Abstract
Study Design:
Original research, cross-sectional study.
Objectives:
Evaluate patient satisfaction with spine care delivered via telemedicine. Identify patient- and visit-based factors associated with increased satisfaction and visit preference.
Methods:
Telemedicine visits with a spine surgeon at 2 practices in the United States between March and May 2020 were eligible for inclusion in the study. Patients were sent an electronic survey recording overall satisfaction, technical or clinical issues encountered, and preference for a telemedicine versus an in-person visit. Factors associated with poor satisfaction and preference of telemedicine over an in-person visit were identified using multivariate logistic regression.
Results:
A total of 772 responses were collected. Overall, 87.7% of patients were satisfied with their telemedicine visit and 45% indicated a preference for a telemedicine visit over an in-person visit if given the option. Patients with technical or clinical issues were significantly less likely to achieve 5 out of 5 satisfaction scores and were significantly more likely to prefer an in-person visit. Patients who live less than 5 miles from their surgeon’s office and patients older than 60 years were also significantly more likely to prefer in-person visits.
Conclusions:
Spine telemedicine visits during the COVID-19 pandemic were associated with high patient satisfaction. Additionally, 45% of respondents indicated a preference for telemedicine versus an in-patient visit in the future. In light of these findings, telemedicine for spine care may be a preferable option for a subset of patients into the future.
Keywords: COVID-19, telemedicine, patient satisfaction, telehealth, spine surgery
Introduction
On March 11, 2020 the World Health Organization (WHO) declared COVID-19 a global pandemic. 1 Shortly thereafter, the United States federal government issued a proclamation reinforcing the immediate threat posed by COVID-19 and the need to enact safety measures. 2 Overnight, clinicians were tasked with providing routine care while avoiding direct contact with patients. To that end, orthopedic and spine providers rapidly introduced and expanded telemedicine programs through previously underutilized digital communication platforms.3-10
Prior to the COVID-19 pandemic, in-person visits were the standard in the United States for orthopedic care. However, in-person clinical visits can be impractical for patients who struggle with mobility or live in remote areas. The potential for telemedicine to improve access to care and reduce costs lead some practices to investigate telemedicine for orthopedic outpatient care, consultation, and rehabilitation even before the COVID-19 pandemic.11-24 These studies demonstrated that telemedicine visits are safe, feasible, associated with high patient satisfaction, and cost-effective in patients with orthopedic concerns.11,15-24
Previous studies included general orthopedic, pediatric orthopedic, sports medicine, arthroplasty, and trauma practices without large numbers of adult patients presenting to spine surgeons. The majority of these investigations focused on one aspect of clinical practice (ie, postoperative rehabilitation, remote consultation with provider present, postoperative visit, etc). Furthermore, some authors have questioned whether telemedicine would be well tolerated by adult spine patients and providers.13,15
Given that telemedicine offerings may persist into the future, it is important to assess spine patient satisfaction with the platform and identify related factors. Patient satisfaction is important to maintaining a successful practice and increases orthopedic patient follow-up. 25 As our outpatient spine practices shifted to telemedicine during the COVID-19 pandemic, we sought to investigate patient satisfaction with telemedicine and identify factors associated with satisfaction and preference for future telemedicine visits.
Materials and Methods
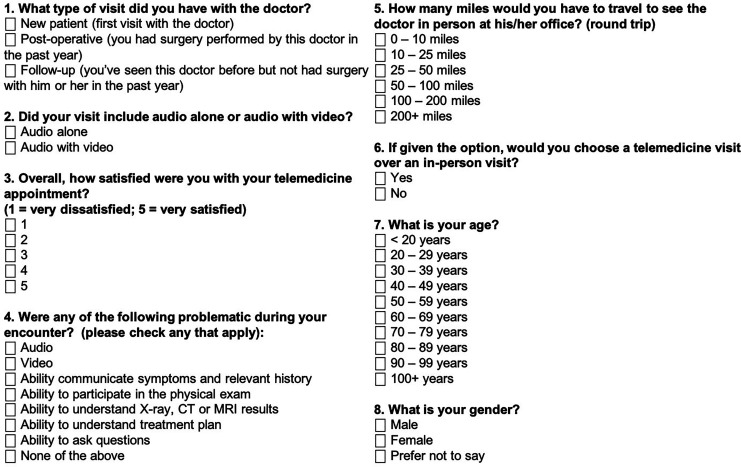
Each site individually obtained institutional review board (IRB) approval prior to contacting patients and initiating data collection. This study included patients from 2 private practices based in Philadelphia, Pennsylvania and Plano, Texas. Patients who had a telemedicine visit with a spine surgeon from March 16, 2020 through May 16, 2020 were identified from the electronic medical record. Visits were conducted by telephone or webcam-based platform at the discretion of the treating surgeon. A total of 27 spine surgeons provided telemedicine visits. Each patient was contacted electronically (email or text) via an IRB-approved message containing a link to a voluntary and anonymous web-based survey (Alphabet Inc). After obtaining informed consent, patients were instructed to complete the survey for their telemedicine visit(s) during the study period. The survey consisted of 8 questions based on prior telemedicine survey-based studies. 16 Patient satisfaction was measured using a 5-point Likert-type scale. Additional questions were designed to assess patient demographics and preference for future visits (Figure 1).
Figure 1.
Eight-question survey sent to patients after their telemedicine visit.
Statistical analysis was performed using Stata version 13.1 (StataCorp LP). Chi-square analyses were used to compare patients based on site, overall satisfaction score 4 out of 5 and below versus 5 out of 5), and on the preference of a telemedicine visit over an in-person visit. Patient and telemedicine visit characteristics were tested for association with satisfaction and telemedicine preference using multivariate regression models, which selected variables in a backward stepwise fashion. Variables with the highest P value were sequentially removed until only those with P values <.200 remained in the model. Multivariate regressions controlled for potential confounding variables to identify independent risk factors for each outcome. All tests were 2-tailed, and the statistical difference was established at a 2-sided alpha level of .05 (P < .05).
No outside funding was utilized to perform this study.
Results
During the first 2 months of the COVID-19 stay at home order, a total of 3120 patients had 3510 telemedicine visits at the 2 institutions included in the study. Final analysis included 772 responses (21.9% response rate) with a similar response rate at both institutions (23% vs 20%, P = .12). The median age range of the survey cohort was 60 to 69 years with the majority of the patients being female (53.8%). There was a relatively even distribution of patients by age category and visit type (Table 1). Primary outcomes included failure to achieve 5 out of 5 satisfaction with telemedicine and a preference to use telemedicine for future visits.
Table 1.
Patient and visit characteristics by site.
| All patients | Site A | Site B | P | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Overall | 772 | 100.0 | 501 | 64.9 | 271 | 35.1 | |
| Visit type | |||||||
| New | 183 | 23.7 | 116 | 23.2 | 67 | 24.7 | .625 |
| Follow-up | 267 | 34.6 | 201 | 40.1 | 66 | 24.4 | <.001 |
| Postoperative | 322 | 41.7 | 184 | 36.7 | 138 | 50.9 | <.001 |
| Audio only | 253 | 32.8 | 46 | 9.2 | 207 | 76.4 | <.001 |
| Miles | |||||||
| 0-10 | 210 | 27.2 | 137 | 27.4 | 73 | 26.9 | .903 |
| 10-25 | 229 | 29.7 | 136 | 27.2 | 93 | 34.3 | .037 |
| 25-50 | 128 | 16.6 | 79 | 15.8 | 49 | 18.1 | .410 |
| 50-100 | 75 | 9.7 | 48 | 9.6 | 27 | 10.0 | .864 |
| 100+ | 128 | 16.6 | 99 | 19.8 | 29 | 10.7 | .001 |
| Age, years | |||||||
| <50 | 151 | 19.6 | 100 | 20.0 | 51 | 18.8 | .703 |
| 50-59 | 173 | 22.4 | 117 | 23.4 | 56 | 20.7 | .392 |
| 60-69 | 235 | 30.4 | 155 | 30.9 | 80 | 29.5 | .683 |
| 70+ | 204 | 26.4 | 121 | 24.2 | 83 | 30.6 | .051 |
| Male sex | 356 | 46.1 | 219 | 43.7 | 137 | 50.6 | .069 |
| Problems | |||||||
| Audio | 75 | 9.7 | 67 | 13.4 | 8 | 3.0 | <.001 |
| Video | 89 | 11.5 | 51 | 10.2 | 38 | 14.0 | .111 |
| History | 38 | 4.9 | 18 | 3.6 | 20 | 7.4 | .020 |
| Exam | 104 | 13.5 | 56 | 11.2 | 48 | 17.7 | .011 |
| Imaging | 33 | 4.3 | 13 | 2.6 | 20 | 7.4 | .002 |
| Treatment plan | 30 | 3.9 | 16 | 3.2 | 14 | 5.2 | .176 |
| Asking questions | 32 | 4.2 | 21 | 4.2 | 11 | 4.1 | .930 |
| Number of problems | |||||||
| 0 | 523 | 67.8 | 344 | 68.7 | 179 | 66.1 | .459 |
| 1 | 162 | 21.0 | 107 | 21.4 | 55 | 20.3 | .729 |
| 2 | 49 | 6.4 | 30 | 6.0 | 19 | 7.0 | .578 |
| 3+ | 38 | 4.9 | 20 | 4.0 | 18 | 6.6 | .104 |
| Prefer telehealth | 346 | 44.8 | 243 | 48.5 | 103 | 38.0 | .005 |
| 5/5 satisfaction | 535 | 69.3 | 384 | 76.7 | 151 | 55.7 | <.001 |
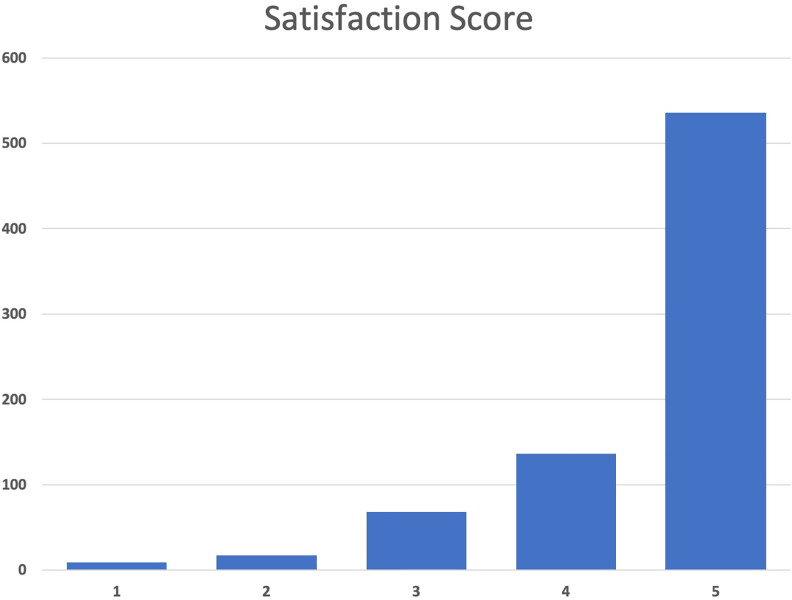
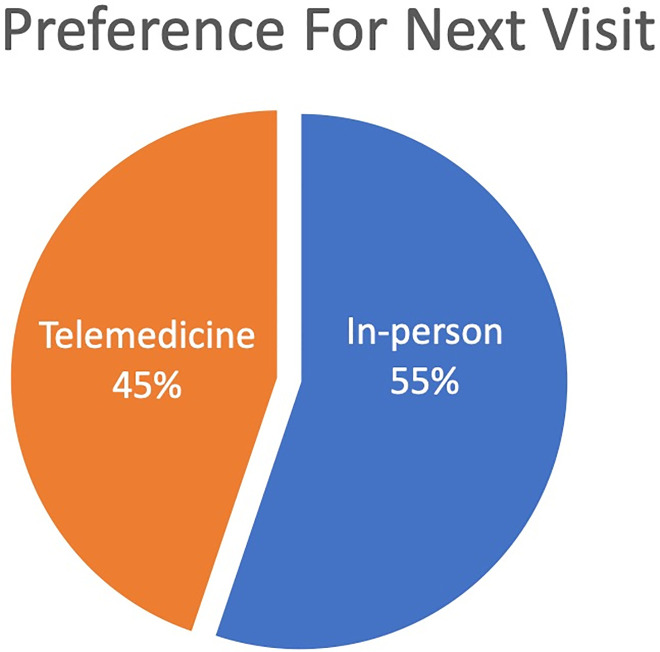
Overall, 87.7% of patients reported that they were satisfied with their telemedicine visit with 70% reporting a score of 5 out of 5 (“very satisfied”) (Figure 2), and 45% of patients stated that they preferred a telemedicine visit compared with an in-person visit (Figure 3). One-third of patients reported an issue with their telemedicine encounter—difficulty with exam was the most common issue, followed by problems with video and audio (13.5%, 11.5%, and 9.7%, respectively). With regard to mileage saved by a telemedicine visit, the majority of patients (56.9%) were within 25 miles round trip of their doctor’s office with a smaller subset of patients traveling over 100 miles (16.6%).
Figure 2.
Distribution of patient satisfaction scores.
Figure 3.
Preference for next visit if given the choice between in-person visit and telemedicine visit.
Patient and Visit Characteristics by Institution
On bivariate analysis, there were several statistically significant differences between the 2 institutions that participated in this study (Table 1). Site B had a significantly greater percentage of audio-only encounters (76.4% vs 9.2%, P < .001). There was also a significant difference in visit types between institutions specifically for follow-ups and postoperative visits. Site B also had a greater percentage of patients that would have traveled 10 to 25 miles (34.3% vs 29.7%, P = .037), whereas site A had a greater percentage of patients who would have traveled over 100 miles (19.8% vs 10.7%, P = .001). Most notably, there was a greater percentage of patients at site A who reported a 5 out of 5 satisfaction score (76.7% vs 55.7%, P < .001) and who preferred telemedicine for their next appointment (48.5% vs 38%, P = .005).
Patient and Visit Characteristics Associated With 5 out of 5 Satisfaction Scores
Bivariate analysis revealed that visit type or mileage did not play a significant role in achieving satisfaction scores. However, those who had audio only for the telemedicine visit were significantly less likely to be very satisfied (Table 2). Patients who did not have any problems were significantly more likely to be very satisfied with their telemedicine visit, whereas patients with one or more problems were significantly more likely to have a lower satisfaction score. Similarly, when looking at the individual types of problems, when any technical or clinical problem was reported, patients were significantly less likely to report a 5 out of 5 satisfaction score (Table 2).
Table 2.
Patient and visit characteristics based on achievement of five out of five satisfaction score and telemedicine preference.
| All patients | 5/5 satisfaction | ≤4/5 satisfaction | P | Prefer in-person visit | Prefer telehealth | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | |||
| Overall | 772 | 100.0 | 535 | 69.3 | 237 | 30.7 | 426 | 55.2 | 346 | 44.8 | ||
| Visit type | ||||||||||||
| New | 183 | 23.7 | 127 | 23.7 | 56 | 23.6 | .974 | 107 | 25.1 | 76 | 22.0 | .306 |
| Follow-up | 267 | 34.6 | 191 | 35.7 | 76 | 32.1 | .328 | 122 | 28.6 | 145 | 41.9 | <.001 |
| Postoperative | 322 | 41.7 | 217 | 40.6 | 105 | 44.3 | .331 | 197 | 46.2 | 125 | 36.1 | .005 |
| Audio only | 253 | 32.8 | 146 | 27.3 | 107 | 45.2 | <.001 | 155 | 36.4 | 98 | 28.3 | .018 |
| Miles | ||||||||||||
| 0-10 | 210 | 27.2 | 145 | 27.1 | 65 | 27.4 | .926 | 140 | 32.9 | 70 | 20.2 | <.001 |
| 10-25 | 229 | 29.7 | 161 | 30.1 | 68 | 28.7 | .694 | 123 | 28.9 | 106 | 30.6 | .594 |
| 25-50 | 128 | 16.6 | 89 | 16.6 | 39 | 16.5 | .951 | 58 | 13.6 | 70 | 20.2 | .014 |
| 50-100 | 75 | 9.7 | 48 | 9.0 | 27 | 11.4 | .295 | 38 | 8.9 | 37 | 10.7 | .408 |
| 100+ | 128 | 16.6 | 91 | 17.0 | 37 | 15.6 | .630 | 65 | 15.3 | 63 | 18.2 | .273 |
| Age, years | ||||||||||||
| <50 | 151 | 19.6 | 112 | 20.9 | 39 | 16.5 | .148 | 64 | 15.0 | 87 | 25.1 | <.001 |
| 50-59 | 173 | 22.4 | 126 | 23.6 | 47 | 19.8 | .253 | 83 | 19.5 | 90 | 26.0 | .031 |
| 60-69 | 235 | 30.4 | 150 | 28.0 | 85 | 35.9 | .029 | 141 | 33.1 | 94 | 27.2 | .075 |
| 70+ | 204 | 26.4 | 140 | 26.2 | 64 | 27.0 | .808 | 135 | 31.7 | 69 | 19.9 | <.001 |
| Male sex | 356 | 46.1 | 237 | 44.3 | 119 | 50.2 | .129 | 196 | 46.0 | 160 | 46.2 | .948 |
| Problems | ||||||||||||
| Audio | 75 | 9.7 | 41 | 7.7 | 34 | 14.4 | .004 | 37 | 8.7 | 38 | 11.0 | .284 |
| Video | 89 | 11.5 | 37 | 6.9 | 52 | 21.9 | <.001 | 53 | 12.4 | 36 | 10.4 | .378 |
| History | 38 | 4.9 | 8 | 1.5 | 30 | 12.7 | <.001 | 31 | 7.3 | 7 | 2.0 | .001 |
| Exam | 104 | 13.5 | 28 | 5.2 | 76 | 32.1 | <.001 | 89 | 20.9 | 15 | 4.3 | <.001 |
| Imaging | 33 | 4.3 | 7 | 1.3 | 26 | 11.0 | <.001 | 27 | 6.3 | 6 | 1.7 | .002 |
| Treatment plan | 30 | 3.9 | 10 | 1.9 | 20 | 8.4 | <.001 | 22 | 5.2 | 8 | 2.3 | .041 |
| Asking questions | 32 | 4.2 | 12 | 2.2 | 20 | 8.4 | <.001 | 22 | 5.2 | 10 | 2.9 | .115 |
| Number of problems | ||||||||||||
| 0 | 523 | 67.8 | 432 | 80.8 | 91 | 38.4 | <.001 | 259 | 60.8 | 264 | 76.3 | <.001 |
| 1 | 162 | 21.0 | 81 | 15.1 | 81 | 34.2 | <.001 | 100 | 23.5 | 62 | 17.9 | .059 |
| 2 | 49 | 6.4 | 15 | 2.8 | 34 | 14.4 | <.001 | 37 | 8.7 | 12 | 3.5 | .003 |
| 3+ | 38 | 4.9 | 7 | 1.3 | 31 | 13.1 | <.001 | 30 | 7.0 | 8 | 2.3 | .003 |
| Site B (vs site A) | 271 | 35.1 | 151 | 28.2 | 120 | 50.6 | <.001 | 168 | 39.4 | 103 | 29.8 | .005 |
Multivariate analysis demonstrated that patients from site B had significantly increased odds to have a satisfaction score less than 5 out of 5 (odds ratio [OR] = 2.68 [95% CI 1.86-3.88]). In the multivariate analysis by problem type, problems with exam and imaging had the greatest impact on lowering satisfaction score below 5 out of 5 (OR 7.03 [95% CI 4.17-11.85] and OR 5.48 [95% CI 2.02-14.86], respectively) (Table 3). A subanalysis was then performed to determine if the number of problems encountered during the telemedicine visit, and not just the type of problem, was associated with poorer satisfaction. The multivariate model that included number of cumulative problems (“number-of-problems” model) instead of problem type (“type-of-problem” model reported in Table 3) showed that the number of problems increased the odds that a patient’s satisfaction score would be less than 5 out of 5 (1 problem OR = 5.26 [95% CI 3.53-7.84], 2 problems OR = 11.89 [95% CI 6.08-23.26], 3 or more problems OR = 21.9 [95% CI 9.16-52.35]) (Table 4). Similar to the “type-of-problem” model, the “number-of-problems” model demonstrated that patients from site B had significantly increased odds to have a satisfaction score less than 5 out of 5 (OR = 3.02 [95% CI 2.1-4.34]).
Table 3.
Significant variables from multivariate analysis for failure to achieve five out of five satisfaction (satisfaction four out of five or less) based on encounter problem type.
| Variable (problem type) | Odds ratio | P | 95% CI |
|---|---|---|---|
| Exam | 7.03 | <.001 | 4.17-11.85 |
| Imaging | 5.48 | .001 | 2.02-14.86 |
| Audio | 2.07 | .015 | 1.15-3.72 |
| Video | 3.32 | <.001 | 2-5.51 |
| History | 2.73 | .044 | 1.03-7.27 |
| Site B (vs site A) | 2.68 | <.001 | 1.86-3.88 |
Table 4.
Significant variables from multivariate analysis for failure to achieve five out of five satisfaction (satisfaction four out of five or less) based on number of problems.
| Variable (no. of problems) | Odds ratio | P | 95% CI |
|---|---|---|---|
| 0 | Reference | — | — |
| 1 | 5.26 | <.001 | 3.53-7.84 |
| 2 | 11.89 | <.001 | 6.08-23.26 |
| 3+ | 21.90 | <.001 | 9.16-52.35 |
| Site B (vs site A) | 3.02 | <.001 | 2.1-4.34 |
Patient and Visit Characteristics Associated With a Preference for Telemedicine
Following a similar trend as seen in the bivariate results for satisfaction scores, on bivariate analysis for telemedicine preference, patients who had 2 or more problems with the telemedicine visit were significantly more likely to prefer an in-person visit over telemedicine (P = .003) (Table 2). This pattern was also seen with respect to individual problems with the exception of problems with audio, video, and asking questions. Again, following a similar trend, patients who had audio only for their telemedicine visit were significantly more likely to prefer an in-person visit (P = .01). The key differences in this analysis are with regard to visit type, miles traveled, and patient age. Patients who live closer to the doctor’s office (ie, within 10 miles round-trip) preferred an in-person visit (P < .001), whereas those who were slightly further (ie, within a 25- to 50-mile round-trip) preferred telemedicine (P = .014). Patients younger than 59 years were significantly more likely to prefer telemedicine (P < .05), whereas patients older than 60 years were significantly more likely to prefer an in-person visit (P < .001) (Table 2).
On multivariate analysis, patients who noted a telehealth preference generally had greater distance to travel, were younger, and had a decreased number of problems with the physical exam when compared to patients with an in-person visit preference (Table 5). In a subanalysis based on number of problems instead of type of problems (Table 6), an increased number of problems was associated with decreased odds of telehealth preference (1 problem OR = 0.62 [95% CI 0.43-0.9], 2 problems OR = 0.36 [95% CI 0.18-0.71], 3 problems OR = 0.30 [95% CI 0.13-0.68]). The “number-of-problems” multivariate model for telehealth preference similarly found that greater travel distance, younger patients, and site A (OR = 0.72, CI 0.52-0.99) were associated with telehealth preference.
Table 5.
Significant variables from multivariate analysis for telemedicine preference based on encounter problem type.
| Variable | Odds ratio | P | 95% CI |
|---|---|---|---|
| Miles | |||
| 0-10 | Reference | — | — |
| 10-25 | 1.67 | .015 | 1.11-2.52 |
| 25-50 | 2.47 | <.001 | 1.53-4.01 |
| 50-100 | 1.99 | .019 | 1.12-3.55 |
| 100+ | 1.83 | .014 | 1.13-2.95 |
| Age 60-69 y (vs age <50 y) | 0.50 | .002 | 0.32-0.77 |
| Age 70+ y (vs age <50 y) | 0.37 | <.001 | 0.23-0.58 |
| Problem with exam | 0.18 | <.001 | 0.1-0.32 |
Table 6.
Significant variables from multivariate analysis for telemedicine preference based on number of problems.
| Variable | Odds ratio | P | 95% CI |
|---|---|---|---|
| Miles | |||
| 0-10 | Reference | — | — |
| 10-25 | 1.59 | .025 | 1.06-2.39 |
| 25-50 | 2.42 | <.001 | 1.51-3.9 |
| 50-100 | 1.89 | .027 | 1.08-3.31 |
| 100+ | 1.71 | .026 | 1.07-2.73 |
| Age 60-69 y (vs age <50 y) | 0.52 | .003 | 0.34-0.8 |
| Age 70+ y (vs age <50 y) | 0.39 | <.001 | 0.25-0.62 |
| No. of problems | |||
| 0 | Reference | — | — |
| 1 | 0.62 | .012 | 0.43-0.9 |
| 2 | 0.36 | .004 | 0.18-0.71 |
| 3+ | 0.30 | .004 | 0.13-0.68 |
| Site B (vs site A) | 0.72 | .043 | 0.52-0.99 |
Discussion
This cross-sectional study examining spine telemedicine visits during the COVID-19 pandemic found that patients overall were highly satisfied, with 70% of patients rating their visit as 5 out of 5 and 87.7% of patients rating their visit as 4 out of 5 or greater. Furthermore, 45% of the responses indicated a preference for telemedicine visit over an in-person visit if given the choice. Prior studies evaluating patient satisfaction with telemedicine nonspine, orthopedic visits have found similarly high patient satisfaction.12,14-16,18,19,21,24 However, direct comparison of their findings to our study is difficult due to their small sample sizes and study designs. European studies examining satisfaction and future visit preference after orthopedic telemedicine consultation included patients accompanied by a nurse or junior surgeon in a controlled setting.12,14
Kane et al 18 completed a prospective, randomized clinical trial to evaluate telemedicine for postoperative follow-up after arthroscopic rotator cuff repair. Of the 28 patients who received telemedicine follow-up, 94.1% were either satisfied or very satisfied with their visit. While these results are comparable to those presented herein, it is important to note the small sample size, specific visit-type (postoperative only) and eligibility requirements of the Kane et al 18 study. Patients without high-speed internet or communication capabilities were excluded. Furthermore, active range of motion is restricted after rotator cuff repair, making the physical examination component less significant. Marsh et al 19 evaluated telemedicine for late follow-up after total joint arthroplasty. A total of 118 patients received web-based follow-up with 75.6% being extremely or very satisfied with their visit. Of the patients seen via telemedicine, 44% said they preferred this method over in-office visits, which was similar to our results (45%); however, this was only for follow-up visits. Sathiyakumar et al 16 completed a randomized clinical trial utilizing telemedicine for fracture care follow-up. In the telemedicine cohort, 89% of patients were satisfied with their care and 75% agreed to future telemedicine visits, but this was based on only 8 patients.
Multivariate analysis identified numerous factors associated with reduced satisfaction and preference for in-person follow-up appointments. While some factors are not modifiable (age, distance traveled), others, such as audio and video reliability, can be optimized to increase patient satisfaction with telemedicine in the future. As might be expected, the odds of not achieving five out of five satisfaction increased with each successive problem. Similarly, patients were increasingly less likely to prefer future telemedicine visits with each problem. According to our analysis, problems with the visit (physical examination, understanding of imaging, ability to communicate history and symptoms, audio, and video) contributed to worse satisfaction. Problems with the physical exam were also associated with reduced telemedicine preference. These issues are likely related to the rapid initiation of the telemedicine programs, the absence of standardized visit protocols, and difficulty with the spine telemedicine examination.12,14,26,27 As discussed, previous telemedicine studies often included technology-related inclusion criteria or office-based assistance. While our patients were encouraged to optimize their connectivity prior to their exams, physician- and patient-based internet issues certainly impacted some of the visits. As we continue to utilize telemedicine, connectivity will hopefully improve and experience with the examination and web-based video platforms increase.
Increased age and travel distance significantly impacted preference for future telemedicine visits in our study. Patients who would normally travel greater than 10 miles round trip were more likely to prefer a future telemedicine visit. Prior studies have found similar results, with patients noting the time and economic benefits associated with telemedicine and reduced travel distance in general.14,15,18,19,24,28-30 While not a modifiable factor, this information can be utilized by spine practitioners when offering telemedicine visits to patients. Despite being as satisfied with their telemedicine visits, patients older than 60 years were less likely to prefer future telemedicine visits. Older patients tend to have a harder time embracing change and accepting technology, including telemedicine.31,32 Aside from their technology preferences, older patients may be less likely to worry about missing work than younger patients, which may also contribute to their reduced preference.
Multivariate analysis for satisfaction and preference found site to be a significant variable. More specifically, patients from site B were less likely to achieve 5 out of 5 satisfaction and less likely to prefer a future visit. The majority (76.4%) of site B visits occurred with audio-alone compared with only 9.2% of site A visits. However, audio-alone was not found to be significant after multivariate analysis. In an effort to limit survey-time and burden, a number of variables that may contribute to telemedicine satisfaction and preference were not captured. Examples include but are not limited to health status, insurance status, ethnicity, transportation means, geographical region (rural vs suburban vs urban), internet connection, device access, employment status, video platform, and clinical problem (cervical, lumbar, etc). While the percentage of respondents was similar between sites, the response rate was only 21.9%, which may also contribute to these findings. Furthermore, there is significant regional variation of COVID-19 within the United States. 33 Perhaps patients in certain geographical regions and communities within the United States may be better suited for telemedicine.
Our study has a number of strengths and limitations. The large number of responses, multiple sites and inclusion of all visit types makes our study unique. To our knowledge, this is the first telemedicine study to focus solely on spine patients presenting to spine surgeons. As a result, these findings are generalizable to other spine surgeons and their practices. In addition to the aforementioned limitations (potential confounding variables and response rate), this study is limited by its retrospective nature and lack of a control group. However, a concurrent control group was not possible due to social distancing restrictions. When feasible, higher level studies are needed to compare telemedicine to in-person visits for spine patients. Future studies should also explore the physician learning curve with telemedicine and assess the quality of the spine telemedicine examination.
The COVID-19 pandemic led to the rapid expansion of telemedicine across medicine. While telemedicine allows for social distancing and has the potential to reduce costs and increase access to care, it is important to establish patient satisfaction with this platform. Our cross-sectional, survey-based study consisting of responses from 772 spine telemedicine visits at two practices in different geographic regions during the COVID-19 pandemic found a high rate of patient satisfaction with telemedicine. Furthermore, 45% of the responses indicated a preference for a telemedicine visit over a traditional in-person visit in the future. Patient- and visit-based factors associated with increased satisfaction and visit preference were identified. In light of these findings, telemedicine for spine care may be a preferable option for a subset of patients into the future.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alexander M. Satin, MD  https://orcid.org/0000-0001-9181-7494
https://orcid.org/0000-0001-9181-7494
Evan D. Sheha, MD  https://orcid.org/0000-0003-4339-6079
https://orcid.org/0000-0003-4339-6079
Bryce Basques, MD, MHS  https://orcid.org/0000-0002-7745-8701
https://orcid.org/0000-0002-7745-8701
References
- 1.World Health Organization. Coronavirus disease 2019 (COVID-19) situation report–51. Published March 11, 2020. Accessed April 14, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
- 2.WhiteHouse.gov. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. Published March 13, 2020. Accessed April 19, 2020. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/
- 3.Jain NS, Alluri RK, Schopler SS, Hah R, Wang JC. COVID-19 and spine surgery: a review and evolving recommendations. Global Spine J. 2020;10:528–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarpong NO, Forrester LA, Levine WN. What’s important: redeployment of the orthopaedic surgeon during the COVID-19 pandemic: perspectives from the trenches. J Bone Joint Surg Am. 2020;107:1019–1021. doi:10.2106/jbjs.20.00574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vannabouathong C, Devji T, Ekhtiari S, et al. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am. 2020;102:734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang ZC, Wang W, Murphy D, et al. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg Am. 2020;102:745–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halawi M, Wang D, Hunt T, 3rd. What’s important: weathering the COVID-19 crisis: time for leadership, vigilance, and unity. J Bone Joint Surg Am. 2020;102:759–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haleem A, Javaid M, Vaishya R, Vaish A. Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma. 2020;11:498–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:e487–e492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.HHS.gov, US Department of Health & Human Services. Notification of enforcement discretion for telehealth remote communications during the COVID-19 Nationwide Public Health Emergency. Accessed September 28, 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
- 11.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019;21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019;25:451–459. [DOI] [PubMed] [Google Scholar]
- 13.Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aarnio P, Lamminen H, Lepisto J, Alho A. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare. 1999;5:62–66. [DOI] [PubMed] [Google Scholar]
- 15.Haukipuro K, Ohinmaa A, Winblad I, Linden T, Vuolio S. The feasibility of telemedicine for orthopaedic outpatient clinics—a randomized controlled trial. J Telemed Telecare. 2000;6:193–198. [DOI] [PubMed] [Google Scholar]
- 16.Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29:e139–e145. [DOI] [PubMed] [Google Scholar]
- 17.Vuolio S, Winblad I, Ohinmaa A, Haukipuro K. Videoconferencing for orthopaedic outpatients: one-year follow-up. J Telemed Telecare. 2003;9:8–11. [DOI] [PubMed] [Google Scholar]
- 18.Kane LT, Thakar O, Jamgochian G, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29:775–783. [DOI] [PubMed] [Google Scholar]
- 19.Marsh J, Bryant D, MacDonald SJ, et al. Are patients satisfied with a web-based followup after total joint arthroplasty? Clin Orthop Relat Res. 2014;472:1972–1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marsh JD, Bryant DM, MacDonald SJ, et al. Feasibility, effectiveness and costs associated with a web-based follow-up assessment following total joint arthroplasty. J Arthroplasty. 2014;29:1723–1728. [DOI] [PubMed] [Google Scholar]
- 21.Sharareh B, Schwarzkopf R. Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty. 2014;29:918–922.1. [DOI] [PubMed] [Google Scholar]
- 22.Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Perez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017;19:e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg. 2011;93:113–120. [DOI] [PubMed] [Google Scholar]
- 24.Sultan AA, Acuña AJ, Samuel LT, et al. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. 2020;40:e712–e715. doi:10.1097/bpo.0000000000001553 [DOI] [PubMed] [Google Scholar]
- 25.Nielsen DM, Gill K, Ricketts DM. Satisfaction levels in orthopaedic out-patients. Ann R Coll Surg Engl. 2005;87:106–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102:e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makhni MC, Riew GJ, Sumathipala MG. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020;102:1109–1115. [DOI] [PubMed] [Google Scholar]
- 28.Fortney JC, Booth BM, Blow FC, Bunn JY. The effects of travel barriers and age on the utilization of alcoholism treatment aftercare. Am J Drug Alcohol Abuse. 1995;21:391–406. [DOI] [PubMed] [Google Scholar]
- 29.DeNino WF, Osler T, Evans EG, Forgione PM. Travel distance as factor in follow-up visit compliance in postlaparoscopic adjustable gastric banding population. Surg Obes Relat Dis. 2010;6:597–600. [DOI] [PubMed] [Google Scholar]
- 30.Lara MD, Baker MT, Larson CJ, Mathiason MA, Lambert PJ, Kothari SN. Travel distance, age, and sex as factors in follow-up visit compliance in the post-gastric bypass population. Surg Obes Relat Di s. 2005;1:17–21. [DOI] [PubMed] [Google Scholar]
- 31.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7:e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lowitt MH, Kessler II, Kauffman CL, Hooper FJ, Siegel E, Burnett JW. Teledermatology and in-person examinations: a comparison of patient and physician perceptions and diagnostic agreement. Arch Dermatol. 1998;134:471–476. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. United States COVID-19 cases and deaths by state. Published January 21, 2020. Accessed September 28, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html