Abstract
Study Design:
Prospective radiological analysis.
Objective:
To investigate the characteristics of the sagittal spinopelvic alignment in the standing and sitting positions under the Roussouly classification in a healthy population.
Methods:
This study using standing and sitting lateral radiographs included 143 volunteers whose spinopelvic parameters were measured. The parameters were compared in the standing and sitting positions. The lumbo-pelvic profile was identified according to the Roussouly classification. The differences in the values of the parameters between the standing and sitting positions were analyzed. The different frequencies of the unchanged apex were assessed.
Results:
All parameter values except the thoracolumbar angle (TLK) were significantly altered. With regard to the classification of the lumbopelvic profile, 15 (10.5%) subjects were excluded because they were evaluated as not belonging to any of the Roussouly types. The remaining 128 subjects were evaluated and classified as follows: 19 (14.8%), type 1; 53 (41.4%), type 2; 9 (7.0%), type 3 + anteverted pelvis (AP); 33 (25.8%), type 3; and 14 (10.9%), type 4. The differences in the pelvic tilt (PT), sacral slope (SS), and thoracic pelvic angle (TPA) values were significantly lower in types 1 and 2 than in other Roussouly types. Corresponding variations in the apical vertebra for the sagittal lumbar curves in the sitting position were observed.
Conclusions:
Subjects with Roussouly type 1 and type 2 sagittal alignments were found to be less capable of performing changes in alignment when changing to the sitting position. The characteristics of the apical movement were also different.
Keywords: sitting, sagittal alignment, Roussouly classification, pelvic alignment, standing
Introduction
With the changes induced by modern lifestyles and the widespread use of technology, people are spending increasingly more time in the sitting position, and various health problems associated with sitting have been reported. 1 It is important to understand the effects of the sitting position on the changes in lumbar alignment and pelvic compensation. Previous studies have investigated the basic changes occurring in the lumbar region and pelvis when moving from the standing to the sitting position, which may be summarized as a straightened curve in the lumbar region (decreased lumbar lordosis, LL), and pelvic retroversion (increased pelvic tilt, PT).2-6
An influential and widely employed classification system of the lumbo-pelvic profile in the sagittal plane has been proposed by Roussouly et al. 7 Taking into consideration the apex of the lumbar curve and the sacral slope (SS) in the standing position, the method allows defining 4 different lumbo-pelvic types, which have recently been extended to 5 by accounting for the presence of pelvic anteversion. 8 Under the Roussouly classification, Yu et al 9 explored the relationship between the cervical spine and global spine alignment showing that it is feasible to use the Roussouly classification in the Chinese population.
While sitting is a common weightbearing position in daily life,10,11 there is not much evidence about how the Roussouly types influence changes in the sagittal parameter values when changing to the sitting position. Exploring the characteristics of such changes in the sitting position under the Roussouly classification may be useful in providing a more specific reference for the surgical plan.
Therefore, imaging studies of healthy young Chinese individuals were conducted in the standing and sitting positions with an aim to provide a comprehensive description of differences in the sagittal parameter values among Roussouly types between standing and sitting positions.
Methods
This was a cross-sectional prospective study that was approved by the Ethics Committee of Peking University Third Hospital and was performed within the principles of the Declaration of Helsinki. Asymptomatic adults were recruited to participate in this study with the approval of the ethics committee (IRB00006761-2 018 192). All volunteers met the following inclusion criteria: an age between 18 and 30 years, not pregnant, no history of a spinal disorder or surgery, and no radiographic abnormalities (such as sagittal or coronal deformities, sacralization, or other sacropelvic anomalies) detected prior to or during the study. Hip, knee, and ankle abnormalities were ruled out by physical examination. All volunteers provided informed consent. A total of 143 volunteers were enrolled.
For each volunteer, lateral full spine radiographs in the standing and sitting positions were obtained keeping the distance between the subject and the radiographic source constant. For standing radiographs, the participants were instructed to stand as straight as possible with their fingers touching the homolateral collar bones. 12 In the sitting position, volunteers were asked to flex their hips and knees to 90° and sit as straight as possible with their fingers touching the homolateral collar bones. 13 A height-adjustable stool without a back-rest was provided for the volunteers so that they could adjust the height to reach a standardized posture and rest their feet flat on the ground. If the volunteers’ feet could not touch the ground after adjusting the stool height, a wooden step was provided.
The radiographs were digitized, and all measurements were performed by means of imaging software (Centricity Radiology Information Systems/Picture Archiving and Communication Systems [RIS/PACS], GE Healthcare) based on standard measurement techniques by two senior spine surgeons, and the average of their results was recorded.
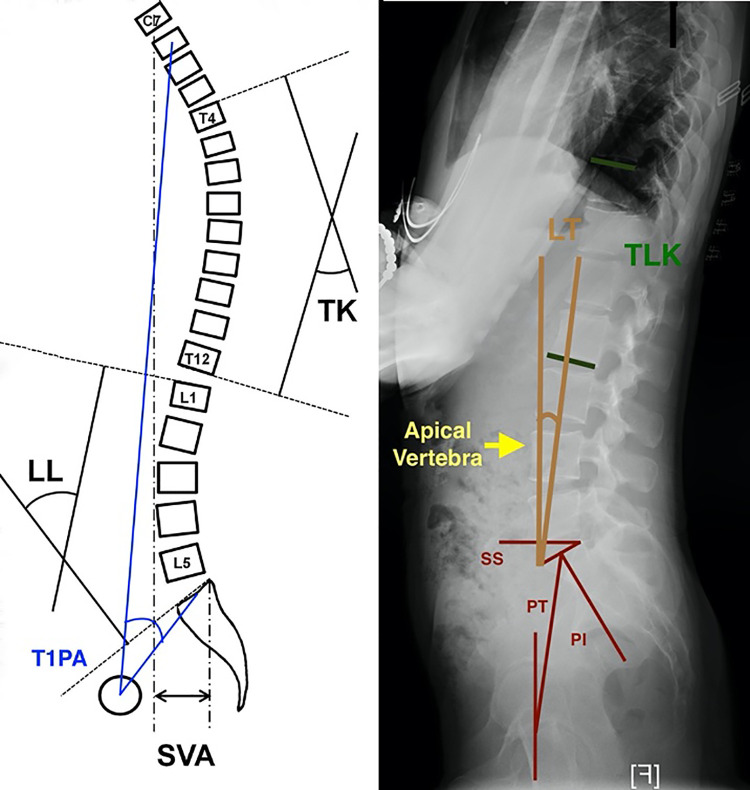
The following parameters were measured (Figure 1). (1) Pelvic parameters: pelvic incidence (PI); pelvic tilt (PT); sacral slope (SS). (2) Local curvature: lumbar lordosis (LL); apical vertebra of LL; thoracic kyphosis (TK); thoracolumbar angle (TLK). (3) Global parameters: sagittal vertical axis (SVA); thoracic pelvic angle (TPA), the angle between the line from the femoral head axis to the centroid of the first thoracic (T1) vertebra and the line from the femoral head axis to the middle of the first sacral (S1) endplate; lordosis tilt (LT), the angle formed by the vertical line and the line through the anterior superior edge of S1 and the first lumbar (L1) vertebra. LT is expressed as a negative value if L1 is posterior to the anterior aspect of S1 and positive if it is anterior to S1.
Figure 1.
Schematic diagram of measured parameters.
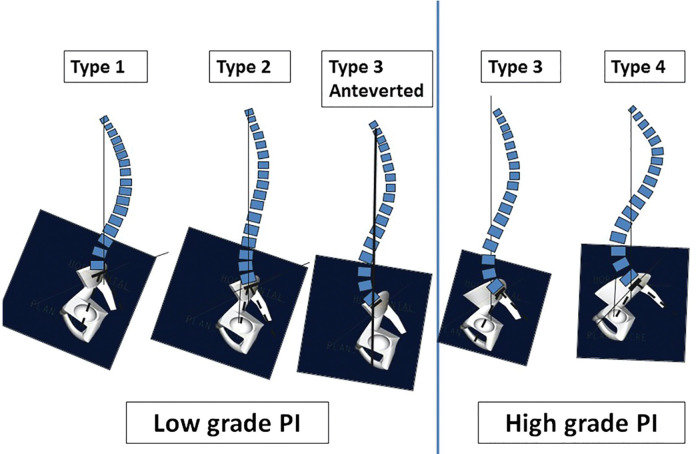
The lumbopelvic profile was identified according to the classification proposed by Roussouly et al. 7 by the apex of the lumbar curve and the measured SS in the standing position. The recently proposed fifth category, which distinguishes subjects characterized by the presence of an anteverted pelvis (type 3 + AP), was also identified 8 (Figure 2).
Figure 2.
Classification of the normal sagittal alignment according to Roussouly into 5 types (taken from Laouissat et al 8 ). Type 1: The SS is less than 35°, associated with a low PI. The apex of LL is located at L5 vertebral body. Type 2: The SS is less than 35°. The apex of LL is located at base of L4 vertebral body. Type 3 + AP: The SS is between 35° and 45°, associated with a low PI. The PT was low or negative. The apex of LL is located at center of L4. Type 3: The SS is between 35° and 45°. The apex of LL is in the center of the L4 vertebral body. Type 4: The SS is greater than 45°, associated with high PI. The apex of LL is located at the base of the L3 vertebral body or higher. SS, sacral slope; PI, pelvic incidence; LL, lumbar lordosis; AP, anteverted pelvis; PT, pelvic tilt.
Statistical Method
All data was analyzed using the SPSS software (version 17.0; IBM Corp). The interobserver reliability was assessed using the intraclass correlation coefficient (ICC). ICC ≥ 0.80 was considered to indicate excellent reliability. Continuous variables were shown as means with standard deviation. An adaptation of the Kolmogorov-Smirnov test was implemented to test for normally distributed data. The paired t test or Wilcoxon rank-sum test in case of non-Gaussian distribution was used to compare continuous parameters in the standing and sitting positions. The changes in the values of the parameters between the standing and sitting positions were analyzed using 1-way analysis of variance (or Kruskal-Wallis test) with post hoc comparisons performed among the various Roussouly types. The different frequencies of the unchanged apex in different positions were assessed by the chi-square test (or Fisher’s exact test). The statistical difference level was .05.
Results
Data of 143 volunteers (94 females and 49 males) was analyzed in this study. The average age of the volunteers was 23.0 ± 2.3 years (range 19.0-29.0 years). The mean body mass index (BMI) was 20.8 ± 2.7 kg/m2.
All parameters were measured with good reproducibility. The interobserver mean ICC was 0.92 (range = 0.82-0.99). The average PI, a morphologic parameter, was 46.5° ± 9.1° (range 25.6° to 69.7°). The mean value, standard deviation, and range of each positional parameter are listed in Table 1. When changing from the standing to sitting position, all spinopelvic sagittal parameter values except TLK were found significantly altered. An increase in the PT was observed (mean 16.4° ± 8.8°, P < .001). The entire spine straightened out when subjects went from standing to sitting positions, with a decrease in both the LL and TK by 24.7° ± 12.2° (P < .001) and 6.0° ± 8.0° (P < .001), respectively. Forward displacement of the SVA occurred with a significant difference in values (mean 46.3 ± 30.8 mm) (P < .001). As a result of a combination of pelvic and trunk changes, an increase in the TPA was observed (mean 17.7° ± 8.1°, P < .001).
Table 1.
The Overall Sagittal Balance Parameters Measured in Standing and Sitting Positions.
| Parameter | Mean ± SD | Range | Parameter | Mean ± SD | Range | t | P |
|---|---|---|---|---|---|---|---|
| PTa (deg) | 11.7 ± 6.5 | −8.3 to 27.6 | PTb (deg) | 28.1 ± 9.7 | 1.3 to 53.0 | −22.345 | <.001 |
| SSa (deg) | 34.8 ± 7.1 | 13.5 to 52.3 | SSb (deg) | 19.9 ± 8.5 | 0.9 to 42.0 | 20.847 | <.001 |
| LLa (deg) | 50.3 ± 10.0 | 23.5 to 72.9 | LLb (deg) | 25.6 ± 11.6 | 1.0 to 54.7 | 24.224 | <.001 |
| LTa (deg) | −5.0 ± 4.9 | −17.0 to 7.7 | LTb (deg) | −1.8 ± 5.7 | −15.2 to 11.9 | −8.205 | <.001 |
| TLKa (deg) | 6.2 ± 5.4 | 0.1 to 27.3 | TLKb (deg) | 6.5 ± 4.8 | 0.1 to 20.1 | −0.687 | .493 |
| TKa (deg) | 26.0 ± 10.3 | 2.4 to 72.0 | TKb (deg) | 20.0 ± 8.9 | 0.7 to 49.6 | 9.019 | <.001 |
| SVAa (mm) | −20.0 ± 22.5 | −69.7 to 74.2 | SVAb (mm) | 26.3 ± 28.3 | −48.9 to 102.7 | −17.946 | <.001 |
| T1PAa (deg) | 5.6 ± 6.0 | −16.3 to 18.7 | T1PAb (deg) | 23.3 ± 8.8 | 3.0 to 43.1 | −26.114 | <.001 |
Abbreviations: PT, pelvic tilt; SS, sacral slope; LL, lumbar lordosis; LT, lordosis tilt; TLK, thoracolumbar angle; TK, thoracic kyphosis; SVA, sagittal vertical axis; T1PA thoracic pelvic angle.
a Standing.
b Sitting.
The interobserver correlation in classifying the Roussouly classification was 0.95. With regard to the classification of the lumbo-pelvic profile, 15 (10.5%) of the 143 subjects were excluded because they were considered not classifiable, that is, not belonging to any of the 5 types due to the apex being located at the third lumbar (L3) vertebra or above and a relatively small SS in the standing position. The remaining 128 subjects were evaluated and classified as follows: 19 (14.8%), type 1; 53 (41.4%), type 2; 9 (7.0%), type 3 + AP; 33 (25.8%), type 3; and 14 (10.9%), type 4 (Table 2). Females and males were similarly distributed (P = .386, Fisher’s exact test).
Table 2.
The Overall Sagittal Parameters Under Roussouly Classification.
| Parameters | Type 1 | Type 2 | Type 3 + AP | Type 3 | Type 4 | P (ANOVA) |
|---|---|---|---|---|---|---|
| PIa (deg) | 37.3 ± 8.0 | 42.6 ± 5.1 | 41.6 ± 3.0 | 53.4 ± 6.1 | 58.0 ± 8.5 | <.001 |
| SSa (deg) | 25.7 ± 5.6 | 31.2 ± 3.7 | 40.8 ± 3.5 | 39.3 ± 2.6 | 46.4 ± 2.5 | <.001 |
| PTa (deg) | 11.6 ± 6.2 | 11.6 ± 5.7 | 0.8 ± 3.6 | 14.0 ± 5.5 | 11.8 ± 7.4 | <.001 |
| LLa (deg) | 40.4 ± 11.1 | 46.7 ± 7.5 | 59.0 ± 8.3 | 55.7 ± 6.0 | 62.6 ± 4.1 | <.001 |
| LTa (deg) | −10.5 ± 3.9 | −6.9 ± 3.4 | −5.9 ± 2.3 | −4.0 ± 3.5 | 1.2 ± 3.6 | <.001 |
| TLKa (deg) | 9.6 ± 7.9 | 6.0 ± 5.1 | 5.7 ± 4.7 | 4.5 ± 4.0 | 5.7 ± 4.0 | .109 |
| TKa (deg) | 26.3 ± 12.4 | 27.5 ± 10.4 | 29.2 ± 9.8 | 26.3 ± 9.4 | 22.5 ± 10.2 | .530 |
| SVAa (mm) | −31.1 ± 19.6 | −21.4 ± 20.4 | −13.6 ± 37.2 | −20.7 ± 23.0 | −15.9 ± 18.1 | .236 |
| T1PAa (deg) | 4.3 ± 5.2 | 5.4 ± 5.0 | −4.0 ± 5.2 | 7.7 ± 5.9 | 6.1 ± 6.3 | <.001 |
Abbreviations: AP, anteverted pelvis; ANOVA, analysis of variance; PT, pelvic tilt; SS, sacral slope; LL, lumbar lordosis; LT, lordosis tilt; TLK, thoracolumbar angle; TK, thoracic kyphosis; SVA, sagittal vertical axis; T1PA thoracic pelvic angle.
a Standing.
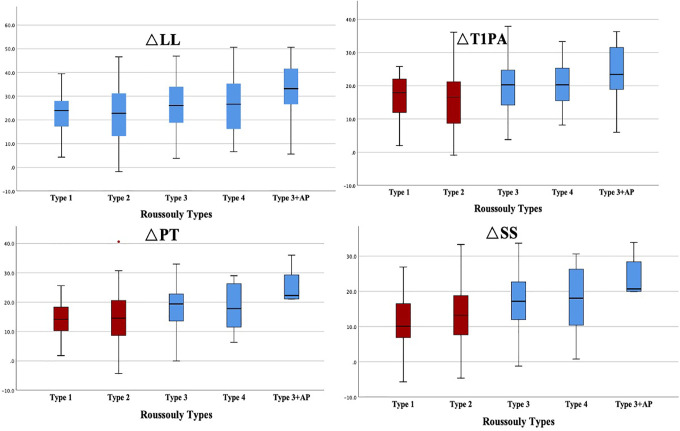
When moving from the standing to the sitting position, the differences in the parameter values (ΔSS, ΔPT, ΔT1PA) between the two positions showed significant changes (P<0.05) (Table 3 and Figure 3). As shown in Figure 3, the differences in the pelvic positional parameter values and in TPA values in type 1 and type 2 were significantly lower than in other Roussouly types. Although there was no statistical difference compared with the other 3 types, the ΔLL values of type 1 and type 2 revealed a decreasing trend (P = .096).
Table 3.
The Measurement Differences Between Positions in Each Roussouly Type.
| Parameters | Type 1 | Type 2 | Type 3 + AP | Type 3 | Type 4 | P (ANOVA) |
|---|---|---|---|---|---|---|
| ΔSS (deg) | 10.9 ± 7.6 | 13.0 ± 7.8 | 20.8 ± 11.3 | 17.4 ± 8.2 | 17.2 ± 8.9 | .004 |
| ΔPT (deg) | 14.0 ± 6.4 | 14.5 ± 8.8 | 22.1 ± 12.0 | 18.5 ± 8.3 | 18.5 ± 7.9 | .030 |
| ΔLL (deg) | 21.6 ± 10.8 | 22.4 ± 11.1 | 30.2 ± 16.8 | 28.0 ± 12.4 | 27.2 ± 12.4 | .096 |
| ΔLT (deg) | 4.8 ± 6.1 | 4.0 ± 4.4 | 0.2 ± 4.1 | 3.2 ± 4.7 | 2.5 ± 4.6 | .143 |
| ΔTLK (deg) | 1.9 ± 5.0 | 0.3 ± 4.1 | 1.4 ± 5.2 | 1.6 ± 4.1 | 1.1 ± 3.9 | .052 |
| ΔTK (deg) | 7.9 ± 8.3 | 6.5 ± 8.0 | 5.2 ± 8.0 | 7.1 ± 7.8 | 1.7 ± 5.9 | .240 |
| ΔSVA (mm) | 52.3 ± 44.7 | 45.3 ± 25.6 | 34.4 ± 48.3 | 51.2 ± 26.0 | 52.2 ± 29.4 | .557 |
| ΔT1PA (deg) | 16.3 ± 7.2 | 15.8 ± 8.0 | 22.9 ± 11.1 | 20.0 ± 7.6 | 20.2 ± 7.1 | .026 |
Abbreviations: Δ, difference value between positions; AP, anteverted pelvis; ANOVA, analysis of variance; PT, pelvic tilt; SS, sacral slope; LL, lumbar lordosis; LT, lordosis tilt; TLK, thoracolumbar angle; TK, thoracic kyphosis; SVA, sagittal vertical axis; T1PA thoracic pelvic angle.
Figure 3.
The differences (ΔLL, ΔSS, ΔPT, ΔT1PA) between positions were compared using 1-way analysis of variance. The same color background represented the same significance subset. LL, lumbar lordosis; SS, sacral slope; PT, pelvic tilt; T1PA, thoracic pelvic angle.
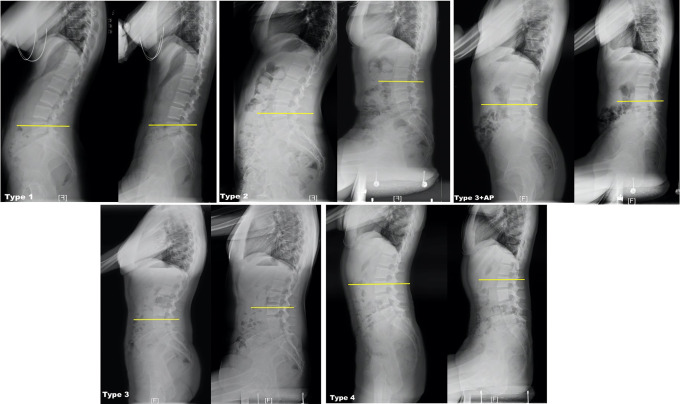
The apex of the lumbar curve in each Roussouly type is recorded in Table 4. Corresponding variations in the apical vertebra for the sagittal lumbar curves were observed (Figure 4). We focused on the unchanged apex position in each type. When moving to the sitting position, the percentages of unchanged apex positions in type 1 and type 3 + AP were 73.7% and 77.8%, respectively. The percentages of unchanged apex positions in type 3 and type 2 were only 33.3% and 54.7%, respectively. Using Fisher’s exact test, we found the unchanged apex position of the lumbar curve among the different Roussouly types to be significantly different (P = .025).
Table 4.
The Overall Lumbar Apical Vertebra in Each Roussouly Type.
| Type 1 | Type 2 | Type 3+AP | Type 3 | Type 4 | |
|---|---|---|---|---|---|
| Lumbar apical vertebra in standing | L5 (n = 19) | L4 (n = 53) | L4 (n = 9) | L4 (n = 33) | L3 (n = 14) |
| Lumbar apical vertebra in sitting | L5 (n = 14) L4 (n = 3) L3 (n = 2) |
L5 (n = 1) L4 (n = 29) L3 (n = 21) L2 (n = 2) |
L5 (n = 1) L4 (n = 7) L3 (n = 1) |
L5 (n = 2) L4 (n = 11) L3 (n = 19) L2 (n = 1) |
L3 (n = 9) L2 (n = 5) |
| Unchanged apex position (%) | 73.7 | 54.7 | 77.8 | 33.3 | 64.3 |
a P = .025 (Fisher’s exact test).
Figure 4.
Changes in lumbar apex vertebra levels (yellow lines) from standing (left) to sitting (right) in each Roussouly type.
Discussion
This study aimed to investigate the characteristics of the sagittal spinopelvic alignment in the standing and sitting positions under the Roussouly classification in a healthy population. Subjects with Roussouly type 1 and type 2 sagittal alignment were found to be less capable of executing changes in alignment when changing to the sitting position. Hitherto, only a few studies have observed the differences between the parameter values in the standing and sitting positions. Endo et al 2 performed an imaging analysis of the sagittal alignment in the standing and sitting positions among 50 healthy people with an average age of 31.5 years. The results showed that in the sitting position the curvature of the lumbar lordosis decreased by 50% and the PT increased by 25%. Other studies2-6,13 had similar results, which may be summarized as a straightened curve in the lumbar region, pelvic retroversion, and forward displacement of the sagittal balance. Our study showed comparable results. Compared with other studies, this study has some innovative aspects. First, there may be different lumbar curvature patterns with the same degree of LL using the Cobb method. We used the LT to describe the relative position of the L1 vertebral body. 7 When moving to the sitting position, the LT increased significantly (P < .001) indicating that the L1 vertebrae tilted forward relative to the sacrum which further indicated that the lumbar curve became more straightened. Second, the conventional method for evaluating the sagittal balance was by using the SVA. However, this method of using the SVA alone to assess the sagittal alignment failed to consider the pelvic compensation. TPA is a novel global spinopelvic parameter that takes into consideration both the trunk inclination and pelvic retroversion. 14 It has an advantage over other spinopelvic measures in that it can be measured in various body positions: standing, sitting, or prone on the operating table. 15 When changing to the sitting position, the increased TPA represents the combined effects of the straightened trunk and the degree of compensatory pelvic rotation. Thus, TPA is an appropriate parameter to describe the sagittal balance in the sitting position. Third, we investigated how the different Roussouly types influenced the changes in sagittal parameter values when moving from standing to sitting positions.
The Roussouly classification was the first classification to describe the various categories of sagittal alignment that help in understanding spinal pathologies. Due to the different patterns of lumbo-pelvic curves, having a knowledge of the overall changes in different positions is not enough. More specific changes in the parameters should be studied under the Roussouly classification. Our study demonstrated that subjects with different Roussouly types presented different changes in sagittal parameter values when moving from standing to sitting positions. Types 1 and 2 had similar trends, in that the ΔPT and ΔSS values were significantly lower than in other types. This phenomenon may be determined by the PI. Maekawa et al 16 found that PI was the most important factor affecting the change in the lumbo-pelvic sagittal alignment (ΔLL, ΔSS, ΔPT) between the sitting and standing positions. Since the PI determines the potential ability for pelvic retroversion, a person with a low PI would be less capable of performing changes in alignment between the sitting and standing positions. When moving from the standing to the sitting position, the loss of the LL causes the weight of the trunk to be shifted posteriorly leading to an increasing SVA.4,5 Our study found that under normal circumstances, subjects under different types of the Roussouly classification were able to achieve the same extent of ΔSVA in the sitting position. But for patients with Roussouly types 1 and 2, if the LL was overcorrected, the pelvic compensatory ability would fail to compensate for the changes in the truncal alignment when changing to the sitting position. We hypothesized that sagittal imbalance will occur more easily as a result showing that the individual will be unable to control the trunk when sitting down, and the trunk will tilt backward easily and uncontrollably. To achieve sagittal balance, the demand on the paraspinal muscles to maintain spinal stability will naturally increase, and it becomes reasonable to assume that these individuals will have more back pain or fatigue when sitting.
The ΔPT and ΔSS in type 3 were similar to those in type 4 despite the larger PI in type 4, and this phenomenon was also observed between type 1 and type 2, which indicated that the apex of the LL, too, could influence the changes in the parameters when moving to the sitting position. The overall changes in the LL apex in the sitting position have been studied. Hey et al 4 found that the apex vertebra moved superiorly for the lumbar curve by approximately one vertebral level in erect sitting, and the apex vertebra moved inferiorly for the thoracic curve by approximately one vertebral level. They also found that the LL decreased by nearly 80% in the natural sitting position; the curvature of the thoracolumbar vertebrae was close to a “C” shape. 5 The ascending apex of lumbar and descending apex of thoracic curve merge to one apex of “C” curve in natural sitting position. The decreased LL and straightened curve may result in the apex vertebra moved superiorly for lumbar. In our study, we analyzed the change in the apex level in each type further. The apex vertebra moving superiorly was more often seen in types 2 and 3. Conversely, the apex vertebra remaining stable was more often seen in types 1 and 3 + AP. It has recently been reported that restoring the apex of lordosis to the levels corresponding to the Roussouly classification would reduce the risk of proximal junction kyphosis (PJK) by a ratio of 4.6. 17 This suggests that surgeons should carefully consider the choice of the osteotomy level in restoring the apex of lordosis. Since the apex of LL in Roussouly type 1 subjects was less changed in the sitting position than in the other types, the apex position would not be suitable for the natural change in the sitting position if the restoration is carried out superiorly.
Recently, greater attention has been paid to the practical applications of the sagittal alignment in the sitting position. Janjua et al 18 used sitting radiographs to demonstrate the spinal flexibility among patients with a thoracolumbar deformity and found that relaxation of the unfused thoracic spine in the sitting position could predict the postoperative increase in kyphosis of the unfused thoracic segments. It has also been reported that restoring the sagittal spinal contour to the normal shapes as stated in the Roussouly classification would reduce the risk of mechanical complications in adult spinal deformities. 19 To the best of our knowledge, this is the first study to describe the sagittal spinopelvic alignment in both standing and sitting positions under the Roussouly classification and could serve as a reference for sagittal alignment reconstruction studies in the future. The effects of the sitting position on the complications in the junction area should also be studied further.
A limitation of this study was that the sitting position considered here was only the standard erect sitting position. Because people usually choose more comfortable sitting positions in daily life, the sagittal spinopelvic alignment might change significantly depending on the specific sitting position. 20 Second, it is worth noting that 15 (10.5%) out of the 143 subjects were excluded from the classification because they were evaluated as not matching any lumbo-pelvic type due to the apex being located at L3 or above and a relatively small SS. In future studies, we should pay greater attention to whether these characteristics of lumbo-pelvic types are specific to the Chinese population. Third, the effect of sitting height on sagittal balance was not taken into account. This will be studied in future.
Conclusions
We presented an overview of the normal ranges of the spinopelvic parameters in the standing and sitting positions. Along with a comprehensive description of the differences in the sagittal parameter values among the various Roussouly types between standing and sitting positions, we found that subjects with Roussouly types 1 and 2 were less capable of performing changes in alignment when changing to the sitting position compared with other Roussouly types. The characteristics of apex movement among Roussouly types were also different with the apex vertebra being stable more often in types 1 and 3 + AP. The characteristic changes under the Roussouly classification occurring in different positions could serve as a reference for sagittal alignment reconstruction.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by AOSPINE China Research Grant (2017-06).
ORCID iD: Weishi Li, MD  https://orcid.org/0000-0001-9512-5436
https://orcid.org/0000-0001-9512-5436
References
- 1.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting–a health hazard. Diabetes Res Clin Pract. 2012;97:368–376. [DOI] [PubMed] [Google Scholar]
- 2.Endo K, Suzuki H, Nishimura H, Tanaka H, Shishido T, Yamamoto K. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J Orthop Sci. 2012;17:682–686. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki H, Endo K, Mizuochi J, et al. Sagittal lumbo-pelvic alignment in the sitting position of elderly persons. J Orthop Sci. 2016;21:713–717. [DOI] [PubMed] [Google Scholar]
- 4.Hey HWD, Wong CYG, Lau ETC, et al. Differences in erect sitting and natural sitting spinal alignment-insights into a new paradigm and implications in deformity correction. Spine J. 2017;17:183–189. [DOI] [PubMed] [Google Scholar]
- 5.Hey HWD, Teo AQA, Tan KA, et al. How the spine differs in standing and in sitting- important considerations for correction of spinal deformity. Spine J. 2017;17:799–806. [DOI] [PubMed] [Google Scholar]
- 6.Suzuki H, Endo K, Sawaji Y, et al. Radiographic assessment of spinopelvic sagittal alignment from sitting to standing position. Spine Surg Relat Res. 2018;2:290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30:346–353. [DOI] [PubMed] [Google Scholar]
- 8.Laouissat F, Sebaaly A, Gehrchen M, Roussouly P. Classification of normal sagittal spine alignment: refounding the Roussouly classification. Eur Spine J. 2018;27:2002–2011. [DOI] [PubMed] [Google Scholar]
- 9.Yu M, Zhao WK, Li M, et al. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur Spine J. 2015;24:1265–1273. [DOI] [PubMed] [Google Scholar]
- 10.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167:875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merchant G, Buelna C, Castañeda SF, et al. Accelerometer-measured sedentary time among Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med Rep. 2015;2:845–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optional patient stance for obtaining a lateral 36′ radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976). 2005;30:427–433. [DOI] [PubMed] [Google Scholar]
- 13.Zhou S, Sun Z, Li W, et al. The standing and sitting sagittal spinopelvic alignment of Chinese young and elderly population: does age influence the differences between the two positions? Eur Spine J. 2020;29:405–412. [DOI] [PubMed] [Google Scholar]
- 14.Protopsaltis TS, Lafage R, Smith JS, et al. The lumbar pelvic angle, the lumbar component of the T1 pelvic angle, correlates with HRQOL, PI-LL mismatch, and it predicts global alignment. Spine (Phila Pa 1976). 2018;43:681–687. [DOI] [PubMed] [Google Scholar]
- 15.Protopsaltis T, Schwab F, Bronsard N, et al. International Spine Study Group. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. [DOI] [PubMed] [Google Scholar]
- 16.Maekawa A, Endo K, Suzuki H, et al. Impact of pelvic incidence on change in lumbo-pelvic sagittal alignment between sitting and standing positions. Eur Spine J. 2019;28:1914–1919. [DOI] [PubMed] [Google Scholar]
- 17.Sebaaly A, Riouallon G, Obeid I, et al. Proximal junctional kyphosis in adult scoliosis comparison of four radiological predictor models. Eur Spine J. 2018;27:613–621. [DOI] [PubMed] [Google Scholar]
- 18.Janjua MB, Tishelman JC, Vasquez-Montes D, et al. The value of sitting radiographs: analysis of spine flexibility and its utility in preoperative planning for adult spinal deformity surgery. J Neurosurg Spine. 2018;29:414–421. [DOI] [PubMed] [Google Scholar]
- 19.Sebaaly A, Gehrchen M, Silvestre C, et al. Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J. 2020;29:904–913. [DOI] [PubMed] [Google Scholar]
- 20.Moon MS, Lee H, Kim ST, Kim SJ, Kim MS, Kim DS. Spinopelvic orientation on radiographs in various body postures: upright standing, chair sitting, Japanese style kneel sitting, and Korean style cross-legged sitting. Clin Orthop Surg. 2018;10:322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]