Abstract
Study Design:
Systematic review and meta-analysis.
Objectives:
Malposition of pedicle screws during instrumentation in the lumbar spine is associated with complications secondary to spinal cord or nerve root injury. Intraoperative triggered electromyographic monitoring (t-EMG) may be used during instrumentation for early detection of malposition. The association between lumbar pedicle screws stimulated at low EMG thresholds and postoperative neurological deficits, however, remains unknown. The purpose of this study is to assess whether a low threshold t-EMG response to lumbar pedicle screw stimulation can serve as a predictive tool for postoperative neurological deficit.
Methods:
The present study is a meta-analysis of the literature from PubMed, Web of Science, and Embase identifying prospective/retrospective studies with outcomes of patients who underwent lumbar spinal fusion with t-EMG testing.
Results:
The total study cohort consisted of 2,236 patients and the total postoperative neurological deficit rate was 3.04%. 10.78% of the patients incurred at least 1 pedicle screw that was stimulated below the respective EMG alarm threshold intraoperatively. The incidence of postoperative neurological deficits in patients with a lumbar pedicle screw stimulated below EMG alarm threshold during placement was 13.28%, while only 1.80% in the patients without. The pooled DOR was 10.14. Sensitivity was 49% while specificity was 88%.
Conclusions:
Electrically activated lumbar pedicle screws resulting in low t-EMG alarm thresholds are highly specific but weakly sensitive for new postoperative neurological deficits. Patients with new postoperative neurological deficits after lumbar spine surgery were 10 times more likely to have had a lumbar pedicle screw stimulated at a low EMG threshold.
Keywords: pedicle screws, monitoring, intraoperative, spinal fusion, EMG, electromyography, lumbar
Introduction
Pedicle screw fixation is commonly performed during lumbar spinal fusion due to its biomechanical superiority in providing stability and support to the spine.1,2 However, malposition of pedicle screws in the lumbar spine is associated with complications secondary to spinal cord or nerve root injury. This may manifest clinically as lower extremity radicular pain, numbness, paresthesia, or weakness, possibly requiring revision surgery and an increased length of hospital stay.3,4 Thus, malpositioned screws can have a significant clinical and financial impact on the efficacy of lumbar spine surgery.
Symptomatic pedicle screws are often due to medial or inferior breach, which have been reported at rates between 5% and 31%.4,5 While these malpositioned screws may be redirected intraoperatively, a portion may require revision surgery due to persistent postoperative neurological symptoms. 3 Although intraoperative techniques such as fluoroscopy, radiography, and three-dimensional navigation can identify the structural malposition of screws,6-8 they lack information regarding the functional proximity of the malpositioned screws to the local nerve roots.
Intraoperative triggered electromyographic monitoring (t-EMG) via electrical stimulation of the pedicle screw is an adjunctive technique used for early detection of breach.9,10 The stimulation threshold can indicate the proximity of the screw to the nerve, guiding the surgical team’s decision to reposition if necessary.9-13 A large retrospective analysis of 4,857 screws in 1,078 patients has shown that pedicle screws stimulated at thresholds below 8 mA have a high specificity for medial pedicle breach. 14
However, the current guidelines for electrophysiological monitoring during lumbar fusion procedures,15,16 published in 2005 and updated in 2014, remain uncertain regarding the use of EMG as an intraoperative adjunct during lumbar pedicle screw instrumentation. The authors found that although lumbar pedicle screws stimulated at low EMG thresholds may indicate breach, the association between EMG testing and postoperative neurological outcomes has not been established. Therefore, quantifying the relationship between pedicle screws stimulated at low EMG thresholds and postoperative neurological deficits may elucidate the utility of t-EMG pedicle screw testing during lumbar spinal fusion.
The purpose of the present study was to perform a systematic review and meta-analysis of the relevant literature to assess whether significant, low threshold t-EMG responses evoked from stimulation of lumbar pedicle screws can serve as a predictive tool for postoperative neurological deficit. Due to the low incidence of postoperative neurological deficits in lumbar spinal fusions, a meta-analysis combining multiple studies allows for a larger patient cohort to more accurately assess the predictive value of SSEP changes.
Methods
Protocol and Registration
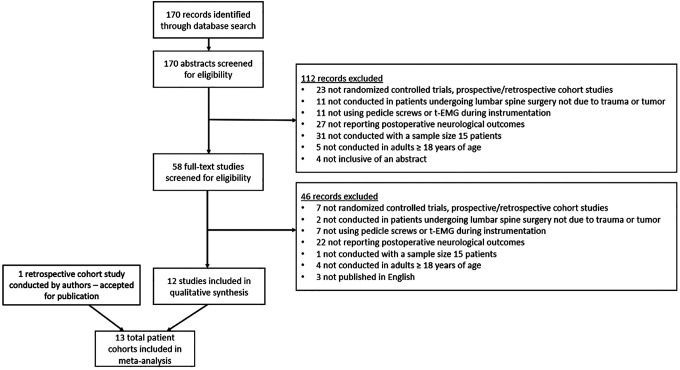
This meta-analysis follows the PRISMA procedure (Figure 1). A study protocol was not registered prior to conducting the study; however, the electronic database searches are included as supplemental materials (Supplemental Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) chart—study elimination process. Footnote: PRISMA chart depicts the elimination process of studies from initial literature search to the finalized patient cohorts. t-EMG, triggered electromyography.
Study Selection
A meta-analysis of the literature using PubMed, Web of Science, and Embase was performed. Published studies that reported EMG responses secondary to lumbar pedicle screw stimulation and postoperative neurological outcomes were included. Patient neurological outcomes were identified as new postoperative neurological deficits localized to the lumbar spine, which included both motor and sensory deficits. All titles and abstracts were independently screened to identify relevant studies. The following keywords were used to identify relevant publications: pedicle screw, EMG/electromyography, lumbar, thoracolumbar. A retrospective cohort study conducted by the authors (Melachuri et al) that was accepted for publication by Spine but not yet published, was also included in this meta-analysis.
Inclusion Criteria
Inclusion criteria included: 1) prospective, retrospective cohort studies and databases, 2) studies conducted in patients undergoing elective lumbar spine surgery that is not due to trauma or tumor, 3) studies that utilized pedicle screws and t-EMG testing 4) studies that reported postoperative neurological outcomes, 5) studies conducted with a sample size ≥ 15 patients, 6) studies conducted in adults ≥ 18 years of age, 7) studies published in English, 8) studies inclusive of an abstract. The following keywords were used to identify relevant publications: pedicle screw, lumbar/thoracolumbar, electromyography/EMG. The study search dated from inception to February 2020.
Data Extraction
The authors (RR, RC, DC) independently screened all titles and abstracts against the inclusion criteria and identified the relevant studies. Studies that did not meet the inclusion criteria were rejected.
For each study, the collected data included study design, spine procedure type, t-EMG stimulation threshold for alarm, number of positive EMG pedicle screws, postoperative neurological deficit outcomes specific to the lumbar spine, and number of true-positives (lumbar pedicle screw stimulated below alarm threshold and postoperative neurological deficit localized to the corresponding side and nerve root), false-positives (lumbar pedicle screw stimulated below alarm threshold but no postoperative neurological deficit localized to the corresponding side and nerve root), false-negatives (no lumbar pedicle screw stimulated below alarm threshold and postoperative neurological deficit localized to the lumbar spine), and true-negatives (no lumbar pedicle screw stimulated below alarm threshold and no postoperative neurological deficit localized to the lumbar spine). The 2 x 2 table was used to calculate sensitivity and specificity as well as the 95% confidence interval.
Statistical Analysis
The statistical analyzes were carried out in R using the MADA package, accessed on March 20, 2020. Analyzes was conducted using a bivariate normal model for the logit-transformed pairs of sensitivities and false-positive rates before the fitting of a linear mixed model. This model preserved the bivariate nature of the data by considering any correlation between sensitivity and specificity. The mean logit sensitivity, specificity, and covariance were estimated from this model. Forest plots and a summary ROC with a 95% confidence ellipsoid were constructed.
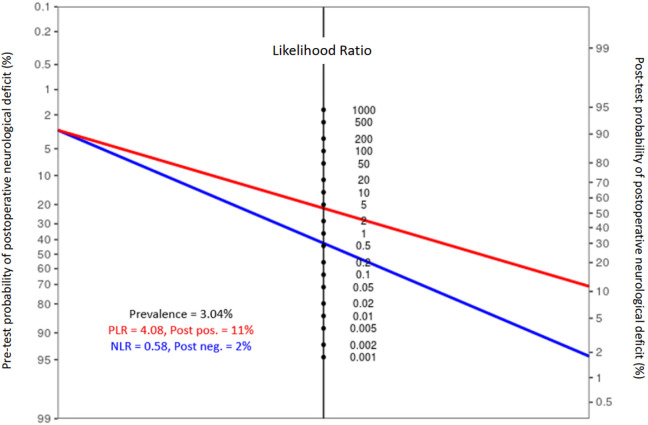
The positive and negative likelihood ratios were calculated for low threshold t-EMG response in predicting postoperative neurological deficit. The likelihood ratios were used to create a Fagan Nomogram with the pre-test probability assumed to be the total incidence of postoperative neurological deficit in the study cohort.
Publication bias and heterogeneity across all studies was assessed with a funnel plot (Supplemental Figure 2). Bias in individual studies with regard to applicability concerns and methods was assessed with the QUADAS-2 tool (Supplemental Figure 3).
Results
Literature Search
One hundred-seventy papers were retrieved on initial search from PubMed, Web of Science, and Embase. After assessing titles and abstracts, 58 papers remained to be screened by full text. Upon full text screening against the inclusion criteria, 12 papers remained (Figure 1). A retrospective cohort study conducted by the authors (Melachuri et al) that was accepted for publication but not yet published, was also included. Statistical analysis included data from these 13 study cohorts. In each of the studies, t-EMG testing was conducted during lumbar pedicle screw placement. The stimulation current threshold that served as an alarm criterion for a positive screw varied between studies and ranged from 5 mA to 11 mA (Table 1). The clinical evaluation period ranged from immediately after the operation to 6 months postoperatively.
Table 1.
Study Characteristics and Demographics.
| Author | Year | Alarm threshold current | Total patients | Total screws | Screws with responses below EMG alarm threshold | Screws repositioned | % male | Mean age |
|---|---|---|---|---|---|---|---|---|
| Alemo 17 | 2010 | 8 mA | 86 | 414 | 28 | 21 | 40.7% | 49 |
| Bindal 18 | 2007 | 7 mA | 25 | 105 | 0 | 0 | 40.0% | 46 |
| Bose 10 | 2002 | 7 mA | 61 | – | – | – | . | 48.4 |
| Clements 19 | 1996 | 11 mA | 25 | 112 | 15 | – | 44.0% | – |
| Darden 20 | 1996 | Determined individually for each pedicle | 132 | 630 | 42 | 21 | 41.70% | 48.7 |
| Feng 21 | 2012 | 10 mA | 16 | 64 | 3 | 3 | 43.80% | – |
| Maguire 22 | 1995 | 6 mA | 29 | 144 | 13 | 10 | 55.2% | 46.5 |
| Papadopoulos 23 | 2005 | 7 mA | 45 | 57 | 0 | 0 | 44.4% | 57.2 |
| Sutter 24 | 2007 | 8 mA | 409 | – | – | – | 39.6% | 62.5 |
| Welch 13 | 1997 | Determined individually for each pedicle | 32 | 164 | 4 | 4 | 53.1% | 46.7 |
| Wood 25 | 2010 | 5 mA | 47 | 212 | 20 | 9 | 38.3% | 51.3 |
| Wood 5 | 2014 | 5 mA | 150 | 627 | 19 | 19 | 44.7% | 58 |
| Melachuri (Retrospective cohort study from authors—accepted for publication) | 2020 | 8 mA | 1179 | 8584 | 187 | – | 44.6 | 55 |
Footnote: EMG, electromyography.
Patient Characteristics
The total study cohort consisted of 2,236 patients. The rate of postoperative neurological deficits in the cohort was 3.04% (68/2236). Of the total patient population, 10.78% (241/2236) incurred at least 1 pedicle screw that was stimulated below the respective EMG alarm threshold. The incidence of postoperative neurological deficits in these patients was 13.28% (32/241). In patients without a low threshold t-EMG response secondary to lumbar pedicle screw stimulation, the deficit rate was only 1.80% (36/1995). Thus, in the cohort with a lumbar pedicle screw stimulated below alarm threshold during t-EMG testing, the postoperative neurological deficit rate was 7.38 times higher than in the cohort without.
In the 9 studies that mentioned screw repositioning, 2,417 lumbar pedicle screws were instrumented in 562 patients. Of these screws, 5.34% (129/2417) were stimulated below their respective EMG alarm thresholds. 67.44% (87/129) of these stimulated screws were repositioned intraoperatively.
Data Analysis
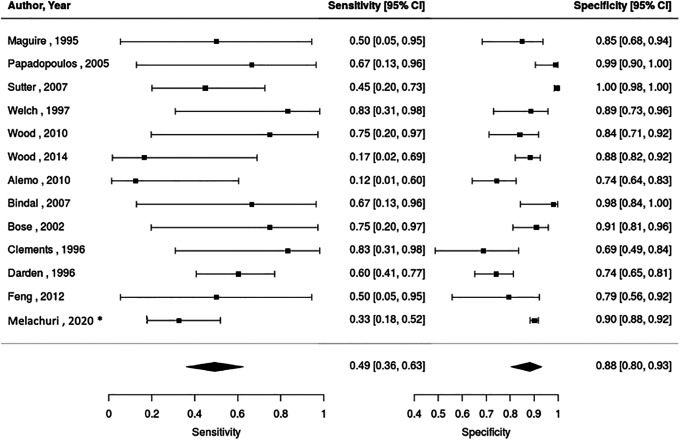
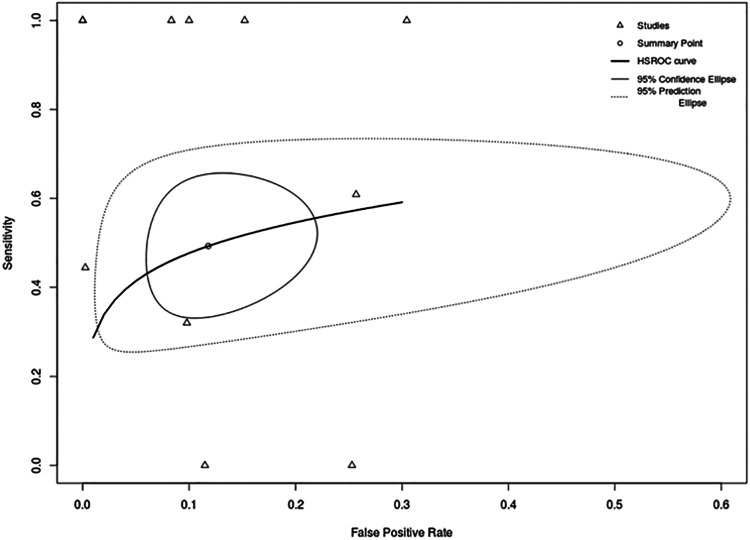
Study sensitivities ranged from 12% to 83% while specificities ranged from 69% to 100% (Figure 2). When we combined data from all of the studies using a bivariate model, sensitivity was 49% (95% CI, 36%-63%) while specificity was 88% (95% CI, 80%-93%). The negative and positive predictive values were 98.2% and 13.3% respectively. The model-based pooled area under the ROC curve was estimated to be 64.2% (Figure 3).
Figure 2.
Forest plot of sensitivity and specificity of pedicle screws stimulated at low t-EMG thresholds in predicting postoperative neurological deficits. Footnote: *This study has been accepted for publication but has not yet been published. t-EMG, triggered electromyography.
Figure 3.
Hierarchical Summary Receiver Operating Characteristic (HSROC) curve. Footnote: The HSROC curve depicts a global summary of test performance.
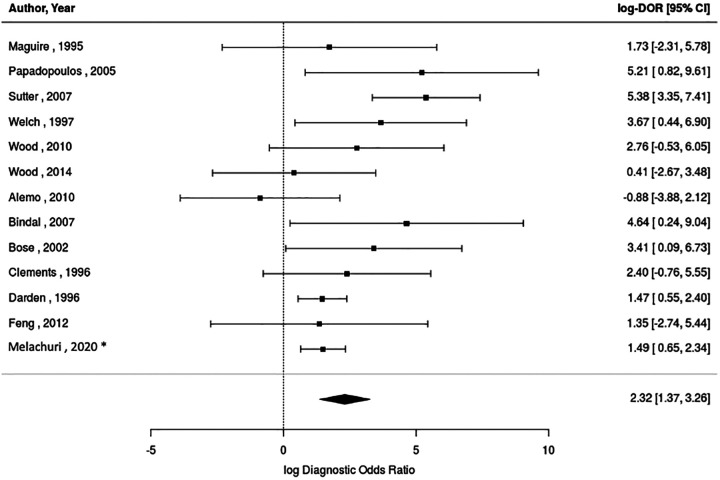
A pooled random effects model of the diagnostic odds ratios of lumbar pedicle screws stimulated below EMG alarm threshold for predicting neurological deficit was 10.14 (95% CI, 3.95-26.04, I2 = 5.78%). This indicates that patients with a new postoperative neurological deficit were 10 times more likely to have a low threshold pedicle screw response upon t-EMG testing compared to patients without a new postoperative neurological deficit. The significant pooled log-diagnostic odds ratios using the random effects model was 2.32 (95% CI, 1.37-3.26). Among the studies, the log-diagnostic odds ratios ranged from −0.88 to 5.38 (Figure 4).
Figure 4.
Forest plot of log-diagnostic odds ratios of pedicle screws stimulated at low t-EMG thresholds in predicting postoperative neurological deficits. Footnote: *This study has been accepted for publication but has not yet been published. t-EMG: triggered electromyography.
The positive and negative likelihood ratios depicted in the Fagan nomogram were 4.08 and 0.58, respectively (Figure 5). The pre-test probability was assumed to be 3.04%, the total incidence of postoperative neurological deficits in the study cohort. For patients with a pedicle screw stimulated below alarm threshold, the estimated post-test probability of developing a new postoperative neurological deficit increased to 11%. For patients without a pedicle screw stimulated below alarm threshold, the estimated post-test probability of developing a new postoperative neurological deficit decreased to 2%.
Figure 5.
Fagan nomogram of positive and negative t-EMG responses below alarm threshold. Footnote: PLR, positive likelihood ratio; NLR, negative likelihood ratio; t-EMG, triggered electromyography.
Subgroup Analysis
A subgroup analysis was conducted to compare the efficacy of utilizing 5-6 mA, 8 mA, and 10-11 mA as the current thresholds in determining postoperative deficit. The 4 studies that used 5-6 mA as their alarm EMG current thresholds had a DOR of 8.99 with a sensitivity of 50% (95% CI, 16%-84%) and a specificity of 88% (95% CI, 83%-91%). The 3 studies that used 8 mA as their current threshold had a DOR 8.37 with a sensitivity of 33% (95% CI, 18%-54%) and a specificity of 95% (95% CI, 58%-99%). Finally, the 2 studies that used 10-11 mA as their current threshold had a DOR of 20.19 with a sensitivity of 76% (95% CI, 23%-97%) and a specificity of 86% (95% CI, 32%-98%).
Discussion
Patients undergoing lumbar spine surgery who experienced new postoperative neurological deficits were 10 times more likely to have had a lumbar pedicle screw stimulated below alarm threshold upon t-EMG testing compared to patients without new postoperative neurological deficit. The Fagan nomogram demonstrates that the probability of postoperative neurological deficit increases from 3.04% to nearly 11% in patients with a pedicle screw stimulated below alarm threshold. To the authors’ knowledge, this is the largest and only systematic review to date that has assessed whether electrically activated lumbar pedicle screws that yield t-EMG responses below a specific threshold are associated with postoperative neurological deficit. This concept is critical to elucidate when discussing the therapeutic role of neurophysiological monitoring.
Previous works have shown that lumbar pedicle screws stimulated below certain thresholds may be associated with symptomatic breach. 26 Symptomatic pedicle screws often breach medially or inferiorly with proximity to the thecal sac or nerve roots. Although lateral and superior breaches are less likely to be symptomatic, the specific consequence of a breach is related to the individual anatomy and position of the screw. Symptomatic breach may result in radicular pain, numbness, weakness, or paresthesia secondary to nerve irritation or compression. 3
The stimulation threshold can indicate the proximity of the malpositioned screw to the nerve, so screws stimulated at low thresholds are more likely to result in deficit. The high diagnostic odds ratio and specificity of lumbar pedicle screws stimulated at low thresholds suggest that pedicle screws that are stimulated below the EMG alarm threshold must be carefully re-examined. Although an EMG threshold of 8 mA has a high sensitivity and specificity in determining medial breach of lumbar pedicle screw, 14 the optimal EMG alarm threshold for determining postoperative neurological deficit remains unknown. The varied EMG thresholds used by the studies in this analysis reduce the ability to pinpoint the diagnostic value of a precise threshold.
Analysis of 13 patient cohorts, each using an EMG alarm threshold between 5 and 11 mA, shows a high specificity and low sensitivity. The low sensitivity and positive predictive values for postoperative deficit indicate that a portion of patients with screws stimulated below alarm threshold do not experience postoperative neurological deficit. This may be due to several reasons. First, muscles of the lower limb are supplied by multiple nerve roots. Thus, injury to a specific nerve root may not manifest clinically as weakness or sensory loss. Second, poor bone quality in some patients may lower the current required to evoke a t-EMG response by creating a low impedance path between a well-placed pedicle screw and the nerve root. Additionally, t-EMG remains technique dependent. Specifically, if screw stimulation is conducted in a wet surgical field, excessive current may be shunted to the neural tissue, resulting in improper stimulation and lower reported thresholds. 27 Utilizing other forms of intraoperative neurophysiological monitoring (IONM) such as SSEPs and TcMEPs as an adjunct to t-EMG testing may reduce the clinical gaps associated with each technique. 28 However, a prospective clinical trial is needed to evaluate the efficacy of combining all 3 modalities to identify and reduce neurological deficits.
Furthermore, analysis shows a high specificity and negative predictive value for postoperative deficit, which indicates that most patients with screws stimulated above alarm threshold do not experience new postoperative neurological deficit. However, an important source of false negatives in t-EMG testing may be patients with preoperative neuropathy, including diabetic neuropathy and chronic radiculopathy. Holland et al has shown that the stimulus thresholds of chronically compressed nerve roots significantly exceed those of normal nerve roots and are often greater than 10 mA, due to axonotmesis. 29 In these patients, stimulation testing at sub-threshold currents of 5-8 mA will result in the reporting of false negative responses. Thus, in patients with peripheral neuropathy, instrumented pedicles may need to be tested at higher stimulus intensities using direct nerve root stimulation thresholds as a guide. 29
Many studies have outlined the proper technique for lumbar pedicle screw instrumentation.9-13,28 Voltage thresholds must be determined at each pedicle at both the bone and nerve root. After threshold determination at the site, the surgeon may probe the pedicle, tap the hole, and place the screw. It is important to ensure that the instruments are electrified at each stage of implantation. 30 However, there is a lack of standardized protocol in response to lumbar pedicle screws stimulated below the EMG alarm threshold.15,16
Guidelines for electrophysiological monitoring during lumbar fusion procedures were published in 2005 and updated in 2014.15,16 The authors found that although there is sufficient evidence that lumbar pedicle screws stimulated at low EMG thresholds may indicate breach, it remains unclear how this affects overall outcome. Furthermore, the guidelines state that there is no evidence to suggest that intraoperative t-EMG testing can improve outcomes, as no studies have shown that intraoperative maneuvers in response to t-EMG testing can prevent postoperative deficits. The results of this study cannot prove that intraoperative t-EMG testing can benefit patient outcomes, but they do establish an association between low-threshold screws and postoperative deficits. Thus, t-EMG may still provide value as an intraoperative adjunct in lumbar spine surgery for several reasons, even if potential deficits may not be prevented intraoperatively. First, alerting the surgeon of a higher postoperative deficit risk intraoperatively itself may allow for more targeted, aggressive therapy/rehabilitation following surgery. Second, even if current outcomes cannot be improved with early t-EMG warning of potential deficit, future research may discover efficacious therapeutic maneuvers in response to t-EMG alarm.
This study serves as preliminary analysis of electromyography’s potential to predict postoperative deficits. Although this meta-analysis is comprehensive in its quality assessment using the QUADAS-2, there are several limitations. It is important to acknowledge that a search bias may have existed due to the difficulty of finding every possible study assessing t-EMG use in lumbar spine surgery. Furthermore, a publication bias may exist due to the dependence of this investigation on currently published data, although the funnel plot (Supplemental Figure 2) provides no evidence of such bias. While there are many studies reporting EMG testing outcomes and breach outcomes, there are fewer primary studies reporting EMG testing outcomes and postoperative clinical outcomes. As such, additional limitations of the study include a) varied EMG alarm threshold currents (ranging from 5-11 mA) which reduces the ability to pinpoint the diagnostic value of a precise threshold current, b) lack of data on specific nerve roots directly stimulated in each patient, c) lack of details of screw repositioning upon intraoperative functional and structural assessment, d) lack of data regarding use of other intraoperative monitoring modalities (i.e. SSEPs and TcMEPS), e) lack of more standard documentation of specific postoperative deficits, and f) lack of documentation of preoperative clinical status. In particular, many studies do not report which specific screws were intraoperatively repositioned and thus, subgroup analysis of the postoperative implications of repositioned screws could not be conducted. Additionally, due to lack of information about preoperative neurological comorbidities such as diabetic neuropathy, we were unable to exclude these patients from the analysis, which may have introduced false negatives into the data.
Despite these limitations, t-EMG testing may provide intraoperative value during lumbar fusion in the context of predicting potential postoperative deficit. The findings serve as a prompt for future clinical trials to evaluate: 1) the optimal EMG alarm threshold for postoperative clinical significance, 2) the efficacy of combined SSEP, MEPs, and t-EMG monitoring in identifying neurological deficit, 3) whether intraoperative t-EMG monitoring improves overall outcomes, 4) the correlation between specific nerve root stimulation and deficits at those levels and 5) the efficacy of intraoperative maneuvers in response to t-EMG alarm.
Conclusion
Intraoperative triggered EMG monitoring may be clinically useful in the context of predicting postoperative neurological deficit. Electrically activated lumbar pedicle screws resulting in low t-EMG alarm thresholds are highly specific but weakly sensitive for new postoperative neurological deficits. Patients with new postoperative neurological deficits after lumbar spine surgery were 10 times more likely to have had a lumbar pedicle screw stimulated at a low EMG threshold.
Supplemental Material
Supplemental Material, sj-jpg-1-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal
Supplemental Material, sj-jpg-2-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal
Supplemental Material, sj-jpg-3-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal
Footnotes
Authors’ Note: All authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Rajiv P. Reddy, BS  https://orcid.org/0000-0001-8862-1458
https://orcid.org/0000-0001-8862-1458
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Guyer DW, Yuan HA, Werner FW, Frederickson BE, Murphy D. Biomechanical comparison of seven internal fixation devices for the lumbosacral junction. Spine (Phila Pa 1976). 1987;12(6):569–573. doi:10.1097/00007632-198707000-00012 [DOI] [PubMed] [Google Scholar]
- 2.Masferrer R, Gomez CH, Karahalios DG, Sonntag VK. Efficacy of pedicle screw fixation in the treatment of spinal instability and failed back surgery: a 5-year review. J Neurosurg. 1998;89(3):371–377. doi:10.3171/jns.1998.89.3.0371 [DOI] [PubMed] [Google Scholar]
- 3.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81(11):1519–1528. doi:10.2106/00004623-199911000-00003 [DOI] [PubMed] [Google Scholar]
- 4.Gautschi OP, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. 2011;31(4):E8. doi:10.3171/2011.7.FOCUS11168 [DOI] [PubMed] [Google Scholar]
- 5.Wood MJ, McMillen J. The surgical learning curve and accuracy of minimally invasive lumbar pedicle screw placement using CT based computer-assisted navigation plus continuous electromyography monitoring—a retrospective review of 627 screws in 150 patients. Int J Spine Surg. 2014;8:27. doi:10.14444/1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi WW, Green BA, Levi ADO. Computer-assisted fluoroscopic targeting system for pedicle screw insertion. Neurosurgery. 2000;47(4):872–878. doi:10.1097/00006123-200010000-00017 [DOI] [PubMed] [Google Scholar]
- 7.Fu TS, Chen LH, Wong CB, et al. Computer-assisted fluoroscopic navigation of pedicle screw insertion: an in vivo feasibility study. Acta Orthop Scand. 2004;75(6):730–735. doi:10.1080/00016470410004102 [DOI] [PubMed] [Google Scholar]
- 8.Youkilis AS, Quint DJ, McGillicuddy JE, Papadopoulos SM. Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48(4):771–778. discussion 778-779. doi:10.1227/00006123-200104000-00015 [DOI] [PubMed] [Google Scholar]
- 9.Calancie B, Lebwohl N, Madsen P, Klose KJ. Intraoperative evoked EMG monitoring in an animal model: a new technique for evaluating pedicle screw placement. Spine (Phila Pa 1976). 1992;17(10):1229–1235. doi:10.1097/00007632-199210000-00017 [DOI] [PubMed] [Google Scholar]
- 10.Bose B, Wierzbowski LR, Sestokas AK. Neurophysiologic monitoring of spinal nerve root function during instrumented posterior lumbar spine surgery. Spine (Phila Pa 1976). 2002;27(13):1444–1450. doi:10.1097/00007632-200207010-00014 [DOI] [PubMed] [Google Scholar]
- 11.Darden BV, Owen JH, Hatley MK, Kostuik J, Tooke SM. A comparison of impedance and electromyogram measurements in detecting the presence of pedicle wall breakthrough. Spine (Phila Pa 1976). 1998;23(2):256–262. doi:10.1097/00007632-199801150-00022 [DOI] [PubMed] [Google Scholar]
- 12.Glassman SD, Dimar JR, Puno RM, Johnson JR, Shields CB, Linden DR. A prospective analysis of intraoperative electromyographic monitoring of pedicle screw placement with computed tomographic scan confirmation. Spine (Phila Pa 1976). 1995;20(12):1375–1379. doi:10.1097/00007632-199506020-00008 [PubMed] [Google Scholar]
- 13.Welch WC, Rose RD, Balzer JR, Jacobs GB. Evaluation with evoked and spontaneous electromyography during lumbar instrumentation: a prospective study. J Neurosurg. 1997;87(3):397–402. doi:10.3171/jns.1997.87.3.0397 [DOI] [PubMed] [Google Scholar]
- 14.Raynor BL, Lenke LG, Bridwell KH, Taylor BA, Padberg AM. Correlation between low triggered electromyographic thresholds and lumbar pedicle screw malposition: analysis of 4857 screws. Spine (Phila Pa 1976). 2007;32(24):2673–2678. doi:10.1097/BRS.0b013e31815a524f [DOI] [PubMed] [Google Scholar]
- 15.Resnick DK, Choudhri TF, Dailey AT, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 15: electrophysiological monitoring and lumbar fusion. J Neurosurg Spine. 2005;2(6):725–732. doi:10.3171/spi.2005.2.6.0725 [DOI] [PubMed] [Google Scholar]
- 16.Sharan A, Groff MW, Dailey AT, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 15: electrophysiological monitoring and lumbar fusion. J Neurosurg Spine. 2014;21(1):102–105. doi:10.3171/2014.4.SPINE14324 [DOI] [PubMed] [Google Scholar]
- 17.Alemo S, Sayadipour A.Role of intraoperative neurophysiologic monitoring in lumbosacral spine fusion and instrumentation: a retrospective study. World Neurosurg. 2010;73(1):72–76. doi:10.1016/j.surneu.2009.04.024 [DOI] [PubMed] [Google Scholar]
- 18.Bindal RK, Ghosh S. Intraoperative electromyography monitoring in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 2007;6(2):126–132. doi:10.3171/spi.2007.6.2.126 [DOI] [PubMed] [Google Scholar]
- 19.Clements DH, Morledge DE, Martin WH, Betz RR. Evoked and spontaneous electromyography to evaluate lumbosacral pedicle screw placement. Spine (Phila Pa 1976). 1996;21(5):600–604. doi:10.1097/00007632-199603010-00013 [DOI] [PubMed] [Google Scholar]
- 20.Darden BV, Wood KE, Hatley MK, Owen JH, Kostuik J. Evaluation of pedicle screw insertion monitored by intraoperative evoked electromyography. J Spinal Disord. 1996;9(1):8–16. doi:10.1097/00002517-199602000-00002 [PubMed] [Google Scholar]
- 21.Feng L, Wei L, Fan Z, Tie L, Du XL, Chen AM. Minimally invasive transforaminal lumbar interbody fusion aided with computer-assisted spinal navigation system combined with electromyography monitoring. Chin Med J (Engl). 2012;125(22):3947–3951. doi:10.3760/cma.j.issn.0366-6999.2012.22.006 [PubMed] [Google Scholar]
- 22.Maguire J, Wallace S, Madiga R, Leppanen RE, Draper V. Evaluation of intrapedicular screw position using intraoperative evoked electromyography. Spine (Phila Pa 1976). 1995;20(9):1068–1074. doi:10.1097/00007632-199505000-00015 [DOI] [PubMed] [Google Scholar]
- 23.Papadopoulos EC, Girardi FP, Sama A, Sandhu HS, Cammisa FP. Accuracy of single-time, multilevel registration in image-guided spinal surgery. Spine J. 2005;5(3):263–267; discussion 268. doi:10.1016/j.spinee.2004.10.048 [DOI] [PubMed] [Google Scholar]
- 24.Sutter MA, Eggspuehler A, Grob D, Porchet F, Jeszenszky D, Dvorak J. Multimodal Intraoperative Monitoring (MIOM) during 409 lumbosacral surgical procedures in 409 patients. In: European Spine Journal; 2007. doi:10.1007/s00586-007-0432-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wood MJ, Mannion RJ. Improving accuracy and reducing radiation exposure in minimally invasive lumbar interbody fusion. J Neurosurg Spine. 2010;12(5):533–539. doi:10.3171/2009.11.SPINE09270 [DOI] [PubMed] [Google Scholar]
- 26.Mikula AL, Williams SK, Anderson PA. The use of intraoperative triggered electromyography to detect misplaced pedicle screws: a systematic review and meta-analysis. J Neurosurg Spine. 2016;24(4):624–638. doi:10.3171/2015.6.SPINE141323 [DOI] [PubMed] [Google Scholar]
- 27.West C.Practical aspects of monitoring spinal motor systems. In: Intraoperative Neurophysiological Monitoring. 2nd ed. Humana; 2005:223–224. [Google Scholar]
- 28.Wilent WB, Rhee JM, Harrop JS, et al. Therapeutic impact of traction release after C5 nerve root Motor Evoked Potential (MEP) alerts in cervical spine surgery. Clin Spine Surg. 2020;33(10):E442–E447. doi:10.1097/BSD.0000000000000969 [DOI] [PubMed] [Google Scholar]
- 29.Holland NR, Lukaczyk TA, Riley LH, Kostuik JP. Higher electrical stimulus intensities are required to activate chronically compressed nerve roots: implications for intraoperative electromyographic pedicle screw testing. Spine (Phila Pa 1976). 1998;23(2):224–227. doi:10.1097/00007632-199801150-00014 [DOI] [PubMed] [Google Scholar]
- 30.Rose RD, Welch WC, Balzer JR, Jacobs GB. Persistently electrified pedicle stimulation instruments in spinal instrumentation: technique and protocol development. Spine (Phila Pa 1976). 1997;22(3):334–343. doi:10.1097/00007632-199702010-00019 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-jpg-1-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal
Supplemental Material, sj-jpg-2-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal
Supplemental Material, sj-jpg-3-gsj-10.1177_21925682211018472 for Triggered Electromyography is a Useful Intraoperative Adjunct to Predict Postoperative Neurological Deficit Following Lumbar Pedicle Screw Instrumentation by Rajiv P. Reddy, Robert Chang, Dominic V. Coutinho, Justin W. Meinert, Katherine M. Anetakis, Donald J. Crammond, Jeffrey R. Balzer, Jeremy D. Shaw, Joon Y. Lee and Parthasarathy D. Thirumala in Global Spine Journal