Abstract
Extended-care interventions have been demonstrated to improve maintenance of weight loss after the end of initial obesity treatment; however, it is unclear whether these programs are similarly effective for African American versus White participants. The current study examined differences in effectiveness of individual versus group telephone-based extended-care on weight regain, compared to educational control, in 410 African American (n=82) and White (n=328) adults with obesity (mean ± SD age=55.6±10.3years, BMI= 36.4±3.7kg/m2). After controlling for initial weight loss, multivariate linear models demonstrated a significant interaction between treatment condition and race, p=.048. Randomization to the individual telephone condition produced the least amount of weight regain in White participants, while the group condition produced the least amount of weight regain in African American participants. Future research should investigate the role of social support in regain for African American versus White participants and examine whether tailoring delivery format by race may improve long-term outcomes.
Keywords: Obesity, Weight loss, Extended-care, Health Disparities, Rural
Comprehensive lifestyle interventions serve as the first-line treatment for obesity (Jensen et al., 2014). Despite their overall effectiveness, research has demonstrated that these programs may not benefit all participants equally (Fitzgibbon et al., 2012; Tussing-Humphreys et al., 2013). Results from trials conducted over the last 20 years have indicated that African American participants, especially African American women, lose significantly less weight than White participants during the initial weight loss phase of these programs (Fitzgibbon et al., 2012; Goode et al., 2017; Hollis et al., 2008; Kumanyika et al.,1991; Tussing-Humphreys et al., 2013). This pattern is particularly concerning given that African American adults are disproportionally burdened by obesity and obesity-related health conditions (Hales et al., 2020; James et al., 2017). As of 2018, 49% of non-Hispanic Black and African American adults in the United States were estimated to have obesity, compared to 42% of non-Hispanic White adults (Hales et al., 2020).
After the end of initial weight loss programs, the provision of additional intervention contact via “extended-care” maintenance interventions have been demonstrated to prevent weight regain and improve long-term weight loss outcomes (Dombrowski, et al., 2014; Ross Middleton, et al., 2012). It is less clear, however, whether these programs are equally effective for African American versus White participants. Notably, evidence suggests that even though African Americans may lose less weight during initial weight-loss periods, they also regain less weight, such that some trials ultimately observed no differences in weight change by race at longer-term follow-up visits (Rickel et al., 2011; Stevens et al., 2001; Wing, 2004). Two studies have investigated whether there may be differential impact of extended-care provision on weight regain in African American versus White participants. Results from the Weight Loss Maintenance trial (Svetkey et al., 2008) demonstrated no interaction between race and treatment condition when investigating the impact of three extended-care conditions on weight regain two years after the end of a 6-month weight-loss program. In this study, participants randomized to receive a personal-contact based extended-care program regained significantly less weight than participants randomized to an interactive technology program or a self-directed program, regardless of race. In contrast, Rickel and colleagues (2011) found a significant race by condition interaction in a trial comparing extended-care delivered via in-person groups or individual telephone calls in rural women. Specifically, African American women maintained their initial weight losses regardless of randomization condition while White women who were randomized to receive extended-care support via in-person groups or individual telephone calls regained significantly less weight than White women randomized to an educational control condition.
Given the different pattern of results demonstrated in the Weight Loss Maintenance Trial (Svetkey et al., 2008) and the study by Rickel and colleagues (2011), it remains important to investigate whether there are differences in the impact of extended care programs by race. Examining differential responses to treatment may help identify treatment modalities that are equally or more efficacious between groups, which is critical to promoting health equity and overcoming historical racial disparities in weight management outcomes. For example, cultural differences (Blixen, et al., 2006), unequal access to resources (Bell, Kerr, & Young, 2019; Matthew & Brodersen, 2018), and/or experiences of racism (Aaron & Stanford, 2021; Cozier et al., 2014) may lead extended-care support and intervention content to be more or less beneficial for some groups. Thus, the current study examined the impact of three different extended-care conditions (individual telephone support, group telephone support, or educational control) on weight regain over 12 months in African American versus White participants living in rural areas. Given similarities in the sample (i.e., adults living in rural areas) and the extended-care modality (i.e., use of telephone calls), hypotheses were based on the pattern of results observed by Rickel and colleagues (2011). It was hypothesized that there would be a significant race by condition interaction, such that African American participants and White participants would demonstrate different patterns of regain by treatment condition. Specifically, it was hypothesized that randomization to either an individual or group-based extended care program would promote better weight-loss maintenance than the educational control condition for White participants, while there would be no difference in weight regain by condition in African American participants.
Research has attributed differences in outcomes to behavioral factors such as participant attendance and adherence, including self-monitoring (Milsom et al., 2011; Ross Middleton et al., 2012; Tussing-Humphreys et al., 2013); therefore, as a secondary aim, the current study examined differences by treatment condition and race in extended-care session attendance and adherence to program goals (e.g., self-monitoring of dietary intake and physical activity and achievement of dietary intake and physical activity goals). Following patterns observed in previous studies, we hypothesized a significant main effect for race such that White participants would have higher rates of attendance and adherence when compared to African American participants. Finally, we proposed to investigate whether there was a significant race by condition interaction for attendance and adherence, mirroring the pattern hypothesized for weight change.
Methods
The current study conducted secondary data analyses on data from the Rural Lifestyle Eating and Activity Program (Rural LEAP) trial (Perri et al., 2020). Rural LEAP was a randomized clinical trial designed to examine the impact of extended care programs for weight-loss maintenance in adults residing in rural communities (Perri et al., 2019). This community-based intervention included three phases: an initial weight-loss program (Phase 1; 4 months), an extended-care phase during which participants were randomized into one of three maintenance programs (Phase 2; 12 months), and a no-contact follow-up period (Phase 3; 6 months). Given that the current study aimed to examine differences in weight regain during the extended-care period, controlling for initial outcomes during the Phase 1 intervention, the current study used data collected during Phase 1 and Phase 2 of the Rural LEAP trial. Study protocol and procedures were reviewed and approved by the Institutional Review Board (IRB) at the University of Florida.
Participants
Participants in the current study were adults who were randomized within Phase 2 of the Rural LEAP study who self-identified as non-Hispanic and either Black/African American or White. Adults who identified as Hispanic were excluded given that Hispanic adults have demonstrated different outcomes in extended-care maintenance programs compared to both White and African American adults (West et al., 2019), and the small number of Hispanic adults that enrolled in the parent study (n=19) severely limited statistical power to investigate between group differences (Perri et al., 2020). Details on participant recruitment (including diagrams of participant flow) have been published previously (Perri et al., 2019, 2020).
Initial Intervention
During Phase 1 of Rural LEAP, all participants received a 16-week, standard behavioral weight-loss program. This program was conducted in person, in groups of 4-16 participants led by trained health coaches (Cooperative Extension Services family and consumer sciences extension agents or individuals with a bachelor’s or master’s degree in nutrition, exercise science, or psychology). Sessions lasted for approximately 90 minutes; session content was based on the lifestyle intervention used in the Diabetes Prevention Program (DPP Research Group, 2002), with modifications made to adapt content to address challenges commonly experienced by individuals from rural areas (e.g., traditional high-fat cooking styles and lack of community resources and exercise facilities) (Perri et al., 2008). Participants were provided with initial caloric goals ranging from 1,200 to 1,500 kcal/day, based on baseline weight, with the calorie goal being 1,200 kcal/day for participants weighing ≤ 113.6 kg and the goal being 1,500 kcal/day for participants weighing > 113.6 kg. Walking-based physical activity goals aimed at gradually increasing walking to 30 min/day above baseline levels. To facilitate these goals, participants were asked to keep daily logs of the types, amounts, and caloric values related to all foods and drinks consumed, along with steps walked each day, which were collected at each group intervention session.
Extended-Care Interventions
In Phase 2, participants who completed at least 50% of the Phase 1 intervention sessions and completed the Month 4 assessment visit were randomly assigned to one of three extended care conditions (individual telephone counseling, group telephone counseling, or an educational control condition). Participants randomized to receive individual telephone counseling called in to a teleconference line for a scheduled, 10-20 min one-on-one session with a health coach. Participants randomized to receive group telephone counseling called into a teleconference line for a scheduled, 60-min group session with a health coach and other participants from their Phase I group. Both individual and group calls occurred biweekly during months 5-10 and monthly during months 11-16, and sessions followed the same structure and included the same problem-solving focus and content. Sessions began with a review of progress toward previous goals and structured problem solving (e.g., see Perri et al., 2001; Perri, Nezu, & Viegener, 1992) to address any challenges reported in meeting these goals, followed by a discussion of a weight management education module and goal setting for changes in dietary intake and physical activity to be completed prior to the next session.
Participants randomized to the educational control condition received 18 weight-management education modules with the same content used in the telephone groups. The modules were delivered to participants via mail or email on the same schedule as the telephone contacts. Throughout Phase 2, all participants were asked to continue to keep daily logs of dietary intake, and to return these logs to their health coach using prepaid postage. During Phase 3, there was no contact between health coaches and participants.
Rural LEAP Trial Outcomes
Of the 528 participants who enrolled in the initial weight loss intervention, 445 attended at least 50% of the Phase 1 intervention sessions and were randomized to the extended-care trial (Perri et al., 2019). The 445 participants randomized to the Rural LEAP trial lost an average (mean ± SD) of −8.3 ± 4.9 kg during the initial weight loss program. Missing data during the trial were handled in two ways: using a missing-at-random (MAR) approach and a missing-not-at-random (MNAR) approach, which assumed that participants who did not return for assessment visits regained 0.3 kg/mo after dropping out; results were similar using both methods, and thus MAR results were presented (Perri et al., 2020). During Phase 2, the active extended-care period, participants randomized to the educational control condition experienced mean weight increases of 2.6% from the end of Phase 1, compared to smaller and non-significant changes of 1.3% for participants in the group telephone counseling condition and no changes (mean change of 0%) for participants in the individual telephone counseling condition.
Measures
Height was measured at baseline by study staff using a stadiometer. Weight was measured at each assessment time point by study staff, masked to randomization condition, using a calibrated, digital scale. Because the current study was aimed at investigating differences in weight-loss maintenance program outcomes between adults who identified as Black or African American versus adults who identified as White, and the maintenance program was discontinued after Phase 2, the current analyses focused on data collected during Phase 2 (Months 4 to 16) of the Rural LEAP trial. Attendance at individual and group sessions during Phase 2 was recorded by health coaches during each session. Adherence to self-monitoring dietary intake was assessed as the proportion of Phase 2 days in which the participant returned a completed log of foods/drinks consumed to their health coach (all logs including at least one meal were coded as “completed”). Achievement of caloric intake goals was based on participants’ self-reported assessment (yes or no) on these logs. For days when logs were not returned (or for incomplete days, when the type of quantity of foods consumed is missing for ≥ 1 meal), it was assumed that the caloric intake goal was not met.
Statistical Analyses
Analyses were conducted in R version 3.6.2. As preliminary analyses, t-tests and chi-squared tests were used to assess whether there were demographic differences between African American and White participants at study baseline (Month 0). As previous studies have demonstrated differences in initial weight loss (change in weight from Month 0 to Month 4) by race, a t-test was also used to assess whether there were differences in Phase 1 weight loss between African American and White participants. Multivariate normal models controlling for Phase 1 weight loss were used to investigate the impact of randomization condition and race over time. As preliminary analyses, these models were used to investigate individual effects of randomization condition and race on weight change from Month 4 to 16, after controlling for Phase 1 weight loss. For the primary aim, a log-likelihood ratio test was used to assess whether a model investigating weight change from Month 4 to Month 16 by randomization condition and race was significantly improved by the inclusion of an interaction term between randomization condition and race. Models assumed missing data were MAR given that analyses from the parent trial demonstrated highly similar results for models using both the MAR and the more conservative MNAR approach (Perri et al., 2020). Attendance and adherence data were substantially skewed; thus, for the secondary aim, non-parametric tests (e.g., Kruskal-Wallis tests) were used to assess differences in attendance and adherence to self-monitoring and dietary intake/activity goals from Month 4 to Month 16 by randomization condition and race, and to test the secondary hypothesis that there would be a significant interaction between randomization condition and race.
Results
Of the 445 participants included in the Rural LEAP trial, 410 identified as either Non-Hispanic African American or Black (n = 82) or Non-Hispanic White (n = 328) and were included in the current study. At study baseline, participants were (mean ± SD) 55.59 ± 10.25 years old and had BMIs of 36.44 ± 3.68 kg/m2; 82.0% of participants reported identifying as female. There were no statistically significant differences between African American and White participants in terms of baseline age, education level, or household income (see Table 1); however, African American participants were more likely than White participants to identify as female and had higher BMI at study baseline (prior to the initiation of the Phase1 weight-loss program). As a result, the final model investigating whether there was an interaction between race and condition controlled for both gender and baseline BMI.
Table 1.
Demographic and baseline characteristics of study participants, by race.
| Characteristics | African American n = 82 |
White n = 328 |
p |
|---|---|---|---|
| Age, years, mean (SD) | 53.96 (10.41) | 55.99 (10.19) | .114 |
| BMI, kg/m2, mean (SD) | 37.06 (3.51) | 35.94 (3.66) | .011 |
| Gender, n (%) | .001 | ||
| Male | 5 (6.10) | 69 (21.04) | |
| Female | 77 (93.90) | 259 (78.96) | |
| Education level, n (%) | .440 | ||
| High school degree or less | 39 (47.56) | 180 (54.88) | |
| Trade, vocational, or associate’s degree | 12 (14.63) | 38 (11.59) | |
| Bachelor’s degree or higher | 31 (37.80) | 110 (33.54) | |
| Household Income, n (%) | .057 | ||
| < $50,000 | 48 (58.54) | 145 (44.21) | |
| > $50,000 | 29 (35.37) | 162 (49.39) | |
| Unknown/Refused | 5 (6.10) | 21 (6.40) |
After completion of the Phase 1 initial weight loss-program, 140 participants (n = 28 African American, n = 112 White) were randomized to receive individual telephone counseling, 127 (n = 25 African American, n = 102 White) were randomized to receive group telephone counseling, and 143 (n = 29 African American, n = 114 White) were randomized to the educational control condition. A total of 392 participants (95.6%) attended the 10-month assessment visit and 375 (91.5%) attended the 16-month assessment visit; there were no differences in retention by intervention group, p = .224 or race, p = .484.
Initial Phase I Weight Loss Outcomes
Participants lost an average (mean ± SD) of −8.46 ± 5.04 kg during the non-randomized Phase I. There were no differences in Phase I weight loss by intervention group, p = .272. There were, however, significant differences in Phase I weight loss by race, such that African American participants lost significantly less weight than White participants (−6.42 ± 4.23 kg versus −8.97 ± 5.10, respectively), t(145.92) = 4.67, p < .001.
Weight Regain During Phase II
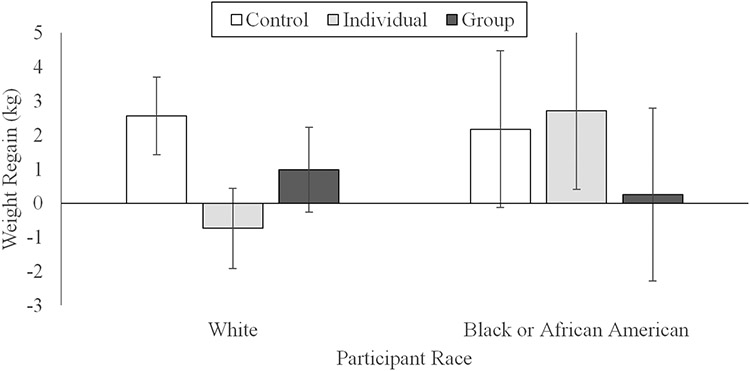
Table 2 provides mean body weights at each assessment by condition and race. After adjusting for Phase I weight losses, participants regained an average (mean ± SD) 1.14 ± 0.31 kg from Month 4 to 16, t(1144) = 3.65, p < .001. After additionally adjusting for gender and BMI, there was a significant impact of treatment condition, p = .003, such that participants in the control condition experienced a significant weight regain of 2.49 kg (95% CI: 1.47, 3.52) while participants in the individual and group conditions experienced non-significant weight regains of 0.02 kg (95% CI: −1.08, 1.03) and 0.84 kg (95% CI: −0.27, 1.96), respectively. Although there was not a significant difference in weight regain between African American participants (who regained, on average, 1.80 ± 0.71 kg) and White participants (who regained, on average, 0.97 ± 0.35 kg), p = .278, there was a condition by race interaction for weight regain from Months 4 to Month 16 (see Figure 1), χ2(1) = 6.07, p = .048. Specifically, White participants randomized to the control condition regained 3.31 kg more (95% CI: 1.69, 4.95) from Month 4 to Month 16 compared to White participants randomized to the individual condition, and 1.72 kg more (95% CI: 0.02, 3.43) than White participants randomized to the group condition. In contrast, there was not a significant difference in weight regain between conditions among African American participants. Decomposing this interaction within conditions, African American participants randomized to the individual condition regained 3.45 kg more (95% CI: −6.04, −0.86) from Month 4 to Month 16 than White participants randomized to this condition; however, there were not significant differences in weight regain between African American and White participants in the group or control conditions. Of note, the weight regains displayed in Figure 1 have been adjusted for initial weight loss, gender, and baseline BMI, and thus do not match differences over time calculated from the outcomes presented in Table 2.
Table 2.
Mean weights (kg) at each time point, by race and condition.
| African American |
White |
|
|---|---|---|
| Condition and Time | Mean (SD) | Mean (SD) |
| Individual Telephone | ||
| Baseline | 102.16 (2.88) | 99.09 (1.44) |
| Month 4 | 95.66 (2.87) | 89.99 (1.44) |
| Month 10 | 96.57 (2.88) | 88.13 (1.44) |
| Month 16 | 98.34 (2.89) | 89.25 (1.45) |
| Group Telephone | ||
| Baseline | 101.2 (3.04) | 102.47 (1.51) |
| Month 4 | 93.73 (3.04) | 93.24 (1.51) |
| Month 10 | 92.6 (3.06) | 92.23 (1.51) |
| Month 16 | 93.83 (3.08) | 94.26 (1.52) |
| Educational Control | ||
| Baseline | 95.63 (2.83) | 99.57 (1.42) |
| Month 4 | 90.22 (2.82) | 91.02 (1.42) |
| Month 10 | 89.78 (2.84) | 90.76 (1.43) |
| Month 16 | 92.36 (2.85) | 93.52 (1.43) |
Figure 1.
Model estimates, after controlling for initial weight loss, gender, and baseline BMI, of the weight regain (mean and 95% CI) experienced by Rural LEAP trial participants during the 12-month extended care intervention period, by race and randomized condition.
Attendance and Adherence During Phase II
Participants randomized to the individual condition attended more counseling sessions compared to participants randomized to the group condition (mean ± SD = 67.94 ± 27.16% versus 54.16 ± 27.94%, respectively), F(1,265) = 16.68, p < .0001. There was not, however, a statistically significant difference in attendance by race (African American participants attended an average of 55.03 ± 28.10% sessions compared to 62.95% ± 28.24% attended by White participants), p = .068, nor was there a significant interaction between randomization condition and race, p = .282.
There were significant differences between conditions in program adherence (i.e., the proportion of days that participants self-monitored caloric intake, met their calorie goals, self-monitored steps, and met their step goals; see Table 3). Specifically, participants in the individual condition self-monitored caloric intake on more days than participants in the control condition, p = .002, met their calorie goal on more days than participants in either the control or group conditions, p < .001 and p = .019, respectively, and self-monitored their steps on more days than participants in the control condition, p = .001. Participants in both the individual and group conditions met their step goals on more days than participants in the control condition, p = .001 and p = .038, respectively. No other between group differences were found, all ps > .05.
Table 3.
Phase 2 adherence to self-monitoring and program goals, by condition.
| Individual Telephone |
Group Telephone |
Educational Control |
||
|---|---|---|---|---|
|
n= 140 |
n = 127 |
n = 143 |
||
| Adherence Outcome | Mean (SD) | Mean (SD) | Mean (SD) | p |
| Self-Monitoring of Caloric Intake, % of days | 51.57 (37.01)a | 43.89 (36.15) | 35.50 (34.22) | <0.001 |
| Met Calorie Goal, % of days | 37.38 (32.32)a,b | 28.90 (29.26) | 24.09 (27.52) | <0.001 |
| Self-Monitoring of Steps | 50.00 (36.58)a | 42.08 (36.45) | 34.28 (34.50) | <0.001 |
| Met Step Goal, % of days | 31.78 (29.23)a | 24.40 (26.96)a | 18.43 (25.20) | <0.001 |
p < .05 versus control
p < .05 versus group
There were significant differences in program adherence by race. African American participants self-monitored their caloric intake and steps and met their calorie and step goals on fewer days than White participants (see Table 4). There were not any significant condition by race interactions for any of the adherence outcomes, all ps > .05.
Table 4.
Phase 2 adherence to self-monitoring and program goals, by race.
| African American | White | ||
|---|---|---|---|
|
n = 82 |
n = 328 |
||
| Adherence Outcome | Mean (SD) | Mean (SD) | p |
| Self-Monitoring of Caloric Intake, % of days | 30.66 (33.45) | 46.82 (36.34) | < .001 |
| Met Calorie Goal, % of days | 20.53 (27.14) | 32.51 (30.50) | < .001 |
| Self-Monitoring of Steps | 27.97 (32.10) | 45.59 (36.52) | < .001 |
| Met Step Goal, % of days | 17.09 (23.36) | 26.77 (28.35) | .002 |
Discussion
Results from the current study demonstrate that there may be important differences by race in the impact of extended-care programs, particularly by modality. Although White participants in the individual condition regained significantly less weight than White participants in the control condition, there was no difference in regain by extended-care condition for African American participants, mirroring the results of Rickel and colleagues (2011). Taken together, these results suggest that African American participants may not experience similar benefit from extended-care programs compared to White participants. Future research should focus on methods to improve the efficacy of extended-care programs for African American participants. Cultural tailoring may be particularly important (Fitzpatrick & Hill-Briggs, 2017; Kumanyika et al., 1991), and recent qualitative work has suggested that African American participants may benefit from community and/or family-based interventions that involve participants’ existing support systems (e.g., friends, family members; (Fitzpatrick & Hill-Briggs, 2017).
A novel finding of the current study was the unexpected differential pattern of results by race in relation to the effectiveness of the individual versus group telephone conditions. Visual inspection of Figure 1 demonstrates that randomization to the individual telephone condition produced the least amount of weight regain in White participants but the most in African American participants. In contrast, randomization to the group condition produced the least amount of weight regain in African American participants. Although there was not a statistically significant difference in weight regain between conditions in African American participants, the differences observed may be clinically meaningful, as they approach thresholds (~2 kg) found to be associated with improvements in metabolic outcomes such as fasting glucose, triglycerides, and HDL/LDL cholesterol (Jensen et al., 2014). This finding suggests that researchers and practitioners should consider how African American and White participants might respond differently to individual and group treatment sessions.
Group settings may be critical for facilitating lifestyle behavior change among African American women. A recent qualitative study aimed at investigating factors influencing weight loss in African American women who had completed a community-based Diabetes Prevention Program found that one of the most salient factors facilitating behavior change was group dynamics; which included the ability to share challenges without fear of judgement and feeling supported by group members and lifestyle coaches (O’Neal et al., 2021). Other qualitative studies have found that social support may play a key role in promoting both weight loss and successful maintenance in African American women (Fitzpatrick et al., 2017; Barnes et al., 2007; Eyler, 2003; Walcott-Mcquigg et al., 1995). Social support has been posited to promote higher levels of self-efficacy and perceived control for weight management behaviors in African American women (Wolfe, 2004), and may be a particularly important source of accountability and safety for engaging in physical activity (Eyler, 2003; Walcott-Mcquigg et al., 1995; Wolfe, 2004). It is possible that the group environment may better facilitate this ongoing positive support. In contrast, it may be that individual telephone calls provide better support for White participants. These individual calls may provide greater opportunity to discuss specific needs of individuals, and support sharing of challenges that a participant may be uncomfortable discussing in a group setting (Renjilian et al., 2001). Future research should investigate what aspects of group versus individual calls are most effective for supporting behavior change in African American versus White adults, and further investigate the role of social support, especially in group settings, on weight loss maintenance in African American adults.
Another key finding of the current study was that, contrary to hypotheses, the differential outcomes by race and condition could not simply be explained by intervention attendance or adherence alone. Despite the preponderance of literature supporting the roles of attendance and adherence to self-monitoring for promoting successful weight loss maintenance (Milsom et al., 2011; Ross Middleton et al., 2012; Tussing-Humphreys et al., 2013), the current results suggest that there may be other important factors driving the observed differential patterns in extended-care outcomes and the success of Africian American adults. Thus, future studies should investigate what other factors may drive differential patterns of weight regain between individual and group maintenance programs in African American versus White participants.
A key limitation of this study was the limited enrollment of African American versus White participants, potentially hampering ability to observe significant between-condition differences within African American participants. Although historically African American adults have been under-represented in weight management trials (McTigue et al., 2003), most trials of comprehensive weight management programs conducted since 2001 have enrolled, at minimum, a representative sample of African American participants (Goode et al., 2017). Few of these more recent trials report race-based outcomes, however, likely because recruitment of representative samples may still leave studies underpowered for these comparisons (Goode et al., 2017); as of 2020, it was estimated that only 14% of adults in the United States self-identified as Black or African American (United States Census Bureau, 2021). Thus, as the current study was a secondary analysis of existing trial data, it was likely underpowered to fully investigate differential impact of extended-care programs by race; however, the exploratory results of the current study support the importance of future, fully-powered randomized trials assessing whether extended-care programs differentially benefit African American versus White participants.
An additional limitation is that the length of the extended-care program was only 12 months, precluding investigations into longer-term outcomes. Finally, the parent trial recruited a sample of adults residing in rural areas, which limits generalizability to non-rural populations. Future studies should investigate whether these results replicate in other samples (e.g., samples including adults residing in urban and suburban areas) and whether delivery modality impacts the effectiveness of extended-care interventions for individuals in other racial/ethnic groups.
Despite these limitations, the current study also has several important strengths. Inference was strengthened by use of a randomized design in the parent study and by controlling for initial weight loss in the current study when investigating the impact of interventions on weight regain. Finally, the parent study was delivered in a community-based setting, allowing for the assessment of these interventions’ effectiveness under real-world conditions.
Conclusion
For high-risk populations, such as African American adults and rural adults with limited access to obesity treatment resources, comprehensive lifestyle interventions represent an opportunity to provide scalable and accessible community-based programs for weight management. Results from the current study have demonstrated, however, differential impacts of extended care modality on weight loss maintenance between African American and White adults. Future research should investigate potential causal mechanisms, including the role of social support for weight loss maintenance in African American adults, and investigate whether tailoring delivery format by race may improve long-term weight loss outcomes. Furthermore, future studies should include more equitable representation of African American participants and participants from other groups disproportionally impacted by obesity (e.g., Hispanic adults, adults living in rural areas; Hales et al., 2018) in order to investigate whether interventions are equally effective in these groups and, if not, to identify methods to improve program outcomes.
References
- Aaron DG, & Stanford FC (2021). Is obesity a manifestation of systemic racism? A ten-point strategy for study and intervention. Journal of Internal Medicine, 290(2), 416–420. 10.1111/JOIM.13270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes AS, Goodrick GK, Pavlik V, Markesino J, Laws DY, & Taylor WC (2007). Weight loss maintenance in African-American women: Focus group results and questionnaire development. Journal of General Internal Medicine, 22(7), 915–922. 10.1007/s11606-007-0195-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CN, Kerr J, & Young JL (2019). Associations between Obesity, Obesogenic Environments, and Structural Racism Vary by County-Level Racial Composition. International Journal of Environmental Research and Public Health 2019, Vol. 16, Page 861, 16(5), 861. 10.3390/IJERPH16050861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blixen CE, Singh A, Xu M, Thacker H, & Mascha E (2006). What women want: understanding obesity and preferences for primary care weight reduction interventions among African-American and Caucasian women. Journal of the National Medical Association, 98(7), 1160. Retrieved from /pmc/articles/PMC2569457/?report=abstract [PMC free article] [PubMed] [Google Scholar]
- Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, & Palmer JR (2014). Racism, Segregation, and Risk of Obesity in the Black Women’s Health Study. American Journal of Epidemiology, 179(7), 875–883. 10.1093/AJE/KWU004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, & Sniehotta FF (2014). Long term maintenance of weight loss with non-surgical interventions in obese adults: Systematic review and meta-analyses of randomised controlled trials. BMJ (Online), 348. 10.1136/bmj.g2646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyler A (2003). Quantitative study of correlates of physical activity in women from diverse racial/ethnic groups Women’s Cardiovascular Health Network Project introduction and methodology. American Journal of Preventive Medicine, 25(3), 5–14. 10.1016/S0749-3797(03)00159-4 [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, & Sharp LK (2012). Weight loss and African–American women: a systematic review of the behavioural weight loss intervention literature. Obesity Reviews, 13(3), 193–213. 10.1111/j.1467-789X.2011.00945.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick SL, & Hill-Briggs F (2017). Strategies for Sustained Weight Management: Perspectives From African American Patients With Type 2 Diabetes. Diabetes Educator, 43(3), 304–310. 10.1177/0145721717699071 [DOI] [PubMed] [Google Scholar]
- Goode RW, Styn MA, Mendez DD, & Gary-Webb TL (2017). African Americans in Standard Behavioral Treatment for Obesity, 2001-2015: What Have We Learned? Western Journal of Nursing Research, 39(8), 1045–1069. 10.1177/0193945917692115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, & Ogden CL (2018). Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. Journal of the American Medical Association, 319(23), 2419–2429. 10.1001/jama.2018.7270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Breif, no 360. Hyattsville, MD: National Center for Health Statistics. https://www.cdc.gov/nchs/products/databriefs/db360.htm [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, Champagne CM, Dalcin A, Erlinger TP, Funk K, Laferriere D, Lin P-H, Loria CM, Samuel-Hodge C, Vollmer WM, & Svetkey LP (2008). Weight Loss During the Intensive Intervention Phase of the Weight-Loss Maintenance Trial. American Journal of Preventive Medicine, 35(2), 118–126. 10.1016/j.amepre.2008.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James CV, Moonesinghe R, Wilson-Frederick SM, Hall JE, Penman-Aguilar A, & Bouye K (2017). Racial/Ethnic Health Disparities Among Rural Adults — United States, 2012–2015. MMWR. Surveillance Summaries, 66(23), 1–9. 10.15585/mmwr.ss6623a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, & Yanovski SZ (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology, 63(25 PART B), 2985–3023. 10.1016/j.jacc.2013.11.004 [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Obarzanek E, Stevens VJ, Hebert PR, & Whelton PK (1991). Weight-loss experience of black and white participants in NHLBI-sponsored clinical trials. The American Journal of Clinical Nutrition, 53(6), 1631S–1638S. 10.1093/ajcn/53.6.1631S [DOI] [PubMed] [Google Scholar]
- Matthew P, & Brodersen DM (2018). Income inequality and health outcomes in the United States: An empirical analysis. The Social Science Journal, 55(4), 432–442. 10.1016/J.SOSCIJ.2018.05.001 [DOI] [Google Scholar]
- McTigue KM, Harris R, Hemphill B, Lux L, Sutton S, Bunton AJ, & Lohr KN (2003). Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine, 139(11). 10.7326/0003-4819-139-11-200312020-00013 [DOI] [PubMed] [Google Scholar]
- Milsom VA, Middleton KMR, & Perri MG (2011). Successful long-term weight loss maintenance in a rural population. Clinical Interventions in Aging, 2011(6), 303–309. 10.2147/cia.s25389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neal LJ, Scarton L, & Dhar B (2021). Group social support facilitates adoption of healthier behaviors among black women in a community-initatied National Diabetes Prevention Program. Health Promotion Practice. 10.1177/15248399211045989 [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, & Viegener BJ (1992). Improving the long-term management of obesity: Theory, research, and clinical guidelines. John Wiley & Sons. https://psycnet.apa.org/record/1992-98264-000 [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, & Viegener BJ (2001). Relapse prevention training and problem-solving therapy in the long-term management of obesity. Journal of Consulting and Clinical Psychology, 69(4), 722–726. 10.1037/0022-006X.69.4.722 [DOI] [PubMed] [Google Scholar]
- Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, Dale MS, Daniels MJ, Radcliff TA, & Martin AD (2008). Extended-care programs for weight management in rural communities: The Treatment of Obesity in Underserved Rural Settings (TOURS) randomized trial. Archives of Internal Medicine, 168(21), 2347–2354. 10.1001/archinte.168.21.2347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perri MG, Ariel-Donges AH, Shankar MN, Limacher MC, Daniels MJ, Janicke DM, Ross KM, Bobroff LB, Martin AD, Radcliff TA, & Befort CA (2019). Design of the Rural LEAP randomized trial: An evaluation of extended-care programs for weight management delivered via group or individual telephone counseling. Contemporary Clinical Trials, 76, 55–63. 10.1016/j.cct.2018.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perri MG, Shankar MN, Daniels MJ, Durning PE, Ross KM, Limacher MC, … Befort CA (2020). Effect of Telehealth Extended Care for Maintenance of Weight Loss in Rural US Communities: A Randomized Clinical Trial. JAMA Network Open, 3(6), e206764. 10.1001/jamanetworkopen.2020.6764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, & Anton SD (2001). Individual versus group therapy for obesity: Effects of matching participants to their treatment preferences. Journal of Consulting and Clinical Psychology, 69(4), 717–721. 10.1037/0022-006X.69.4.717 [DOI] [PubMed] [Google Scholar]
- Rickel KA, Milsom VA, Ross KM, Hoover VJ, Peterson ND, & Perri MG (2011). Differential response of African American and Caucasian women to extended-care programs for obesity management. Ethnicity and Disease, 21(2), 170–175. [PMC free article] [PubMed] [Google Scholar]
- Ross Middleton KM, Patidar SM, & Perri MG (2012). The impact of extended care on the long-term maintenance of weight loss: A systematic review and meta-analysis. Obesity Reviews, 13(6), 509–517. 10.1111/j.1467-789X.2011.00972.x [DOI] [PubMed] [Google Scholar]
- Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, West DS, Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, & Cohen J (2001). Long-term weight loss and changes in blood pressure: Results of the trials of hypertension prevention, phase II. Annals of Internal Medicine, 134(1), 1–11. 10.7326/0003-4819-134-1-200101020-00007 [DOI] [PubMed] [Google Scholar]
- Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM, Vollmer WM, Gullion CM, Funk K,., Smith P, Samuel-Hodge C, Myers V, Lien LF, Laferriere D, Kenndy B, Jerome GJ Heinith F, Harsha DW, Evans P … Aicher K (2008). Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. JAMA, 299(10), 1139–1148. 10.1001/jama.299.10.1139 [DOI] [PubMed] [Google Scholar]
- The Diabetes Prevention Program (DPP) Reserach Group. (2002). The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care, 25(12), 2165–2171. 10.2337/diacare.25.12.2165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tussing-Humphreys LM, Fitzgibbon ML, Kong A, & Odoms-Young A (2013). Weight loss maintenance in African American women: A systematic review of the behavioral lifestyle intervention literature. Journal of Obesity, Vol. 2013, Article ID 437369, 31 pages. 10.1155/2013/437369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walcott-Mcquigg JA, Sullivan J, Dan A, & Logan B (1995). Psychosocial Factors Influencing Weight Control Behavior of African American Women. Western Journal of Nursing Research, 17(5), 502–520. 10.1177/019394599501700504 [DOI] [PubMed] [Google Scholar]
- West DS, Dutton G, Delahanty LM, Hazuda HP, Rickman AD, Knowler WC, … Cassidy Begay M (2019). Weight Loss Experiences of African American, Hispanic, and Non-Hispanic White Men and Women with Type 2 Diabetes: The Look AHEAD Trial. Obesity, 27(8), 1275–1284. 10.1002/OBY.22522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR (2004). Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obesity Research, 12(9), 1426–1434. 10.1038/oby.2004.179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe WA (2004). A review: maximizing social support--a neglected strategy for improving weight management with African-American women. Ethnicity & Disease, 14(2), 221–218. [PubMed] [Google Scholar]