Abstract
Purpose
In 2018, the Act to Improve Training Conditions and the Status of Medical Residents (AITR) was fully implemented in South Korea. This study aimed to investigate the effects of AITR implementation on the clinical outcomes of patients who underwent emergency abdominal surgery.
Materials and Methods
A total of 2571 patients who underwent emergency abdominal surgery after visiting the emergency room (ER) between 2015 and 2019 was included. Electronic medical records were retrospectively reviewed. In addition, a comparative analysis was performed for patient groups treated before and after AITR implementation.
Results
The median patient age was 48.0 years, and 49.2% of them were male. Appendicitis was the most common diagnosis (82.6%), followed by major abdominal emergencies (9.9%) and cholecystitis (7.5%). The median time from arrival to surgery was 439 min, and 52 (2.0%) patients died. A comparison of patients who underwent surgery before (pre-AITR; 1453, 56.5%) and after (post-AITR; 1118, 43.5%) AITR implementation revealed a significant difference in age, number of residents on a 24-h shift, and diagnosis. The time from ER arrival to surgery was not significantly longer after AITR implementation than before AITR implementation (434 min vs. 443 min, p=0.230). AITR was not a significant risk factor for mortality (p=0.225).
Conclusion
The time from ER arrival to emergency surgery did not increase significantly after AITR implementation, and there was no difference in the patients’ clinical outcomes.
Keywords: Preceptorship, internship and residency, patient safety, work schedule tolerance, general surgery
INTRODUCTION
Since medical resident training began at Johns Hopkins Hospital in 1889, the education and work of residents have drawn focus in many countries.1 People began to take interest in the working hours of medical residents after Libby Zion’s death in 1984 at 18 years of age due to a resident’s prescription error while he was on continuous duty.2 Since then, attention has been paid to misdiagnosis and patient safety due to the heavy workload of residents. In 1999, New York City enacted a law that limits the working hours of residents to 80 h per week. In 2003, the Accreditation Council for Graduate Medical Education (ACGME) extended the law on resident working hours across the United States.3
Similarly, in 2010, a 9-year-old died due to an error in the administration route of chemotherapy in South Korea. With the enactment of the Patient Safety Law, also known as the “Jonghyun Law” there has been a growing interest in limiting the working hours of residents4,5 to address concerns for the deterioration of patient safety due to an excessive workload and poor environment of medical residents in South Korea. In July 2015, a special law on the restriction of working hours for medical resident training was proposed. After several discussions, the law, officially called the Act to Improve Training Conditions and the Status of Medical Residents (AITR), was enacted in November 2017 and fully implemented in 2018.6
Prior to the enforcement of the AITR, there were studies on the introduction of an ideal method for limiting resident working hours and related patient outcomes. However, research after the implementation of AITR is limited.5,7,8,9 In addition, studies on post-AITR data focusing on surgery are extremely rare. In this study, we hypothesized that the implementation of the AITR would have affected clinical outcomes in patients undergoing emergency abdominal surgery and that there would be an observable change in the time from emergency room (ER) arrival to emergency operation after AITR implementation. Accordingly, this study aimed to investigate the effects of the AITR on the clinical outcomes and time from ER arrival to surgery in patients who underwent emergency abdominal surgery.
MATERIALS AND METHODS
Patient selection and data collection
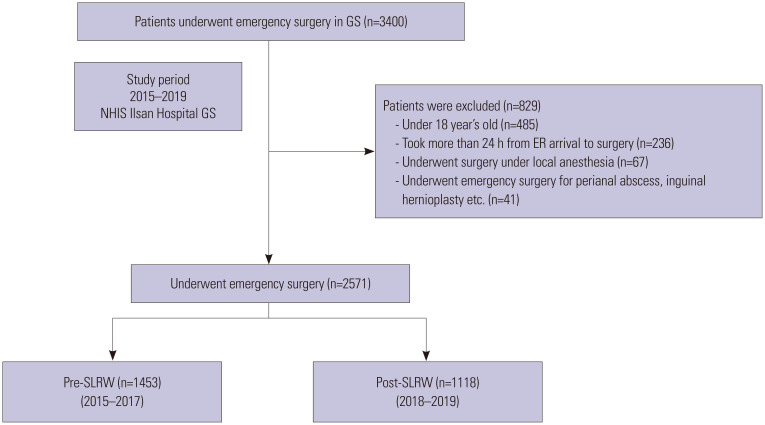
Our study included 3400 patients who underwent emergency abdominal surgery after visiting the emergency department of National Health Insurance Service Ilsan Hospital (NHISIH) between 2015 and 2019. The electronic medical records of the patients were retrospectively reviewed. A total of 2571 patients was enrolled, excluding patients under 18 years of age who underwent surgery >24 h after ER arrival and those who underwent surgery under local anesthesia. Patients with perianal abscesses and inguinal hernias were excluded (Fig. 1). Operations for patients with acute appendicitis and cholecystitis were considered minor emergency surgeries, while operations for conditions such as panperitonitis and bowel ischemia were considered major emergency surgeries.
Fig. 1. Flow chart showing the number of patients who underwent emergency abdominal surgery. NHIS, National Health Insurance Service; ER, emergency room; GS, Department of General Surgery; SLRW, special law on restriction of working hours in training.
Patient characteristics were compared between the patients who underwent surgery between 2015 and 2017 (pre-AITR) and those who underwent surgery between 2018 and 2019 (post-AITR). In addition, we analyzed the time from ER arrival to surgery, length of hospital stay, and death during hospitalization after AITR implementation. We confirmed the name of the resident on the 24-h shift based on the duty list submitted to the hospital. We confirmed initial laboratory test results and vital signs at the time of admission to the ER to establish the severity of disease; consequently, we performed a subgroup analysis according to the diagnosis.
Hospital setting
The present study was conducted at NHISIH, which is a secondary general hospital with 815 beds and is a medical resident training institution. The AITR has been applied in NHISIH since January 2018, limiting the working hours of residents to <80 h per week. Before the AITR was implemented, each resident worked 24-h shifts, three to four times a week, and after its implementation, each resident worked 24-h shifts, one to three times a week. The number of residents in the 24-h shift was determined according to the total number of residents and the day of the shift. Senior (3rd and 4th year) and junior (1st and 2nd year) residents were paired for a 24-h shift. From 7:00 am to 7:00 am the next day, the resident first examined the patient and then notified the on-call staff member. During the study period, day surgery was applied for surgery for appendicitis and cholecystitis. However, the surgeries could be delayed considering whether there was elective surgery the next day. Therefore, the decision of surgery was entirely dependent on the on-call surgeon.
AITR
The core contents of the AITR are as follows: first, the working hours of a resident must not exceed 80 h per week, on average, for 4 weeks. Second, the maximum continuous training is limited to 36 h. Third, a minimum of 10 h of rest should be guaranteed between consecutive training sessions. Fourth, leave pertaining to childbirth and abortion/stillbirth for female residents is stipulated in accordance with the Labor Standards Law. Fifth, 24 h of continuous rest should be guaranteed at least once per week. Failure to comply with the above criteria may result in fining the training institution or cancelation of the training hospital designation. In addition, a training environment evaluation committee under the Ministry of Health and Welfare should be established to implement a comprehensive resident training plan every 5 years.
Outcome measures
The primary endpoint of this study was a change in the clinical outcomes of patients who underwent emergency abdominal surgery after AITR implementation. In-hospital mortality and length of hospital stay were confirmed as clinical outcomes. The secondary endpoints were changes in the time from ER arrival to surgery before and after AITR implementation in patients who underwent emergency abdominal surgery and the independent effect of AITR on mortality. Moreover, the researchers confirmed the clinical outcomes before and after AITR implementation according to the diagnosis of the patient.
Statistical analyses
Continuous variables, expressed as median and interquartile range, were compared using Student’s t-test. Nominal variables were compared using the chi-squared test and Fisher’s exact test. In addition, a logistic regression analysis was performed to determine whether AITR was an independent risk factor for mortality. A p value of <0.05 at a 95% confidence interval (CI) was considered statistically significant. All analyses were performed using SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA).
Ethics statement
This study was approved by the Institutional Review Board (IRB) of National Health Insurance Service Ilsan Hospital (IRB approval no. NHIMC 2020-03-060) and adhered to the tenets of the Declaration of Helsinki. The requirement for informed consent was waived by the IRB of NHISIH owing to the retrospective nature of this study. All personal information of the study participants was de-identified.
RESULTS
Patient characteristics
The median age of the 2571 patients was 48.0 years (33.0–60.0) and 1265 (49.2%) were male. The number of patients who underwent emergency abdominal surgery was 474 (18.4%), 480 (18.7%), 501 (19.5%), 597 (23.2%), and 522 (20.3%) in 2015 to 2019, respectively. There were 1453 (56.5%) patients in the pre-AITR period and 1118 (43.5%) patients in the post-AITR period. The most common diagnoses for emergency abdominal surgery were acute appendicitis (82.6%), cholecystitis (7.5%), and major emergencies, such as panperitonitis (9.9%) (Table 1). The initial laboratory tests performed in the ER revealed the following: hemoglobin (Hb) level, 13.9 (12.8–15.2); white blood cell count, 12.07 (9.27–15.05); segmented neutrophil count, 79.0 (70.6–85.3); C-reactive protein (CRP) level, 2.09 (0.50–7.62); blood urea nitrogen (BUN) level, 12.40 (9.80–15.78); creatinine level, 0.76 (0.61–0.90); albumin level, 4.20 (3.90–4.50); and total bilirubin level, 0.97 (0.71–1.34). In addition, the average values of the initial vital signs on arrival were as follows: systolic blood pressure (SBP), 125 (113–139); pulse rate, 81 (71–91); and body temperature, 37.1 (36.7–37.5) (Table 1).
Table 1. Patient Characteristics (n=2571).
| Variables | Value | ||
|---|---|---|---|
| Age (yr) | 48.0 (33.0–60.0) | ||
| Sex (male) | 1265 (49.2) | ||
| Total patients consulted for GS in ER | |||
| 2015–2017 | 3480 | ||
| 2018–2019 | 2617 | ||
| Transfer to other hospital | |||
| 2015–2017 | 174 (5.0) | ||
| 2018–2019 | 104 (4.0) | ||
| Patient who underwent emergency surgery within 24 hr | |||
| Before AITR enforcement | 1453 (56.5) | ||
| After ATIR enforcement | 1118 (43.5) | ||
| Year | Total number of resident | Emergency surgery | |
| 2015 | 6 | 474 (18.4) | |
| 2016 | 6 | 480 (18.7) | |
| 2017 | 5 | 501 (19.5) | |
| 2018 | 6 | 597 (23.2) | |
| 2019 | 8 | 522 (20.3) | |
| Diagnosis | |||
| Appendicitis | 2124 (82.6) | ||
| Cholecystitis | 193 (7.5) | ||
| Major emergency surgery | 254 (9.9) | ||
| Laboratory test | |||
| Hemoglobin (g/dL) | 13.9 (12.8–15.2) | ||
| White blood cell count (103/uL) | 12.07 (9.27–15.05) | ||
| Neutrophil count (%) | 79.0 (70.6–85.3) | ||
| C-reactive protein (mg/dL) | 2.09 (0.50–7.62) | ||
| Blood urea nitrogen (mg/dL) | 12.40 (9.80–15.78) | ||
| Creatinine (mg/dL) | 0.76 (0.61–0.90) | ||
| Albumin (g/dL) | 4.20 (3.90–4.50) | ||
| Total bilirubin (mg/dL) | 0.97 (0.71–1.34) | ||
| Vital sign | |||
| Systolic blood pressure (mm Hg) | 125 (113–139) | ||
| Pulse rate (beats/min) | 81 (71–91) | ||
| Body temperature (°C) | 37.1 (36.7–37.5) | ||
| Number of residents on 24-hr shift | |||
| 1 | 492 (19.1) | ||
| 2 | 1778 (69.2) | ||
| 3 | 302 (11.7) | ||
| Time from ER arrival to surgery (min) | 439.0 (331.0–638.0) | ||
| Length of hospital stay (day) | 4 (4–6) | ||
| Mortality | 52 (2.0) | ||
AITR, Act to Improve Training Conditions and the Status of Medical Residents; ER, emergency room.
Data are presented as interquartile range or n (%).
There were two residents per 24-h shift in 69.2%, one in 19.1%, and three in 11.7% of the shifts. The median time from ER arrival to operation was 439.0 (331.0–638.0), and the median length of hospital stay was 4 (4–6). Fifty-two (2.0) patients died (Table 1).
Analysis of the impact of AITR application
The differences between the 1453 and 1118 patients who underwent surgery in the pre- and post-AITR period, respectively, were statistically significant, as were blood urea nitrogen level (p=0.020), total bilirubin level (p<0.001), number of residents per 24-h shift (p=0.004), and type of diagnosis. The median time from ER arrival to surgery in the post-AITR period was longer than that in the pre-AITR period, but the difference was not significant [434.0 (331.0–614.0) vs. 443.0 (333.0–672.0), p=0.230]. In addition, there were no significant differences in the length of hospital stay [4 (4–6) vs. 4 (3–6), p=0.761] and mortality [34 (2.3) vs. 18 (1.6), p=0.192] between the groups (Table 2).
Table 2. Comparison of Patient Characteristics Before and After AITR Implementation.
| Characteristics | Pre-AITR (n=1453) | Post-AITR (n=1118) | p value | |
|---|---|---|---|---|
| Age (yr) | 46 (33–58) | 49 (34–61) | 0.001 | |
| Sex (male) | 715 (49.2) | 550 (49.2) | >0.999 | |
| Laboratory test | ||||
| Hemoglobin <10 (g/dL) | 36 (2.4) | 36 (3.2) | 0.205 | |
| Abnormal WBC count (103/uL) | 1033 (71.3) | 758 (68.3) | 0.108 | |
| Neutrophil count >80 (%) | 660 (45.5) | 513 (46.3) | 0.721 | |
| C-reactive protein >1.0 (mg/dL) | 872 (61.0) | 699 (63.5) | 0.187 | |
| Blood urea nitrogen >20 (mg/dL) | 138 (9.6) | 137 (12.5) | 0.020 | |
| Creatinine >1.0 (mg/dL) | 215 (14.9) | 163 (14.8) | >0.999 | |
| Albumin <3.0 (g/dL) | 63 (4.4) | 37 (3.9) | 0.527 | |
| Total bilirubin >2.0 (mg/dL) | 113 (7.8) | 46 (4.2) | <0.001 | |
| Vital sign | ||||
| SBP <90 (mm Hg) | 27 (1.9) | 14 (1.3) | 0.224 | |
| Pulse rate >100 (bpm) | 164 (11.3) | 153 (13.7) | 0.067 | |
| Body temperature >37.8 (°C) | 234 (16.1) | 190 (17.0) | 0.547 | |
| Diagnosis | <0.001 | |||
| Appendicitis | 1238 (85.2) | 886 (79.2) | ||
| Cholecystitis | 65 (4.5) | 128 (11.4) | ||
| Major emergency surgeries | 150 (10.3) | 104 (9.3) | ||
| Number of residents on 24-hr shift | 0.004 | |||
| 1 | 301 (20.7) | 191 (17.1) | ||
| 2 | 966 (66.5) | 812 (72.6) | ||
| 3 | 186 (7.2) | 115 (10.3) | ||
| Time from ER arrival to surgery (min) | 434.0 (331.0–614.0) | 443.0 (333.0–672.0) | 0.230 | |
| Length of hospital stay (day) | 4 (4–6) | 4 (3–6) | 0.761 | |
| Mortality | 34 (2.3) | 18 (1.6) | 0.192 | |
AITR, Act to Improve Training Conditions and the Status of Medical Residents; ER, emergency room; SBP, systolic blood pressure.
Data are presented as interquartile range or n (%).
A comparative analysis of the survivors and non-survivors indicated significant differences between the two groups in terms of age, Hb <10 g/dL, neutrophil count >80%, CRP >1.0 mg/dL, BUN >20 mg/dL, creatinine >1.0 mg/dL, albumin <3.0 g/dL, SBP <90 mm Hg, pulse rate >100 bpm, diagnosis, and length of hospital stay (Supplementary Table 1, only online). Based on the significant factors, logistic regression analysis confirmed that age, creatinine >1.0 mg/dL, albumin <3.0 g/dL, and major emergency surgery were independent risk factors (Table 3). However, AITR [odds ratio, 0.660; 95% CI, 0.337–1.292; p=0.225] was not an independent risk factor for mortality (Table 3).
Table 3. Risk Factors Associated with Mortality.
| Variables | OR (95% CI) | p value | |
|---|---|---|---|
| Age | 1.049 (1.025–1.073) | <0.001 | |
| C-reactive protein >1.0 (mg/dL) | 2.115 (0.943–4.748) | 0.069 | |
| Creatinine >1.0 (mg/dL) | 2.087 (1.086–4.010) | 0.027 | |
| Albumin <3.0 (g/dL) | 2.396 (1.163–4.940) | 0.018 | |
| Diagnosis (reference appendicitis) | |||
| Cholecystitis | 0.643 (0.082–5.070) | 0.675 | |
| Major emergency surgery | 8.636 (3.884–19.202) | <0.001 | |
| AITR implementation | 0.660 (0.337–1.292) | 0.225 | |
AITR, Act to Improve Training Conditions and the Status of Medical Residents; OR, odds ratio; CI, confidence interval.
Logistic regression analysis included age, hemoglobin <10 g/dL, neutrophil count >80%, C-reactive protein >1.0 mg/dL, blood urea nitrogen >20 mg/dL, creatinine >1.0 mg/dL, albumin <3.0 g/dL, systolic blood pressure <90 mm Hg, pulse rate >100 bpm, and diagnosis.
Subgroup analysis by diagnosis
On performing a subgroup analysis of patients who underwent major emergency surgery, there was no statistically significant difference in the time from ER arrival to surgery [413.5 (292.8–558.5) vs. 409.0 (300.0–557.0), p=0.658] between the groups. Similarly, no significant difference was found between the groups in terms of length of hospital stay [13.5 (9.0–23.4) vs. 15.5 (9.0–25.5), p=0.597] and mortality [24 (16.0) vs. 15 (14.4), p=0.732] (Table 4).
Table 4. Subgroup Analysis of Patients Who Underwent Major Emergency Surgery.
| Variables | Pre-AITR (n=150) | Post-AITR (n=104) | p value | |
|---|---|---|---|---|
| Age (yr) | 68.0 (51.8–79.0) | 68.5 (53.0–79.8) | 0.792 | |
| Sex (male) | 81 (54.0) | 50 (48.1) | 0.353 | |
| Laboratory test | ||||
| Hemoglobin <10 (g/dL) | 17 (11.3) | 21 (20.2) | 0.052 | |
| Abnormal WBC (103/uL) | 94 (62.7) | 66 (63.5) | >0.999 | |
| Neutrophil count >80 (%) | 88 (58.7) | 60 (57.7) | 0.898 | |
| C-reactive protein >1.0 (mg/dL) | 91 (61.9) | 56 (53.8) | 0.202 | |
| Blood urea nitrogen >20 (mg/dL) | 61 (40.7) | 45 (43.3) | 0.679 | |
| Creatinine >1.0 (mg/dL) | 60 (40.0) | 40 (38.5) | 0.805 | |
| Albumin <3.0 (g/dL) | 45 (30.0) | 25 (24.0) | 0.296 | |
| Total bilirubin >2.0 (mg/dL) | 14 (9.3) | 4 (3.8) | 0.094 | |
| Vital sign | ||||
| SBP <90 (mm Hg) | 12 (8.0) | 7 (6.7) | 0.705 | |
| Pulse rate >100 bpm | 40 (15.7) | 36 (34.6) | 0.174 | |
| Body temperature > 37.8 (°C) | 22 (14.7) | 13 (12.5) | 0.622 | |
| Number of residents on 24-hr shift | 0.511 | |||
| 1 | 31 (20.7) | 16 (15.4) | ||
| 2 | 104 (69.3) | 75 (72.1) | ||
| 3 | 15 (10.0) | 13 (12.5) | ||
| Diagnosis | 0.891 | |||
| Hollow viscus perforation | 102 (68.0) | 69 (66.3) | ||
| Abdominal trauma | 9 (6.0) | 5 (4.8) | ||
| Bowel strangulation | 37 (24.7) | 28 (26.9) | ||
| Other* | 2 (1.3) | 2 (1.9) | ||
| Time from ER arrival to surgery (min) | 413.5 (292.8–558.5) | 409.0 (300.0–557.0) | 0.658 | |
| Length of hospital stay (day) | 13.5 (9.0–23.4) | 15.5 (9.0–25.5) | 0.597 | |
| Mortality | 24 (16.0) | 15 (14.4) | 0.732 | |
AITR, Act to Improve Training Conditions and the Status of Medical Residents; ER, emergency room; SBP, systolic blood pressure.
Data are presented as interquartile range or n (%).
*Foreign body removal, colostomy injury due to dog bite were included in other diagnosis.
In the subgroup analysis of patients who underwent minor emergency surgery, we found significant differences in age (p<0.001), number of residents per 24-h shift (p=0.003), and diagnosis (appendicitis: 95% vs. 87.4%; cholecystitis 5.0% vs. 12.6%; p<0.001) between the groups. However, as in major emergency surgery, there were no significant differences between the groups with respect to the time from ER arrival to surgery [436.0 (332.0–619.0) vs. 446.5 (336.0–685.0) min, p=0.169], length of hospital stay [4 (4–5) vs. 4 (3–5), p<0.316], and mortality [10 (0.8) vs. 3 (0.3), p=0.132] (Table 5).
Table 5. Subgroup Analysis of Patients Who Underwent Minor Emergency Surgery.
| Variables | Pre-AITR (n=1299) | Post-AITR (n=1005) | p value | |
|---|---|---|---|---|
| Age (yr) | 44 (31–55) | 48 (33–59.25) | <0.001 | |
| Sex (male) | 634 (48.7) | 500 (49.3) | 0.755 | |
| Laboratory test | ||||
| Hemoglobin <10 (g/dL) | 18 (1.4) | 15 (1.5) | 0.861 | |
| Abnormal WBC (103/uL) | 939 (72.3) | 692 (68.9) | 0.073 | |
| Neutrophil count >80 (%) | 572 (44.0) | 453 (45.1) | 0.618 | |
| C-reactive protein >1.0 (mg/dL) | 781 (60.9) | 643 (64.6) | 0.071 | |
| Blood urea nitrogen >20 (mg/dL) | 77 (6.0) | 92 (9.2) | 0.003 | |
| Creatinine >1.0 (mg/dL) | 155 (12.0) | 123 (12.4) | 0.790 | |
| Albumin <3.0 (g/dL) | 18 (1.4) | 12 (1.4) | >0.999 | |
| Total bilirubin >2.0 (mg/dL) | 99 (7.7) | 42 (4.2) | 0.001 | |
| Vital sign | ||||
| SBP <90 (mm Hg) | 15 (0.6) | 7 (0.7) | 0.256 | |
| Pulse rate >100 bpm | 124 (9.5) | 117 (11.5) | 0.114 | |
| Body temperature >37.8 (°C) | 212 (16.3) | 177 (17.5) | 0.449 | |
| Number of residents on 24-hr shift | 0.003 | |||
| 1 | 270 (20.7) | 175 (17.3) | ||
| 2 | 862 (66.2) | 737 (72.7) | ||
| 3 | 171 (13.1) | 102 (10.1) | ||
| Diagnosis | <0.001 | |||
| Appendicitis | 1238 (95.0) | 886 (87.4) | ||
| Cholecystitis | 65 (5.0) | 128 (12.6) | ||
| Time from ER arrival to surgery (min) | 436.0 (332.0–619.0) | 446.5 (336.0–685.0) | 0.169 | |
| Length of hospital stay (day) | 4 (4–5) | 4 (3–5) | 0.316 | |
| Mortality | 10 (0.8) | 3 (0.3) | 0.132 | |
AITR, Act to Improve Training Conditions and the Status of Medical Residents; ER, emergency room; SBP, systolic blood pressure.
Data are presented as interquartile range or n (%).
DISCUSSION
The effect of AITR on clinical outcomes, such as mortality and hospital stay (the primary endpoint of this study), was not statistically significant. Multivariate analysis also showed that AITR was not an independent risk factor for mortality. In addition, there was no statistically significant difference in the time from ER arrival to surgery after AITR implementation (the secondary endpoint of this study). In subgroup analyses of major and minor emergency surgeries, there were no significant differences in the time from ER arrival to surgery after AITR implementation. In addition, there were no significant differences in length of hospital stay or mortality before and after AITR implementation (Tables 4 and 5). It is also noteworthy that there were no significant differences in the time for ER arrival to surgery and clinical outcomes, even though the on-call staff for each disease group was different. Subgroup analysis for patients with appendicitis and cholecystitis was additionally performed to confirm changes by disease, but there were no clinical indicators showing a significant difference due to AITR implementation (Supplementary Table 2 and 3, only online). This suggests that the limitation of working hours of residents has not had a direct factor on delaying the treatment of urgent conditions or decreasing the quality of medical care.
The main contents of the medical resident work limit system implemented by the ACGME in 2003 were designed to limit the average working hours per week to ≤80 h and prohibit continuous work for >24 h, limit on-call duties to every third night, and provide at least a 24-h period off every 7 days.3,10 In line with this, various working models, such as night floating models and post-call models, were introduced in training institutions to limit the working hours of all residents.11 After discussing the issue of long working hours for residents in the United Kingdom in 1996, the working hours of medical residents were restricted according to the European Working Time Directive in 2009.12 This pattern soon expanded across Europe, and although the form and details of work vary among countries, the main aim was to limit the average overtime to 48 h per week, in addition to the detailed regulations proposed by the ACGME.13,14 There have been several studies in the United States and Europe on the effect of working time restrictions on patient clinical outcomes,1,11,14,15,16,17,18,19,20 and most have reported that limiting working hours for medical residents does not increase patient morbidity and mortality.18,19
Similar to training institutions in the United States, in South Korea, individual hospitals prepared for a decrease in the number of doctors due to AITR implementation in various ways.5,9 In a previous study, a night floating system was introduced, in which daytime and nighttime work did not overlap, and shifts lasted for 12 h. According to the study, the clinical outcomes of patients were not significantly different before and after AITR implementation. However, the response time to ER calls at night was significantly reduced.5 In the case of NHISIH, the same classical night on-call system was operated even after AITR implementation. The classical night on call system inevitably leads to an increase in the intensity of work of the resident’s night-shift time after AITR. To investigate the effect of the increased work intensity on patient clinical outcomes, when the ER arrival time was divided into regular time and night-shift time, there was no significant difference in the patients’ clinical outcomes according to the ER arrival time (Table 6). Also, there was no difference in the clinical outcomes of the two groups when the surgery start time was divided into regular time and night-shift time for comparative analysis (Table 6).
Table 6. Subgroup Analysis according to ER Arrival Time and Operation Start Time.
| ER arrival time | Operation start time | ||||||
|---|---|---|---|---|---|---|---|
| Day-time (n=1660) | Night-time (n=911) | p value | Day-time (n=1201) | Night-time (n=1370) | p value | ||
| Age (yr) | 49 (34–61) | 46 (32–57) | <0.001 | 47 (32–59) | 48 (34–60) | 0.027 | |
| Sex (male) | 794 (47.8) | 471 (51.7) | 0.060 | 593 (49.4) | 672 (49.1) | 0.870 | |
| Laboratory test | |||||||
| Hemoglobin <10 (g/dL) | 40 (2.4) | 31 (3.4) | 0.147 | 26 (2.2) | 45 (3.3) | 0.084 | |
| Abnormal WBC count (103/uL) | 1097 (66.5) | 694 (76.3) | <0.001 | 876 (73.3) | 915 (67.1) | 0.001 | |
| Neutrophil count >80 (%) | 737 (44.7) | 436 (48.0) | 0.112 | 565 (48.2) | 608 (44.6) | 0.176 | |
| C-reactive protein >1.0 (mg/dL) | 1159 (71.3) | 412 (45.5) | <0.001 | 677 (57.2) | 894 (66.4) | <0.001 | |
| Blood urea nitrogen >20 (mg/dL) | 183 (11.2) | 92 (10.2) | 0.442 | 122 (10.3) | 153 (11.3) | 0.404 | |
| Creatinine >1.0 (mg/dL) | 260 (15.9) | 118 (13.1) | 0.056 | 162 (13.6) | 216 (16.0) | 0.100 | |
| Albumin <3.0 (g/dL) | 65 (4.2) | 35 (4.2) | 0.991 | 45 (4.0) | 55 (4.3) | 0.710 | |
| Total bilirubin >2.0 (mg/dL) | 122 (7.4) | 37 (4.1) | 0.001 | 68 (5.7) | 91 (6.7) | 0.288 | |
| Vital sign | |||||||
| SBP <90 (mm Hg) | 23 (1.4) | 18 (2.0) | 0.253 | 21 (1.7) | 20 (1.5) | 0.560 | |
| Pulse rate >100 (bpm) | 200 (12.0) | 117 (12.6) | 0.558 | 157 (13.1) | 160 (11.7) | 0.284 | |
| Body temperature > 37.8 (°C) | 273 (16.4) | 151 (16.6) | 0.933 | 199 (16.6) | 225 (16.4) | 0.921 | |
| Diagnosis | <0.001 | <0.001 | |||||
| Appendicitis | 1422 (85.7) | 702 (77.1) | 959 (79.9) | 1165 (85.0) | |||
| Cholecystitis | 91 (5.5) | 102 (11.2) | 135 (11.2) | 58 (4.2) | |||
| Major emergency surgery | 147 (8.9) | 107 (11.7) | 107 (8.9) | 147 (10.7) | |||
| Number of residents on 24-h shift | 0.269 | 0.888 | |||||
| 1 | 321 (19.3) | 171 (18.8) | 225 (18.7) | 267 (19.5) | |||
| 2 | 1133 (68.3) | 645 (70.8) | 835 (69.5) | 943 (68.8) | |||
| 3 | 206 (12.4) | 95 (10.4) | 141 (11.7) | 160 (11.7) | |||
| AITR | 716 (43.0) | 402 (44.1) | 0.626 | 551 (45.9) | 567 (41.4) | 0.022 | |
| Surgery at night time | 1041 (62.7) | 329 (36.1) | <0.001 | ||||
| Night-time arrival at ER | 619 (51.5) | 1041 (76.0) | <0.001 | ||||
| Time from ER arrival to surgery (min) | 400 (322–515) | 599 (379–877) | <0.001 | 504 (348–841) | 411 (322–527) | <0.001 | |
| Length of hospital stay (day) | 4 (4–6) | 4 (4–6) | 0.616 | 4 (4–6) | 4 (4–6) | 0.021 | |
| Mortality | 36 (2.2) | 16 (1.8) | 0.477 | 19 (1.6) | 33 (2.4) | 0.137 | |
AITR, Act to Improve Training Conditions and the Status of Medical Residents; ER, emergency room; SBP, systolic blood pressure.
Data are presented as interquartile range or n (%).
Although AITR has been implemented, the total number of emergency abdominal surgical cases has not decreased, and the fact that there appears to be no difference in the clinical outcomes of patients could be considered the effect of additional manpower and resource input. In a study on the association between resident working hours and a medical emergency team (MET) that operated continuously for 24 h, there was no significant difference in the clinical outcomes of patients after restriction of resident working hours. However, the MET activation rate was significantly increased and was concentrated on weekends and holidays.9 This may be attributed to switching the workload of specialists to that of the MET. Our institution also hired a surgical hospitalist. In line with the AITR, a rapid response team was created in 2019, and the number of physician assistant nurses increased from four to five. Therefore, the absence of a difference in the clinical outcomes of patients after the implementation of AITR may have been influenced by the input of additional manpower and resources.
Recently, in the United States and Europe, where restrictions on working hours for residents were implemented nationwide before South Korea, attention has been paid to the results of strict restrictions on working hours for residents that lower their satisfaction with training.16,17,20 A randomized controlled trial of Flexibility In Duty-hour Requirements for Surgical Trainees (FIRST trial) was conducted in the United States, where the total working hours were unchanged, but detailed continuous working hours restrictions and rest time guarantees were flexibly operated. As a result, there was no significant difference in the clinical outcomes of the patients. However, in the flexible group, forced leave during surgery decreased, while the continuity of the patient’s treatment increased. This led to an improvement in overall training satisfaction as in this study and previous domestic studies.16 Similarly, in this study, there was no significant difference in the clinical outcomes of patients before and after AITR implementation, and additional studies focusing on effective resident education are needed. Meanwhile, however, the medical departments directly affected by the AITR are those dealing with emergency and critically ill patients, including general surgery. In South Korea, these departments face difficulties in recruiting residents every year. Therefore, for training institutions where it is difficult to recruit residents, the AITR could affect clinical outcomes. Therefore, we may need to consider implementing supportive systems in addition to the AITR.
This study had some limitations. First, it was a single-center, retrospective study. Multicenter research is needed because the number of residents and the method of operation of the resident program differ among hospitals. Second, there was no correction for hospital environment. The change in time from ER arrival to surgery may be the result of multiple factors under the influence of the emergency department, anesthesia department, and operating room. Third, the time taken from the arrival at the ER to consultation and the time taken from the request for consultation to the response were not reflected. After the AITR was applied, it was thought to be important to reflect this due to the limitation of the number of medical residents working in all departments, but it could not be confirmed. Finally, the working hours of the residents may not have been accurately observed. In fact, a study has reported that even in the United States, it is common for medical residents to work in hospitals with false-working hours because of an ethical dilemma regarding handoff.21 Similarly, in this study, there is a possibility that the actual working hours of the residents were not reflected because they were simply divided and compared before and after the implementation of the AITR. Despite these limitations, to the best of our knowledge, this study is meaningful in that it is the first to analyze clinical results after the full implementation of the AITR in South Korea. Additional multicenter prospective studies on this topic are warranted in the future.
ACKNOWLEDGEMENTS
This work was supported by National Health Insurance Service Ilsan Hospital grant NHIMC-2020-CR-043.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Sungho Lee and Ji Young Jang.
- Data curation: Sungho Lee, Ji Young Jang, Yeon Su Kim, and Kwanhoon Park.
- Formal analysis: Sungho Lee, Ji Young Jang, and MiWoo Lee.
- Funding acquisition: Ji Young Jang.
- Investigation: all authors.
- Methodology: Sungho Lee and Ji Young Jang.
- Project administration: Sungho Lee and Ji Young Jang.
- Resources: all authors.
- Software: Yeon Su Kim, Kwanhoon Park, and MiWoo Lee.
- Supervision: Sungho Lee, Ji Young Jang, and MiWoo Lee.
- Validation: Sungho Lee and Ji Young Jang.
- Visualization: Sungho Lee and Ji Young Jang.
- Writing—original draft: Sungho Lee, Ji Young Jang, Yeon Su Kim, and Kwanhoon Park.
- Writhing—review & editing: Sungho Lee and Ji Young Jang.
- Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIALS
Comparison of the Characteristics of Survivors and Non-Survivors
Subgroup Analysis of Patients with Appendicitis
Subgroup Analysis of Patients with Cholecystitis
References
- 1.Rosenbaum L, Lamas D. Residents’ duty hours--toward an empirical narrative. N Engl J Med. 2012;367:2044–2049. doi: 10.1056/NEJMsr1210160. [DOI] [PubMed] [Google Scholar]
- 2.McNoble DJ. Expanded liability of hospitals for the negligence of fatigued residents. J Leg Med. 1990;11:427–449. doi: 10.1080/01947649009510837. [DOI] [PubMed] [Google Scholar]
- 3.Whang EE, Mello MM, Ashley SW, Zinner MJ. Implementing resident work hour limitations: lessons from the New York State experience. Ann Surg. 2003;237:449–455. doi: 10.1097/01.SLA.0000059966.07463.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jo JH. Will sudden death of 9 years old boy lead to a new law for patient safety? [accessed on 2021 September 11]. Available at: http://ohmynews.com/NWS_Web/Mobile/at_pg.aspx?CNTN_CD=A0001852173#cb.%204081.
- 5.Yu HW, Choi JY, Park YS, Park HS, Choi Y, Ahn SH, et al. Implementation of a resident night float system in a surgery department in Korea for 6 months: electronic medical record-based big data analysis and medical staff survey. Ann Surg Treat Res. 2019;96:209–215. doi: 10.4174/astr.2019.96.5.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National congress of the Republic of Korea. Enforcement Regulations of the Act for Improving the Training Environment and Improving the Status of Medical resident. Ministry of Health and Welfare [Internet] [accessed on 2021 September 11]. Avalilable at: https://www.law.go.kr/LSW//lsInfoP.do?lsiSeq=177754&ancYd=20151222&ancNo=13600&efYd=20171223&nwJoYnInfo=N&efGubun=Y&chrClsCd=010202&ancYnChk=0#0000.
- 7.Heo R, Park CW, You CJ, Choi DH, Park K, Kim YB, et al. Does work time limit for resident physician affect short-term treatment outcome and hospital length of stay in patients with spontaneous intracerebral hemorrhage?: a two-year experience at a single training hospital in South Korea. J Cerebrovasc Endovasc Neurosurg. 2020;22:245–257. doi: 10.7461/jcen.2020.E2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim DJ, Kim SG. Comparative study of the operative experience of surgical residents before and after 80-hour work week restrictions. Ann Surg Treat Res. 2018;95:233–239. doi: 10.4174/astr.2018.95.5.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moon KM, Huh JW, Park S, Hong SB, Lim CM, Koh Y. Resident working hour restrictions increased the workload of the medical emergency team: a retrospective observational study. J Patient Saf. 2019;15:e94–e97. doi: 10.1097/PTS.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 10.Iglehart JK. Revisiting duty-hour limits--IOM recommendations for patient safety and resident education. N Engl J Med. 2008;359:2633–2635. doi: 10.1056/NEJMp0808736. [DOI] [PubMed] [Google Scholar]
- 11.Poulose BK, Ray WA, Arbogast PG, Needleman J, Buerhaus PI, Griffin MR, et al. Resident work hour limits and patient safety. Ann Surg. 2005;241:847–856. doi: 10.1097/01.sla.0000164075.18748.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cappuccio F, Miller MA, Lockley SW. Sleep, health, and society: from aetiology to public health. Oxford: Oxford University Press; 2010. [Google Scholar]
- 13.Dumon KR, Traynor O, Broos P, Gruwez JA, Darzi AW, Williams NN. Surgical education in the new millennium: the European perspective. Surg Clin North Am. 2004;84:1471–1491. viii. doi: 10.1016/j.suc.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Businger AP, Laffer U, Kaderli R. Resident work hour restrictions do not improve patient safety in surgery: a critical appraisal based on 7 years of experience in Switzerland. Patient Saf Surg. 2012;6:17. doi: 10.1186/1754-9493-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denson JL, McCarty M, Fang Y, Uppal A, Evans L. Increased mortality rates during resident handoff periods and the effect of ACGME duty hour regulations. Am J Med. 2015;128:994–1000. doi: 10.1016/j.amjmed.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 16.Bilimoria KY, Chung JW, Hedges LV, Dahlke AR, Love R, Cohen ME, et al. National cluster-randomized trial of duty-hour flexibility in surgical training. N Engl J Med. 2016;374:713–727. doi: 10.1056/NEJMoa1515724. [DOI] [PubMed] [Google Scholar]
- 17.Silber JH, Bellini LM, Shea JA, Desai SV, Dinges DF, Basner M, et al. Patient safety outcomes under flexible and standard resident duty-hour rules. N Engl J Med. 2019;380:905–914. doi: 10.1056/NEJMoa1810642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moonesinghe SR, Lowery J, Shahi N, Millen A, Beard JD. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients’ outcomes: systematic review. BMJ. 2011;342:d1580. doi: 10.1136/bmj.d1580. [DOI] [PubMed] [Google Scholar]
- 19.Jamal MH, Doi SA, Rousseau M, Edwards M, Rao C, Barendregt JJ, et al. Systematic review and meta-analysis of the effect of North American working hours restrictions on mortality and morbidity in surgical patients. Br J Surg. 2012;99:336–344. doi: 10.1002/bjs.8657. [DOI] [PubMed] [Google Scholar]
- 20.Landrigan CP, Rahman SA, Sullivan JP, Vittinghoff E, Barger LK, Sanderson AL, et al. Effect on patient safety of a resident physician schedule without 24-hour shifts. N Engl J Med. 2020;382:2514–2523. doi: 10.1056/NEJMoa1900669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter RO, Spooner J, Arbogast PG, Tarpley JL, Griffin MR, Lomis KD. Work hours restrictions as an ethical dilemma for residents: a descriptive survey of violation types and frequency. Curr Surg. 2006;63:448–455. doi: 10.1016/j.cursur.2006.06.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparison of the Characteristics of Survivors and Non-Survivors
Subgroup Analysis of Patients with Appendicitis
Subgroup Analysis of Patients with Cholecystitis