Abstract
Study Design:
Multicenter retrospective study.
Objectives:
We aim to investigate features of cervical spondylotic myelopathy (CSM) associated with anterior cervical spondylolisthesis (ACS) during posterior decompression surgery.
Methods:
A total of 732 patients with CSM were enrolled, who underwent posterior decompression surgery between July 2011 and November 2015 at 17 institutions. The patients with ACS (group A), defined as an anterior slippage of ≥2 mm on plain radiographs, were compared with those without ACS (group non-A). Also, the characteristics of patients with ACS progression (group P), defined as postoperative worsening of ACS ≥2 mm or newly developed ACS, were investigated. Moreover, kyphosis was defined as C2-C7 angle in neutral position ≤−5°. The Japanese Orthopedic Association (JOA) scoring system was used for clinical evaluation.
Results:
Group A consisting of 62 patients (8.5%) had worse preoperative clinical status but comparable surgical outcomes to group non-A. Furthermore, ACS was associated with greater age, and the degree of slippage did not affect myelopathy grades. Seventeen patients (2.3%) were observed in group P, and preoperative ACS was a significant predisposing factor for the progression without clinical impact. Among the patients in group A, preoperative cervical kyphosis was a risk factor for lower JOA recovery rate.
Conclusions:
Although the presence of ACS increases the risk of postoperative progression, it is not a contraindication for posterior decompression. However, surgeons need to consider the indication of fusion surgery for the patients who have ACS accompanied by kyphosis because of the poor surgical outcomes.
Keywords: anterior cervical spondylolisthesis, kyphosis, cervical spondylotic myelopathy, posterior decompression surgery, laminoplasty, selective laminectomy
Introduction
Cervical spondylotic myelopathy (CSM) is essentially caused by age-related degeneration, which leads to spinal cord dysfunction and impairment. The pathology of CSM consists of spondylosis, protruding disc, facet arthritis, and hypertrophy of the ligamentum flavum.1,2 Because CSM is thought to be a progressive disease, patients with moderate or severe CSM frequently require surgical intervention. In addition, due to the global increase in the aging population, the need for surgical treatment is expected to increase over time. 1
Cervical posterior decompression surgeries without fixation, which include open-door laminoplasty, 3 double-door laminoplasty, 4 and selective laminectomy with muscle preservation, 5 are widely used for CSM treatment because of satisfactory surgical outcomes with less invasive technique. However, the ideal procedure to produce the best surgical outcomes is yet to be determined for specific pathological conditions such as anterior and posterior cervical spondylolisthesis,6-11 kyphotic cervical alignment, 12 and signal intensity change on magnetic resonance imaging (MRI). 12 With respect to anterior cervical spondylolisthesis (ACS) in previous studies, fewer clinical studies exist compared to those concerning the lumbar spine and the clinical efficacy of ACS on CSM is controversial.6-11 Several studies have shown that ACS significantly worsens preoperative myelopathy and surgical outcomes,6,11 whereas others have concluded that ACS does not affect CSM before and after laminoplasty.9,10 In addition, little has been reported on postoperative progression of cervical slippage after decompression surgery compared with those involving the lumbar spine.7,9
The reason for this controversy could be due to small sample size and nonuniform definitions of cervical spondylolisthesis in previous studies.6-11,13-18 Therefore, we conducted a multicenter retrospective study with 732 CSM patients who underwent posterior decompression surgeries to identify the impact of cervical spondylolisthesis on myelopathy; this has been the largest series reported to date. Cervical spondylolisthesis was defined as an anterior slippage of 2 mm or more on a neutral lateral radiograph, according to the previous reports.11,13,16 Moreover, we focused on the clinical impact of ACS associated with cervical kyphosis, which was reported to exacerbate myelopathy grade in a previous study. 12 The aim of this study was to investigate the features of preoperative ACS and any progression following posterior decompression surgery.
Materials and Methods
Patients
Seven hundred thirty-two patients were enrolled; all were diagnosed with CSM and underwent posterior decompression surgeries between July 2011 and November 2015 at one of 17 institutions with a minimum follow-up of 1 year. Patients were excluded if they were diagnosed with ossification of posterior longitudinal ligament, disc herniation, trauma, infection, tumor, renal failure requiring hemodialysis, collagen disease such as rheumatoid arthritis, or history of previous cervical surgery. Clinical data on each patient was collected retrospectively using patient charts and operative records. Institutional review board approval was granted by the Tokyo Dental College Ichikawa General Hospital Ethics Guideline (Approval Number: I-316R), and all study participants provided informed consent.
Surgical Procedures
Posterior decompression surgeries included open-door laminoplasty (n = 291), double-door laminoplasty (n = 221), and selective laminectomy (n = 220). Surgical technique of each procedure is described elsewhere.3-5 On postoperative day 1, patients were out of bed and standing. Use of and duration of cervical collar varied and was determined by surgeon preference.
Anterior Cervical Spondylolisthesis
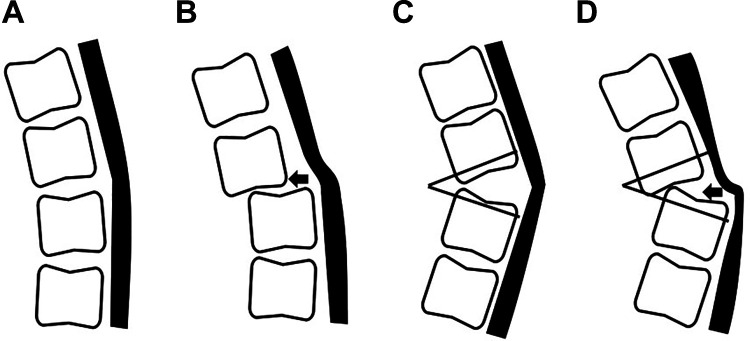
Flexion-extension lateral radiographs were taken at a 1.5 m film focal distance for all patients. Anterior slippage was measured by the distance from the vertical line from posteroinferior corner of cranial vertebral body to the vertical line from posterosuperior corner of caudal vertebral body on a cervical plain radiograph in the neutral position. ACS was defined as anterior slippage of ≥2 mm and patients with posterior cervical spondylolisthesis (PCS) were excluded from this study (Figure 1).14,16,18 If a patient had cervical vertebrae with anterior slippage at more than 2 levels, the level with the most distant anterolisthesis was used for analysis. The patients were divided into 2 groups based on degree of preoperative anterior slippage. Group A and group non-A included patients with preoperative ACS ≥2 mm and those with under 2 mm, respectively. Comparative studies of demographic, radiological, and clinical factors were performed between the groups.
Figure 1.
Definition of preoperative ACS and progression of ACS after surgery. (A) Preoperative ACS was defined as anterior slippage of ≥2 mm on performing a cervical plain radiograph in the neutral position. (B) Progression of ACS was defined as follows: postoperative worsening of ACS ≥2 mm on the level with preoperative ACS (B.1) or newly developed ACS ≥2 mm at the final follow-up (B.2). ACS, anterior cervical spondylolisthesis.
Progression of Anterior Cervical Spondylolisthesis
Progression of ACS following decompression surgery was defined as (1) postoperative worsening of ACS ≥2 mm in group A or (2) presence of newly developed ACS ≥2 mm at the final follow-up period in group non-A regarding the other previous studies (Figure 1).15,16 The enrolled patients were divided into group P and group non-P, which consisted of patients who showed progression of ACS after surgery and those without progression of ACS, respectively. We conducted a comparative analysis to identify demographic, radiological, and clinical features between the groups.
Cervical Kyphosis
Cervical kyphosis was defined as C2-C7 angle in neutral position ≤−5° according to a previous study. 19 Demographic, radiological, and clinical factors were analyzed considering the presence of cervical kyphosis.
Outcomes
Data including demographic factors, age, sex, height, body weight, body mass index (BMI), and follow-up period was collected. For radiological analysis, C2-C7 angles in neutral, flexion, and extension positions, range of motion (ROM), and C2-C7 sagittal vertical axis (SVA) were measured. The C2-C7 angle was measured by the angle between the horizontal line of C2 lower endplate and the horizontal line of C7 lower endplate according to Cobb’s method. 20 The ROM of the cervical spine was measured as the difference of C2-C7 angle between flexion and extension positions. 21 C2-C7 SVA was defined as a distance between a plumb line dropped from the center of C2 and the posterior superior aspect of C7. 22 Japanese Orthopedic Association (JOA) scoring system for CSM was estimated before surgery and at final follow-up. The recovery rate according to JOA scores was calculated by the Hirabayashi method et al. 23
Statistical Analysis
SPSS Statistics version 22.0 (IBM Corp) was used to perform statistical analyses. Student’s t test and χ2 test were performed for univariate analysis. If the expected value was lower than 5 in at least 20% of the cells, a Fisher’s exact test was used as an alternative to a χ2 test. To identify a predisposing factor of ACS, a univariate logistic regression analysis was used to determine the significance of various parameters. Age was classified into 7 groups for analysis: 21 to 30, 31 to 40, 41 to 50, 51 to 60, 61 to 70, 71 to 80, and 81 to 90 years. Meanwhile, other variables were considered as continuous. Factors with P < .25 in the univariate logistic regression analysis were then included in the multivariate logistic regression analysis. Differences were considered significant at P < .05.
Results
Prevalence and Level of Anterior Cervical Spondylolisthesis
A total of 491 male and 241 female subjects were enrolled; mean age was 67.4 ± 11.4 (range, 27-93) years. Sixty-two patients (8.5%) had preoperative ACS. C4/5 (n = 25, 40.3%) was the level most frequently involved, followed by C3/4 and C5/6 (n = 11, 17.7%), C7/T1 (n = 9, 14.5%), and C2/3 and C6/7 (n = 3, 4.8%; Supplementary Figure 1).
Demographic and Radiological Information Regarding Anterior Cervical Spondylolisthesis
Table 1 shows demographic data for groups A and non-A. The patients in group A showed increased age, shorter height, and lower body weight and BMI compared with group non-A. Radiologically, the patients in group A had significantly larger preoperative C2-C7 SVA than those in group non-A.
Table 1.
Demographic and radiological factors regarding ACS using univariate analysis.
| Variables | Group A, n (%) or mean ± SD | Group non-A, n (%) or mean ± SD | P value |
|---|---|---|---|
| Number of patients | 62 (8.5) | 670 (91.5) | |
| Age (years) | 73.1 ± 10.1 | 66.8 ± 11.4 | <.01** |
| Sex | .31 | ||
| Male | 38 (61.3) | 453 (67.6) | |
| Female | 24 (38.7) | 217 (32.4) | |
| Height (cm) | 156.0 ± 9.2 | 160.0 ± 9.9 | <.01** |
| Body weight (kg) | 55.8 ± 9.7 | 61.2 ± 12.3 | <.01** |
| BMI (kg/m2) | 22.8 ± 2.8 | 23.8 ± 3.6 | .045* |
| Follow-up period (months) | 23.4 ± 9.0 | 22.2 ± 8.3 | .27 |
| C2-C7 angle (°) | |||
| Neutral | 12.2 ± 14.3 | 12.9 ± 13.2 | .70 |
| Flexion | −9.4 ± 15.1 | −9.9 ± 12.4 | .82 |
| Extension | 23.1 ± 14.7 | 24.4 ± 13.4 | .48 |
| ROM (°) | 33.5 ± 13.4 | 34.9 ± 13.4 | .54 |
| C2-C7 SVA (mm) | 27.2 ± 14.5 | 22.8 ± 13.9 | .02* |
Abbreviations: ACS, anterior cervical spondylolisthesis; Group A, patients with preoperative ACS; Group non-A, patients without ACS; BMI, body mass index; ROM, range of motion; C2–C7 SVA, C2–C7 sagittal vertical axis. * indicates P <0.05, ** indicates P <0.01.
Factors Affecting Preoperative Cervical Spondylolisthesis
To identify factors associated with the preoperative ACS, univariate and multivariate logistic regression analyses were performed. Univariate logistic regression analysis showed that increased age, decreased height, lower BMI, and larger C2-C7 SVA were significantly associated with preoperative ACS (Table 2). Among the factors, age was the most significant predisposing factor for preoperative ACS by multivariate logistic regression analysis (Table 2).
Table 2.
Univariate and multivariate logistic regression analyses of demographic and radiological characteristics for anterior cervical spondylolisthesis.
| Univariate logistic regression analysis | Multivariate logistic regression analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age | 1.76 | 1.34-2.32 | <.001 | 1.75 | 1.32–2.32 | <.001 |
| Sex | .26 | |||||
| Height | 0.96 | 0.94-0.99 | .002 | .26 | ||
| Body weight | 0.96 | 0.94-0.98 | .001 | .08 | ||
| BMI | 0.92 | 0.85-0.998 | .044 | .19 | ||
| C2-C7 angle | ||||||
| Neutral | .70 | |||||
| Flexion | .59 | |||||
| Extension | .45 | |||||
| ROM | .45 | |||||
| C2-C7 SVA | 1.02 | 1.003-1.04 | .022 | .21 | ||
Abbreviations: OR, odds ratio; CI, confidence interval; BMI, body mass index; ROM, range of motion; C2–C7 SVA, C2–C7 sagittal vertical axis.
Clinical Impact of Preoperative Anterior Cervical Spondylolisthesis on Myelopathy
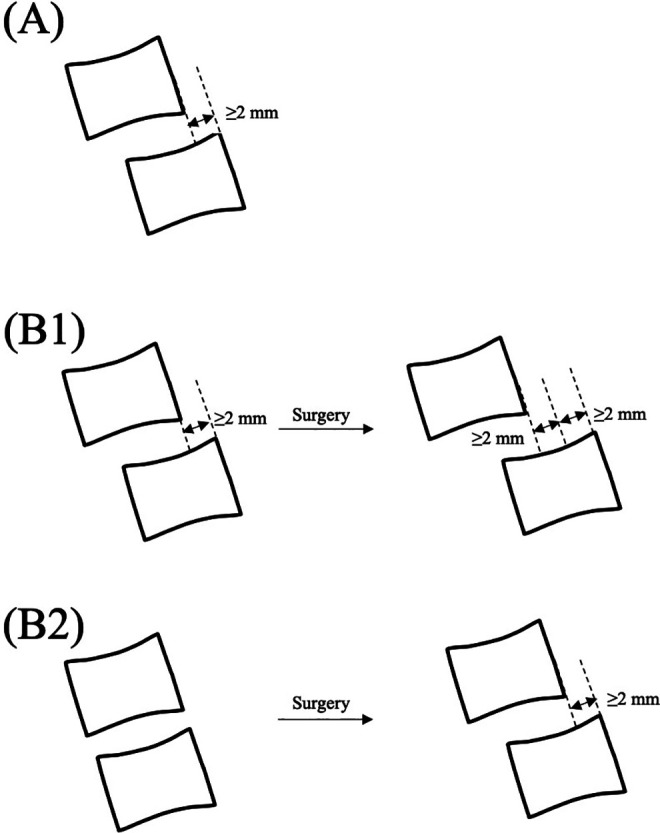
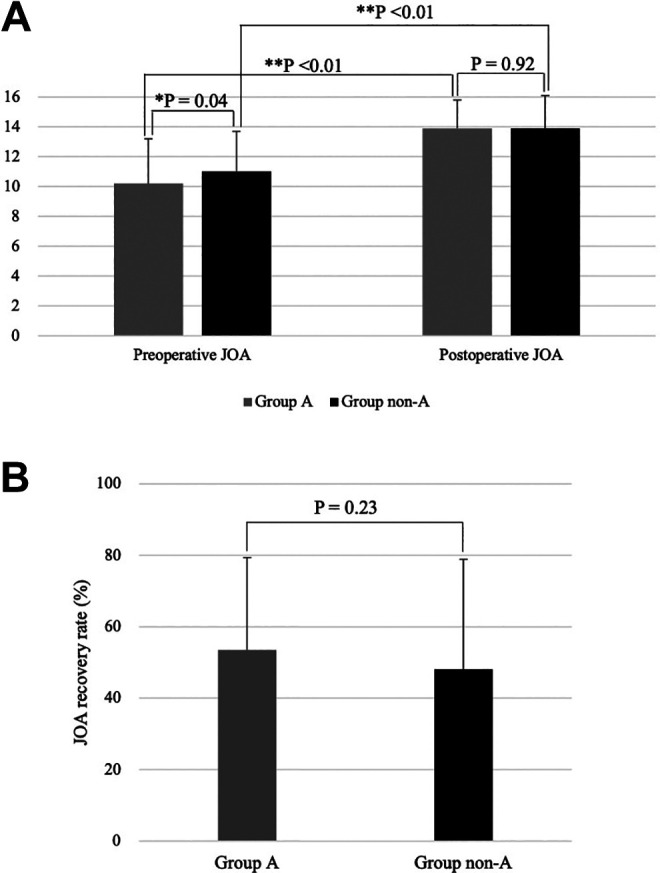
Preoperative JOA score was significantly lower in group A than in group non-A (10.2 ± 3.0 and 11.0 ± 2.7, P = .04; Figure 2). In contrast, we did not see significant differences in postoperative JOA scores or JOA recovery rates between group A and group non-A (13.9 ± 2.2 and 13.9 ± 1.9, P = .92; 53.5 ± 30.8% and 48.1 ± 25.9%, P = .23, respectively; Figure 2). The correlation analysis between the degree of anterior slippage ≥2 mm and clinical factors such as pre- and postoperative JOA score and JOA recovery rate did not show statistically significant associations among the groups (Figure 3).
Figure 2.
(A) Pre- and postoperative JOA score and (B) JOA recovery rate of patients who underwent cervical posterior decompression surgery. Group A, patients with preoperative ACS; group non-A, patients without ACS. JOA, Japanese Orthopedics Association; ACS, anterior cervical spondylolisthesis. *Indicates P < .05, **indicates P < .01.
Figure 3.
Correlation analysis between ACS and clinical factors. (A) Correlation analysis between ACS and preoperative JOA (r = 0.05, P = .73). (B) Correlation analysis between ACS and postoperative JOA (r = 0.02, P = .91). (C) Correlation analysis between ACS and JOA recovery rate (r = 0.01, P = .96). ACS, anterior cervical spondylolisthesis; JOA, Japanese Orthopaedics Association.
Clinical Impact of Preoperative Anterior Cervical Spondylolisthesis Associated With Cervical Kyphosis on Myelopathy
Among the group A patients, those with cervical kyphosis showed a significantly lower JOA recovery rate compared with those without cervical kyphosis (36.4 ± 23.5% and 56.3 ± 35.1%; P = .043; Figure 4). Though average C2-C7 angles in neutral, flexion, and extension positions were significantly different, other demographic and radiological factors were comparable between the groups (Table 3).
Figure 4.
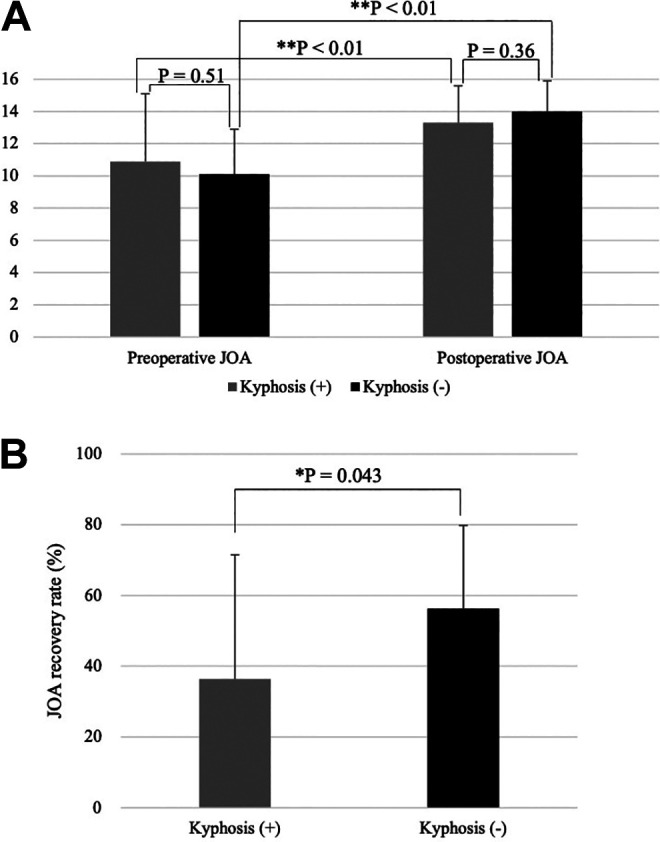
(A) Pre- and postoperative JOA score and (B) JOA recovery rate in patients with anterior cervical spondylolisthesis associated with presence of kyphosis. JOA, Japanese Orthopedics Association. *Indicates P < .05 and **indicates P < .01.
Table 3.
Demographic and radiological factors regarding cervical kyphosis in the patients who have anterior cervical spondylolisthesis using univariate analysis.
| Variables | Kyphosis (+), n (%) or mean ± SD | Kyphosis (−), n (%) or mean ± SD | P value |
|---|---|---|---|
| Number of patients | 8 (12.9) | 54 (87.1) | |
| Age (years) | 68.5 ± 17.0 | 73.7 ± 8.7 | .42 |
| Sex | .48 | ||
| Male | 4 (50.0) | 34 (68.2) | |
| Female | 4 (50.0) | 20 (31.8) | |
| Height (cm) | 154.7 ± 9.3 | 156.2 ± 9.2 | .67 |
| Body weight (kg) | 56.0 ± 10.0 | 55.8 ± 9.7 | .94 |
| BMI (kg/m2) | 23.3 ± 2.8 | 22.7 ± 2.8 | .83 |
| Follow-up period (months) | 20.8 ± 4.9 | 23.8 ± 9.3 | .53 |
| C2-C7 angle (°) | |||
| Neutral | −8.7 ± 2.9 | 15.3 ± 12.6 | <.01** |
| Flexion | −26.5 ± 8.4 | −6.8 ± 14.1 | <.01** |
| Extension | 5.8 ± 10.0 | 25.8 ± 13.4 | <.01** |
| ROM (°) | 32.3 ± 16.5 | 33.7 ± 14.7 | .81 |
| C2-C7 SVA (mm) | 31.3 ± 23.0 | 26.5 ± 12.9 | .59 |
Abbreviations: BMI, body mass index; ROM, range of motion; C2–C7 SVA, C2–C7 sagittal vertical axis. ** indicates P <0.01.
Prevalence and Characteristics of Postoperative Progression of Anterior Cervical Spondylolisthesis
Postoperative progression (newly developed or worsening) of ACS was observed with a frequency of 2.3% (17/732) among the subjects. The distribution of levels was as follows: C4/5 (n = 10, 58.8%) followed by C3/4 (n = 4, 23.5%) and C2/3 (n = 3, 17.6%; Supplementary Figure 2). Among group P and the group non-P, the patients who had preoperative ACS were observed to be 23.5% and 8.1%, respectively. The patients who had preoperative ACS showed a significantly higher frequency of the progression of ACS after surgery (P = .048) by Fisher’s exact test (Table 4).
Table 4.
Demographic and radiological factors regarding progression of ACS using univariate analysis.
| Variables | Group P, n (%) or mean ± SD | Group non-P, n (%) or mean ± SD | P value |
|---|---|---|---|
| Number of patients | 17 (2.3) | 715 (97.7) | |
| Age (years) | 70.3 ± 9.3 | 67.3 ± 10.5 | .29 |
| Sex | .83 | ||
| Male | 11 (64.7) | 480 (67.1) | |
| Female | 6 (35.3) | 235 (32.9) | |
| Height (cm) | 155 ± 11.1 | 160 ± 9.8 | .049* |
| Body weight (kg) | 56.9 ± 11.4 | 60.8 ± 12.2 | .19 |
| BMI (kg/m2) | 23.2 ± 3.5 | 23.7 ± 3.5 | .63 |
| Follow-up period (months) | 25.6 ± 8.4 | 22.2 ± 8.4 | .10 |
| Presence of preoperative ACS | 4 (23.5) | 58 (8.1) | .048* |
| C2-C7 angle (°) | |||
| Neutral | 6.3 ± 9.3 | 13.0 ± 13.4 | .04* |
| Flexion | −15.1 ± 10.5 | −10.1 ± 12.3 | .11 |
| Extension | 17.6 ± 10.5 | 24.5 ± 13.5 | .04* |
| ROM (°) | 32.7 ± 10.6 | 34.8 ± 13.5 | .54 |
| C2-C7 SVA (mm) | 26.9 ± 10.7 | 23.1 ± 14.1 | .26 |
Abbreviations: ACS, anterior cervical spondylolisthesis; Group P, patients with postoperative progression of ACS; Group non-P, patients without postoperative progression of ACS; BMI, body mass index; ROM, range of motion; C2–C7 SVA, C2–C7 sagittal vertical axis. * indicates P <0.05.
Additionally, shorter height and smaller C2-C7 angle in neutral and extension positions were associated with progression of ACS (Table 4). The average preoperative JOA scores, postoperative JOA scores, and JOA recovery rate in group P and in group non-P were 10.6 ± 2.2 and 10.9 ± 2.7 (P = .66), 14.0 ± 1.8 and 13.9 ± 2.2 (P = .89), and 50.4 ± 25.4% and 48.8 ± 30.6% (P = .85), respectively (Figure 5).
Figure 5.
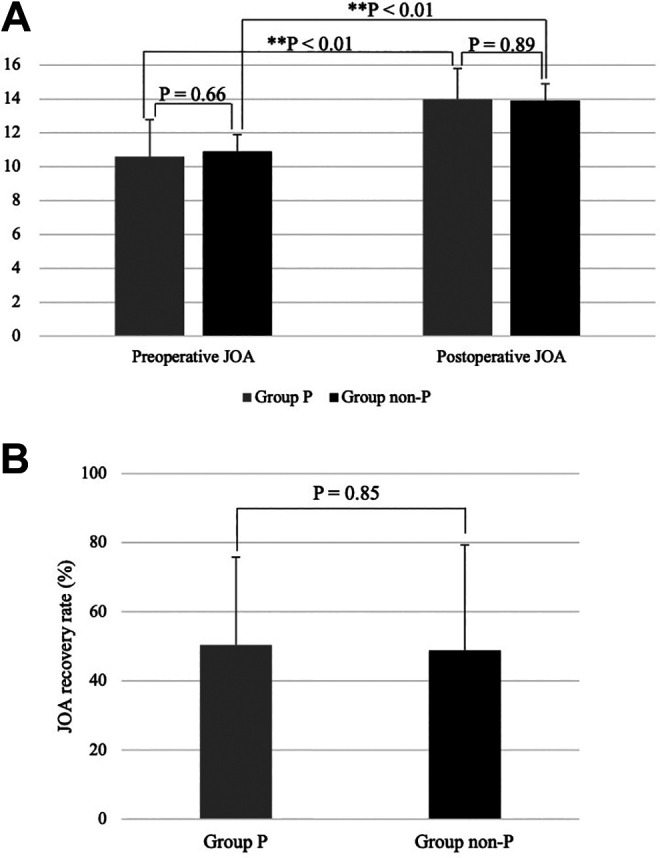
(A) Pre- and postoperative JOA score and (B) JOA recovery rate in patients who developed postoperative progression of ACS after cervical posterior decompression surgery. Group P, patients with postoperative progression of ACS; Group non-P, patients without postoperative progression of ACS; JOA, Japanese Orthopedics Association; ACS, anterior cervical spondylolisthesis. **Indicates P < .01.
Discussion
The current multicenter retrospective study demonstrated that the CSM patients who had ACS ≥2 mm on plain radiograph were significantly related to greater age by multivariate regression analysis. Although preoperative neurological status was worse, comparable surgical outcomes were achieved in patients with preoperative ACS after posterior decompression surgery. Nevertheless, ACS associated with cervical kyphosis was a significant risk factor for lower JOA recovery rate. Although patients with ACS demonstrated significantly higher incidence of postoperative progression of anterior slippage, the presence of preoperative ACS and progression of ACS did not worsen surgical outcomes.
The clinical impact of cervical spondylolisthesis on CSM is contentious and the controversy may be attributed to nonuniform definitions of cervical spondylolisthesis in previous studies; the minimum degree (usually 0-3 mm) and direction of slippage (anterior, posterior, or both anterior and posterior directions) and cervical position (neutral or flexion-extension positions) for imaging varied.6-11,14-18 We defined the minimum degree of cervical spondylolisthesis as 2 mm with only anterior direction on neutral lateral radiograph in this study, referencing other reports which demonstrated that a less severe spondylolisthesis (ie, a 1- or 2-mm slip) may frequently cause few or no symptoms13,16 and different pathology between anterior and posterior spondylolistheses. 11 Though the detailed data is shown later in the discussion, patients with cervical spondylolisthesis defined as anterior slippage ≥2 mm on neutral lateral radiograph significantly affected preoperative degree of myelopathy and incidence of progression of slippage after posterior decompression surgery. These results supported that our definition of cervical spondylolisthesis is clinically appropriate to analyze the effect of spondylolisthesis on myelopathy severity.
Our multivariate logistic regression analyses identified that increased age was a significant predisposing factor for preoperative ACS. This result was in accordance with previous studies which speculated that changes of spinal elements due to age, such as facet joints and discs triggered cervical spondylolisthesis.6,13 To the best of our knowledge, only 2 previous studies have demonstrated that older patients are more likely to have cervical spondylolisthesis than younger patients.8,10 However, these 2 previous studies defined cervical spondylolisthesis as a slippage consisting of both anterior and posterior directions.8,10 This may be problematic because several studies demonstrated different pathology between ACS and PCS.6,7,11 Therefore, our finding is clinically important because this is the first study to demonstrate the correlation between occurrence of cervical spondylolisthesis with only anterior direction and aging among the patients with CSM.
We demonstrated that the CSM patients with ACS had significantly worse preoperative clinical status than those without ACS, but that the distance of ACS did not correlate with myelopathy grades. Kawasaki et al 11 ascertained that although CSM patients with ACS had a significantly wider cervical spinal canal than those with PCS, the ACS had a greater impact on severity of CSM. The results of their study are consistent with that of our study in terms of finding a greater clinical impact of ACS on myelopathy. On the contrary, Sakai et al 7 reported that average preoperative JOA score of patients with ACS are comparable to those without ACS. We can speculate on 2 factors influencing the different impacts of ACS on the preoperative myelopathy between the studies. First, our study included a larger number of patients (N = 732) than in the previous study (N = 132). The greater power of the larger sample size in our study may provide a more reliable analysis. Second, the average age of patients with ACS in the current study (73.1 ± 10.1 years) was greater than that in the previous study (66.3 ± 8.7 years). Several studies have shown that older symptomatic patients have significantly worse myelopathy grades than younger patients, and the different age distribution between the 2 studies may have affected the preoperative clinical status of the patients.24,25 We do not know the reason why the correlation was not observed between distance of ACS and myelopathy grades, but speculate that factors other than spondylolisthesis may affect the degree of myelopathy among the patients.
The current study showed that the CSM patients with ACS had comparable surgical outcomes to those without ACS after posterior decompression surgery. To our knowledge, 2 other studies analyzed the impact of preoperative ACS on myelopathic severity after posterior decompression surgery.6,7 Sakai et al 7 demonstrated that patients with ACS showed significantly better surgical outcomes than those with PCS following laminoplasty. Our satisfactory surgical outcomes of the patients with ACS following posterior decompression are comparable with their study. On the other hand, Oichi et al 6 reported that ACS was a significant risk factor for poor surgical outcomes owing to residual anterior spinal cord compression in flexion position following laminoplasty. We can speculate on factors explaining the different results between the studies. First, our study included a larger sample size (N = 732) than the study by Oichi et al 6 (N = 125). Second, although we performed a comparative clinical analysis between symptomatic patients with ACS and those without ACS in this study, the previous study did not conduct this kind of comparative study, and consequently, potential confounders which might affect the relationship between ACS and myelopathy were not evaluated. These differences between the studies may support a reliability of our results, indicating that posterior decompression surgery is a favorable surgical method for CSM patients with ACS.
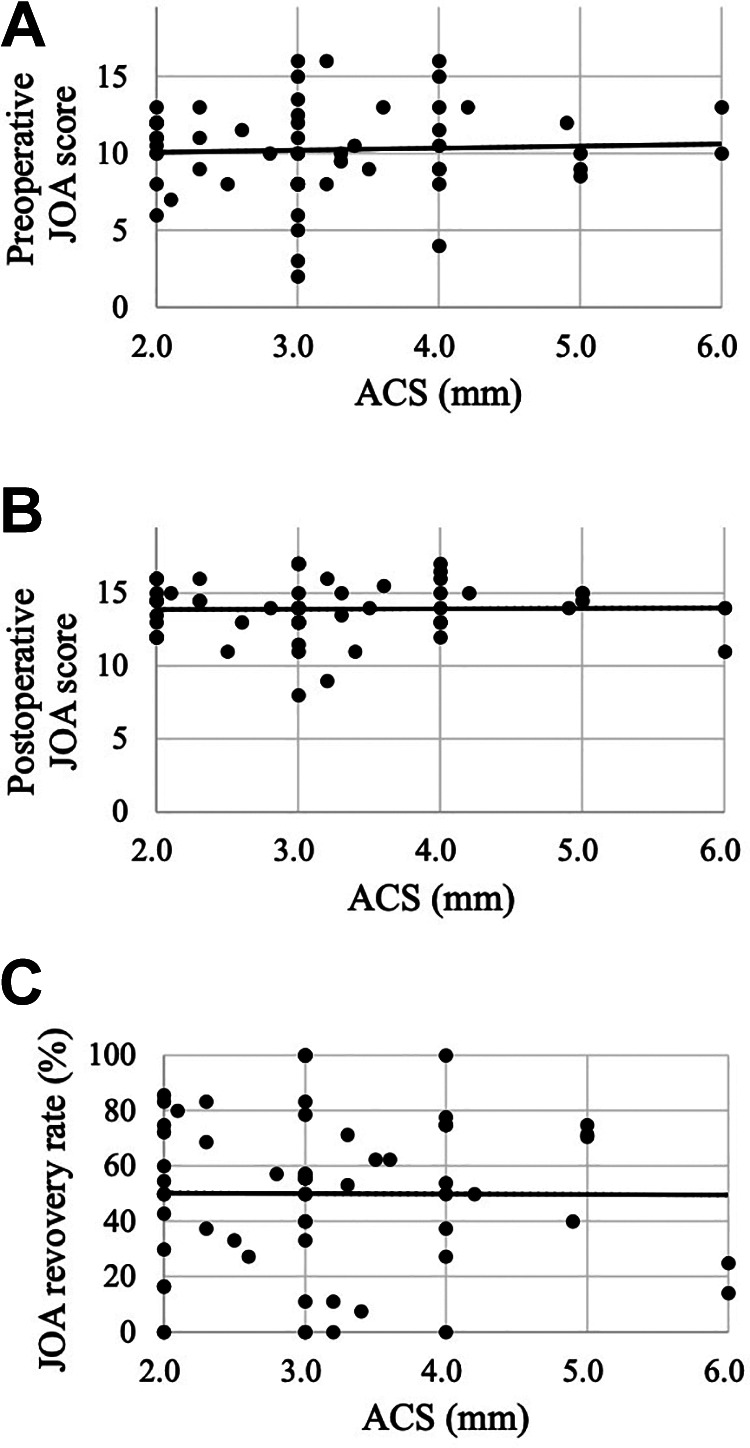
Our study showed that only ACS or kyphosis did not impact surgical outcomes following posterior decompression surgery, but the presence of both ACS and cervical kyphosis significantly decreased the JOA recovery rate. We speculated the mechanism as follows. Among the patients with ACS, anterior spinal cord compression is likely to persist in flexion position compared with those without ACS (Figure 6A and B). 6 However, posterior decompression surgery provided a sufficient effect overwhelming the residual anterior spinal cord compression in the patients with ACS, and consequently, satisfactory surgical outcomes were obtained. Similarly, preoperative kyphosis is reported as a predisposing factor of residual anterior spinal cord compression after posterior decompression surgery, which may worsen the surgical outcomes (Figure 6C). 12 Nevertheless, our satisfactory surgical outcomes for the patients with kyphosis (Supplementary Figure 3) implied that the effect of decompression surgery overcomes residual anterior compression on the spinal cord among the patients with kyphosis as well as those with ACS, whereas a combination of ACS and cervical kyphosis may result in the largest residual anterior spinal cord compression in the patients considering the existence of ACS and kyphosis (Figure 6D). Thus, the effect of cervical posterior decompression surgery is insufficient and, subsequently, the surgical outcomes are significantly worse in the patients who have both ACS and cervical kyphosis. Therefore, the instrumentation surgery which can correct ACS and cervical kyphosis may be a surgical option for the patients with ACS and kyphosis.
Figure 6.
Spinal cord decompression in patients with flexion position after posterior surgery considering ACS and kyphosis. (A) Normal alignment without ACS, (B) ACS with normal alignment, (C) kyphosis without ACS, and (D) ACS associated with kyphosis. The patients who have ACS and kyphosis are more likely to have persistent anterior spinal cord compression due to insufficient indirect decompression. ACS, anterior cervical spondylolisthesis.
We presume that preoperative ACS associated with kyphosis causes the most severe residual anterior compression of spinal cord during flexion of cervical spine, and it negatively affects the outcomes of posterior decompression surgery referencing a speculation of another study (Figure 6). 6 Therefore, we should consider the instrumentation surgery to correct spondylolisthesis and alignment other than posterior decompression for patients who have ACS accompanied with kyphosis.
We identified a significantly higher incidence of progression of anterior slippage among patients with ACS than among the patients without ACS. Also, shorter height and smaller C2-C7 angle in neutral and extension positions were significantly associated with progression of ACS. However, progression did not worsen surgical outcomes following posterior decompression surgery. This result was unexpected because all previous studies demonstrated that preoperative ACS did not significantly correlate with progression of slippage after laminoplasty.6,7 The authors in the previous study speculated that the result was caused by stabilization of cervical soft tissue, which were associated with contracture and unexpected bony fusion in facet joints following laminoplasty. 6 We consider that the discordant results between the studies can be explained by recent advances of posterior surgical procedure in our hospitals. For example, our study included 220 cases of selective laminectomy, which is reported to minimize a cervical contracture by limiting the number of decompressions and reducing exposure. 5 With regard to previous studies which indicated negative correlations between muscle strength and height 26 and between muscle volume and spinal malalignment, 27 we speculate that the muscle weakness associated with shorter height and cervical hypolordosis can result in difficulty maintaining a sagittal balance, making subsequent slippage more likely to occur postoperatively.
Some limitations must be considered when interpreting the present results. First, this is a retrospective study and thus sample and control biases are difficult to control. Second, this is a multicenter study and different surgeons have different indications for surgery, skills, and postoperative treatment which might influence surgical outcomes. Third, symptomatic patients who have severe ACS are more likely to undergo anterior or posterior decompression with instrumentation surgery; however, such cases were excluded in the current study. To address these limitations, further prospective investigation is needed with a longer follow-up period.
In conclusion, this multicenter retrospective study included the largest number of symptomatic patients to analyze the clinical effect of ACS on myelopathy. We showed that preoperative ACS is significantly associated with increased age among the CSM patients by multivariate logistic regression analysis. The definition of ACS with regard to clinical significance on myelopathy severity was controversial in previous studies. However, we have shown that symptomatic patients with ACS ≥2 mm on a plain radiograph have significantly lower preoperative JOA score and favorable surgical outcomes after posterior decompression surgery. Although the degree of ACS did not correlate with the severity of CSM, preoperative ACS associated with kyphosis significantly decreased JOA recovery rate, possibly due to persistent anterior spinal cord compression. The patients with ACS demonstrated a significantly higher incidence of postoperative progression of anterior slippage, but posterior decompression surgery provides favorable surgical outcomes for the patients regardless of this progression of slippage. Taken together, posterior decompression surgery can be a beneficial intervention for CSM patients with ACS with satisfactory outcomes, but addition of instrumentation surgery should be considered for the patients who have ACS associated with kyphosis.
Supplemental Material
Supplemental Material, 20200902_Supplementary_Figure for Clinical Effects of Anterior Cervical Spondylolisthesis on Cervical Spondylotic Myelopathy After Posterior Decompression Surgery: A Retrospective Multicenter Study of 732 Cases by Ken Ninomiya, Junichi Yamane, Ryoma Aoyama, Satoshi Suzuki, Yuta Shiono, Yuichiro Takahashi, Nobuyuki Fujita, Eijirou Okada, Osahiko Tsuji, Mitsuru Yagi, Kota Watanabe, Takahito Iga, Masaya Nakamura, Morio Matsumoto, Ken Ishii and Narihito Nagoshi in Global Spine Journal
Acknowledgments
We would like to thank Keiichi Sakuma for data collection.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ken Ninomiya, MD, PhD  https://orcid.org/0000-0001-6891-865X
https://orcid.org/0000-0001-6891-865X
Ryoma Aoyama, MD, PhD  https://orcid.org/0000-0003-1607-359X
https://orcid.org/0000-0003-1607-359X
Narihito Nagoshi, MD, PhD  https://orcid.org/0000-0001-8267-5789
https://orcid.org/0000-0001-8267-5789
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Tetreault L, Goldstein CL, Arnold P, et al. Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery. 2015;77(suppl 4):S51-S67. [DOI] [PubMed] [Google Scholar]
- 2.Bakhsheshian J, Mehta VA, Liu JC. Current diagnosis and management of cervical spondylotic myelopathy. Global Spine J. 2017;7:572-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988;13:870–876. [DOI] [PubMed] [Google Scholar]
- 4.Kurokawa T, Tsuyama N, Tanaka H. Double-door laminoplasty through longitudinal splitting of the spinous processes for cervical myelopathy. Rinsho Seikei Geka. 1984;19:483–490. [Google Scholar]
- 5.Shiraishi T, Kato M, Yato Y, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine (Phila Pa 1976). 2012;37:E286–E296. [DOI] [PubMed] [Google Scholar]
- 6.Oichi T, Oshima Y, Taniguchi Y, et al. Cervical anterolisthesis: a predictor of poor neurological outcomes in cervical spondylotic myelopathy patients after cervical laminoplasty. Spine (Phila Pa 1976). 2016;41:E467–E473. [DOI] [PubMed] [Google Scholar]
- 7.Sakai Y, Matsuyama Y, Inoue K, Naoki I. Postoperative instability after laminoplasty for cervical myelopathy with spondylolisthesis. J Spinal Disord Tech. 2005;18:1–5. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki A, Tamai K, Terai H, et al. Clinical outcome of cervical laminoplasty and postoperative radiological change for cervical myelopathy with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2016;41:1808–1812. [DOI] [PubMed] [Google Scholar]
- 9.Shigematsu H, Ueda Y, Takeshima T, et al. Degenerative spondylolisthesis does not influence surgical results of laminoplasty in elderly cervical spondylotic myelopathy patients. Eur Spine J. 2010;19:720–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawakami M, Tamaki T, Ando M, Yamada H, Matsumoto T, Yoshida M. Preoperative instability does not influence the clinical outcome in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disord Tech. 2002;15:277–283. [DOI] [PubMed] [Google Scholar]
- 11.Kawasaki M, Tani T, Ushida T, Ishida K. Anterolisthesis and retrolisthesis of the cervical spine in cervical spondylotic myelopathy in the elderly. J Orthop Sci. 2007;12:207–213. [DOI] [PubMed] [Google Scholar]
- 12.Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003;28:1258-1262. [DOI] [PubMed] [Google Scholar]
- 13.Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop. 2011;35:869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HC, Jun HS, Kim JH, Chang IB, Song JH, Oh JK. The effect of the pedicle-facet angle on degenerative cervical spondylolisthesis. J Korean Neurosurg Soc. 2015;58:341–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park MS, Moon SH, Lee HM, et al. The natural history of degenerative spondylolisthesis of the cervical spine with 2- to 7-year follow-up. Spine (Phila Pa 1976). 2013;38:E205–E210. [DOI] [PubMed] [Google Scholar]
- 16.Park MS, Moon SH, Oh JK, Lee HW, Riew KD. Natural history of cervical degenerative spondylolisthesis. Spine (Phila Pa 1976). 2019;44:E7–E12. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki A, Daubs MD, Inoue H, et al. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine (Phila Pa 1976). 2013;38:E1115–E1120. [DOI] [PubMed] [Google Scholar]
- 18.Jun HS, Kim JH, Ahn JH, et al. T1 slope and degenerative cervical spondylolisthesis. Spine (Phila Pa 1976). 2015;40:E220–E226. [DOI] [PubMed] [Google Scholar]
- 19.Sodeyama T, Goto S, Mochizuki M, Takahashi J, Moriya H. Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord. Spine (Phila Pa 1976).1999;24:1527–1532. [DOI] [PubMed] [Google Scholar]
- 20.Cobb JR. Outline for the study of scoliosis. Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 21.Liu S, Lafage R, Smith JS, et al. Impact of dynamic alignment, motion, and center of rotation on myelopathy grade and regional disability in cervical spondylotic myelopathy. J Neurosurg Spine. 2015;23:690–700. [DOI] [PubMed] [Google Scholar]
- 22.Van Royen BJ, Toussaint HM, Kingma I, et al. Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Eur Spine J. 1998;7:408–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976). 1981;6:354–364. [DOI] [PubMed] [Google Scholar]
- 24.Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T. Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery. 2003;52:122–126. [DOI] [PubMed] [Google Scholar]
- 25.Nakashima H, Tetreault LA, Nagoshi N, et al. Does age affect surgical outcomes in patients with degenerative cervical myelopathy? Results from the prospective multicenter AOSpine International study on 479 patients. J Neurol Neurosurg Psychiatry. 2016;87:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harbo T, Brincks J, Andersen H. Maximal isokinetic and isometric muscle strength of major muscle groups related to age, body mass, height, and sex in 178 healthy subjects. Eur J Appl Physiol. 2012;112:267–275. [DOI] [PubMed] [Google Scholar]
- 27.Hiyama A, Katoh H, Sakai D, et al. Correlation analysis of sagittal alignment and skeletal muscle mass in patients with spinal degenerative disease. Sci Rep. 2018;8:15492. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, 20200902_Supplementary_Figure for Clinical Effects of Anterior Cervical Spondylolisthesis on Cervical Spondylotic Myelopathy After Posterior Decompression Surgery: A Retrospective Multicenter Study of 732 Cases by Ken Ninomiya, Junichi Yamane, Ryoma Aoyama, Satoshi Suzuki, Yuta Shiono, Yuichiro Takahashi, Nobuyuki Fujita, Eijirou Okada, Osahiko Tsuji, Mitsuru Yagi, Kota Watanabe, Takahito Iga, Masaya Nakamura, Morio Matsumoto, Ken Ishii and Narihito Nagoshi in Global Spine Journal