Abstract
Background
Pneumonia, which is the third leading cause of death in South Korea, is continuously increasing with the aging society. The Health Insurance Review and Assessment of South Korea conducted a quality assessment (QA) for improving the outcome of community-acquired pneumonia (CAP).
Methods
We conducted a nationwide cross-sectional study of hospitalized CAP in South Korea. First to third QA data were gathered into a single database. The national health insurance database was merged with the QA database for analyzing the medical claims data. Comorbidities, pneumonia severity, and pneumonia care appropriateness were calculated using Charlson comorbidity index (CCI), CURB-65, and core assessment of CAP scores (CAP scores), respectively.
Results
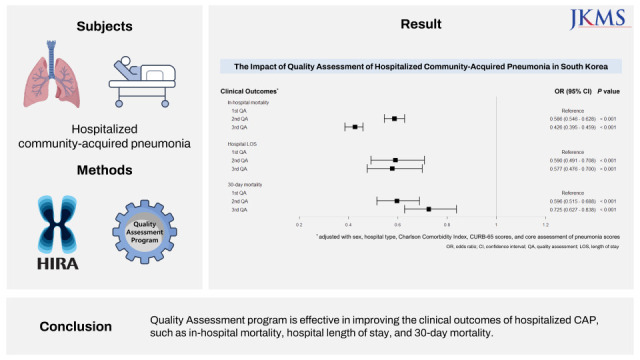
Overall, 54,307 patients were enrolled. The CAP scores significantly improved on QA program implementation (P < 0.001). All the variables demonstrated an association with in-hospital mortality, hospital length of stay (LOS), and 30-day mortality in the univariate analyses. Following the adjustments, higher CCI and CURB-65 scores were associated with higher in-hospital mortality, longer hospital LOS, and higher 30-day mortality. Male sex was associated with higher in-hospital/30-day mortality and shorter hospital LOS. Higher CAP scores were associated with shorter hospital LOS (P < 0.001). Upon QA program implementation, in-hospital mortality (P < 0.001), hospital LOS (P < 0.001), and 30-day mortality (P < 0.001) improved.
Conclusion
Continuing QA program is effective in improving the clinical outcomes of hospitalized CAP.
Keywords: Community-Acquired Infections, Pneumonia, Prognosis, Quality of Health Care
Graphical Abstract
INTRODUCTION
The global burden of pneumonia, which is the third leading cause of death in South Korea, is enormous.1,2,3 In 2018, 45.4 patients per 100,000 populations succumbed to pneumonia, which is approximately three times higher than that of 2010.4 Moreover, the mortality of pneumonia is steadily increasing owing to the change in the aging society.5 Approximately 257.6 patients of 100,000 individuals succumbed to pneumonia in the ≥ 65 years-old age group in Korea in 2018.4 Although, the social status of South Korea has evolved from a developing country to a developed country, pneumonia still remains a tremendous burden both on the socioeconomic status and public health.6
Most pneumonia are acquired in the community, so-called community-acquired pneumonia (CAP).7,8,9,10 Among them, the patients who need hospitalization were main burden of poor outcomes of CAP, such as mortality.11,12,13,14 In order to improve the clinical outcomes of CAP, the Health Insurance Review and Assessment Service (HIRA) of South Korea managed a nationwide quality assessment (QA) program for hospitalized CAP care since 2013. Until 2019, three times of QA period were successfully conducted, and related data was collected prospectively by the HIRA. The objective of this study was to evaluate the changes of clinical outcomes and to investigate the risk factors which are associated with poor outcomes by using the hospitalized CAP QA database.
METHODS
Data sources
The HIRA collaborated with the Korean Academy of Tuberculosis and Respiratory Diseases in developing the QA program.15 An official assignment of Joint Project on Quality Assessment Research was procured from the HIRA, and we were granted access to the QA database for analyzing the factors associated with the prognosis of CAP in South Korea. The QA database was collected and manipulated by the HIRA. The QA data tables contain demographic information of the patients with CAP as follows. 1) Age, 2) sex, 3) hospital type, 4) first visited route, 5) type of admitted room, 6) type of severity assessment tools of pneumonia and its scores (e.g., CURB-65 and pneumonia severity index), 7) smoking status and whether perform smoking cession education or not, 8) vaccination status of pneumococcus, 9) lists of antibiotics and its duration, and 10) treatment outcomes (hospital length of stay [LOS], in-hospital mortality, and 30-day mortality). They also contain several core measure scores for CAP.15
The HIRA is also responsible for evaluating all the Korean citizens’ medical claims data.16 South Korea has a well-established mandatory nationwide medical claims system, which included most of the medication and comorbidities. These are matched by anonymized join-key with QA database. We analyzed the comorbidities of patients from one year before the index time of admission owing to CAP in the HIRA database.
Study population
The QA database included the data reported from the three rounds of QA; 1st QA (October 2014–December 2014), 2nd QA (April 2016–June 2016), and 3rd QA (October 2017–December 2017). The patients who met the criteria of hospitalized CAP were enrolled. Inclusion and exclusion criteria were as follows.15
Inclusion criteria
1) Patients aged ≥ 18 years
2) Patients who had at least one diagnosis code of pneumonia (J10.x–J18.x and J20.x as primary or diagnosis within 2nd position) from the International Classification of Disease, Tenth Revision (ICD-10)
3) Patients who were treated using intravenous (IV) antibiotics for more than 3 days
4) Hospitals which claimed at least five cases of hospitalized CAP
Exclusion criteria
1) Patients who had the following conditions not meeting the criteria of CAP: a) hospital acquired pneumonia, b) ventilator-associated pneumonia, c) postoperative pneumonia, d) patients who had transferred from other health care facilities, and e) patients who were admitted to the hospital for more than 2 days in the recent 90 days
2) Patients who were not treated with IV antibiotics first at the hospitals, such as those who were transferred from other hospital with previous antibiotics use or who were not administered antibiotics within 72 hours of admission
3) Patients who were delayed appropriate treatment owing to inevitable causes such as emergent operation
4) Patients who had the following conditions: a) patients who were recently diagnosed with malignant cancer (≤ 3 months), b) patients who received chemo- or radiation therapy within 3 months, c) patients who take immunosuppressant agents, d) patients who were treated with high dose steroids with a composition greater than 20 mg/day (≥ 14 days), e) patients who regularly underwent dialysis, and f) patients who have human immunodeficiency virus or acquired immune deficiency syndrome
5) Hospitals which claimed less than 5 cases of hospitalized CAP
6) Patients who are in or transferred from nursing hospitals
Definition of class of hospitals in South Korea
Hospitals were classified into hospital, general hospital, and tertiary hospital according to their capacity based on the number of hospital beds and specialties, as defined by the Korean Health Law. Hospital is defined by a medical institution for hospitalized patients with 30–100 beds, general hospitals are defined as hospitals with more than 100 beds and at least seven specialty areas, and tertiary hospitals should have more than 500 beds with more than 20 specialty departments that serve as teaching hospitals to medical students and nurses.
Core Assessment of CAP score measurement
As mentioned above, the QA program include the scores that evaluate the appropriateness of pneumonia care. These scores were composed of 8 categories that represent the pattern of pneumonia treatment as follows: 1) oxygen assessment, 2) use of severity assessment of pneumonia, 3) sputum smear, 4) sputum culture, 5) blood culture before antibiotics, 6) antibiotics within 8 hours of arrival, 7) education of quit smoking, and 8) pneumococcal vaccination. These are calculated by the weighted values of each score and were summarized into total scores (0–10 points) (Supplementary Table 1).
Comorbidities
The Charlson comorbidity index (CCI) was calculated as stated in previous articles (Supplementary Table 2).17,18 It was based on the ICD-10 diagnosis codes for predicting the prognosis.19 The HIRA database was matched with the QA database one year prior from the incidence of each pneumonia case, and calculated from the lists of diagnosis.
Statistical analyses
We used the analysis of variance and χ2 test for independence to compare the differences in the continuous and categorical variables between the three groups. Simple and multiple linear regression analyses were used to determine the factors affecting the hospital LOS. Univariable and multivariable logistic regression analyses were used to evaluate the factors of in-hospital and 30-day mortality. A P value of < 0.05 was considered statistically significant. Post hoc tests were performed by the Bonferroni t-test. All the statistical analyses were performed using the SAS Enterprise Guide 6.1 (SAS Institute, Cary, NC, USA) and RStudio Team (2020) (RStudio: Integrated Development for R. RStudio, PBC, Boston, MA, USA; http://www.rstudio.com/).
Ethics statement
This study was approved by the Institutional Review Board of The Catholic University of Korea Yeouido St. Mary’s Hospital (approval No. SC19ZNDE0020). Informed consent was waived owing to the retrospective nature of the study.
RESULTS
Hospitalized CAP demographics
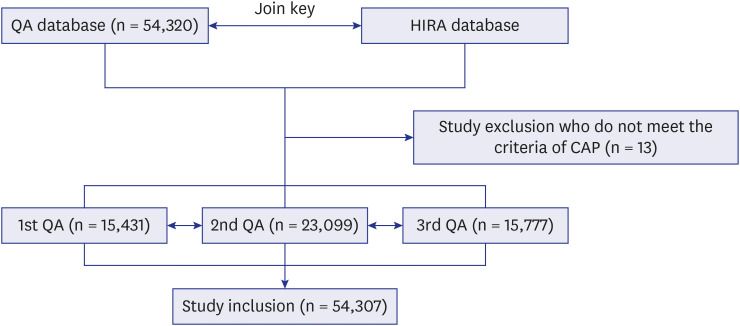
After excluding the cases based on the exclusion criteria, 54,307 patients were finally included (Fig. 1). Male predominance was found, and the mean age of the hospitalized CAP cases was mid-sixties with increasing upon the proceedings of the QA rounds (P < 0.001). Approximately 58.8% and 11.8% of the patients with CAP were admitted to general and tertiary hospitals, respectively. Severity of pneumonia was assessed by the CURB-65 (66.2%). The mean CURB-65 scores were higher in 3rd QA than 1st and 2nd QA on post hoc analyses (P < 0.001). Most frequent accompanying disease was chronic pulmonary disease (59.7%). Other common comorbid conditions were described in Supplementary Table 3. CCI scores were higher in the 3rd QA round than others (1st QA, 2.96 ± 2.04; 2nd QA, 2.91 ± 2.01; 3rd QA, 3.10 ± 2.11; P < 0.001). Approximately one fourth of the patients were current or ex-smokers. The status of pneumococcal vaccination increased with the proceeding of QA program (53.2% vs. 71.5% vs. 80.5%, P < 0.001). Details were summarized in Table 1 and Supplementary Table 3.
Fig. 1. Schematic diagram of the study. Both QA database and medical claims database were manipulated by the HIRA of South Korea. All the data were matched by anonymous join keys. From 1st to 3rd QA rounds, 54,307 hospitalized CAP cases were collected, after excluding the non-CAP cases.
QA = quality assessment, HIRA = Health Insurance Review and Assessment Service, CAP = community-acquired pneumonia.
Table 1. Demographics of hospitalized CAP in Korea.
| Total (n = 54,307) | 1st QA (n = 15,431) | 2nd QA (n = 23,099) | 3rd QA (n = 15,777) | P value | |
|---|---|---|---|---|---|
| Age, yr | 64.4 ± 18.9 | 65.2 ± 17.6 | 66.1 ± 17.7 | < 0.001 | |
| Male sex | 7,369 (47.8) | 10,682 (46.2) | 7,853 (49.9) | < 0.001 | |
| Hospital types | < 0.001 | ||||
| Tertiary | 1,666 (10.8) | 2,720 (11.8) | 2,024 (12.8) | ||
| General | 8,809 (57.1) | 13,766 (59.6) | 9,351 (59.3) | ||
| Hospital | 4,956 (32.1) | 6,613 (28.6) | 4,402 (27.9) | ||
| ER visit | 9,793 (63.5) | 14,677 (63.5) | 9,323 (59.1) | < 0.001 | |
| Admission room | < 0.001 | ||||
| GW | 14,042 (91.0) | 22,087 (95.6) | 14,919 (94.6) | ||
| ICU | 1,355 (8.8) | 998 (4.3) | 846 (5.4) | ||
| ER | 34 (0.2) | 13 (0.1) | 12 (0.1) | ||
| Severity index use | 8,977 (58.2) | 15,592 (67.5) | 11,890 (75.4) | < 0.001 | |
| CURB | 8,813 (57.1) | 15,442 (66.9) | 11,723 (74.3) | < 0.001 | |
| Score | 1.10 ± 1.05 | 1.11 ± 0.98 | 1.21 ± 0.99 | < 0.001 | |
| Confusion | 888 (10.1) | 1,881 (8.2) | 781 (5.0) | < 0.001 | |
| Urea > 20 mg/dL | 2,232 (14.5) | 5,333 (23.1) | 3,894 (24.7) | < 0.001 | |
| RR > 30 count/hour | 264 (1.7) | 590 (2.6) | 261 (1.7) | 0.687 | |
| SBP < 90 mmHg or DBP < 60 mmHg | 547 (3.5) | 1,216 (5.3) | 1,024 (6.5) | < 0.001 | |
| PSI | 92 (0.6) | 97 (0.4) | 106 (0.7) | 0.351 | |
| Score | 85.87 ± 37.82 | 66.95 ± 30.44 | 81.96 ± 29.69 | < 0.001 | |
| CCI, points | 2.96 ± 2.04 | 2.91 ± 2.01 | 3.10 ± 2.11 | < 0.001 | |
| Smoking status | 0.022 | ||||
| Current | 1,348 (12.9) | 2,093 (11.5) | 1,503 (11.6) | ||
| Ex (≤ 1 yr) | 217 (2.1) | 323 (1.8) | 213 (1.6) | ||
| Ex (> 1 yr) | 1,098 (10.5) | 1,920 (10.5) | 1,586 (12.2) | ||
| Never | 7,758 (74.5) | 13,889 (76.2) | 9,691 (74.6) | ||
| Pneumococcal vaccination | 4,663 (53.2) | 9,590 (71.5) | 7,665 (80.5) | < 0.001 | |
| Antibiotics | |||||
| Triple | 181 (1.2) | 219 (1.0) | 198 (1.3) | 0.476 | |
| Dual | 4,653 (30.2) | 6,988 (30.3) | 5,173 (32.8) | < 0.001 | |
| Single | 10,590 (68.7) | 15,883 (68.8) | 10,404 (66.0) | < 0.001 | |
| CAP scores, points | 6.54 ± 2.35 | 7.11 ± 2.18 | 7.54 ± 2.03 | < 0.001 | |
| Hospital LOS, days | 10.50 ± 6.88 | 9.68 ± 6.10 | 9.78 ± 6.07 | < 0.001 | |
| Outcome | < 0.001 | ||||
| Improved | 13,372 (87.0) | 21,081 (91.4) | 14,155 (89.8) | ||
| Transfer | 1,042 (6.8) | 1,223 (5.3) | 975 (6.2) | ||
| Death + Hopeless discharge | 960 (6.2) | 774 (3.4) | 637 (4.0) | ||
| 30-day mortality | 912 (5.9) | 666 (2.9) | 607 (3.9) | < 0.001 | |
Values are presented as number of patients (%) or mean ± standard deviation.
QA = quality assessment, ER = emergent room, GW = general ward, ICU = intensive care unit, RR = respiration rate, SBP = systolic blood pressure, DBP = diastolic blood pressure, PSI = pneumonia severity index, CCI = Charlson comorbidity index, CAP = community-acquired pneumonia, LOS = length of stay.
CAP changes by proceeding of QA program
Overall quality of CAP care, CAP scores, improved as the QA progressed (1st QA vs. 2nd QA vs. 3rd QA, 6.54 ± 2.35 vs. 7.11 ± 2.18 vs. 7.54 ± 2.03, respectively; P < 0.001). Antibiotic administration before 8 hours of hospital arrival (94.4%) and blood culture before initial administration of IV antibiotics (93.5%) were performed in most cases. Moreover, examination of the oxygen saturation (74.6%), sputum smear (73.1%), and sputum culture (75.5%) were assessed in more than 70% of the cases. However, the use of severity assessment tools (62.0%) and the evaluation of vaccination status (40.4%) were not performed frequently. Most of the hospitalized patients with CAP had not been educated regarding smoking cessation (10.5%) (Table 2).
Table 2. Core measures of QA of hospitalized CAP in South Korea.
| Core assessment | 1st QA (n = 15,431) | 2nd QA (n = 23,099) | 3rd QA (n = 15,777) | P value |
|---|---|---|---|---|
| Oxygenation assessment (≤ 24 hr) | 10,481 (67.9) | 17,249 (74.7) | 12,800 (81.1) | < 0.001 |
| Use of severity assessment tool (≤ 24 hr) | 7,975 (51.7) | 14,362 (62.2) | 11,312 (71.7) | < 0.001 |
| Sputum smear (≤ 24 hr) | 10,234 (66.3) | 17,397 (75.3) | 12,085 (76.6) | < 0.001 |
| Sputum cultures (≤ 24 hr) | 10,538 (68.3) | 17,887 (77.4) | 12,571 (79.7) | < 0.001 |
| Blood cultures prior to first antibiotics | 14,121 (91.5) | 21,662 (93.8) | 14,992 (95.0) | < 0.001 |
| First antibiotics administration (≤ 8 hr) | 14,241 (92.3) | 21,870 (94.7) | 15,147 (96.0) | < 0.001 |
| Smoking cessation education | 1,565 (10.1) | 2,416 (10.5) | 1,716 (10.9) | 0.034 |
| Screening of vaccination | 4,663 (30.2) | 9,590 (41.5) | 7,665 (48.6) | < 0.001 |
| CAP scores, points | 6.54 ± 2.35 | 7.11 ± 2.18 | 7.54 ± 2.03 | < 0.001 |
QA = quality assessment; CAP = community-acquired pneumonia.
Change of in-hospital mortality
Univariate and multivariate logistic regression analyses were performed to evaluate the effect of the variables in in-hospital mortality. Sex, hospital types, CURB-65 scores, CCI scores, CAP scores, and QA rounds were selected as variables. In the univariate analyses, all the variables demonstrated statistical difference on the in-hospital mortality. Male sex, higher CCI scores, higher CURB-65 scores, and higher CAP scores were associated with higher in-hospital mortality (P < 0.001). The hospital types showed higher in-hospital mortality in general or tertiary hospital than hospital (P = 0.005 and P < 0.001, each). After adjusting for the confounding factors in multivariate analyses, male sex (odds ratio [OR], 1.730; 95% confidence interval [CI], 1.635–1.831; P < 0.001) and higher CURB-65 scores (OR, 2.559; 95% CI, 2.479–2.641; P < 0.001) were associated with poor in-hospital mortality for hospitalized CAP. Higher level of hospital type (general hospital vs. hospital [OR, 1.315; 95% CI, 1.188–1.434; P = 0.001] and tertiary hospital vs. hospital [OR, 1.395; 95% CI, 1.242–1.568; P < 0.001]) was associated with poor in-hospital mortality also. Proceeding of QA rounds (2nd QA vs. 1st QA [OR, 0.586; 95% CI, 0.546–0.628; P < 0.001] and 3rd QA vs. 1st QA [OR, 0.426; 95% CI, 0.395–0.459; P < 0.001]) was associated with lower in-hospital mortality (Table 3).
Table 3. Univariate and multivariate logistic analyses of in-hospital mortality of hospitalized CAP in Korea.
| Characteristics | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Male sex | 1.903 (1.831–1.977) | < 0.001 | 1.730 (1.635–1.831) | < 0.001 | |
| Hospital types | |||||
| Hospital | Ref. | Ref. | Ref. | Ref. | |
| General hospital | 1.126 (1.078–1.176) | 0.005 | 1.315 (1.188–1.434) | 0.001 | |
| Tertiary hospital | 1.423 (1.335–1.516) | < 0.001 | 1.395 (1.242–1.568) | < 0.001 | |
| CCI scores | 1.246 (1.234–1.258) | < 0.001 | 1.149 (1.134–1.164) | < 0.001 | |
| CURB-65 scores | 2.875 (2.794–2.958) | < 0.001 | 2.559 (2.479–2.641) | < 0.001 | |
| CAP scores | 1.054 (1.045–1.063) | < 0.001 | 1.005 (0.981–1.031) | 0.505 | |
| QA | |||||
| 1st QA | Ref. | Ref. | Ref. | Ref. | |
| 2nd QA | 0.603 (0.577–0.630) | < 0.001 | 0.586 (0.546–0.628) | < 0.001 | |
| 3rd QA | 0.518 (0.493–0.545) | < 0.001 | 0.426 (0.395–0.459) | < 0.001 | |
OR = odds ratio, CI = confidence interval, CCI = Charlson comorbidity index, CAP = community-acquired pneumonia, QA = quality assessment.
Change in hospital stays
Simple and multiple linear regression analyses were performed to evaluate the associated factors with hospital LOS in hospitalized CAP. Sex, hospital type, CCI, CURB-65 scores, CAP scores, and QA rounds were selected as variables. Multi-collinearity between variables was not observed and significance was set at P < 0.001 in the analyses. In the simple linear regression analyses, all the variables were significantly associated with hospital LOS. However, the hospital type was not consistently associated with hospital LOS in the multiple linear regression analyses (general hospital vs. hospital [OR, 1.709; 95% CI, 1.411–2.070; P < 0.001] and tertiary hospital vs. hospital [OR, 0.766; 95% CI, 0.571–1.026; P = 0.074]). Male sex (exponentiation of the β coefficient [exp(β)], 0.761; 95% CI, 0.658–0.881; P < 0.001), higher CAP scores (exp(β), 0.866; 95% CI, 0.813–0.922; P < 0.001), and proceeding of QA program (2nd QA vs. 1st QA [exp(β), 0.590; 95% CI, 0.491–0.708; P < 0.001] and 3rd QA vs. 1st QA [exp(β), 0.577; 95% CI, 0.476–0.700; P < 0.001]) were associated with shorter hospital LOS. Higher CCI scores (exp(β), 1.190; 95% CI, 1.148–1.233; P < 0.001) and higher CURB-65 scores (exp(β), 3.551; 95% CI, 3.290–3.829; P < 0.001) were significantly associated with longer hospital LOS (Table 4).
Table 4. Simple and multiple linear regression analyses for the hospital length of stay in hospitalized CAP in Korea.
| Characteristics | Simple linear | Multiple linear | |||||
|---|---|---|---|---|---|---|---|
| β | Exp(β) (95% CI) | P value | β | Exp(β) (95% CI) | P value | ||
| Male sex | −0.452 | 0.636 (0.572–0.708) | < 0.001 | −0.273 | 0.761 (0.658–0.881) | < 0.001 | |
| Hospital types | |||||||
| Hospital | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |
| General hospital | 0.358 | 1.430 (1.207–1.695) | < 0.001 | 0.536 | 1.709 (1.411–2.070) | < 0.001 | |
| Tertiary hospital | −0.421 | 0.656 (0.546–0.788) | < 0.001 | −0.267 | 0.766 (0.571–1.026) | 0.074 | |
| CCI scores | 0.324 | 1.382 (1.343–1.423) | < 0.001 | 0.175 | 1.190 (1.148–1.233) | < 0.001 | |
| CURB-65 scores | 1.369 | 3.930 (3.686–4.190) | < 0.001 | 1.280 | 3.551 (3.290–3.829) | < 0.001 | |
| CAP scores | 0.0002 | 1.046 (1.021–1.072) | < 0.001 | −0.164 | 0.866 (0.813–0.922) | < 0.001 | |
| QA | |||||||
| 1st QA | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | |
| 2nd QA | −0.823 | 0.439 (0.386–0.499) | < 0.001 | −0.528 | 0.590 (0.491–0.708) | < 0.001 | |
| 3rd QA | −0.719 | 0.487 (0.423–0.560) | < 0.001 | −0.549 | 0.577 (0.476–0.700) | < 0.001 | |
Exp(β) = exponentiation coefficient β, CI = confidence interval, CCI = Charlson comorbidity index, CAP = community-acquired pneumonia, QA = quality assessment.
The 30-day mortality improvement
The 30-day mortality was defined by the index date of admission owing to hospitalized CAP, which was evaluated by the univariate and multivariate logistic regression analyses. Sex, hospital types, CURB-65, CCI, CAP scores, and QA rounds were selected as variables. Most variables, except comparing hospital type between general hospital and hospital, demonstrated the association with 30-day mortality in the univariate analyses (P < 0.001). In the multivariate analyses, male sex (OR, 1.214; 95% CI, 1.077–1.370; P < 0.001), hospital types (general hospital vs. hospital [OR, 1.302; 95% CI, 1.045–1.622; P = 0.019] and tertiary hospital vs. hospital [OR, 1.353; 95% CI, 1.056–1.734; P = 0.017]), CCI scores (OR, 1.035; 95% CI, 1.009–1.062, P = 0.008), CURB-65 scores (OR, 2.881; 95% CI, 2.725–3.045; P < 0.001), and proceeding QA program (2nd QA vs. 1st QA [OR, 0.596; 95% CI, 0.515–0.688; P < 0.001] and 3rd QA vs. 1st QA [OR, 0.725; 95% CI, 0.627–0.838; P < 0.001]) were still associated with the 30-day mortality (Table 5).
Table 5. Univariate and multivariate logistic analyses of 30-day mortality of hospitalized CAP in Korea.
| Characteristics | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Male sex | 1.413 (1.296–1.540) | < 0.001 | 1.214 (1.077–1.370) | < 0.001 | |
| Hospital types | |||||
| Hospital | Ref. | Ref. | Ref. | Ref. | |
| General hospital | 1.212 (0.987–1.489) | 0.067 | 1.302 (1.045–1.622) | 0.019 | |
| Tertiary hospital | 1.560 (1.241–1.960) | < 0.001 | 1.353 (1.056–1.734) | 0.017 | |
| CCI scores | 1.134 (1.112–1.155) | < 0.001 | 1.035 (1.009–1.062) | 0.008 | |
| CURB-65 scores | 3.010 (2.862–3.165) | < 0.001 | 2.881 (2.725–3.045) | < 0.001 | |
| CAP scores | 1.066 (1.045–1.088) | < 0.001 | 0.987 (0.936–1.041) | 0.635 | |
| QA | |||||
| 1st QA | Ref. | Ref. | Ref. | Ref. | |
| 2nd QA | 0.473 (0.427–0.523) | < 0.001 | 0.596 (0.515–0.688) | < 0.001 | |
| 3rd QA | 0.637 (0.573–0.708) | < 0.001 | 0.725 (0.627–0.838) | < 0.001 | |
OR = odds ratio, CI = confidence interval, CCI = Charlson comorbidity index, CAP = community-acquired pneumonia, QA = quality assessment.
DISCUSSION
Pneumonia is the most common infectious disease with enormous socioeconomic burden.2 Many efforts have been taken to enhance the quality of care for improving the clinical outcomes.20,21,22 This QA program was developed for these reasons. However, there is a lack of evidence supporting the importance of continuing QA program for hospitalized CAP.
Certain significant findings regarding the association between the QA program and the prognosis of hospitalized CAP were noted. First, the QA program revealed its efficacy in improving the prognosis of CAP. Clinical outcomes were improved upon the progress of the QA program even after adjusting the confounding factors. Hospital LOS was decreased with the proceeding of the QA program. The QA program contributes to reduce the mortality of hospitalized CAP in South Korea. Second, higher CAP scores were associated with better clinical outcomes. CAP score evaluates the appropriateness of medical care. It is associated with decreasing the hospital LOS after adjusting for the confounding factors. These results indicate the need for a high CAP score. Third, CAP scores improved based on the QA proceeding. It represents that the homogeneity and consistency of pneumonia care were improved in South Korea. Moreover, these results support that the well-organized management of pneumonia care is associated with improvement in the clinical outcomes of CAP. To the best of our knowledge, it is the first nationwide population-based study that reveals the importance of well-organized management in improving the prognosis of pneumonia. We anticipate this study to serve as basis for setting up public programs for pneumonia care in other countries. Fourth, pneumonia severity assessment, such as CURB-65, is a particularly important factor for estimating prognosis. Age also plays a key role; we evaluated the logistic regression analyses using two models, with CURB-65 scores or CURB scores, in the subgroup analyses; OR by CURB decreased greatly than that of CURB-65. Nevertheless, it still demonstrates the clinical significance. This indicates that aging contributes to the majority of poor prognoses. If patients were aged 1 year older, the in-hospital mortality (OR, 1.105) and 30-day mortality (OR, 1.094) were increased in the subgroup analyses (Supplementary Tables 4 and 5). It is well correlated with the report of Statistics Korea on the poor mortality of elderly society. Changing to aging society of super-aging society could probably continue to influence the prognosis of pneumonia in South Korea; thus, a proper guideline for hospitalized CAP in elderly patients is warranted. Fifth, we found that the tertiary or general hospital showed higher in-hospital mortality and 30-day mortality compared to that of hospital. Usually, the patients who are admitted to higher level of hospital types have more comorbidities, have more severe status of pneumonia, or were more aged people compared to those of hospital. However, current scoring system of pneumonia severity did not reflect patient factors, such as sex, CCI scores, and CURB-65 scores, that were associated with prognosis of CAP. Therefore, the severity of CAP must be classified using those variables. The development of more reasonable composite scoring systems is recommended with further supplementary research in near future.
There were several limitations to this study. First, the severe comorbid conditions that may be related to the increase of pneumonia or affected the disease severity, such as recently diagnosed caner (≤ 3 months), those treated with chemotherapy or radiation therapy recently (≤ 3 months), those with an immunodeficient condition or take immunosuppressant drugs, or those undergoing dialysis, were excluded. However, we can essentially evaluate the effect of sex, age, severity of pneumonia, and other comorbidities without the confounding conditions by excluding these factors since these conditions affect the development or prognosis of pneumonia. Second, there are no data on the microbiological findings. However, we included the patients without previous IV antibiotic use, without admission to other healthcare facilities more than two days within 3 months, and without hospital-acquired pneumonia. Therefore, the antibiogram of the patients in this study were anticipated as community-associated infection without risk of multi-drug resistant microorganisms. Considering further studies, the results of microbial culture should be included in the QA database. Third, seasonal effects can affect to the results of this study. Previous studies showed the different incidence and mortality of CAP by seasonal effect due to the different etiology, temperature, and etc.23,24 1st and 3rd QA were performed in fall/winter and 2nd QA was performed in spring season. Unless there are limitations from seasonal bias, we compared the clinical outcomes of 1st QA and 3rd QA (both at fall/winter) in multivariable analyses. Additional studies about seasonal effects to the clinical outcomes of CAP should be followed in upcoming QA analyses.
In conclusion, this study is the first nationwide cross-section study, which included the total hospitalized patients with CAP in South Korea. We reported the efficacy of the nationwide well-organized CAP care program in improving the prognosis of hospitalized CAP, and hope our study serves as a basis for future research.
ACKNOWLEDGMENTS
We thank the staff at the Quality Assessment Analysis Division of the Health Insurance Review and Assessment Service (HIRA) for providing the data. We would like to thank Editage (www.editage.co.kr) for English language editing.
Footnotes
Funding: This research was supported by the Health Insurance Review and Assessment Service (HIRA; HIRA research data number M20210128972). This research was supported by a grant of the Institute of Clinical Medicine Research in the Yeouido St. Mary’s Hospital, The Catholic University of Korea, Korea (grant number YSI 2020-20).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Jeong SH, Yoon HK.
- Data curation: Shim EK, Shin JH.
- Formal analysis: Lee YH, An TJ.
- Funding acquisition: Jeong SH.
- Investigation: Yoon HK, Myong JP.
- Methodology: Myong JP.
- Software: Lee YH, An TJ.
- Validation: Yoon HK, Myong JP, Kwon SO.
- Visualization: An TJ.
- Writing - original draft: An TJ.
- Writing - review & editing: An TJ, Yoon HK, Jeong SH.
SUPPLEMENTARY MATERIALS
Core assessment of CAP score measurement
Charlson weighted index of comorbidities
Post hoc analyses and details of comorbidities of hospitalized CAP in South Korea
Univariate and multivariate logistic analyses of in-hospital mortality of hospitalized CAP in Korea by CURB scores
Univariate and multivariate logistic analyses of 30-day mortality of hospitalized CAP in Korea by CURB scores
References
- 1.Prina E, Ranzani OT, Torres A. Community-acquired pneumonia. Lancet. 2015;386(9998):1097–1108. doi: 10.1016/S0140-6736(15)60733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(11):1191–1210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim HI, Kim SW, Chang HH, Cha SI, Lee JH, Ki HK, et al. Mortality of community-acquired pneumonia in Korea: assessed with the pneumonia severity index and the CURB-65 score. J Korean Med Sci. 2013;28(9):1276–1282. doi: 10.3346/jkms.2013.28.9.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Statistics Korea. Causes of Death Statistics in 2019. Daejeon, Korea: Statistics Korea; 2020. [Google Scholar]
- 5.Luna CM, Palma I, Niederman MS, Membriani E, Giovini V, Wiemken TL, et al. The impact of age and comorbidities on the mortality of patients of different age groups admitted with community-acquired pneumonia. Ann Am Thorac Soc. 2016;13(9):1519–1526. doi: 10.1513/AnnalsATS.201512-848OC. [DOI] [PubMed] [Google Scholar]
- 6.Yoon HK. Changes in the epidemiology and burden of community-acquired pneumonia in Korea. Korean J Intern Med. 2014;29(6):735–737. doi: 10.3904/kjim.2014.29.6.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heo JY, Seo YB, Choi WS, Lee J, Yoon JG, Lee SN, et al. Incidence and case fatality rates of community-acquired pneumonia and pneumococcal diseases among Korean adults: catchment population-based analysis. PLoS One. 2018;13(3):e0194598. doi: 10.1371/journal.pone.0194598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang JG, Ahn JH. Reasons and risk factors for readmission following hospitalization for community-acquired pneumonia in South Korea. Tuberc Respir Dis (Seoul) 2020;83(2):147–156. doi: 10.4046/trd.2019.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ko RE, Min KH, Hong SB, Baek AR, Lee HK, Cho WH, et al. Characteristics, management, and clinical outcomes of patients with hospital-acquired and ventilator-associated pneumonia: a multicenter cohort study in Korea. Tuberc Respir Dis (Seoul) 2021;84(4):317–325. doi: 10.4046/trd.2021.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeon EJ, Cho SG, Shin JW, Kim JY, Park IW, Choi BW, et al. The difference in clinical presentations between healthcare-associated and community-acquired pneumonia in university-affiliated hospital in Korea. Yonsei Med J. 2011;52(2):282–287. doi: 10.3349/ymj.2011.52.2.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohn JW, Park SC, Choi YH, Woo HJ, Cho YK, Lee JS, et al. Atypical pathogens as etiologic agents in hospitalized patients with community-acquired pneumonia in Korea: a prospective multi-center study. J Korean Med Sci. 2006;21(4):602–607. doi: 10.3346/jkms.2006.21.4.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi MJ, Song JY, Noh JY, Yoon JG, Lee SN, Heo JY, et al. Disease burden of hospitalized community-acquired pneumonia in South Korea: analysis based on age and underlying medical conditions. Medicine (Baltimore) 2017;96(44):e8429. doi: 10.1097/MD.0000000000008429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoon YK, Kim EJ, Chun BC, Eom JS, Park DW, Sohn JW, et al. Prescription of antibiotics for adults hospitalized with community-acquired pneumonia in Korea in 2004: a population-based descriptive study. Respirology. 2012;17(1):172–179. doi: 10.1111/j.1440-1843.2011.02077.x. [DOI] [PubMed] [Google Scholar]
- 14.Kim B, Myung R, Lee MJ, Kim J, Pai H. Trend of antibiotic usage for hospitalized community-acquired pneumonia cases in Korea based on the 2010-2015 national health insurance data. J Korean Med Sci. 2020;35(47):e390. doi: 10.3346/jkms.2020.35.e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong JY, Kang YA. Evaluation of the quality of care among hospitalized adult patients with community-acquired pneumonia in Korea. Tuberc Respir Dis (Seoul) 2018;81(3):175–186. doi: 10.4046/trd.2017.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim L, Kim JA, Kim S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol Health. 2014;36:e2014008. doi: 10.4178/epih/e2014008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.An TJ, Kim Y, Park YB, Kim K, Cho DY, Yoo KH, et al. Inhaled corticosteroid is not associated with a poor prognosis in COVID-19. Respirology. 2021;26(8):812–815. doi: 10.1111/resp.14108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park SC, Kim YS, Kang YA, Park EC, Shin CS, Kim DW, et al. Hemoglobin and mortality in patients with COPD: a nationwide population-based cohort study. Int J Chron Obstruct Pulmon Dis. 2018;13:1599–1605. doi: 10.2147/COPD.S159249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Chu LA, Bratzler DW, Lewis RJ, Murray C, Moore L, Shook C, et al. Improving the quality of care for patients with pneumonia in very small hospitals. Arch Intern Med. 2003;163(3):326–332. doi: 10.1001/archinte.163.3.326. [DOI] [PubMed] [Google Scholar]
- 21.Lee JS, Nsa W, Hausmann LR, Trivedi AN, Bratzler DW, Auden D, et al. Quality of care for elderly patients hospitalized for pneumonia in the United States, 2006 to 2010. JAMA Intern Med. 2014;174(11):1806–1814. doi: 10.1001/jamainternmed.2014.4501. [DOI] [PubMed] [Google Scholar]
- 22.Sinyangwe C, Graham K, Nicholas S, King R, Mukupa S, Källander K, et al. Assessing the quality of care for pneumonia in integrated community case management: a cross-sectional mixed methods study. PLoS One. 2016;11(3):e0152204. doi: 10.1371/journal.pone.0152204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang HH. Community-acquired pneumonia in elderly patients. Korean J Med. 2010;79(4):346–355. [Google Scholar]
- 24.Ferreira-Coimbra J, Sarda C, Rello J. Burden of community-acquired pneumonia and unmet clinical needs. Adv Ther. 2020;37(4):1302–1318. doi: 10.1007/s12325-020-01248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Core assessment of CAP score measurement
Charlson weighted index of comorbidities
Post hoc analyses and details of comorbidities of hospitalized CAP in South Korea
Univariate and multivariate logistic analyses of in-hospital mortality of hospitalized CAP in Korea by CURB scores
Univariate and multivariate logistic analyses of 30-day mortality of hospitalized CAP in Korea by CURB scores