. To facilitate a rigorous comparative genomics approach, Sanger sequencing of the wzi gene24 was used to screen for concordance between the clinical culture isolate and a preceding colonizing rectal isolate from the same patient (Fig. 1a). Cases and controls accumulated at a similar rate throughout the enrollment period (Fig. 1b). The median time between detection of Klebsiella colonization and subsequent infection was 10 days (range = 0–443 days, Fig. 1c). In some instances, the progression from colonization to infection was simple, wherein a single wzi type was detected in all colonizing Klebsiella isolates and the subsequent infecting isolate (Fig. 1d, “Patient 1”). In other instances, the infection trajectory was more complicated, wherein some patients exhibited single or multiple strain replacements in the gut prior to infection (Fig. 1d, “Patient 2” and “Patient 3”), or mixed colonization where only one colonizing isolate caused the subsequent infection (Fig. 1d, “Patient 2” and “Patient 4”). Collectively, these data indicate concordant infections are detectable in colonized patients in the context of highly dynamic Klebsiella populations.
Fig. 1. Description of Klebsiella isolate collection.
a Schematic representation of Klebsiella isolate collection and wzi-based concordance testing for WGS selection. b Rectal isolate selected for WGS collection dates stratified by case status. c Histogram of the number of days between identification of a rectal Klebsiella isolate concordant with the clinical isolate from the same patient. d Trace diagrams of wzi typing in Klebsiella colonizing and infecting isolates in infected patients.
In total, 85 cases of infection with an identical wzi type to a colonizing rectal isolate (cases) were selected for WGS, including 39 bloodstream infections, 23 urinary tract infections, 19 pneumonias, and 4 other sites of infection (including two cases of cholecystitis, one case of empyema, and one case of ecthyma). Based on antibiotic susceptibility data from medical records, 44 of 85 (51.8%) of the clinical isolates from cases were pan-sensitive apart from intrinsic ampicillin resistance. The most common AMR phenotypes were resistance to first- and second-generation cephalosporins, the combinatorial β-lactam/β-lactamase-inhibitors ampicillin-sulbactam and piperacillin-tazobactam, and trimethoprim-sulfamethoxazole (Supplementary Fig. S1). Cases were matched to two colonized controls (who remained asymptomatic) based on sex, age, and date of rectal swab collection. In addition, controls had the same type of clinical culture collected as their corresponding case, but with no cultivatable bacteria. Two strata included only a single control because of the inability to find an appropriate match, and an additional 8 controls were removed from the study following WGS based on species classification outside of Klebsiella. In the final case-control design, 85 cases, including the clinical and rectal isolates, and 160 control rectal isolates were evaluated (Table 1).
Table 1.
Patient demographics and select baseline characteristics
| Patient variable | Case | Control | Odds ratio (OR)* | 95% CI | Fisher P-value | |
|---|---|---|---|---|---|---|
| (N = 85) | (N = 160) | |||||
| Sex | Female | 40 (47.1%) | 76 (47.5%) | |||
| Male | 45 (52.9%) | 81 (50.6%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| Median age (range) | 60 (83–25) | 59 (85–27) | ||||
| Infection site | Blood | 39 (45.9%) | ||||
| Respiratory | 19 (22.4%) | |||||
| Urine | 23 (27.1%) | |||||
| Other | 4 (4.71%) | |||||
| Mean weighted Elixhauser score (±SD) | 22.2 ± 11.6 | 19.7 ± 11.9 | 1.02 | 0.994 to 1.04 | 0.127 | |
| Depression | Yes | 30 (35.3%) | 44 (27.5%) | 1.31 | 0.761 to 2.26 | 0.327 |
| No | 55 (64.7%) | 113 (70.6%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| Prior diuretics | Yes | 30 (35.3%) | 38 (23.8%) | 1.69 | 0.905 to 3.05 | 0.101 |
| No | 55 (64.7%) | 119 (74.4%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| Prior Vitamin D | Yes | 18 (21.2%) | 19 (11.8%) | 1.66 | 0.972 to 4.44 | 0.0591 |
| No | 67 (78.8%) | 138 (86.3%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| Prior pressors/inotrope | Yes | 20 (23.5%) | 14 (8.75%) | 3.06 | 1.40 to 6.68 | 0.00502 |
| No | 65 (76.6%) | 143 (89.4%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| High-risk antibiotics | Yes | 30 (35.3%) | 32 (20.0%) | 2.21 | 1.18 to 4.14 | 0.013 |
| No | 55 (64.7%) | 125 (78.1%) | ||||
| Missing | 0 (0.0%) | 3 (1.88%) | ||||
| Albumin | <2.5 g/dL | 35 (41.2%) | 34 (21.3%) | 2.86 | 1.49 to 5.48 | 0.00157 |
| ≥2.5 g/dL | 47 (55.3%) | 116 (72.5%) | ||||
| Missing | 3 (3.53%) | 10 (6.25%) | ||||
*Two-sided test. No adjustments were made for multiple comparisons. OR for sex was incalculable due to use of sex as a matching variable.
Bold text indicates significant results (P-value ≤ 0.01 after adjustment for clinical variables).
Description of sequenced Klebsiella isolates
Following the determination of isolates for WGS, genomic DNA was extracted from all Klebsiella isolates and subjected to Illumina sequencing (Supplementary Data 1). Assembled genomes were generally of high quality, wherein the median number of contigs was 110.5 (range = 43–876 contigs) and the median N50 was 459,591 bp (range = 147,972–3,285,432 bp). All genomes were of expected length, wherein the median genome size was 5.50 Kb (range = 5.06–6.26 Kb). Sequencing quality was similar between rectal case and control isolates, which were used for most subsequent analyses (Supplementary Fig. S2). As expected, species assignment based on WGS included the three most common members of the Klebsiella pneumoniae species complex (K. pneumoniae, K. variicola, K. quasipneumoniae). K. pneumoniae, K. variicola, and K. quasipneumoniae were evenly distributed amongst the four sites of infection and control rectal swabs (Supplementary Fig. S3a). Case and control rectal isolates within a stratum may be the same or different species, as reflected in either high (100–80%) or low (60–30%) overall nucleotide identity (Supplementary Fig. S3b). For the rectal and clinical isolate of a given case of infection, matching wzi types were highly predictive of overall nucleotide identity (median % nucleotide identity = 99.65%, range = 95.04–99.88%, Supplementary Fig. S3c). The time between detection of Klebsiella colonization and subsequent infection was negatively correlated with sequence similarity; however, the effect was minimal (r2 = 0.06, Supplementary Fig. S3d). Interestingly, instances of lower nucleotide identity similarity (<98%) between the rectal and clinical isolates from concordant cases of infection appeared to be due to large genomic losses or additions (Supplementary Fig. S3e), which may be driven by plasmids or other mobile genetic elements (MGEs). Indeed, these case clinical and rectal isolate pairs displayed differences in the number of annotations that corresponded to differences in genome size (Supplementary Fig. S3f–g).
To confirm concordance between case clinical and rectal isolates, wzi strain typing was performed from the assembled genomes. All wzi types matched results from Sanger sequencing, and construction of a wzi approximately-maximum-likelihood tree revealed a total of 147 unique wzi types identified (Supplementary Fig. S4). Then, multi-locus sequence typing was performed across all isolates. One-hundred thirty-one unique sequence types (STs) were identified, and all case rectal and case clinical STs were identical. Rarefaction of STs indicated that cases and controls were equally rich (Supplementary Fig. S5). ST253 was the most abundant ST but still low frequency (10/245 rectal isolates, 4.08%), and 44 rectal isolates were non-typable (44/245, 17.96%). Overall, hypervirulent clonal groups (CGs)25 were rare, comprising 2.35% of cases and 1.35% of controls. Only two isolates of hypervirulent ST23 were identified, and only one caused an infection. MDR CGs25, frequently containing extended-spectrum β-lactamases, carbapenemases, or both, were more common, representing 18.8% of cases and 9.38% of controls. These included 1 ST11, 4 ST14, 3 ST15, 1 ST16, 3 ST17, 5 ST37, 2 ST147, 1 ST152, 1 ST258, and 3 ST307. 85.7% (210/245) of the isolates in our collection were from non-hypervirulent, non-MDR CGs. Combined, MDR CGs were significantly associated with case status (odds ratio = 2.24, 95% C.I. 1.03 to 4.93, Fisher P = 0.043). Construction of a core genome phylogeny demonstrated the presence of three Klebsiella species within our cohort and multiple lineages across colonizing and invasive isolates of each species (Supplementary Data 1; Fig. 2a). Together, these data indicate that sequenced Klebsiella isolates were highly diverse, without a dominant hypervirulent or MDR CG within the population.
Fig. 2. Klebsiella rectal isolates are highly diverse and infection-associated genes span that diversity.
a Core genome phylogeny tree of sequenced Klebsiella rectal isolates. The inner ring indicates the species, the middle ring indicates a clonal group of concern (hypervirulent [Hv] CG: clonal groups 23, 25, 380; MDR CG: 14/15, 17/20, 37, 147, 258, 307), and the outer ring indicates site of infection for concordant clinical isolate. b Heatmap of infection-associated gene presence/absence organized vertically by core genome phylogeny and horizontally by the strength of association (Odds ratio) between gene presence and infection following adjustment for patient variables.
To enable the identification of infection-associated genes in rectal samples, we assembled a pangenome (Supplementary Data 2). The rectal isolate pangenome consisted of 26,089 total annotations. The core genome (genes present in ≥95% genomes) was comprised of 3921 genes, and the accessory genome (genes present in <95% genomes) consisted of 22,168 genes (Supplementary Fig. S6a). To assess the similarity of the accessory genome between Klebsiella isolates in our collection, pairwise Jaccard distances were calculated after excluding the core genome and summarized as a mean for each isolate (244 pairwise comparisons per isolate). Interestingly, the mean pairwise Jaccard distance for all rectal isolates was 0.73 ± 0.04, indicating that the accessory genome of each isolate was highly dissimilar from other isolates. No differences were observed between mean pairwise Jaccard distances for cases and controls (Supplementary Fig. S6b). Overall, the cohort of Klebsiella isolates exhibited high pangenome diversity.
Genes associated with Klebsiella infection
To identify genes in the accessory genome associated with infection we used Scoary, collapsing linked genes that displayed identical presence/absence patterns across all sequenced isolates (e.g., organized in operons, linked to MGEs, etc.) into units and comparing unit frequencies between cases and controls (Supplementary Data 3)26. Thirty-seven genes across 34 units were significantly associated with infection (Q-value ≤ 0.2, 2166 tests). Two units contained genes with identical presence/absence patterns (group_5875-tehA_2-group_10494 and group_5455-sul2); the remaining units contained a single gene. Overall, 36 genes were associated with cases, one was associated with controls (Table 2).
Table 2.
Genes associated with patient case status
| Gene | Annotation | Case frequency | Control frequency | Unadjusted | Adjusted for clinical variables | Mediation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratio | P-value | Q-value** | Odds ratio | P-value** | Direct β | Direct P-value** | Indirect β | Indirect P-value** | ||||
| aac(6')-Ib-cr5 | fluoroquinolone-acetylating aminoglycoside 6'-N-acetyltransferase AAC(6')-Ib-cr5 | 0.176 | 0.006 | 30.68 | 0.0011 | 0.00131 | 52.41 | 0.0003 | 3.0601 | 0.0045 | 0.086 | 0.01 |
| blaOXA-1 | oxacillin-hydrolyzing class D β-lactamase OXA-1 | 0.153 | 0.006 | 25.54 | 0.002 | 0.0053 | 49.29 | 0.0003 | 2.9698 | 0.0064 | 0.077 | 0.03 |
| blaCTX-M-15 | class A extended-spectrum β-lactamase CTX-M-15 | 0.165 | 0.013 | 13.94 | 0.0007 | 0.0053 | 19.17 | 0.0004 | 2.3386 | 0.004 | 0.047 | 0.1567 |
| group_13461 | IS1380 family transposase ISEcp1 | 0.165 | 0.013 | 13.94 | 0.0007 | 0.0053 | 18.69 | 0.0003 | 2.482 | 0.0022 | 0.019 | 0.5833 |
| group_13458 | hypothetical protein | 0.141 | 0.013 | 11.46 | 0.0018 | 0.01959 | 17.57 | 0.0006 | 2.0832 | 0.0112 | 0.034 | 0.3483 |
| group_13460 | hypothetical protein | 0.153 | 0.013 | 12.69 | 0.0011 | 0.01065 | 16.73 | 0.0005 | 2.3118 | 0.0047 | 0.024 | 0.5217 |
| group_13437 | hypothetical protein | 0.176 | 0.031 | 5.97 | 0.001 | 0.05505 | 7.28 | 0.0014 | 1.6137 | 0.0054 | 0.005 | 0.875 |
| group_5875-tehA_2-group_10494* | HTH-type transcriptional regulatory protein GabR - tellurite-resistance protein TehA - hypothetical protein | 0.129 | 0.025 | 5.65 | 0.004 | 0.1908 | 7.09 | 0.0029 | 1.8251 | 0.0053 | 0.007 | 0.8383 |
| tnpR | transposon Tn3 resolvase | 0.176 | 0.031 | 5.97 | 0.001 | 0.05505 | 6.24 | 0.0017 | 1.6379 | 0.0054 | 0.023 | 0.45 |
| blaTEM-1 | class A broad-spectrum β-lactamase TEM-1 | 0.212 | 0.038 | 6.28 | 0.0002 | 0.01236 | 5.46 | 0.0009 | 1.6623 | 0.0021 | 0.035 | 0.1783 |
| group_9575 | tyrosine recombinase XerC | 0.259 | 0.056 | 5.39 | 0.0001 | 0.0053 | 4.72 | 0.0019 | 1.3993 | 0.0044 | 0.048 | 0.05 |
| group_13467 | IS6 family transposase IS6100 | 0.224 | 0.044 | 5.75 | 0.0002 | 0.01093 | 4.58 | 0.0026 | 1.5338 | 0.003 | 0.023 | 0.4017 |
| group_5455-sul2* | IS91 family transposase - sulfonamide-resistant dihydropteroate synthase Sul2 | 0.129 | 0.025 | 5.07 | 0.0077 | 0.1908 | 4.52 | 0.0258 | 2.0214 | 0.0053 | −0.033 | 0.3617 |
| group_13965 | hypothetical protein | 0.153 | 0.038 | 4.11 | 0.0066 | 0.16685 | 3.59 | 0.0264 | 1.0196 | 0.0806 | 0.074 | 0.01 |
| group_9537 | hypothetical protein | 0.235 | 0.081 | 3.71 | 0.0009 | 0.13482 | 3.3 | 0.0035 | 1.0141 | 0.0216 | 0.049 | 0.025 |
| group_13443 | hypothetical protein | 0.224 | 0.075 | 3.81 | 0.001 | 0.16685 | 3.23 | 0.005 | 1.0762 | 0.0178 | 0.06 | 0.0083 |
| group_7606 | hypothetical protein | 0.141 | 0.025 | 6.26 | 0.0021 | 0.10991 | 3.07 | 0.0916 | 1.106 | 0.0975 | 0.097 | 0.0001 |
| dgcE | hypothetical protein | 0.341 | 0.138 | 3.37 | 0.0003 | 0.07663 | 3.06 | 0.0016 | 0.9197 | 0.0133 | 0.048 | 0.0083 |
| aqpZ_2 | aquaporin Z | 0.247 | 0.094 | 3.96 | 0.0005 | 0.16685 | 2.97 | 0.0085 | 0.923 | 0.0385 | 0.074 | 0.0001 |
| group_2409 | ISL3 family transposase ISEc38 | 0.259 | 0.106 | 3.07 | 0.002 | 0.1908 | 2.67 | 0.0083 | 0.803 | 0.0487 | 0.05 | 0.01 |
| pdeC_2 | putative cyclic di-GMP phosphodiesterase PdeC | 0.365 | 0.169 | 2.88 | 0.0008 | 0.10991 | 2.66 | 0.0026 | 0.7709 | 0.0296 | 0.041 | 0.015 |
| sul1 | sulfonamide-resistant dihydropteroate synthase Sul1 | 0.141 | 0.031 | 4.97 | 0.0037 | 0.17478 | 2.64 | 0.0939 | 1.102 | 0.0994 | 0.12 | 0.0001 |
| qacEΔ1 | quaternary ammonium compound efflux SMR transporter QacE Δ 1 | 0.153 | 0.031 | 5.46 | 0.0019 | 0.12853 | 2.63 | 0.1011 | 1.1732 | 0.0745 | 0.107 | 0.0001 |
| arsD_1 | arsenical resistance operon trans-acting repressor ArsD | 0.318 | 0.144 | 3.19 | 0.0006 | 0.17478 | 2.62 | 0.0043 | 0.7263 | 0.0563 | 0.068 | 0.0001 |
| group_774 | hypothetical protein | 0.459 | 0.25 | 2.55 | 0.0013 | 0.1391 | 2.55 | 0.0016 | 0.8601 | 0.0088 | 0.042 | 0.0033 |
| group_7231 | hypothetical protein | 0.306 | 0.138 | 2.69 | 0.0032 | 0.16685 | 2.54 | 0.0071 | 0.7807 | 0.0373 | 0.026 | 0.1733 |
| group_9530 | hypothetical protein | 0.459 | 0.238 | 2.64 | 0.0009 | 0.08496 | 2.38 | 0.0037 | 0.8449 | 0.0094 | 0.015 | 0.3533 |
| ltrA | hypothetical protein | 0.424 | 0.225 | 2.57 | 0.0013 | 0.16683 | 2.33 | 0.0051 | 0.7495 | 0.0229 | 0.037 | 0.015 |
| group_9528 | hypothetical protein | 0.353 | 0.163 | 2.87 | 0.001 | 0.12853 | 2.31 | 0.0134 | 0.7418 | 0.0384 | 0.032 | 0.0917 |
| group_622 | hypothetical protein | 0.482 | 0.269 | 2.71 | 0.0006 | 0.12566 | 2.24 | 0.0063 | 0.9086 | 0.0049 | 0.015 | 0.3683 |
| group_4187 | Antirestriction protein KlcA | 0.424 | 0.219 | 2.54 | 0.0017 | 0.12566 | 2.24 | 0.0092 | 0.7747 | 0.0191 | 0.021 | 0.1983 |
| umuD_2 | Protein UmuD | 0.6 | 0.369 | 2.42 | 0.0016 | 0.10991 | 2.1 | 0.0114 | 0.8272 | 0.0098 | 0.006 | 0.7 |
| umuC_2 | Protein UmuC | 0.682 | 0.456 | 2.52 | 0.0012 | 0.10991 | 2.09 | 0.0141 | 0.8239 | 0.0107 | 0.006 | 0.71 |
| group_2513 | hypothetical protein | 0.071 | 0.225 | 0.26 | 0.0038 | 0.16685 | 0.25 | 0.0031 | −1.2577 | 0.0119 | −0.02 | 0.3617 |
*Loci have identical presence/absence patterns across all sequenced isolates and are clustered for analysis.
**Bold text indicates significant results (unadjusted Q-value ≤ 0.2, P-value ≤ 0.01 after adjustment for clinical variables, and direct and/or indirect effect P-value ≤ 0.01).
To control for patient variables in our comparative genomics analysis, we leveraged a previously constructed multivariate model for infection risk in the larger cohort from which this nested case-control study was derived. This model was comprised of mean weighted Elixhauser comorbidity score, depression, prior diuretic use, vitamin D use, pressors/inotrope use, high-risk antibiotic use, and low albumin. Prior medication use was defined as >48 h but <90 days prior to the colonizing swab and albumin was measured within 48 h of the colonizing swab10. High-risk antibiotics, based on their impact on indigenous gut microbiota, were defined as β-lactam/β-lactamase inhibitor combinations, carbapenems, third- and fourth-generation cephalosporins, fluoroquinolones, clindamycin, and oral vancomycin27. Consistent with the explanatory value of these variables in the overall cohort, the variables used for adjustment trended towards or were significantly associated with infection in the nested case-control study (Table 1). We then used inverse probability of treatment weighting to adjust for these variables in measuring the association of each gene with the outcome of infection.
Following adjustment for clinical variables including comorbidities and antibiotic exposure, 28 of 37 genes remained significantly associated with infection (P-value ≤ 0.01; Table 2, Fig. 2b). These 28 infection-associated genes fell into four categories. First, many infection-associated genes encode AMR proteins even after correction for exposure to high-risk antibiotics. These included aac(6')-Ib-cr5, encoding an aminoglycoside acetyltransferase that also has activity against fluoroquinolones28, and blaOXA-1, blaCTX-M-15, blaTEM-1 encoding broad-spectrum β-lactamases. Second, several infection-associated genes have predicted protein functions that may alter the physiology of the bacteria directly. These include the predicted aquaporin gene aqpZ_2, tellurite-resistance gene tehA_2, arsenate resistance gene arsD_1, and diguanylate cyclase gene dgcE. Third, certain MGEs and plasmid maintenance genes were associated with infection (e.g., IS1380 family transposase ISEcp1, Transposon Tn3 resolvase, IS6 family transposase IS6100, umuDC_2). The remainder of infection-associated genes encode hypothetical proteins. Interestingly, certain genes were highly associated with one another, suggesting the presence of linked genes that may be acquired simultaneously through horizontal gene transfer (HGT) events (Supplementary Fig. S7).
None of the Klebsiella genes associated with infection encoded known virulence factors. To directly assess the association of known virulence genes with infection, we used the Kleborate genotyping tool, which is an in silico platform for rapid genotyping of Klebsiella genomes (Supplementary Data 4)25. Consistent with the paucity of hypervirulent STs, most well-characterized Klebsiella virulence factors were rare in our dataset, including salmochelin (iro), aerobactin (iuc), and colibactin (clb) synthesis loci, and hypermucoviscosity regulators RmpA/A2 (Table 3). The yersiniabactin (ybt) synthesis locus was more frequent overall, and in cases versus controls, but was not associated with infection (odds ratio = 1.7, P = 0.144). Correspondingly, the virulence score, which is a composite metric of the virulence loci listed above, was not significantly different between cases and controls (Case virulence score = 0.294 ± 0.784, Control virulence score = 0.163 ± 0.513, P = 0.115, Student’s t-test). Even when assessed directly and after controlling for clinical variables, canonical virulence factors are not associated with infection in this group of colonized, intensive care patients.
Table 3.
Klebsiella genotype association with infection
| Genotype | Case frequency | Control frequency | Unadjusted | Adjusted for clinical variables | ||
|---|---|---|---|---|---|---|
| Odds ratio | P-value | Odds ratio | P-value | |||
| Virulence determinants | ||||||
| ybt | 0.207 | 0.133 | 1.7 | 0.144 | 1.78 | 0.155 |
| col | 0.024 | 0.007 | 3.72 | 0.286 | 0.629 | 0.709 |
| iuc | 0.024 | 0.007 | 3.72 | 0.286 | 0.436 | 0.507 |
| iro | 0.012 | 0.007 | 1.84 | 0.668 | 0.476 | 0.602 |
| rmpA | 0.024 | 0.007 | 3.72 | 0.286 | 0.436 | 0.507 |
| rmpA2 | 0.012 | 0.007 | 1.84 | 0.668 | 0.937 | 0.964 |
| AMR determinants* | ||||||
| AGly acquired (aminoglycosides) | 0.268 | 0.067 | 5.133 | 7.01E-05 | 3.77 | 0.00427 |
| Flq (fluoroquinolones) | 0.220 | 0.040 | 6.75 | 1.14E-04 | 6.69 | 0.000507 |
| MLS (macrolides) | 0.098 | 0.013 | 8.0 | 0.010 | 6.41 | 0.0649 |
| Phe (phenicols) | 0.171 | 0.027 | 7.51 | 0.001 | 6.35 | 0.00332 |
| Rif (rifampin) | 0.012 | 0.000 | N/A | N/A | N/A | N/A |
| Sul (sulfonamides) | 0.268 | 0.047 | 7.49 | 1.22E-05 | 5.19 | 0.00226 |
| Tet (tetracyclines) | 0.183 | 0.100 | 2.01 | 0.076 | 1.88 | 0.128 |
| Tmt (trimethoprim) | 0.244 | 0.053 | 5.73 | 8.86E-05 | 4.28 | 0.00285 |
| Omp mutation | 0.037 | 0.020 | 1.86 | 0.453 | 1.55 | 0.676 |
| Bla (β-lactamase that is “other”) | 0.573 | 0.520 | 1.24 | 0.438 | 1.27 | 0.379 |
| Bla Carb (carbapenemase) | 0.061 | 0.007 | 9.68 | 0.040 | 36.2 | 0.00151 |
| Bla ESBL (extended-spectrum β-lactamases) | 0.207 | 0.087 | 2.76 | 0.011 | 2.94 | 0.0116 |
| Bla broad (broad-spectrum β-lactamases) | 0.354 | 0.347 | 1.03 | 0.915 | 0.902 | 0.734 |
| Bla broad inhR (broad-spectrum β-lactamases with resistance to β-lactamase inhibitors) | 0.110 | 0.107 | 1.03 | 0.942 | 1.05 | 0.922 |
*Kleborate25 predicted AMR genotypes absent in our dataset are not shown.
Bold text indicates significant results (P-value ≤ 0.01).
Next, we aimed to adjust for the effects of phylogeny on the association between each group of genes and infection. We used treeWAS to test for the confounding potential of clonality and recombination in the population structure by simulating a null genetic dataset across the phylogenetic tree29. The output of treeWAS is three complimentary scores: The Terminal score counts the four possible combinations of genotype and phenotype without regard to phylogeny, whereas the Simultaneous and Subsequent scores account for population structure29 in measuring the association between genotype and phenotype. Of the 28 infection-associated genes after adjustment (Table 2), 23 genes were also significant (P ≤ 0.01) by the Terminal score; group_774, group_9530, ltrA, group_622, group_4187, and group_2513 were not (Supplementary Fig. S8, Supplementary Table 1). Other than group_2513, 27 genes were significantly associated with infection by either the Simultaneous or Subsequent score, or both (Supplementary Fig. S8). For subsequent analyses, we focused on these 27 genes associated with infection both after adjustment for clinical variables and after at least one test of independence from bacterial phylogeny.
AMR genes are associated with infection independent of prior exposure to antibiotics
The identification of multiple AMR genes associated with infection after adjustment for exposure to high-risk antibiotics was unexpected. To investigate the association between AMR genes and infection further, we used two independent approaches. First, we identified classes of AMR genes as defined by Kleborate25 in our strain set. Overall, the prevalence of many of these AMR determinants was low (<25%). Consistent with results from Scoary, AMR determinants for aminoglycosides, fluoroquinolones, phenicols, sulfonamides, and trimethoprim were significantly associated with infection after adjustment. In addition, carbapenamase genes were also significantly associated with infection, and extended-spectrum β-lactamases (ESBL) approached significance (P = 0.011; Table 3). Notably, one case rectal isolate (Kp10372, Supplementary Data 4) displayed a hypervirulent (ST23, ybt+, col+, iuc+, rmpA/A2+), MDR (KPC-3) genotype. The Kleborate Resistance Score25 was not significantly different between cases and controls (Case resistance score = 0.2 ± 0.483, Control resistance score = 0.163 ± 0.418, P = 0.528, Student’s t-test); however, this score is heavily weighted by the presence of carbapenemases in the context of colistin resistance, the latter of which was not detected in our dataset25. Next, we assessed phenotypic resistance across four antibiotic classes, using an agar dilution method with antibiotic concentrations at the Clinical & Laboratory Standards Institute breakpoint for resistance30. Screen results were confirmed for 12 randomly selected Klebsiella isolates using the broth microdilution method. Overall, phenotypic AMR rates were low (<25%). Phenotypic resistance to chloramphenicol and gentamicin did not correlate well to genotypic resistance and was not associated with infection (Supplementary Table 2). Conversely, phenotypic resistance to ciprofloxacin, cefazolin, cefuroxime, and cefepime was associated with infection following adjustment for clinical variables (Supplementary Table 2).
Given the consistent association of AMR genes and phenotypes despite adjustment for exposure to high-risk antibiotics as a group, we evaluated whether their association with infection is due to exposure to specific cognate antibiotics. For example, aac(6')-Ib-cr5 may be associated with exposure to aminoglycosides, a class that was not included in adjustment. Interestingly, prior antibiotic exposure by specific classes was not associated with the presence of most infection-associated genes in unadjusted analysis (Supplementary Fig. S7). Next, we explicitly adjusted for each class of antibiotic, in addition to clinical variables by IPTW, and assessed the association of each gene with infection. Even after individual adjustment for 18 classes of antibiotics (no patients had a prior exposure to daptomycin or polymyxin), all AMR genes remained significantly associated with infection (Supplementary Fig. S9). These data suggest an alternative explanation exists for the association between infection and AMR genes.
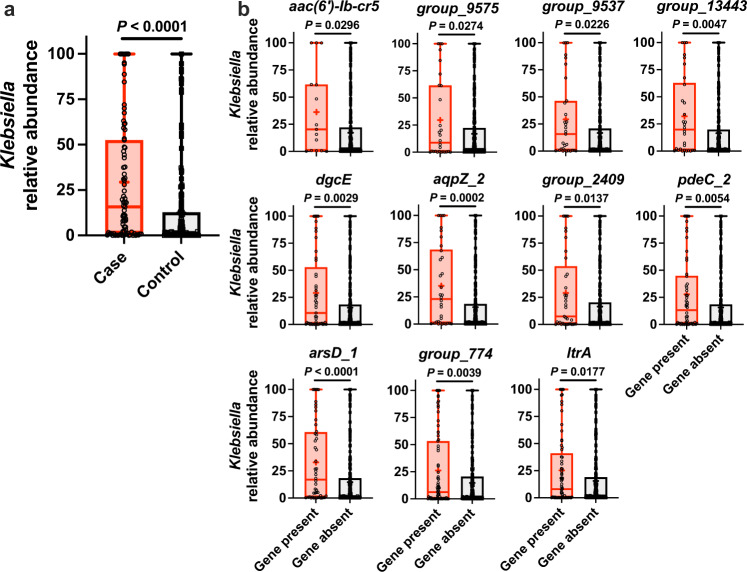
Gut relative abundance mediates association between certain genes and Klebsiella infection
We previously identified that high Klebsiella relative abundance in the gut is associated with infection11, and that genes associated with infection can enhance fitness in the gut23. Therefore, we hypothesized that the Klebsiella genes associated with infection may act by enabling gut dominance that in turn increases the risk of infection. Klebsiella relative abundance measurements from the rectal swabs most proximal to infection for cases and matched controls were available for 233 of 245 sequenced rectal isolates11. Reanalysis of these data was consistent with that of the original study, wherein cases had significantly higher Klebsiella relative abundance in the gut compared to controls (Fig. 3a). Mean relative abundance was not significantly different between species (Supplementary Fig. S10a). Abundance was higher in patients exposed to high-risk antibiotics, and when stratified by antibiotics exposure the abundance in cases was significantly higher than controls (Supplementary Fig. S10b, c). Analysis of Klebsiella gut relative abundance based on gene presence/absence (rather than case status) identified 11 of the 27 infection-associated genes associated with increased relative abundance (Fig. 3b), whereas the other 16 infection-associated genes were not associated with increased relative abundance (Supplementary Fig. S10d).
Fig. 3. Specific infection-associated genes are associated with increased Klebsiella gut relative abundance.
a Comparison of Klebsiella gut relative abundance in patient rectal swabs between cases (n = 83) and controls (n = 149, mean displayed, ****P-value ≤ 0.00005, two-sided Student’s t-test) and b in patient rectal swabs stratified by gene presence/absence (25% percentile and 75% percentile bound the box, median displayed as line, mean displayed as plus sign, and range displayed as whiskers, *P-value ≤ 0.05, **P-value ≤ 0.005, ***P-value ≤ 0.0005, ****P-value ≤ 0.00005, two-sided Student’s t-test). Each data point represents a single patient rectal swab. Source data are provided as a Source Data file. Sample sizes for aac(6')-Ib-cr5 present n = 15, aac(6')-Ib-cr5 absent n = 217, group_9575 present n = 28, group_9575 absent n = 204, group_9537 present n = 31, group_9537 absent n = 201, group_13443 present n = 30, group_13443 absent n = 202, dgcE present n = 49, dgcE absent n = 183, aqpZ_2 present n = 34, aqpZ_2 absent n = 198, group_2409 present n = 37, group_2409 absent n = 195, pdeC_2 present n = 54, pdeC_2 absent n = 178, arsD_1 present n = 48, arsD_1 absent n = 184, group_774 present n = 75, group_774 absent n = 157, ltrA present n = 69, and ltrA absent n = 163.
To test the hypothesis that infection-associated genes may act through gut dominance we undertook a mediation analysis, a statistical approach that estimates the strength of both the direct associations between each gene and the outcome of infection and indirect association through gut relative abundance. For seven gene units, the association with infection was mediated, at least in part, by gut abundance (Table 2; indirect P-value, indicated in bold). The AMR gene aac(6')-Ib-cr5 had both a strong direct association with infection and an indirect mediation by abundance (P-value ≤ 0.01). The hypothetical protein group_774 also had both significant direct and indirect effects. The remaining five genes (hypothetical protein group_13443, dgcE, aqpZ_2, transposase group_2409, and arsD_1) had only significant indirect effects, indicating that their association with infection is mediated by gut relative abundance. Collectively, these findings begin to suggest biological roles for Klebsiella genes associated with infection, in which some genes may act through high gut relative abundance, but others likely have separate functions.
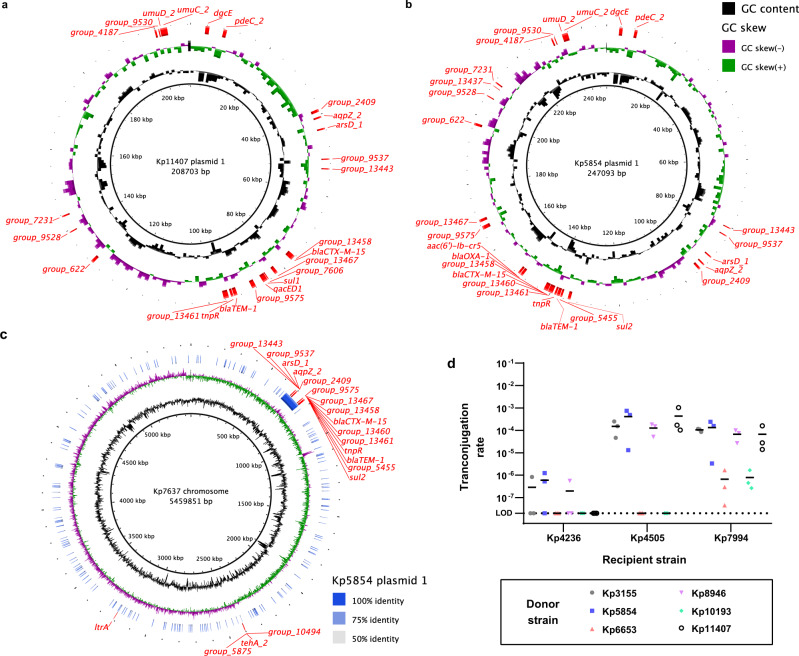
Most infection-associated genes are carried on plasmids
Given the diversity of functions and frequencies of the infection-associated genes, we sought to determine the genetic context of these genes as part of the accessory genome. Based on nucleotide homology, many of these genes have been previously detected on plasmids31–33. Consistent with plasmid carriage, certain infection-associated genes, including both AMR and non-AMR genes, are highly associated with one another (Supplementary Fig. S7) and appear to be linked (Fig. 2b). Furthermore, we detected the loss or gain of groups of infection-associated genes between some case clinical and rectal pairs, rather than individual genes (strata 211, 214, 701, 713, 716, Supplementary Fig. S3f). To determine the association between plasmids and infection-associated genes, we used the PlasmidFinder tool to detect replicons in the rectal isolates in our dataset34. We detected a replicon in 163 of 245 isolates (66.5%, 72.94% of case rectal isolates, 63.13% of control isolates), with a median of 2 replicons per isolate (Supplementary Data 5, range = 0–10 replicons). There was no significant difference between the number of replicons per isolate between cases and controls (Supplementary Fig. S11a). The three most common replicons were Col(pHAD28), IncFIB(K), and IncFII(K), and these replicons were distributed across the core genome phylogeny (Supplementary Fig. S11b); however, no replicon was significantly associated with infection (Supplementary Table 3).
To determine whether infection-associated genes are located on plasmids or the chromosome, we performed long-read sequencing and hybrid assembly with existing short read data on 10 isolates from cases of infection (Figs. 4a–c, S12). All of these isolates contained plasmids with infection-associated genes, and no two plasmids containing infection-associated genes were identical in terms of size, organization and gene content. At one extreme, the rectal case isolate Kp11407 contained a 208,703 bp hybrid IncFIB(K)/IncFII(K) plasmid encoding all 18 infection-associated loci present in this isolate (Fig. 4a). This plasmid closely aligns to the conjugative plasmid pUUH239.2 (CP002474.1), which was linked to a nosocomial K. pneumoniae outbreak35. Notably, this plasmid also contains several heavy metal resistance operons, including ars, pco, and sil35, which may enhance resistance to innate immune responses36. A second case rectal isolate, Kp5854, encoded 23 of 27 infection-associated loci on a 247,093 bp hybrid IncFIB(K)/IncFII(K) plasmid (Fig. 4b). This plasmid closely aligns to pF16KP0070-1 (CP052586.1), which also encodes ars, pco, and sil. Interestingly, in the corresponding clinical isolate, this plasmid appears to have integrated into the chromosome with the loss of some infection-associated genes (Fig. 4c; stratum 713, Supplementary Fig. S3g). These isolates also contained four additional infection-associated genes that mapped to the chromosome. The number of plasmid-encoded, infection-associated genes varied widely between plasmids (Supplementary Fig. S12). In contrast to Kp11407 and Kp5854, Kp11162 contained one plasmid with two infection-associated genes and a second plasmid with four (Supplementary Fig. S12g, h). Across these isolates 23 of all 27 infection-associated genes were found on at least one plasmid (Supplementary Fig. S12). Only group_774 and the tehA_2 gene cluster were not found on at least one plasmid. This suggests that these large plasmids facilitate acquisition of infection-associated loci and are likely drivers of the association between many genes and infection.
Fig. 4. Infection-associated genes are present on large, conjugative plasmids.
a Plasmid map of Kp11407 plasmid 1. b Plasmid map of Kp5854 plasmid 1. c Alignment of Kp7637 chromosome and Kp5854 plasmid 1. d Transconjugation rates using Kp3155, Kp5854, Kp6653, Kp8946, Kp10193, and Kp11407 as donor strains to Kp4236, Kp4505, and Kp7994, which are K. quasipneumoniae, K. pneumoniae, and K. variicola, respectively, as recipient strains (mean displayed, N.D. = none detected). For d, each data point represents a single biological replicate. Source data are provided as a Source Data file.
Infection-associated genes are transmissible by plasmids
To determine if infection-associated genes could be horizontally transmitted, we performed transconjugation assays between rectal isolates. Kp3155, Kp5854, Kp6653, Kp8946, Kp10193, and Kp11407 were selected as donor strains, as these K. pneumoniae case rectal isolates contained various infection-associated genes, including blaCTX-M-15 and dgcE, as well as the IncFIB(K) replicon. Three cefuroxime-sensitive control isolates lacking these genes, K. pneumoniae (Kp4505), K. variicola (Kp7994), and K. quasipneumoniae (Kp4236), were selected as recipient strains. Kp7994 and Kp4236 lack plasmid replicons, and Kp4505 contains an IncFIB(K) replicon. Conjugation to Kp4236 was limited, with inconsistent or lack of transfer across donor strains. In contrast, conjugation was readily detected from donors Kp3155, Kp5854, Kp8946, Kp11407 to recipient Kp4505, and from all donors to Kp7994 (Fig. 4d). All transconjugants were cefuroxime resistant, indicating the transfer of blaCTX-M-15, and were PCR-positive for dgcE. Therefore, we concluded that these large plasmids are conjugative, resulting in the transfer of infection-associated genes.
Validation of infection-associated genes in a geographically distinct patient cohort
Finally, we aimed to validate our findings across multiple geographical locations. To this end, we screened a cohort of Klebsiella colonized patients from a single academic medical center in Maryland, USA for six infection-associated genes: aac(6')-Ib-cr5, blaCTX-M-15, group_13461, group_13467, dgcE, and aqpZ_2. These genes were selected because they were representative of the many facets of our findings, encapsulating known AMR genes (aac(6')-Ib-cr5, blaCTX-M-15), MGEs (group_13461, group_13467), and those where the relationship between gene presence and infection was (aac(6')-Ib-cr5, dgcE, aqpZ_2) and was not (blaCTX-M-15, group_13461, group_13467) significantly mediated by Klebsiella gut relative abundance. Moreover, these genes are found on conjugative plasmids (Fig. 4). This second cohort consisted of 55 cases of Klebsiella infection and 432 asymptomatically colonized control patients. Since wzi concordance data was not available, we screened both case isolates and a rectal isolate from each patient for each gene. Rectal isolates were not available for three infected patients and a clinical isolate was not available for one patient. In total, 538 Klebsiella isolates (54 clinical isolates, 52 case rectal isolates, 432 control rectal isolates) were screened for the presence or absence of target genes using a multiplex RT-PCR assay. As an internal control for Klebsiella detection, we included a previously validated assay for the fiu gene11. Based on either clinical or rectal isolates from cases, we observed a significant association with infection for all genes except aqpZ_2 (Table 4). Overall, 82.4% (42/51 of available pairs) of clinical-rectal pairs returned concordant RT-PCR results, which was highly consistent with our previous study using wzi sequencing to determine concordance10. As in the primary cohort (Supplementary Fig. S7), the presence of these genes in case rectal isolates were associated with one another (Supplementary Fig. S13), suggesting that these genes in the Maryland isolates may also be linked through conjugative plasmids. The strongest associations were between dgcE and apqZ_2 and between aac(6')-Ib-cr5, blaCTX-M-15, group_13461 and group_13467. Overall, five of six genes were reproducibly associated with case status in colonized patients in two geographically-distinct cohorts.
Table 4.
Gene association with positive clinical cultures in a geographically independent cohort of Klebsiella colonized patients
| Gene | Sample | Frequency | Odds ratio | 95% CI | P-value |
|---|---|---|---|---|---|
| aac(6')-Ib-cr5 | Case clinical | 0.167 | 4.88 | 1.96 to 11.1 | 0.0009 |
| Case rectal | 0.115 | 3.18 | 1.22 to 8.41 | 0.0276 | |
| Control rectal | 0.039 | ||||
| dgcE | Case clinical | 0.481 | 2.28 | 1.29 to 3.99 | 0.0074 |
| Case rectal | 0.5 | 2.46 | 1.37 to 4.41 | 0.0039 | |
| Control rectal | 0.289 | ||||
| group_13461 | Case clinical | 0.204 | 4.55 | 2.06 to 9.6 | 0.0005 |
| Case rectal | 0.192 | 4.23 | 1.93 to 9.24 | 0.0042 | |
| Control rectal | 0.053 | ||||
| group_13467 | Case clinical | 0.296 | 3.81 | 1.94 to 7.29 | 0.0002 |
| Case rectal | 0.25 | 3.02 | 1.48 to 6.1 | 0.0043 | |
| Control rectal | 0.1 | ||||
| blaCTX-M-15 | Case clinical | 0.185 | 4.94 | 2.19 to 11.4 | 0.0005 |
| Case rectal | 0.173 | 4.55 | 1.83 to 10.9 | 0.0013 | |
| Control rectal | 0.044 | ||||
| aqpZ_2 | Case clinical | 0.296 | 1.58 | 0.83 to 2.93 | 0.164 |
| Case rectal | 0.327 | 1.82 | 0.98 to 3.38 | 0.076 | |
| Control rectal | 0.213 |
Bold text indicates significant results (P-value ≤ 0.05).
Discussion
In this study, we have identified novel Klebsiella genes associated with infection in colonized patients. The findings from this diverse collection of Klebsiella isolates, carefully adjusted for patient risk factors and phylogeny, and validated in a second geographically distinct cohort, provides important insights into the broader dynamics of Klebsiella pathogenesis. Most of these genes were found across a diverse set of plasmids, suggesting that these genes are either direct mediators of fitness and virulence or indirect markers of large, conjugative plasmids that increase infection risk as a unit. These genes can be separated into two categories: those whose association with infection is mediated through increased abundance in the gut, and those that have a direct association with infection. Genes whose effect on infection risk is not mediated through intestinal dominance may act at a subsequent step of pathogenesis. These genes associated with infection are readily mobilized within and across members of the Klebsiella pneumoniae species complex, and changes in infection-associated gene content and genetic context were detectable within colonized patients who progressed to infection. Collectively, this study provides a set of genetic signatures of infection that have potential for predicting risk of infection in patients colonized by diverse Klebsiella.
The majority of infection-associated loci in our dataset are present on plasmids, which can vary in size, gene content, copy number, and conjugative ability (Fig. 4a–c, Supplementary Fig. S12). This plasmid carriage creates genetic linkage between genes that are associated with infection, raising the possibility that some are direct effectors of fitness or virulence whereas others are robust markers for these effectors. In some instances, clear relationships exist between linked genes. For example, nucleotide cyclases are often present in tandem with cyclic nucleotide phosphodiesterases, thus the linkage of dgcE and pdeC_2 is expected. dgcE and pdeC_2 may regulate expression of type 1 and 3 pili through modulation of cyclic di-GMP levels. Expression of the type 1 pilus reduces virulence in the lung and spleen but enhances gut colonization in murine models37,38. Therefore, dgcE may enhance fitness in the gut while pdeC_2 may enhance fitness in extra-intestinal sites. Likewise, the linkage of blaCTX-M-15 and group_13461 is expected since ISEcp1 transposases are known to mobilize and promote the expression of CTX-M-type β-lactamases39,40. Conversely, relationships between other linked genes, such as arsD_1 and the various AMR genes, are more difficult to understand. It may be the case that these infection-associated genes act at different stages of infection or one or both are robust genetic markers for fitness genes elsewhere on the plasmid.
The strong association between multiple AMR genes and infection following adjustment for high-risk antibiotic exposure indicates that the relationship between antibiotic resistance and infection is complex in Klebsiella. Antibiotic resistance genes could be associated with infection by enabling intestinal outgrowth and dominance after exposure to a cognate antibiotic. However, the ESBL determinants blaCTX-M-15, blaOXA-1, and blaTEM-1 were associated with infection independent of antibiotic exposure and their association was not significantly mediated by gut relative abundance. Notably, antibiotic exposure rates are low (<10% for most classes) in our original study population10. Therefore, detection of these antibiotic resistance genes is more likely a marker of other infection-associated genes and/or plasmids, rather than conferring resistance to a cognate antibiotic. It may be the case that these strains acquired these genes earlier in their evolutionary history; however, prospective comparative genomics studies are necessary to pinpoint such events. Potential fitness benefits of AMR genes in the absence of antibiotics are intriguing, yet highly AMR Klebsiella STs are generally less virulent in experimental models than their hypervirulent counterparts, and specific mutations that confer AMR can have deleterious effects on Klebsiella fitness41–44. On the other hand, plasmid acquisition of AMR is less costly than chromosomal mutations45. Therefore, AMR genes may be linked to plasmid-encoded genes that enhance infection risk, and then complicate treatment of infections after they are initiated.
The identification of non-AMR genes associated with infection as mediated by gut dominance adds to our understanding of bacterial genotypes and the risk for infection in Klebsiella colonized patients. We previously demonstrated that the ter operon, annotated as a tellurite-resistance operon, is a microbiome-dependent gut fitness factor23. Similarly, the arsD_1 gene identified in this study is part of an arsenic resistance (ars) operon. Tellurite and arsenic are both toxic metalloids, implying that the ars operon may be playing an analogous role to ter. Consistent with this, gut relative abundance mediates the association between arsD_1 and infection (Table 2). Conversely, we did not find evidence that gut relative abundance mediates the association between the tellurite-resistance gene tehA_2 gene and infection, although it is predicted to encode a different molecular function than ter. These data highlight the complex interplay between bacterial genotype and gut fitness, and the need to understand the role of colonization fitness to both assess infection risk and prophylactic decolonization therapies. The risk of Klebsiella disease in colonized patients may not warrant prophylactic antibiotic administration, especially in the context of rising rates of AMR; however, non-antibiotic options are currently being explored (reviewed in46). A better understanding of how bacterial pathogens, such as Klebsiella, successfully colonize and dominate the gut is needed to ensure the efficacy of any decolonization approach.
Although this study advances our understanding of infection in patients colonized by diverse Klebsiella, it is not without its limitations. First, this study is retrospective and relies on the availability of clinical data in the electronic medical record. Prospective studies with longer timeframes aimed at evaluating the association between genes identified in this study and infection would be useful for validating our findings. Second, many infection-associated genes are associated with one another and these genes are plasmid-borne. This finding is important; however, it complicates the evaluation of the causal relationship between individual genes and infection. Experimental studies are necessary to determine the causal relationship between each gene and disease. Additionally, we did not comprehensively assess the genomic architecture and HGT potential of our strains. It may be the case that only a subset of genes is frequently transferred between strains and/or only a subset of strains is able to easily donate and receive these genes. Notably, all plasmid donor strains that we tested were K. pneumoniae that encoded an IncFIB(K) replicon (Supplementary Data 5), therefore limiting our ability to assess the universality of the HGT phenotype. Further assessment of the Klebsiella plasmidome will be critical to fully interpret the role of the infection-associated genes identified in this study, as well as the characterization of cryptic plasmids that could be missed with replicon-based analysis such as PlasmidFinder. Moreover, more complicated approaches such as shotgun metagenomics are necessary to contextualize plasmid borne genes in polymicrobial reservoirs of bacteria with pathogenic potential, such as the gut. In our combined approach across three species, the majority of our genomes were from K. pneumoniae. There may be K. variicola or K. quasipneumoniae-specific infection-associated genes that we were unable to detect. Third, the Klebsiella genes associated with infection likely differ by patient population. We found different genes associated with infection (ter, psicose utilization locus) in a hospital-wide comparative genomics study and experimentally validated them as encoding fitness factors22,23. That patient population may have different risk factors and stronger barriers to infection. Among intensive care and hematology/oncology patients, the genes associated with infection were highly reproducible in a geographically independent cohort. Finally, this study focused on gene presence in the accessory genome and does not consider the role of mutations within the core or accessory genomes.
This study provides insights into infection risk from diverse lineages of the K. pneumoniae species complex. The well-characterized virulence genes of hypervirulent clonal groups, many of which are plasmid-borne25, were rare and not informative in assessing infection risk in this population. MDR isolates were more frequent representing six clonal groups, but overall, 85.7% (210/245) of the isolates in our collection were from non-hypervirulent, non-MDR CGs. Given the predominance of non-hypervirulent, or “classical” strains worldwide25, efforts to understand the pathogenesis and enact preventative therapies is likely to have a substantial payoff. The varied combinations of infection-associated genes found across case isolates suggests that a diverse accessory genome acquired through HGT drives infection risk in Klebsiella. Certain combinations have become fixed; some hypervirulent Klebsiella clones have carried their plasmids for decades. However, new combinations can arise within a colonized patient (Fig. 4; Supplementary Fig. S12). Even in seemingly fixed plasmid-strain combinations, exchange has occurred leading to multiple instances of the convergence of virulence and MDR determinants25. In total, this study adds to the growing understanding of the Klebsiella accessory genome as a critical determinant of infection risk.
The insights from this study can be used to predict infection risk in colonized, hospitalized patients and trigger infection prevention interventions. We have previously identified certain patient risk factors associated with infection, and that gut dominance is associated with infection independently of these clinical factors10,11. Here we identified infection-associated genes independent of patient risk factors and that part of the association is mediated by gut dominance. We have also developed the tools to measure these risks, including a robust qPCR assay to measure intestinal dominance and the genotyping PCR assays implemented in this study. The fact that AMR genes and phenotypes are strongly associated with infection could also enable the use of standard culture approaches to detect these genes, and therefore, high-risk colonizing strains. It is possible that these approaches can be combined with queries of the electronic medical record for clinical variables to generate an integrated risk score for a colonized patient. In the near term, this score could be used to identify patients for trials of decolonization therapies. Eventually, integrated risk models could identify at-risk patients who could most benefit from effective prevention interventions.
Methods
Ethics statement
Patient enrollment and sample collection at the University of Michigan was approved by and performed in accordance with the Institutional Review Boards (IRB) of the University of Michigan Medical School (Study number HUM00123033). Patient enrollment and sample collection at Johns Hopkins University was approved and performed in accordance with the IRB of the Johns Hopkins University (Study number IRB00129775). Patients were retrospectively enrolled after routine samples were taken in the course of clinical care. This study was performed with a waiver of informed consent since the research involves no more than minimal risk to the subjects, could not practicably be carried out without the waiver, and uses discarded samples. Patient enrollment was identical at both sites.
Sample collection and strain selection
At Michigan Medicine, Klebsiella isolates were selected from a large cohort of Klebsiella colonized patients. Cohort identification, enrollment, clinical data extraction, chart review, and case definitions are described in detail elsewhere10. During the study period, patient rectal swabs were screened for the presence of Klebsiella by plating on MacConkey agar followed by taxonomic identification using MALDI TOF mass spectrometry. Up to three Klebsiella isolates per rectal swab, and any subsequent Klebsiella positive clinical cultures, were archived. Minimum inhibitory concentration data from case clinical isolates was extracted from the Michigan Medicine clinical microbiology lab. To identify concordant infections, Klebsiella rectal swab and case clinical isolates were subjected to wzi PCR and Sanger sequencing, and the wzi type was assigned by uploading the consensus wzi sequence to the BigsDB database (https://bigsdb.pasteur.fr). Each case was matched to two controls based on sex, age (±10 years), and date of rectal swab collection (±90 days). Several cases could only be matched to a control swab within 120 days (n = 6). Case matching was conducted in R, version 4.0.3.
At the Johns Hopkins University, adult patients admitted to medical or surgical ICUs are routinely screened for VRE rectal colonization on admission and weekly thereafter until ICU discharge. Residual Amies broth from rectal ESwabs (COPAN Diagnostics, Inc., Murrieta, California) were inoculated on a MacConkey agar plate using the WASP DT (COPAN) automated specimen processer, and isolates were archived as above.
Whole-genome sequencing, assembly, and annotation
Archived Klebsiella isolates were cultured in Luria-Bertani (LB, Becton, Dickinson and Company, Franklin Lakes, NJ) broth at 37 °C with shaking for genomic DNA extraction. Genomic DNA was extracted using the DNeasy UltraClean Microbial Kit (Qiagen, Hilden, Germany) per manufacturer’s instructions. Extracted genomic DNA was then checked for quality and purity and submitted to the University of Michigan Advanced Genomics Core, where it was sequenced on an Illumina NovaSeq using a 300 cycle S4 flow cell (Illumina, San Diego, USA) to generate approximately 6,000,000 150 bp paired-end reads. Resulting reads were trimmed using Trimmomatic v0.3947 and assembled into scaffolds using SPAdes v3.13.048. Genome assemblies within each stratum were compared using QUAST v5.0.249, wherein each genome assembly was compared to the case rectal isolate genome assembly. Genome annotation was performed using Prokka v1.14.650, and a pangenome was assembled using Roary v3.13.051, with settings “-i 90” and “-s.” Finally, assembly genotyping was performed using Kleborate v1.0.025 and PlasmidFinder v2.0.134. For long-read sequencing, genomic DNA was checked for quality and purity and submitted to the University of Michigan Advanced Genomics Core, where it was sequenced on a GridION X5 platform using a MinION flow cell (Oxford Nanopore Technology, Oxford, UK). Low-quality read ends were trimmed with NanoFilt v2.5.052 and assembled using Unicycler v0.4.8 using the “bold” setting53. The core gene alignment was created using Illumina assemblies with cognac using the default parameters54. The wzi gene sequences from each Illumina assemblies were identified by BLAST v2.9.055. The BLAST output was parsed to extract the aligned sequence from each query, and the gene sequences were aligned with MAFFT v7.310. Approximate maximum likelihood trees were generated from the wzi alignment and cognac alignment with fastTree v2.1.1056. Phylogenetic trees were visualized with the APE R package v5.357. Rarefaction was performed using iNEXT v2.0.2058, with setting “q = 0.” All analyses were performed in R v4.0.5. Plasmid maps and corresponding alignments were constructed and visualized using BRIG v0.9559. All code developed for this manuscript is available at https://github.com/rdcrawford/Bachman_CU8.
Phenotypic antibiotic screen
To screen for phenotypic antibiotic resistance, all Klebsiella rectal isolates were arrayed into 96-well plates and stored at −80 °C in 20% LB-glycerol. We were unable to locate one isolate in our freezer following WGS, thus it was omitted from phenotypic analysis. Then Klebsiella rectal isolates were sub-cultured in LB broth at 37 °C overnight and replica plated on antibiotic containing LB-agar. Antibiotic concentrations (36 mg/mL ampicillin, 32 mg/mL chloramphenicol, 16 mg/mL gentamicin, 1 mg/mL ciprofloxacin, 32 mg/mL cefazolin, 32 mg/mL cefuroxime, 16 mg/mL cefepime) were selected in accordance with CLSI criteria for resistance. All assays were performed in triplicate.
Transconjugation assay
Single colonies of Kp4236, Kp4505, Kp7994 (recipient strains; chloramphenicol resistant), and Kp3155, Kp5854, Kp6653, Kp8946, Kp10193, Kp11407 (donor strains; cefuroxime resistant) were sub-cultured overnight in 1 mL of LB broth at 37 °C with shaking. The next day, overnight cultures were harvested by centrifugation and resuspended in 1 mL sterile phosphate-buffered saline (PBS). 50 µL of Kp4236, Kp4505, or Kp7994 resuspension was mixed with 50 µL of each donor strain resuspension and spotted on LB-agar. 50 µL of unmixed resuspension of each strain was spotted in parallel. Bacterial spots were grown overnight at 37 °C, then harvested into 1 mL sterile PBS by scraping and serially plated on differential growth media. Transconjugation rates were calculated by quantifying the bacterial density of dual-resistant colonies divided by the total density of the recipient strain. Transconjugates were confirmed by qPCR targeting the dcgE gene using unmixed strains as a reference (assay details below). All assays were performed in triplicate, and 3 transconjugate colonies and 3 unmixed recipient and donor colonies were selected per assay for PCR confirmation.
RT-PCR design and assay
To screen for the presence of aac(6')-Ib-cr5, blaCTX-M-15, group_13461, group_13467, dgcE, and aqpZ_2, multiplex real-time PCR assays were designed using PanelPlex (DNA Software, Ann Arbor, USA) and combined with a previously validated Klebsiella-specific fiu assay11. All primer and probe sequences can be found in Supplementary Table 4. Clinical and rectal isolates were arrayed and sub-cultured in 150 µL LB overnight at 37 °C. To extract genomic DNA, overnight cultures were harvested by centrifugation and resuspended in 100 µL of PCR-grade water, boiled at 95 °C for 5 min, and pelleted. Then, 5 µL of the supernatant was used as a PCR template. Primer (Integrated DNA Technologies, Coralville, USA) and probe (Thermo Fisher Scientific, Waltham, USA) concentrations were 400 nM and 200 nM, respectively11. Real-time PCR was performed using a QuantStudio 3 real-time thermocycler (Thermo Fisher Scientific, Waltham, USA) using the following protocol: 50 °C for 2 min, 95 °C for 15 min, then 40 cycles of 94 °C for 1 min and 60 °C for 1 min. All assays were performed in duplicate unless replicates conflicted, wherein a third replicate was performed, and all isolate arrays included 3 positive controls and 3 randomly dispersed negative controls. The target gene was assigned as present in an isolate if a reaction was (1) positive for fiu, (2) amplified within 2 Ct of the range of the positive control Cts, and (3) results were concordant between all replicates.
Statistical analysis
For clinical variable comparisons, odds ratios and associated 95% confidence intervals were calculated using conditional logistic regression in R (version 3.6.3) and a P-value ≤ 0.05 was considered statically significant. For infection-associated gene discovery, a P-value ≤ 0.05 and Q-value ≤ 0.2 was used as a cutoff for further exploration. For these analyses, Scoary v1.6.1626 was used with the “–collapse” and “-n” settings with our custom core genome phylogeny, limited to genes that were 5–95% frequent in the dataset. For analyses considering population structure, treeWAS v1.129 was used with the phen.type = “discrete” setting and our custom core genome phylogeny. For gene-gene associations, odds ratios were calculated using Fishers exact test in R Studio v1.2.5001. To account for the inflated type I error rate due to the large number of comparisons, a P-value ≤ 0.01 was considered statistically significant for subsequent clinical variable adjustment, mediation, population structure, and genotyping analyses.
Next, we considered adjustment of clinical variables. Inverse probability of treatment weighting method was used for this purpose60. The analysis is performed separately for each gene. In the propensity score model, a logistic regression was used with the clinical variables as predictors and binary gene presence/absence as the outcome. The predicted probabilities estimated from the regression model were used to compute weights and then included in the outcome model. The outcome model is a logistic regression with Klebsiella infection as the outcome and gene (presence/absence) as the predictor, while incorporating the matched nature of the data. Following IPTW analysis, we assessed if each gene was associated with infection after individually adjusting for exposure to each class of antibiotics. We repeated the described IPTW analysis using the same weights, controlling for each prior exposure as a covariate in the outcome model one at a time. The “survey” package (v4.1-1) in R was used to obtain the robust standard error.
We then conducted a mediation analysis on each gene that was significantly associated with infection to explore if the relationship between gene presence/absence and infection is mediated through abundance. Specifically, we assessed (1) the direct effect defined as the effect of gene presence on infection, adjusting for abundance as a continuous variable and clinical factors, (2) the indirect effect of the gene on infection mediated through abundance after adjusting clinical factors. To account for the matched case-control design, a generalized linear mixed model was used with a random effect for the strata defining matched case-controls. A significant mediation (i.e., indirect) effect indicates evidence that the effect of the gene on infection is mediated through abundance, and direct effects were also reported. The P-values for these effects were assessed to identify genes to investigate further. We conducted the analyses using the ‘mediation’ (v4.5.0) and ‘lme4’ packages (v1.1-29)61,62 in R v3.6.3.
For in vitro experiments, one-sample t-test, unpaired Student’s t-tests, and ANOVA followed by indicated post-hoc test was used to determine significant differences between groups following log transformation of experimental values. For in vitro experiments, a P-value ≤ 0.05 was considered statistically significant. Experimental replicates represent biological replicates. Statistical testing was two-sided in all circumstances. Statistical analysis of in vitro experiments was performed using Prism 8 (GraphPad Software, La Jolla, CA).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
The authors would like to thank the University of Michigan Advanced Genomics Core of the University of Michigan Medical School’s Biomedical Research Core Facilities for their assistance with whole-genome sequencing. Additionally, we acknowledge support from the Bioinformatics Core of the University of Michigan Medical School’s Biomedical Research Core Facilities. Figure 1a was created with BioRender.com. This work was supported by funding from National Institution of Health (https://www.nih.gov/) grants R01AI125307 to MAB and 1R01AI148259-01 to ESS. J.V. was supported by the Postdoctoral Translational Scholar Program (NIH UL1TR002240). R.C. was supported by the University of Michigan bioinformatics training grant (NIH T32GM070449). L.U. was supported by the Molecular Mechanisms in Microbial Pathogenesis Training Program (T32 AI007528). C.L.H. was supported by the Lung Immunopathology Training Program (T32HL007517). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Source data
Author contributions
Conceptualization: J.V., L.Z., P.J.S., P.D.T., K.R., K.S.K., M.A.B. Methodology: E.K.R., R.C., E.S.S., L.Z., K.R., M.A.B. Investigation: J.V., E.K.R., L.U., A.P., R.C., S.M., C.L.H., Y.S., A.T. Visualization: J.V., R.C. Funding acquisition: M.A.B. Project administration: M.A.B. Supervision: MAB. Writing—original draft: J.V., E.R., L.U., S.M., M.A.B. Writing—review & editing: J.V., E.K.R., L.U., A.P., R.C., S.M., C.L.H., Y.S., A.T., E.S.S., L.Z., P.J.S., P.D.T., K.R., K.S.K., M.A.B.
Peer review
Peer review information
Nature Communications thanks David Rosen, Edward Feil and the other anonymous reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Data availability
The sequencing data generated in this study have been deposited in the Sequence Read Archive (SRA) database under accession code PRJNA789565. The human subjects data are available under restricted access for the protection of the rights and welfare of human research subjects. Deidentified human data are available under restricted access and can be obtained from MAB within 1 year upon request, pending approval from the University of Michigan Institutional Review Board. The remaining data generated in this study are provided in the Supplementary Information/Source Data file. Source data are provided with this paper.
Code availability
All code developed for this manuscript is available at https://github.com/rdcrawford/Bachman_CU8.
Competing interests
K.R. is supported in part from an investigator-initiated grant from Merck & Co, Inc. and has consulted for Bio-K + International, Inc., Roche Molecular Systems, Inc., and Seres Therapeutics. All other authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-022-31990-1.
References
- 1.Long, S. W. et al. Whole-genome sequencing of a human clinical isolate of the novel species Klebsiella quasivariicola sp. nov. Genome Announc.10.1128/genomeA.01057-17 (2017). [DOI] [PMC free article] [PubMed]
- 2.Rodrigues C, et al. Description of Klebsiella africanensis sp. nov., Klebsiella variicola subsp. tropicalensis subsp. nov. and Klebsiella variicola subsp. variicola subsp. nov. Res. Microbiol. 2019;170:165–170. doi: 10.1016/j.resmic.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Wyres KL, Lam MMC, Holt KE. Population genomics of Klebsiella pneumoniae. Nat. Rev. Microbiol. 2020;18:344–359. doi: 10.1038/s41579-019-0315-1. [DOI] [PubMed] [Google Scholar]
- 4.Magill SS, et al. Multistate point-prevalence survey of health care–associated infections. N. Engl. J. Med. 2014;370:1198–1208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CDC. The Direct Medical Costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention (Centers for Disease Control & Prevention, 2009).
- 6.O’Neill. Tackling Drug-Resistant Infections Globally: Final Report And Recommendations. https://amr-review.org (2016).
- 7.Martin, R. M. et al. Molecular epidemiology of colonizing and infecting isolates of Klebsiella pneumoniae. mSphere1, e00261–16 (2016). [DOI] [PMC free article] [PubMed]
- 8.Collingwood A, et al. Epidemiological and microbiome associations between Klebsiella pneumoniae and vancomycin-resistant enterococcus colonization in intensive care unit patients. Open forum Infect. Dis. 2020;7:ofaa012. doi: 10.1093/ofid/ofaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gorrie CL, et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae Infection in intensive care patients. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2017;65:208–215. doi: 10.1093/cid/cix270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rao, K. et al. Risk Factors for Klebsiella infections among hospitalized patients with preexisting colonization. mSphere10.1128/mSphere.00132-21 (2021). [DOI] [PMC free article] [PubMed]
- 11.Sun, Y. et al. Measurement of Klebsiella intestinal colonization density to assess infection risk. mSphere10.1128/mSphere.00500-21 (2021). [DOI] [PMC free article] [PubMed]
- 12.Russo, T. A. & Marr, C. M. Hypervirulent Klebsiella pneumoniae. Clin. Microbiol. Rev.10.1128/CMR.00001-19 (2019). [DOI] [PMC free article] [PubMed]
- 13.Wyres KL, et al. Genomic surveillance for hypervirulence and multi-drug resistance in invasive Klebsiella pneumoniae from South and Southeast Asia. Genome Med. 2020;12:11. doi: 10.1186/s13073-019-0706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin RM, Bachman MA. Colonization, infection, and the accessory genome of Klebsiella pneumoniae. Front. Cell. Infect. Microbiol. 2018;8:4. doi: 10.3389/fcimb.2018.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snitkin ES, et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci. Transl. Med. 2012;4:148ra116. doi: 10.1126/scitranslmed.3004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Long, S. W. et al. Population genomic analysis of 1,777 extended-spectrum beta-lactamase-producing Klebsiella pneumoniae isolates, houston, texas: unexpected abundance of clonal group 307. mBio. 10.1128/mBio.00489-17 (2017). [DOI] [PMC free article] [PubMed]
- 17.Marvig RL, Sommer LM, Molin S, Johansen HK. Convergent evolution and adaptation of Pseudomonas aeruginosa within patients with cystic fibrosis. Nat. Genet. 2015;47:57–64. doi: 10.1038/ng.3148. [DOI] [PubMed] [Google Scholar]
- 18.Allen JP, et al. A comparative genomics approach identifies contact-dependent growth inhibition as a virulence determinant. Proc. Natl Acad. Sci. USA. 2020;117:6811–6821. doi: 10.1073/pnas.1919198117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aggarwal SD, et al. Function of BriC peptide in the pneumococcal competence and virulence portfolio. PLoS Pathog. 2018;14:e1007328. doi: 10.1371/journal.ppat.1007328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mageiros L, et al. Genome evolution and the emergence of pathogenicity in avian Escherichia coli. Nat. Commun. 2021;12:765. doi: 10.1038/s41467-021-20988-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bornstein K, et al. Genetic changes associated with the temporal shift in invasive non-typhoidal Salmonella serovars in Bamako Mali. PLoS Negl. Trop. Dis. 2019;13:e0007297. doi: 10.1371/journal.pntd.0007297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin, R. M. et al. Identification of pathogenicity-associated Loci in Klebsiella pneumoniae from hospitalized patients. mSystems10.1128/mSystems.00015-18 (2018). [DOI] [PMC free article] [PubMed]
- 23.Vornhagen J, et al. A plasmid locus associated with Klebsiella clinical infections encodes a microbiome-dependent gut fitness factor. PLoS Pathog. 2021;17:e1009537. doi: 10.1371/journal.ppat.1009537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brisse S, et al. wzi Gene sequencing, a rapid method for determination of capsular type for Klebsiella strains. J. Clin. Microbiol. 2013;51:4073–4078. doi: 10.1128/JCM.01924-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lam MMC, et al. A genomic surveillance framework and genotyping tool for Klebsiella pneumoniae and its related species complex. Nat. Commun. 2021;12:4188. doi: 10.1038/s41467-021-24448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brynildsrud O, Bohlin J, Scheffer L, Eldholm V. Rapid scoring of genes in microbial pan-genome-wide association studies with Scoary. Genome Biol. 2016;17:238. doi: 10.1186/s13059-016-1108-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baggs J, et al. Risk of subsequent sepsis within 90 Days after a hospital stay by type of antibiotic exposure. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2018;66:1004–1012. doi: 10.1093/cid/cix947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robicsek A, et al. Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat. Med. 2006;12:83–88. doi: 10.1038/nm1347. [DOI] [PubMed] [Google Scholar]
- 29.Collins C, Didelot X. A phylogenetic method to perform genome-wide association studies in microbes that accounts for population structure and recombination. PLoS Comput. Biol. 2018;14:e1005958. doi: 10.1371/journal.pcbi.1005958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CLSI. Methods for Dilution Antimicrobial Susceptibility Tests fo Bacteria That Grow Aerobically. 10th edn (Clinical and Laboratory Standards Institute, 2015).
- 31.Alcock BP, et al. CARD 2020: antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2020;48:D517–D525. doi: 10.1093/nar/gkz1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J, Rosen BP. The arsD gene encodes a second trans-acting regulatory protein of the plasmid-encoded arsenical resistance operon. Mol. Microbiol. 1993;8:615–623. doi: 10.1111/j.1365-2958.1993.tb01605.x. [DOI] [PubMed] [Google Scholar]
- 33.Serfiotis-Mitsa D, et al. The structure of the KlcA and ArdB proteins reveals a novel fold and antirestriction activity against Type I DNA restriction systems in vivo but not in vitro. Nucleic acids Res. 2010;38:1723–1737. doi: 10.1093/nar/gkp1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carattoli A, Hasman H. PlasmidFinder and in Silico pMLST: identification and typing of plasmid replicons in whole-genome sequencing (WGS) Methods Mol. Biol. 2020;2075:285–294. doi: 10.1007/978-1-4939-9877-7_20. [DOI] [PubMed] [Google Scholar]
- 35.Sandegren L, Linkevicius M, Lytsy B, Melhus A, Andersson DI. Transfer of an Escherichia coli ST131 multiresistance cassette has created a Klebsiella pneumoniae-specific plasmid associated with a major nosocomial outbreak. J. Antimicrob. Chemother. 2012;67:74–83. doi: 10.1093/jac/dkr405. [DOI] [PubMed] [Google Scholar]
- 36.Djoko KY, Ong CL, Walker MJ, McEwan AG. The role of copper and zinc toxicity in innate immune defense against bacterial pathogens. J. Biol. Chem. 2015;290:18954–18961. doi: 10.1074/jbc.R115.647099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khater F, et al. In silico analysis of usher encoding genes in Klebsiella pneumoniae and characterization of their role in adhesion and colonization. PLoS One. 2015;10:e0116215. doi: 10.1371/journal.pone.0116215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosen, D. A., Twentyman, J. & Hunstad, D. A. High levels of cyclic Di-GMP in Klebsiella pneumoniae Attenuate virulence in the lung. Infect. Immun.10.1128/IAI.00647-17 (2018). [DOI] [PMC free article] [PubMed]
- 39.Bonnet R. Growing group of extended-spectrum beta-lactamases: the CTX-M enzymes. Antimicrob. Agents Chemother. 2004;48:1–14. doi: 10.1128/AAC.48.1.1-14.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poirel L, Decousser JW, Nordmann P. Insertion sequence ISEcp1B is involved in expression and mobilization of a bla(CTX-M) beta-lactamase gene. Antimicrobial agents Chemother. 2003;47:2938–2945. doi: 10.1128/AAC.47.9.2938-2945.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruchmann, S., Feltwell, T., Parkhill, J. & Short, F. L. Identifying virulence determinants of multidrug-resistant Klebsiella pneumoniae in Galleria mellonella. Pathog. Dis. 10.1093/femspd/ftab009 (2021). [DOI] [PMC free article] [PubMed]
- 42.Xiong H, et al. Distinct contributions of neutrophils and CCR2+ monocytes to pulmonary clearance of different Klebsiella pneumoniae strains. Infect. Immun. 2015;83:3418–3427. doi: 10.1128/IAI.00678-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olonisakin TF, et al. CD36 provides host protection against Klebsiella pneumoniae intrapulmonary infection by enhancing lipopolysaccharide responsiveness and macrophage phagocytosis. J. Infect. Dis. 2016;214:1865–1875. doi: 10.1093/infdis/jiw451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wong JLC, et al. OmpK36-mediated Carbapenem resistance attenuates ST258 Klebsiella pneumoniae in vivo. Nat. Commun. 2019;10:3957. doi: 10.1038/s41467-019-11756-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vogwill T, MacLean RC. The genetic basis of the fitness costs of antimicrobial resistance: a meta-analysis approach. Evol. Appl. 2015;8:284–295. doi: 10.1111/eva.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gargiullo L, Del Chierico F, D’Argenio P, Putignani L. Gut microbiota modulation for multidrug-resistant organism decolonization: present and future perspectives. Front. Microbiol. 2019;10:1704. doi: 10.3389/fmicb.2019.01704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bankevich A, et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012;19:455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gurevich A, Saveliev V, Vyahhi N, Tesler G. QUAST: quality assessment tool for genome assemblies. Bioinformatics. 2013;29:1072–1075. doi: 10.1093/bioinformatics/btt086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seemann T. Prokka: rapid prokaryotic genome annotation. Bioinformatics. 2014;30:2068–2069. doi: 10.1093/bioinformatics/btu153. [DOI] [PubMed] [Google Scholar]
- 51.Page AJ, et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics. 2015;31:3691–3693. doi: 10.1093/bioinformatics/btv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.De Coster W, D’Hert S, Schultz DT, Cruts M, Van Broeckhoven C. NanoPack: visualizing and processing long-read sequencing data. Bioinformatics. 2018;34:2666–2669. doi: 10.1093/bioinformatics/bty149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wick RR, Judd LM, Gorrie CL, Holt KE. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 2017;13:e1005595. doi: 10.1371/journal.pcbi.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crawford RD, Snitkin ES. cognac: rapid generation of concatenated gene alignments for phylogenetic inference from large, bacterial whole genome sequencing datasets. BMC Bioinforma. 2021;22:70. doi: 10.1186/s12859-021-03981-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 56.Price MN, Dehal PS, Arkin AP. FastTree: computing large minimum evolution trees with profiles instead of a distance matrix. Mol. Biol. Evol. 2009;26:1641–1650. doi: 10.1093/molbev/msp077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paradis E, Claude J, Strimmer K. APE: Analyses of phylogenetics and evolution in R language. Bioinformatics. 2004;20:289–290. doi: 10.1093/bioinformatics/btg412. [DOI] [PubMed] [Google Scholar]
- 58.Hsieh TC, Ma KH, Chao A. iNEXT: an R package for rarefaction and extrapolation of species diversity (Hill numbers) Methods Ecol. Evol. 2016;7:1451–1456. doi: 10.1111/2041-210X.12613. [DOI] [Google Scholar]
- 59.Alikhan NF, Petty NK, Ben Zakour NL, Beatson SA. BLAST Ring Image Generator (BRIG): simple prokaryote genome comparisons. BMC Genom. 2011;12:402. doi: 10.1186/1471-2164-12-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haukoos JS, Lewis RJ. The propensity score. Jama. 2015;314:1637–1638. doi: 10.1001/jama.2015.13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tingley, D., Yamamoto, T., Hirose, K., Keele, L. & Imai, K. mediation: R package for causal mediation analysis. J. Stat. Softw.10.18637/jss.v059.i05 (2014).
- 62.Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw.67, 48 (2015).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
The sequencing data generated in this study have been deposited in the Sequence Read Archive (SRA) database under accession code PRJNA789565. The human subjects data are available under restricted access for the protection of the rights and welfare of human research subjects. Deidentified human data are available under restricted access and can be obtained from MAB within 1 year upon request, pending approval from the University of Michigan Institutional Review Board. The remaining data generated in this study are provided in the Supplementary Information/Source Data file. Source data are provided with this paper.
All code developed for this manuscript is available at https://github.com/rdcrawford/Bachman_CU8.