Abstract
Study design:
Prospective comparative cohort study.
Objectives:
The study aims to elucidate the relationship between Modic endplate changes and clinical outcomes after a lumbar microdiscectomy.
Methods:
Consecutive patients undergoing microdiscectomy for lumbar disc herniation (LDH) were prospectively studied. Pre-operative clinical and radiological parameters were recorded. The pain was assessed by Numeric pain rating scale (NPRS), and functional assessment by Oswestry Disability Index (ODI). Minimal clinically important difference (MCID) in outcome was calculated for both the groups. Complications related to surgery were studied. Follow-up was done at 6 weeks, 3 months, 6 months and 1 year. Mac Nab criteria were used to assess patient satisfaction at 1 year.
Results:
Out of 309 patients, 86 had Modic changes, and 223 had no Modic changes. Both groups had similar back pain (p-value: 0.07) and functional scores (p-value: 0.85) pre-operatively. Postoperatively patients with Modic changes had poorer back pain and ODI scores in the third month, sixth month and 1 year (p-value: 0.001). However, MCID between the groups were not significant (p-value: 0.18 for back pain and 0.58 for ODI scores). Mac Nab criteria at 1 year were worse in Modic patients (p-value: 0.001). No difference was noted among Modic types in the pre-operative and postoperative pain and functional outcomes. Four patients in Modic group (4.7%) and one patient in the non-Modic group (0.5%) developed postoperative discitis (p-value: 0.009).
Conclusions:
Preoperative Modic changes in lumbar disc herniation is associated with less favorable back pain, functional scores and patient satisfaction in patients undergoing microdiscectomy.
Keywords: lumbar disc herniation, microdiscectomy, modic changes, endplate changes, low back pain, outcomes, discitis
Introduction
Microdiscectomy is the gold standard for the surgical treatment of symptomatic lumbar disc herniation. 1 Patients presenting with persistent radicular leg pain after a trial of conservative treatment and whose symptoms correlate with disc herniation in magnetic resonance imaging (MRI) have been shown to have a high success rate (75-80%) after a microdiscectomy.2,3 However, in some patients, though the radicular pain is relieved, the preoperative back pain persists after microdiscectomy, and they experience poor functional outcomes after surgery.
Modic et al. in 1988 described the degenerative vertebral endplate and subchondral marrow changes in MRI. 4 Since then, numerous studies have shown that Modic changes have a strong association with low back pain.5-7 Modic changes are quite frequent, with a 43% prevalence rate in patients with non-specific low back pain and only 6% in the general population. 8 Various theories were proposed for the etiology of Modic changes like degeneration, trauma, inflammation and infection, but the exact pathogenesis underlying Modic change is unclear.
Although few studies correlated Modic changes and clinical outcomes after microdiscectomy, the results were inconclusive.9-13 Hence, we aim to analyze whether the presence of Modic changes in preoperative MRI influences the clinical outcomes after a microdiscectomy.
Materials and Methods
Study Design
After Institutional Review Board approval, a prospective comparative cohort study was conducted on consecutive patients undergoing microdiscectomy for lumbar disc herniation, at a single center from April 2018 to February 2019. Informed written consent to participate in study was obtained from all patients. Patients with symptomatic single-level disc herniation, with correlating MRI findings, between 18 to 65 years of age, and who failed a trial of conservative management with medicines, physiotherapy or selective nerve root blocks and epidural steroids were included. Patients with cauda equina syndrome and significant motor deficits were operated at the earliest and were also included. Patients with prior lumbar surgery, lumbar instability, severe canal stenosis, facetal hypertrophy, high risk for anesthesia, and patients who were lost to follow up during the study period were excluded. A total of 341 microdiscectomy procedures were done during the study period, and 309 patients who satisfied the inclusion criteria formed the study population.
Clinical Assessment
Patient’s demographic details, body mass index (BMI), smoking habits, comorbidities, duration of symptoms, findings of neurological examination were recorded preoperatively. Pain assessment was done by Numeric pain rating scale (NPRS) and functional assessment by Oswestry disability index (ODI) at defined periods (preoperative, at the time of discharge, 6 weeks, 3 months, 6 months and 1 year). At the end of 1 year, patient satisfaction with surgery was assessed using MacNab’s criteria. Patients were asked to rate their level of well-being with answers of—excellent, good, fair, or poor. The minimum clinically important difference (MCID) in outcomes was calculated as described by Solberg et al. 14 Complications related to surgery were studied.
Radiological Assessment
Radiographs of the lumbar spine in flexion and extension views were taken to rule out segmental instability. Disc herniation was confirmed by 1.5 Tesla MRI (Siemens), and type of herniation (Extrusion, Protrusion, and Sequestration), level, and location were noted. Preoperative T1 and T2 weighted MRI sequences were assessed for the presence of Modic changes and were classified into Type 1 (hypo-intense signal in T1 and hyper-intense signal in T2) and Type 2 (hyper-intense signal in T1 and iso-intense or slightly increased signal in T2). Location of the Modic change in relation to endplate was noted as entire, central, anterior, or posterior. Disc degeneration (DD) was graded using the Modified Pfirrmann scale, 15 and endplate damage was assessed by Total endplate score (TEPS). 16 Computed Tomography (CT) scan was done in selected patients with endplate erosions in MRI. A senior musculoskeletal radiologist reported all findings of MRI.
Surgical Procedure
All patients underwent a standard microdiscectomy procedure by either of 3 senior spine surgeons. Extruded disc fragments were excised, annulus rent identified or created to remove loose fragments in the disc space, and nerve roots were adequately decompressed. Two doses of an antibiotic (Cefuroxime 1.5 g), first at a half-hour before incision and second at 12 hours postoperatively was given. Patients were assisted with mobilization on the same day and discharged from the hospital on the second day after a wound check. Restricted activity was advised for 4 weeks, and then back strengthening exercises were started, and a gradual return to routine activities was allowed.
Follow Up
All patients were followed up at 6 weeks, 3 months, 6 months, 1 year either by hospital visits or telephonic interviews.
Statistical Analysis
Based on the presence or absence of Modic changes in the baseline MRI, patients were grouped into two—Modic and non-Modic. Modic group was further divided into subgroups based on the type of Modic changes—Type 1 and Type 2. Descriptive and statistical analyses were performed on preoperative variables like age, gender, BMI, smoking history, diabetes, duration of symptoms, and neurological deficit to understand the evenness of distributions across the groups. Later MRI assessments and clinical outcomes were assessed statistically to understand the effects of Modic changes using student’s t-test for continuous variables and chi-square tests for categorical variables. Relationships were considered significant for p-values < 0.05.
Results
Out of 309 patients, 86 had Modic changes, and 223 had no Modic changes. 202 patients were male, and 107 were female (M: F—1.9: 1), and the mean age of patients in Modic group was 43.1 years and non-Modic group was 42.2 years (range: 18-65 years). Mean BMI was 25.3 (Modic) and 24.8 (non-Modic). There were no differences in baseline demographic characteristics between 2 groups, including smoking history and medical comorbidities (Table 1). Minimum follow up was 1 year (range 12-24 months).
Table 1.
Clinical and MRI Characteristics of the Study Cohort.
| Modic | Non-Modic | p-valuea | |
|---|---|---|---|
| Number of Patients | 86 (27.8%) | 223 (72.2%) | |
| Sex (Male: Female) | 50:36 | 152:71 | 0.097 |
| Age (Years) | 43.1 ± 10.3 | 42.2 ± 13.4 | 0.533 |
| BMI (Kg/m2) | 25.3 ± 4.4 | 24.8 ± 3.5 | 0.318 |
| History of smoking | 9 | 17 | 0.420 |
| Diabetes | 11 | 32 | 0.723 |
| Duration of symptoms | |||
| Back pain (weeks) | 69.6 (1week- 10 years) | 54.5 (1 week- 10 years) | 0.296 |
| Leg pain (weeks) | 13.6 (3 days- 1 year) | 21.2 (1 week- 1 year) | 0.035 |
| Neurological status | |||
| Normal neurology (Motor power—MRC <3/5) | 64 (74.40%) | 171 (76.70%) | 0.801 |
| 19 (22.10%) | 47 (21.10%) | ||
| Cauda equina Syndrome (Percentage within group) | 3 (3.50%) | 5 (2.20%) | |
| MRI | |||
| Grade of Disc Degeneration (DD) | 4.9 ± 1.38 | 4.1 ± 1.2 | 0.001 |
| Total endplate score (TEPS) | 6.7 ± 2.2 | 3.8 ± 1.3 | 0.001 |
| Type of herniation | |||
| Extrusion | 80 (93.00%) | 175 (78.50%) | 0.005 |
| Protrusion | 3 (3.50%) | 39 (17.50%) | |
| Sequestration (percentage within group) | 3 (3.50%) | 9 (4.00%) |
MRC: Medical Research Council grade.
a Boldface values show parameters with statistically significant difference (p-value < 0.05).
Mean duration of symptoms in Modic patients was 69.6 weeks for back pain and 13.6 for leg pain, compared to 54.5 weeks and 21.2 weeks in non-Modic patients. Motor weakness (MRC grade ≤3) was seen in 19 patients (22.10%) in Modic group and 47 patients (21.10%) in non-Modic group. Only 8 patients in our study group (3 in Modic (3.50%) and 5 (2.20%) in non-Modic) presented with cauda equina syndrome. No statistical difference in clinical presentations were seen between 2 groups except for a lesser duration of leg pain in Modic patients (Table 1).
The most common level of disc herniation noted was L4-5 (49.5%) and L5-S1 (46.9%). Regarding the type of herniation, 255 patients had extrusion (Modic group-80, non-Modic-175), 42 had protrusion (Modic group-3, non-Modic-39), and sequestration was found in 12 patients only (Modic group-3, non-Modic-9) (Table 1). On modified Pfirrmann scoring, the mean grade of disc degeneration was 4.9 in Modic group as compared to 4.1 in the non-Modic group. Total endplate score was 6.7 in Modic group and 3.8 in non-Modic group. Both scores were significantly higher in Modic group (Table 1). Based on the location of Modic change in relation to the endplate, the most common location noted was “entire” (51.2%) followed by “central” (26.7%), “anterior” (16.3%), “posterior” (5.8%) (Figure 1).
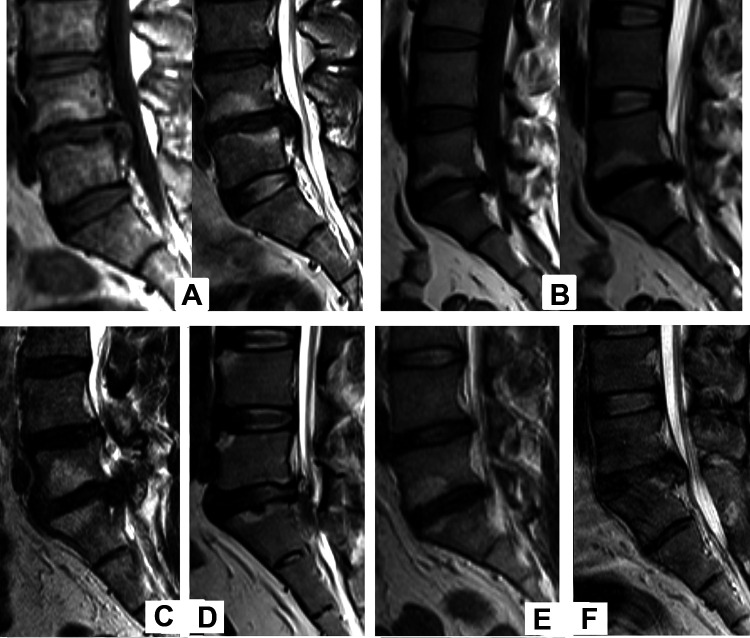
Figure 1.
Sagittal T1 and T2-weighted MRI showing (A) Type 1 Modic change, (B) Type 2 Modic change. Based on the location of Modic change in relation to endplate (T2 image), further divided into (C) Entire, (D) Central, (E) Anterior, and (F) Posterior.
Pain Outcomes
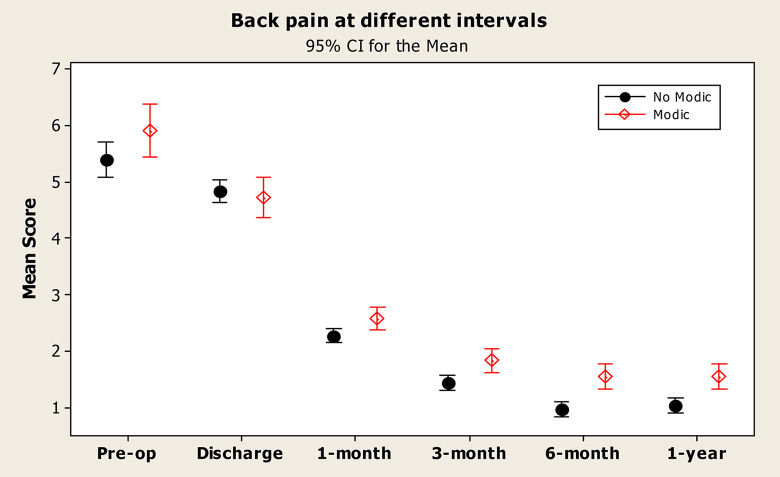
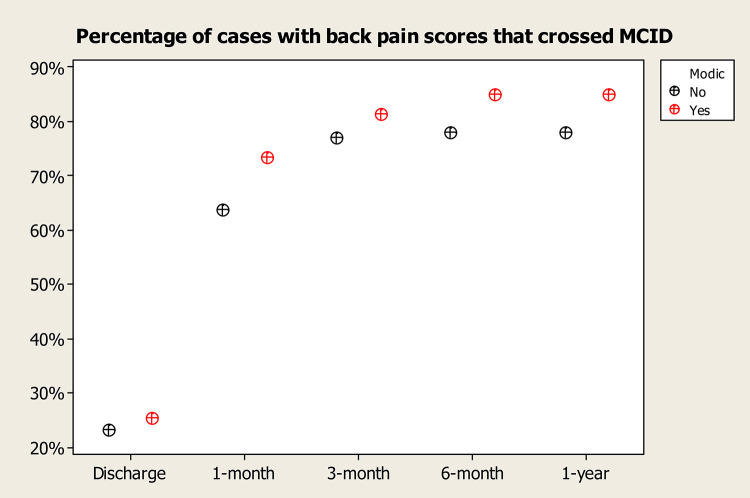
On clinical pain outcome analysis, NPRS for back pain improved from a mean of 5.9 (preoperative) to 1.6 (postoperative) at the end of 1 year in Modic patients and 5.4 (preoperative) to 1.1 (postoperative) in non-Modic patients (Figure 2). Statistically significant improvement in back pain was seen in non-Modic group as compared to Modic group (p-value: 0.001). Leg pain NPRS score improved from a mean of 8 (preoperative) to 0.6 (postoperative) at the end of 1 year in Modic patients, in comparison to 7.8 (preoperative) to 0.5 (postoperative) in non-Modic group (Figure 3). No statistically significant difference noted in the improvement of leg pain between both groups (Table 2). Both the Modic and non-Modic group had good outcomes and met MCID with relation to back pain NPRS, leg pain NPRS in comparison to preoperative status. However, the MCID between the Modic and Non-Modic group was not significant (p-value: 0.18 for back pain and 0.62 for leg pain, at 1 year) (Table 3) (Figures 4 and 5).
Figure 2.
Numeric pain rating scale (NPRS) for back pain at different time intervals. NPRS improved in both groups postoperatively with statistically significant improvement in back pain noted in non-Modic group as compared to Modic group.
Figure 3.
Numeric pain rating scale (NPRS) for leg pain at different time intervals. NPRS improved in both Modic and non-Modic groups postoperatively with no statistically significant difference between the 2 groups.
Table 2.
Pain Scores, Functional Outcomes and Patient Satisfaction by MacNab Outcome Analysis in Modic and Non-Modic Group.
| Modic | Non-Modic | p-valuea | |
|---|---|---|---|
| Numeric Pain Rating Scale | |||
| Back pain | |||
| Pre-operative | 5.9 ± 2.2 | 5.4 ± 2.4 | 0.073 |
| At discharge | 4.7 ± 1.7 | 4.8 ± 1.6 | 0.611 |
| 6 weeks | 2.6 ± 0.9 | 2.3 ± 1.0 | 0.011 |
| 3 months | 1.8 ± 1.0 | 1.5 ± 1.0 | 0.002 |
| 6 months | 1.6 ± 1.0 | 0.9 ± 1.0 | <0.001 |
| 1 year Post-operative | 1.6 ± 1.1 | 1.1 ± 1.0 | <0.001 |
| Leg pain | |||
| Pre-operative | 8.0 ± 1.4 | 7.8 ± 1.6 | 0.371 |
| At discharge | 2.2 ± 1.6 | 2.3 ± 1.4 | 0.544 |
| 6 weeks | 1.3 ± 1.2 | 1.1 ± 0.9 | 0.128 |
| 3 months | 0.8 ± 0.9 | 0.7 ± 1.0 | 0.606 |
| 6 months | 0.6 ± 0.9 | 0.6 ± 0.9 | 0.432 |
| 1 year post-operative | 0.6 ± 0.9 | 0.5 ± 0.9 | 0.216 |
| Oswestry Disability Index | |||
| Pre-operative | 68.3 ± 12 | 67.7 ± 39.2 | 0.852 |
| At discharge | 60.2 ± 10 | 57.6 ± 9.5 | 0.040 |
| 6 weeks | 40.8 ± 7.0 | 41.2 ± 21.3 | 0.832 |
| 3 months | 29.2 ± 6.1 | 27.4 ± 7.0 | 0.028 |
| 6 months | 23.4 ± 5.8 | 19.9 ± 6.7 | <0.001 |
| 1 year post-operative | 23.4 ± 5.8 | 18.9 ± 6.9 | <0.001 |
| MacNab outcome at 1 year | |||
| Excellent | 26 (30.2%) | 122 (54.7%) | <0.001 |
| Good | 37 (43%) | 77 (34.5%) | |
| Fair | 22 (25.6%) | 22 (9.9%) | |
| Poor | 1 (1.2%) | 2 (0.9%) |
a Boldface values show parameters with statistically significant difference (p-value < 0.05).
Table 3.
Percentage of Patients Who Had Minimal Clinically Important Difference (MCID).
| Percentage of patients with MCID and p value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Discharge | 1 month | 3 months | 6 months | 1 year | ||||||
| Back Pain (NPRS) | ||||||||||
| Modic | 25.6 | 0.68 | 73.3 | 0.11 | 81.4 | 0.42 | 84.9 | 0.18 | 84.9 | 0.18 |
| Non Modic | 23.3 | 63.7 | 77.1 | 78 | 78 | |||||
| Leg pain (NPRS) | ||||||||||
| Modic | 90.7 | 0.49 | 94.2 | 0.12 | 97.7 | 0.67 | 97.7 | 0.67 | 97.7 | 0.62 |
| Non Modic | 87.9 | 98.2 | 98.2 | 98.2 | 98.7 | |||||
| ODI | ||||||||||
| Modic | 17.4 | 0.47 | 77.9 | 0.31 | 95.3 | 0.99 | 100 | 0.33 | 100 | 0.58 |
| Non Modic | 13.5 | 72.2 | 94.6 | 97.8 | 98.2 | |||||
Figure 4.
Percentage of patients with back pain scores that met minimum clinically important difference (MCID) at various time intervals.
Figure 5.
Percentage of patients with leg pain scores that met minimum clinically important difference (MCID) at various time intervals.
Functional Outcomes
Functional outcomes measures showed improvement in ODI score from a mean 68.3 (preoperative) to 23.4 (1 year postoperative) in Modic patients as compared to an improvement from 67.7 (preoperative) to 19 (1 year postoperative) in non-Modic patients (Figure 6). Statistically, a significant difference was noted between 2 groups, with Modic patients having worse ODI scores at the end of 1 year (p-value: 0.001) (Table 2). Though both Modic and non-Modic groups had significant improvement in ODI and met MCID when compared to preoperative status, the MCID between the Modic and Non-Modic groups was not significant (p-value: 0.58, at 1year) (Table 3) (Figure 7).
Figure 6.
Functional outcome measures using Oswestry Disability Index (ODI) at different time intervals. ODI scores showed improvement in both groups with statistically significant difference noted in non-Modic group.
Figure 7.
Percentage of patients with Oswestry disability index (ODI) scores that met minimum clinically important difference (MCID) at various time intervals.
Patient Satisfaction
Mac Nab outcome analysis for satisfaction after surgery at the end of 1 year showed 73.2% excellent or good outcomes in Modic patients and 89.2% in non-Modic patients. Fair or poor results were noted in 26.8% of Modic patients compared to 10.8% of non-Modic patients. Pearson’s chi-square test showed that MacNab’s outcome was significantly worse in Modic patients (Figure 8).
Figure 8.
Mac Nab outcome analysis for satisfaction after surgery at the end of 1 year. Modic group patients had worse outcomes in comparison with non-modic group.
Modic Subgroups
In the Modic group, Type 1 was seen in 6 patients (7%), Type 2 in 68 patients (79%), and 12 (14%) had mixed (Type 1 and 2) changes (Figure 1). None of the study population had Type 3 changes. Mixed changes were grouped under Type 1, and on subgroup analysis, there was no difference in the pain, functional outcomes, or patient satisfaction between 2 types (Table 4). Incidence of postoperative discitis was 11.1% (2 out of 18 patients) in Type 1 Modic changes, which was significantly higher compared to 2.9% (2 out of 68 patients) in Type 2 Modic changes.
Table 4.
Radiological Assessment, Pain Scores, Functional Outcome and Patient Satisfaction Analysis of Modic Subgroups—Type 1 and Type 2.
| Type 1 Modic | Type 2 Modic | p-valuea | |
|---|---|---|---|
| Number | 18 (5.8%) | 68 (22%) | |
| Disc Degeneration grade | 4.9 ± 1.3 | 4.8 ± 1.4 | 0.728 |
| Total Endplate Score | 6.8 ± 1.9 | 6.6 ± 2.3 | 0.796 |
| Numeric Pain Rating Scale | |||
| Back pain | |||
| Pre-operative | 5.4 ± 1.8 | 6 ± 2.3 | 0.260 |
| 1 year post-operative | 1.8 ± 1.3 | 1.5 ± 0.9 | 0.285 |
| Leg pain | |||
| Pre-operative | 8.4 ± 0.7 | 7.9 ± 1.6 | 0.063 |
| 1 year post-operative | 0.8 ± 0.8 | 0.6 ± 0.9 | 0.428 |
| Oswestry Disability Index | |||
| Pre-operative | 72.7 ± 7.7 | 67.1 ± 12.7 | 0.023 |
| 1 year post-operative | 25.2 ± 6.4 | 22.9 ± 5.6 | 0.178 |
| Mac Nab outcome at 1 year | |||
| Excellent | 4 (22.2%) | 22 (32.4%) | |
| Good | 7 (38.9%) | 30 (44.1%) | |
| Fair | 7 (38.9%) | 15 (22.1%) | |
| Poor | 0 | 1 (1.5%) | 0.491 |
a Boldface values show parameters with statistically significant difference (p-value < 0.05).
Based on the location of Modic change (entire, central, anterior, posterior) in relation to endplate (Figure 1), there was no difference in back pain (p-value: 0.696), ODI score (p-value: 0.528) and patient satisfaction (p-value: 0.453) between different types at the end of 1 year.
When evaluated for confounding factors age, BMI, and smoking, we found that patients with age more than 50 years were less satisfied with surgery in both groups. Also, within the non-Modic group, patients with age >50 years showed comparatively less favorable function scores at 1 year. No statistical difference in outcomes was found in both groups of patients with regard to BMI (p-value: 0.71) and smoking habit (p-value: 0.56) (Tables 5 and 6).
Table 5.
Pain Scores, Functional Outcome and Patient Satisfaction Analysis in Relation to Age, BMI and Smoking in Modic Patients.
| Age (years) | p valuea | BMI (Kg/m2) | p value | Smoking | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| ≤50 | >50 | <25 | ≥25 | N | Y | ||||
| Back pain | |||||||||
| Pre op | 5.6 | 7 | 0.002 | 5.7 | 6.2 | 0.30 | 6 | 4.8 | 0.29 |
| 1 year | 1.5 | 1.6 | 0.79 | 1.5 | 1.7 | 0.39 | 1.6 | 1.6 | 0.99 |
| Leg pain | |||||||||
| Pre op | 8 | 8 | 0.79 | 8 | 8 | 0.95 | 8 | 8.2 | 0.64 |
| 1 year | 0.6 | 0.9 | 0.18 | 0.8 | 0.4 | 0.02 | 0.6 | 0.7 | 0.93 |
| ODI | |||||||||
| Pre op | 68 | 68.7 | 0.78 | 70.5 | 65.6 | 0.06 | 68.2 | 68.6 | 0.94 |
| 1 year | 22.9 | 25 | 0.07 | 23.1 | 23.8 | 0.62 | 23.5 | 22.7 | 0.75 |
| Mac Nab (at 1 yr) | |||||||||
| Excellent | 55.5 | 29.5 | 29.8 | 30.8 | 28.6 | 44.4 | |||
| Good | 27.7 | 60.2 | 42.6 | 43.6 | 45.5 | 22.2 | |||
| Fair | 15.5 | 10.2 | 27.7 | 23.1 | 24.7 | 33.3 | |||
| Poor | 1.4 | 0 | 0.001 | 0 | 2.6 | 0.71 | 1.3 | 0 | 0.56 |
a Boldface values show parameters with statistically significant difference (p-value < 0.05).
Table 6.
Pain Scores, Functional Outcome and Patient Satisfaction Analysis in Relation to Age, BMI and Smoking in Non-Modic Patients.
| Age (years) | p valuea | BMI (kg/m2) | p value | Smoking | p value | ||||
|---|---|---|---|---|---|---|---|---|---|
| ≤50 | >50 | <25 | ≥25 | N | Y | ||||
| Back pain | |||||||||
| Pre op | 5.2 | 5.8 | 0.08 | 5.3 | 5.5 | 0.7 | 5.3 | 6.5 | 0.08 |
| 1 year | 1 | 1.2 | 0.28 | 1.1 | 1.1 | 0.98 | 1 | 1.4 | 0.09 |
| Leg pain | |||||||||
| Pre op | 8 | 7.5 | 0.3 | 7.9 | 7.8 | 0.46 | 7.8 | 8.2 | 0.29 |
| 1 year | 0.5 | 0.6 | 0.19 | 0.5 | 0.5 | 0.91 | 0.5 | 0.9 | 0.23 |
| ODI | |||||||||
| Pre op | 68.1 | 66.8 | 0.73 | 64.9 | 70.9 | 0.28 | 67.8 | 66.3 | 0.73 |
| 1 year | 17.7 | 21.9 | 0.001 | 19.2 | 18.7 | 0.56 | 18.8 | 21 | 0.17 |
| Mac Nab (at 1 yr) | |||||||||
| Excellent | 63.9 | 33.8 | 54.2 | 55.2 | 55.8 | 41.2 | |||
| Good | 23.9 | 58.8 | 33.1 | 36.2 | 34 | 41.2 | |||
| Fair | 11 | 7.4 | 11.9 | 7.6 | 9.2 | 17.6 | |||
| Poor | 1.3 | 0 | 0.001 | 0.8 | 1 | 0.76 | 1 | 0 | 0.54 |
a Boldface values show parameters with statistically significant difference (p-value < 0.05).
Complications
4 patients in the Modic group (4.7%) developed discitis in the immediate postoperative period (within 10 days), and all of them underwent debridement. 2 patients had Modic type 1 change and 2 patients had Type 2 Modic changes. All 4 patients had endplate erosions in the preoperative CT scan. Pseudomonas was grown in 3 out of 4 patients, and all 3 patients ended up with third surgery in the form of instrumented stabilization and fusion of the infected vertebral segment (Figure 9). Other patients had no growth in culture and healed with debridement and antibiotics. In non-Modic patients, 1 patient (0.5%) presented with discitis after 5 weeks of microdiscectomy. He underwent debridement, and culture showed Pseudomonas growth.
Figure 9.
A case example of postoperative discitis. (A) Type 2 Modic change (sagittal T1 and T2 weighted MRI) with endplate erosions in pre-operative CT scan (arrow). (B) 10 days postoperative MRI (sagittal and axial) showing discitis. The patient underwent debridement and interbody fusion (C). Follow-up X-ray at 1 year shows good healing.
Recurrent disc prolapse was seen in 1 patient in the Modic group and 4 patients in the non-Modic group, and all 5 patients required a second surgery. The mean duration for recurrence of disc herniation was 6.8 months (range: 6 weeks-14 months). There was no statistical difference in the recurrence rate between the 2 groups (p-value: 0.694). Similarly, no difference in intraoperative and postoperative complications was noted. There were 4 cases of dural tears and 2 cases of persistent radiculopathy. All dural tears were managed with dural patch and watertight closure. Re-exploration and removal of residual disc fragments were done for 2 patients with persistent radiculopathy.
Discussion
Previous studies on Modic change and outcomes after microdiscectomy reported conflicting results and were limited by small sample sizes or retrospective study design. 9 Our study prospectively analyzed the presence of Modic changes, Modic type, its location in relation to endplate in the preoperative MRI and correlated with the clinical outcomes after lumbar microdiscectomy. The confounding factors like age, body mass index, smoking history on the outcomes also were analyzed.
The prevalence of Modic change was 27.8% in our study cohort. Modic change was associated with a higher grade of disc degeneration and a higher total endplate score in our study. Kerttula et al. made a similar observation in their prospective study of 54 patients with type I Modic change. 17 They found an increase in the size of endplate lesions, a decrease in the disc height, and change in disc signal intensity at the end of 1-year and postulated that Modic change is a sign of fast progressive pathologic degeneration.
Outcomes in Modic vs Non-Modic
Studies have shown that Modic change is associated with chronic, non-specific low back pain.5-7 However, in our study, the duration of back pain and its severity in the pre-operative period is similar to patients without Modic changes. Postoperatively radicular pain improved significantly in all patients, regardless of the presence of pre-operative Modic changes. However, back pain scores, functional scores, and satisfaction scores were worse in the Modic group at 3 months, 6 months and 1 year. A similar finding was noted by Chin et al. in a prospective study on 30 patients undergoing microdiscectomy. Patients without Modic changes showed a mean improvement in VAS (Visual Analogue scale) for low back pain by 75% and ODI scores by 84% at the end of 6 months as compared to 67% and 58% respectively in patients with Modic changes. 10 Sorlie et al. prospectively analyzed 178 patients of disc herniation after microdiscectomy and found that at the end of 1 year, Type 1 Modic changes and smoking had a negative impact on the improvement in back pain. 12 Lurie et al. in their study on the MRI predictors of surgical outcomes for lumbar disc herniation, showed type 1 Modic change had worse clinical outcomes after discectomy. 11 Ohtori et al. in a prospective study on 45 patients undergoing microdiscectomy, refuted above correlations as they did not find any difference between Type 1 Modic and non-Modic patients with regard to relief of back pain. 13 A systematic review by Laustsen et al. studied the influence of Modic changes on outcomes following surgery. 9 They reported a less favorable improvement in back pain scores and ODI scores after discectomy. These authors however questioned whether the difference surpasses MCID. Our study have documented that though statistically significant difference in back pain and ODI scores were noted between Modic group and Non-Modic group, it did not meet MCID.
Does the Type of Modic Changes Affect Outcomes?
Type 2 Modic changes were most common (79%) in our cohort. Type 2 is considered to be a more benign, fatty replacement of marrow. In contrast, Type 1 Modic is considered as an aggressive lesion with an active inflammatory process in the marrow and is shown to have the strongest association with chronic low back pain. 18 Modic changes are not stable and can convert from one type to another, and each represents different stages of the same pathological process. 19 Type 3 Modic changes represent sclerosis and tend to be present in elderly individuals. They are reported to be relatively rare (<5%) even in larger study samples.20,21 Our study population was less than 65 years with a mean age around 43 years; this could possibly explain the absence of Type 3 changes in our study group. In our study, there was no difference found between types of Modic change with regard to clinical, functional outcomes, and patient satisfaction at 1 year of surgery. However, the incidence of postoperative discitis was higher in Type 1 Modic changes.
Etiopathogenesis of Modic Changes
Modic et al., in their original paper, suggested mechanical stress and microfractures to vertebral endplates to be the cause of Modic change. 4 Later, inflammatory mediators in the degenerated discs were implicated in marrow changes. 22 The isolation of Propionibacterium acnes in the disc material of patients undergoing discectomy by Stirling et al. led to the hypothesis of sub-clinical infection in the etiopathogenesis of degenerative disc disorders. 23 Albert et al. were the first to propose a bacterial cause in Modic type 1 change following annular and endplate damage. 18 They proposed that anaerobic bacteria could enter the disc and set in a low-grade infection, and Modic changes were the visible sign of surrounding inflammation. In a different prospective study, they followed 61 patients who underwent discectomy and culture of disc samples for 2 years. 24 They found that out of 46% who had culture positive for anaerobic organisms, 80% developed new Modic changes. However, none of those with aerobic bacteria, and only 44% of patients with negative cultures developed new Modic changes. Albert et al. also assessed the effect of antibiotic treatment (amoxicillin–clavulanate) in a pilot study of 32 patients with low back pain and Modic type 1 changes. 25 After treatment, they noted clinically relevant and statistically significant improvement in all outcome measures. They again confirmed the findings of these studies in a randomized control trial (RCT). 26
Ohtori et al. followed up 71 patients with Modic Type 1 changes for 2 years and reported that 4.2% were diagnosed with pyogenic spondylitis using a blood investigation, MRI Scan, biopsy, and Positron Emission Tomography (PET) scan. 27 Ninomiya et al. have demonstrated a positive correlation between the presence of Type 1 Modic changes and the occurrence of postoperative surgical site infection in patients undergoing lumbar laminectomy, and they hypothesized that vertebral edema might help bacteria to migrate hematogenously into the disc space. 28 In our study, the relatively high incidence of postoperative discitis in the Modic group, more so in Type 1 Modic, and the finding of preoperative endplate erosions in patients who developed discitis supports the hypothesis of low-grade infection in Modic changes.
Significance and Limitations of the Study
The interpretation of the results of this study warrants caution. Although a statistically significant difference in back pain, ODI score was observed between the Modic and non-Modic group, the noted difference may not be clinically significant, as MCID between the groups did not show a significant difference. The unequal number of Type 2 (79%) and Type 1 Modic changes (21%), in our study, could have possibly resulted in the insignificant difference and whether an equal number of Type 1 and Type 2 Modic changes would have shown a significant difference in outcomes remains to be seen. Though the location of Modic change was studied, the volume of Modic changes and its effect on outcomes was not evaluated in our study. Patients with cauada equina syndrome and neuro deficit tend to have poor outcomes in comparison to patients with normal neurology. As our study population had similar numbers of patients with neuro deficit in both the Modic and Non-Modic group, we believe while comparing outcomes between Modic and non-Modic group, this is unlikely to cause a bias. However, no separate analysis of outcomes between patients with cauda equina syndrome, neuro deficit, and normal neurology was made. Since the study population included patients who underwent microdiscectomy, sequestrated or protrusion type which is more likely to conservatively managed were less in number. Hence, a comparative analysis of outcomes between types of herniation was not possible. In our study, the Modic group had greater numbers of postoperative spondylodiscitis (4.7%) compared to the non-Modic group (0.5%); however, the overall incidence of spondylodiscitis was low. Also, Type 1 Modic changes are often confused with early spondylodiscitis and remain a grey area. Out of 4 postoperative spondylodiscitis in Modic group, two had Type 1 Modic changes with endplate erosions, whether they were an early spondylodiscitis remains speculative. More focused research is needed in this subject.
Conclusion
Our study has shown a negative association between the presence of Modic change in preoperative MRI and postoperative back pain, functional outcomes and patient satisfaction at 1 year in patients with lumbar disc herniation undergoing microdiscectomy. However, the difference was not clinically significant. Modic changes were associated with higher grades of disc degeneration and higher Total endplate scores. However, no difference in clinical outcomes was seen between different types of Modic changes. We also found a higher incidence of postoperative discitis and the need for repeat procedures in patients with Modic changes.
Abbreviations
- BMI
Body Mass Index
- CT
Computed Tomography
- MCID
Minimal clinically important difference
- MRI
Magnetic Resonance Imaging
- MRC
Medical Research Council grade
- NPRS
Numeric Pain Rating scale
- ODI
Oswestry Disability Index
- PET
Positron Emission Tomography
- VAS
Visual Analogue Scale.
Footnotes
Authors’ Note: The study was approved by Institutional Review Board of Ganga Medical centre and Hospitals (Registered with CDSCO-Regn no: ECR/1146/Inst/TN/2018). IRB Approval No of Project: 2018/05/05.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was self-funded by Ganga orthopaedic research and education foundation (GOREF).
ORCID iD: Shanmuganathan Rajasekaran, MS, DNB, MCh, PhD  https://orcid.org/0000-0001-6043-006X
https://orcid.org/0000-0001-6043-006X
Ajoy Prasad Shetty T., MS, DNB  https://orcid.org/0000-0001-5885-7152
https://orcid.org/0000-0001-5885-7152
Kanna P. Rishi Mugesh, MS, MRCS, FNB  https://orcid.org/0000-0001-5817-4909
https://orcid.org/0000-0001-5817-4909
T. Pushpa B., DNB, FRCR  https://orcid.org/0000-0001-8451-1729
https://orcid.org/0000-0001-8451-1729
References
- 1.Porchet F, Bartanusz V, Kleinstueck FS, et al. Microdiscectomy compared with standard discectomy: an old problem revisited with new outcome measures within the framework of a spine surgical registry. Eur Spine J. 2009;18(Suppl 3):360–366. doi:10.1007/s00586-009-0917-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dewing CB, Provencher MT, Riffenburgh RH, Kerr S, Manos RE. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine. 2008;33(1):33–38. doi:10.1097/BRS.0b013e31815e3a42 [DOI] [PubMed] [Google Scholar]
- 3.Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96(1 Suppl):34–44. doi:10.3171/spi.2002.96.1.0034 [DOI] [PubMed] [Google Scholar]
- 4.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193–199. doi:10.1148/radiology.166.1.3336678 [DOI] [PubMed] [Google Scholar]
- 5.Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15(9):1312–1319. doi:10.1007/s00586-006-0185-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine. 2005;30(10):1173–1180. doi:10.1097/01.brs.0000162396.97739.76 [DOI] [PubMed] [Google Scholar]
- 7.Rahme R, Moussa R. The Modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. Am J Neuroradiol. 2008;29(5):838–842. doi:10.3174/ajnr.A0925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17(11):1407–1422. doi:10.1007/s00586-008-0770-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laustsen AF, Bech-Azeddine R. Do Modic changes have an impact on clinical outcome in lumbar spine surgery? A systematic literature review. Eur Spine J. 2016;25(11):3735–3745. doi:10.1007/s00586-016-4609-y [DOI] [PubMed] [Google Scholar]
- 10.Chin KR, Tomlinson DT, Auerbach JD, Shatsky JB, Deirmengian CA. Success of lumbar microdiscectomy in patients with Modic changes and low-back pain: a prospective pilot study. J Spinal Disord Tech. 2008;21(2):139–144. doi:10.1097/BSD.0b013e318093e5dc [DOI] [PubMed] [Google Scholar]
- 11.Lurie JD, Moses RA, Tosteson ANA, et al. Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine. 2013;38(14):1216–1225. doi:10.1097/BRS.0b013e31828ce66d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sørlie A, Moholdt V, Kvistad KA, et al. Modic type I changes and recovery of back pain after lumbar microdiscectomy. Eur Spine J. 2012;21(11):2252–2258. doi:10.1007/s00586-012-2419-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohtori S, Yamashita M, Yamauchi K, et al. Low back pain after lumbar discectomy in patients showing endplate Modic type 1 change. Spine. 2010;35(13):E596–E600. doi:10.1097/BRS.0b013e3181cd2cb8 [DOI] [PubMed] [Google Scholar]
- 14.Solberg T, Johnsen LG, Nygaard ØP, Grotle M. Can we define success criteria for lumbar disc surgery? Acta Orthop. 2013;84(2):196–201. doi:10.3109/17453674.2013.786634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffith JF, Wang Y-XJ, Antonio GE, et al. Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine. 2007;32(24):E708–E712. doi:10.1097/BRS.0b013e31815a59a0 [DOI] [PubMed] [Google Scholar]
- 16.Rajasekaran S, Venkatadass K, Naresh Babu J, Ganesh K, Shetty AP. Pharmacological enhancement of disc diffusion and differentiation of healthy, ageing and degenerated discs: results from in-vivo serial post-contrast MRI studies in 365 human lumbar discs. Eur Spine J. 2008;17(5):626–643. doi:10.1007/s00586-008-0645-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerttula L, Luoma K, Vehmas T, Grönblad M, Kääpä E. Modic type I change may predict rapid progressive, deforming disc degeneration: a prospective 1-year follow-up study. Eur Spine J. 2012;21(6):1135–1142. doi:10.1007/s00586-012-2147-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albert HB, Kjaer P, Jensen TS, Sorensen JS, Bendix T, Manniche C. Modic changes, possible causes and relation to low back pain. Med Hypotheses. 2008;70(2):361–368. doi:10.1016/j.mehy.2007.05.014 [DOI] [PubMed] [Google Scholar]
- 19.Kuisma M, Karppinen J, Niinimäki J, et al. A three-year follow-up of lumbar spine endplate (Modic) changes. Spine. 2006;31(15):1714–1718. doi:10.1097/01.brs.0000224167.18483.14 [DOI] [PubMed] [Google Scholar]
- 20.Sheng-Yun L, Letu S, Jian C, et al. Comparison of Modic changes in the lumbar and cervical spine, in 3167 patients with and without spinal pain. PLoS One. 2014;9:e114993. doi:10.1371/journal.pone.0114993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Y, Bao J, Yan Q, Wu C, Yang H, Zou J. Distribution of Modic changes in patients with low back pain and its related factors. Eur J Med Res. 2019;24(1):34. doi:10.1186/s40001-019-0393-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burke JG, Watson RWG, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br. 2002;84(2):196–201. doi:10.1302/0301-620x.84b2.12511 [DOI] [PubMed] [Google Scholar]
- 23.Stirling A, Worthington T, Rafiq M, Lambert PA, Elliott TS. Association between sciatica and Propionibacterium acnes. Lancet. 2001;357(9273):2024–2025. doi:10.1016/S0140-6736(00)05109-6 [DOI] [PubMed] [Google Scholar]
- 24.Albert HB, Lambert P, Rollason J, et al. Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J. 2013;22(4):690–696. doi:10.1007/s00586-013-2674-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Albert HB, Manniche C, Sorensen JS, Deleuran BW. Antibiotic treatment in patients with low-back pain associated with Modic changes Type 1 (bone oedema): a pilot study. Br J Sports Med. 2008;42(12):969–973. doi:10.1136/bjsm.2008.050369 [DOI] [PubMed] [Google Scholar]
- 26.Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013;22(4):697. doi:10.1007/s00586-013-2675-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ohtori S, Koshi T, Yamashita M, et al. Existence of pyogenic spondylitis in Modic type 1 change without other signs of infection: 2-year follow-up. Eur Spine J. 2010;19(7):1200–1205. doi:10.1007/s00586-010-1358-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ninomiya K, Fujita N, Hosogane N, et al. Presence of Modic type 1 change increases risk of postoperative pyogenic discitis following decompression surgery for lumbar canal stenosis. J Orthop Sci. 2017;22(6):988–993. doi:10.1016/j.jos.2017.07.003 [DOI] [PubMed] [Google Scholar]