Abstract
OBJECTIVE
To examine changes in diabetes-related preventable hospitalization costs and to determine the contribution of each underlying factor to these changes.
RESEARCH DESIGN AND METHODS
We used data from the 2001–2014 U.S. National (Nationwide) Inpatient Sample (NIS) for adults (≥18 years old) to estimate the trends in hospitalization costs (2014 USD) in total and by condition (short-term complications, long-term complications, uncontrolled diabetes, and lower-extremity amputation). Using regression and growth models, we estimated the relative contribution of following underlying factors: total number of hospitalizations, rate of hospitalization, the number of people with diabetes, mean cost per admission, length of stay, and cost per day.
RESULTS
During 2001–2014, the estimated total cost of diabetes-related preventable hospitalizations increased annually by 1.6% (92.9 million USD; P < 0.001). Of this 1.6% increase, 75% (1.2%) was due to the increase in the number of hospitalizations, which is a result of a 3.8% increase in diabetes population and a 2.6% decrease in the hospitalization rate, and 25% (0.4%) was due to the increase in cost per admission, for a net result of a 1.6% increase in cost per day and a 1.3% decline in mean length of stay. By component, the cost of short-term complications, lower-extremity amputations, and long-term complications increased annually by 4.2, 1.9, and 1.5%, respectively, while the cost of uncontrolled diabetes declined annually by 2.6%.
CONCLUSIONS
The total cost of diabetes-related preventable hospitalizations had been increasing during 2001–2014, mainly resulting from increases in number of people with diabetes and cost per hospitalization day. The underlying factors identified in our study could lead to efforts that may lower future hospitalization costs.
In 2015, more than 30 million people—9.4% of the U.S. population—were estimated to have diabetes either diagnosed or undiagnosed (1). The total hospital inpatient care costs reached 486 billion USD in 2017 (2), including 69.7 billion USD specifically due to diabetes (an increase from 49.9 billion USD in 2002) (3).
The Agency for Healthcare Research and Quality identified four diabetes-related conditions that result in preventable hospitalizations: short-term complications, long-term complications, uncontrolled diabetes, and lower-extremity amputations. Hospitalizations from these conditions could potentially be prevented with good ambulatory care (4); patients actively pursuing appropriate care; clinicians successfully diagnosing, treating, and educating patients in outpatient settings (5); and support for good care outside the clinical setting. Avoiding preventable hospitalizations could help to curtail large and rising health care costs, which have been a major concern among policy makers and health care professionals. Hospitalization costs can be decomposed into two primary underlying factors: 1) the number of preventable hospitalizations (derived from hospitalization rates among people with diabetes and the number of people with diabetes) and 2) cost per admission (derived from length of stay and cost per day).
Trends in diabetes-related hospitalization costs associated with the four specific preventable conditions above have previously been examined (6–8), with costs increasing between 2005 and 2010 (7) and during 2005–2014 (8). However, no previous studies have explored how primary and secondary underlying factors have contributed to the trends in total costs and for each of the four condition-specific causes of diabetes-related preventable hospitalizations. Exploring the trends and their underlying factors, overall and for each of the four conditions, might help identify opportunities to reduce the total cost burden of diabetes-related hospitalizations.
The objectives of our study were as follows: 1) to examine the long-term trends in diabetes-related preventable hospitalization costs, in total and by condition, among adults with diagnosed diabetes during 2001–2014 and 2) to examine the trends for each underlying factor and their individual contributions to these costs.
RESEARCH DESIGN AND METHODS
Data Sources
We used data from the 2001–2014 Healthcare Cost and Utilization Project (HCUP) National (Nationwide) Inpatient Sample (NIS). The NIS is the largest all-payer hospital inpatient care database in the U.S. It provides information on primary and secondary diagnoses and procedures, admission and discharge status, payments (charges and cost-to-charge ratios [CCRs]) and payment sources, and weights for producing nationally representative estimates. The NIS is drawn from the states participating in HCUP: 33–46 states with 7–8 million unweighted inpatient records per year during 2001–2014 (9). For each study year, we merged core, hospital, trend weight, and CCR files following NIS guidelines.
To obtain estimates of the population aged ≥18 years with diagnosed diabetes, we used data published by the Centers for Disease Control and Prevention (available from https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html), which are based on the 2001–2014 National Health Interview Survey (NHIS).
Identifying Diabetes-Related Preventable Hospitalizations
We identified the four diabetes-related conditions resulting in preventable hospitalizations using definitions developed by the Agency for Healthcare Research and Quality (4) and ICD-9 codes. These include: 1) short-term diabetes complications (e.g., diabetic ketoacidosis, hypersomolarity, or coma [ICD-9 codes 250.1–250.3]), 2) long-term diabetes complications (e.g., renal, ophthalmic, or neurological manifestations and peripheral circulatory disorders [ICD-9 codes 250.4–250.9]), 3) uncontrolled diabetes without complications (e.g., high glucose concentrations [ICD-9 codes 250.02 or 250.03]), and 4) diabetes-related lower-extremity amputations (procedure code 84.1) (10). Identification of these conditions was based on primary diagnosis, except for lower-extremity amputations, for which secondary diagnosis was also used. Overall costs were calculated for people with any of the four conditions; the sum of costs across the four conditions may exceed the overall cost because those with lower-extremity amputations as a secondary diagnosis may also have had a diabetes-related primary diagnosis.
Decomposition of the Total Cost
The total costs of diabetes-related preventable hospitalizations were decomposed according to primary and secondary contributing factors (Fig. 1). At the first level, total cost was calculated as a product of the total number of diabetes-related preventable hospitalizations and the mean cost per admission. At the second level, the number of preventable hospitalizations was calculated as a product of the estimated number of people with diabetes and the rate of preventable hospitalizations in this population. Similarly, mean cost per admission was calculated as a product of mean length of stay per admission and mean cost per day. Thus, any observed changes in total cost over time are the result of changes in the four level 2 factors (Fig. 1).
Figure 1—
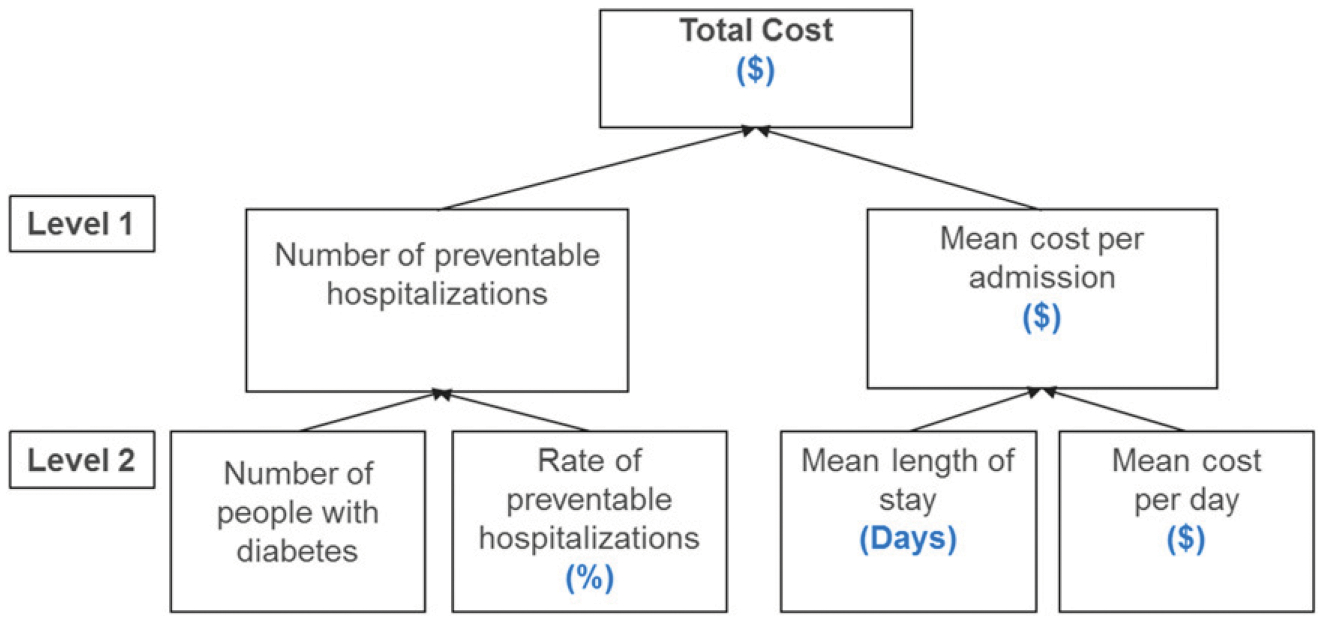
Framework for decomposition of diabetes-related preventable hospitalization total costs.
Estimation
For each study year, we estimated total diabetes-related preventable hospitalization cost and total number of preventable hospitalizations, weighted by appropriate trend weights and with complex sampling design accounted for.
During the study period there was a change in NIS design. Through 2011, the data consisted of all discharges from a 20% stratified sample of U.S. community hospitals participating in HCUP. From 2012 onward, the data consisted of a 20% sample of discharges from all U.S. community hospitals participating in HCUP. The definitions of hospitals and hospitalizations were also changed in 2012 from those used by the American Hospital Association Annual Survey to those used by statewide data organizations that contributed to HCUP. The new definition excludes the long-term acute care hospitals classified as community hospitals by the American Hospital Association if they had average length of stay <30 days (11). NIS adjusts for these changes using trend weights for years preceding 2012 (12,13). In addition, year-specific hospitalizations were reweighted following the NIS user guides (14) to account for missing costs due to nonparticipation by some states.
Hospital charges are different from hospital costs. Hospital charges are the amounts that hospitals bill for the in-patient stay, whereas hospital costs also include professional fees and non-covered charges and reflect the actual cost of hospital services, including wages, supplies, and utility costs (15). For cost estimates, we converted hospital charges to hospital costs by multiplying charges by hospital-specific CCRs, as recommended in NIS guidelines (14). We then computed the cost per day of stay by dividing the cost per admission by the corresponding length of stay. All costs were adjusted to 2014 U.S. dollars using the gross domestic product price index (16,17).
Diabetes-related preventable hospitalization rates were calculated by dividing the total number of diabetes-related preventable hospitalizations by the total number of people with diabetes. Length of stay was calculated as the difference between the admission date and the discharge date, with same-day stays recoded as 1 day.
Estimation of Trends
For each of the four preventable diabetes outcomes, we estimated average annual change and average annual percent change (AAPC) from 2001 to 2014. We used ordinary least squares to estimate trends of average annual change. Because most series were not linear, we used joinpoint regression (18) to estimate their trends in terms of AAPC.
Data preparation was conducted in SAS 9.3 (SAS Institute, Cary, NC). We used SUDAAN 9.3 (Research Triangle Institute, Research Triangle Park, NC) to estimate diabetes-related preventable hospitalizations and associated costs, accounting for the complex survey design, and STATA, version 14, for analyzing adjusted models. Estimates were considered statistically significant if P <0.05 (t test).
Decomposition of Trends
We used the method described by Dunn et al. (19), one of the commonly used methods for the decomposition of economic growth, to decompose trends in total costs at each level (Fig. 1). For example, if the total cost at time t (tct) is the product of total number of hospitalizations (hospt) and mean cost per admission (mct), then the cost increases can be decomposed into those attributable to the two factors as follows:
where TCt is total cost growth index, a ratio of total cost at time t (current year) (tct) to total cost at time 0 (base year) (i.e., ), HOSPt is the growth indices for total number of hospitalizations , and MCt is the growth index for mean cost per admission . We applied this approach to trends estimated as AAPC during 2001–2014 that account for nonlinearity in trends. To assess the sensitivity of our results, we also decomposed the estimates between 2001 and 2014 assuming linearity in trends (Supplementary Table 2).
RESULTS
Estimated total cost for diabetes-related preventable hospitalizations was 4.5 billion USD in 2001, increasing 1.6% (92.9 million USD; P <0.001) annually to 5.9 billion USD in 2014 (Figs. 2 and 3 and Table 1). Costs were consistently highest for long-term complications, which increased annually by 1.5% or 45.1 million USD (2.7 billion USD, 59% of the total in 2001, and 3.3 billion USD, 57% of total in 2014). Lower-extremity amputations carried the next-highest costs, increasing annually by 1.9% or 26.7 million USD (1.6 billion USD, 36% of the total in 2001, and 2.1 billion USD, 36% in 2014). Short-term complication costs increased annually by 4.2% or 44.0 million USD (0.8 billion USD, 17.5% of the total in 2001, and 1.4 billion USD, 23% in 2014). In contrast, the costs for uncontrolled diabetes were lower and declined annually by 2.6% or 4.3 million USD (0.3 billion USD, 5.6% of the total in 2001, and 0.2 billion USD, 3% of total in 2014).
Figure 2—
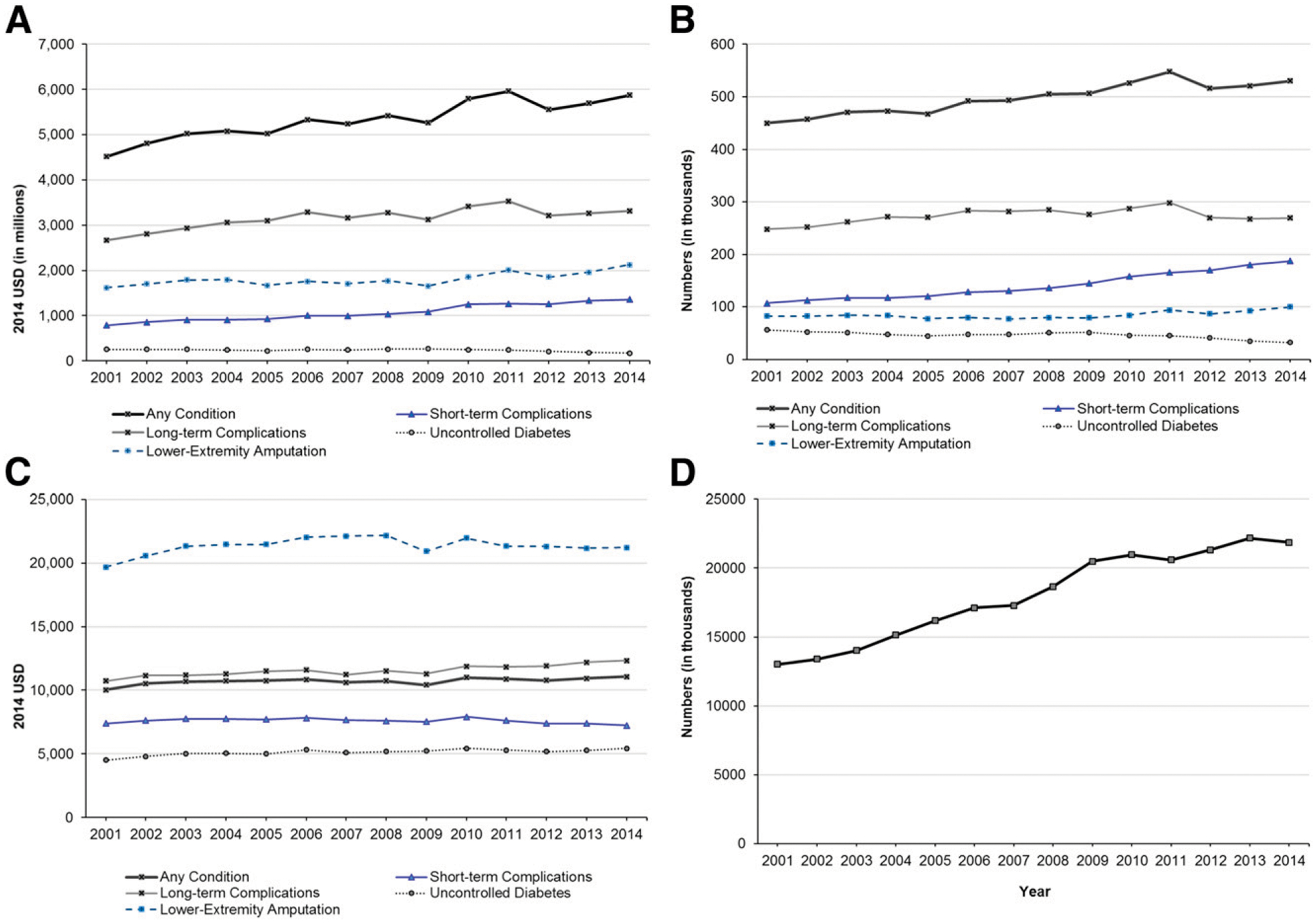
A–G:Trends in diabetes-related preventable hospitalizations overall and by level 1 and level 2contributing factors, total by condition, during 2001–2014. A: Total costs. B: Number of preventable hospitalizations. C: Mean cost per admission. D: Number of people with diabetes. E: Mean length of stay. F: Rate of preventable hospitalizations. G: Mean cost per day. Outcomes accounted for complex sampling design and trends weights for national estimates. Costs were adjusted to 2014 USD using the gross domestic product deflator.
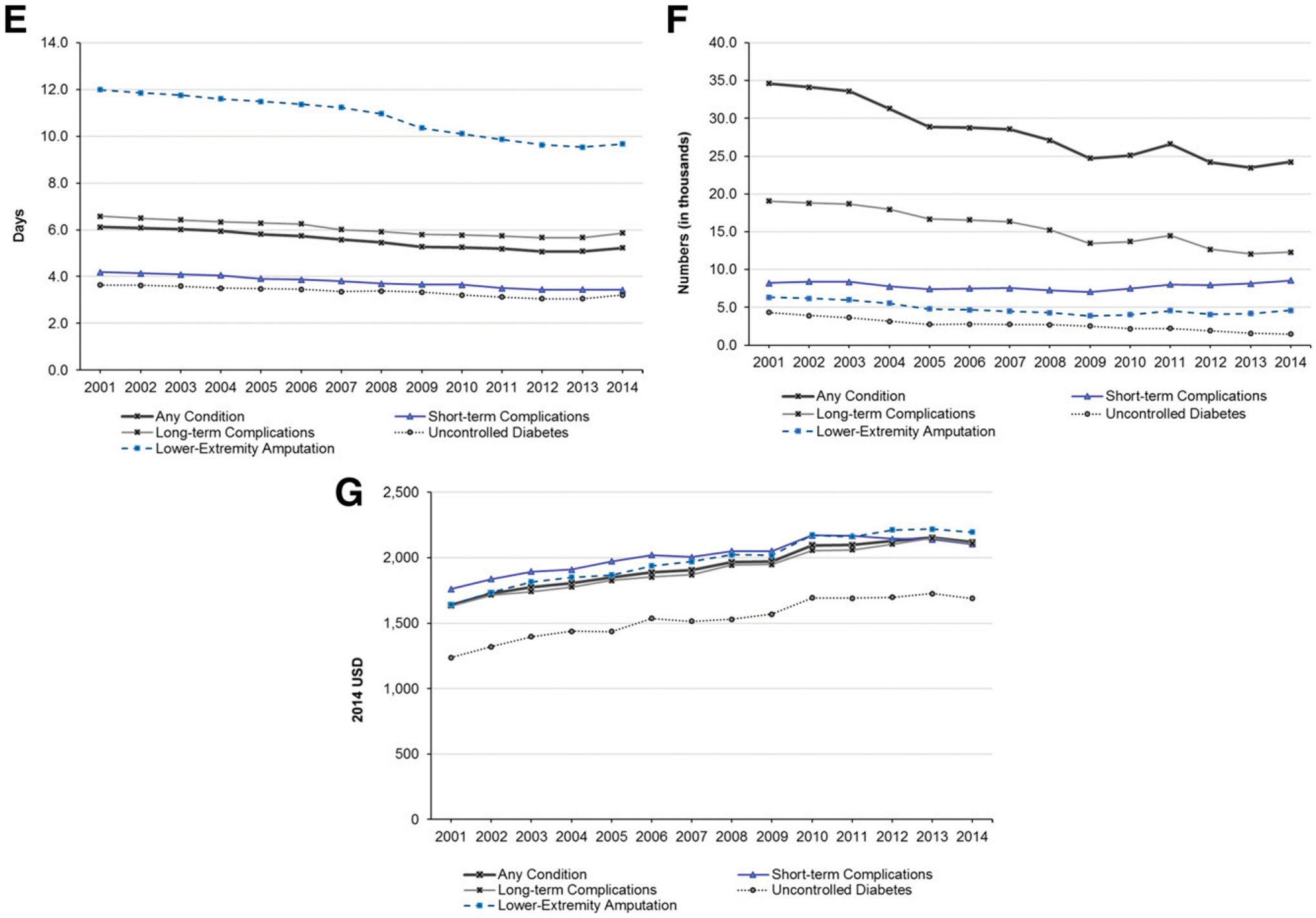
Figure 3—
A–E: Annual average percentage trends in diabetes-related preventable hospitalization (DRPH) costs, total and by contributing factors, overall and by condition, 2001–2014. A: Any diabetes-related preventable hospitalizations. B: Diabetes-related short-term complications. C: Diabetes-related long-term complications. D: Uncontrolled diabetes. E: Diabetes-related lower-extremity amputation. ***P <0.001.
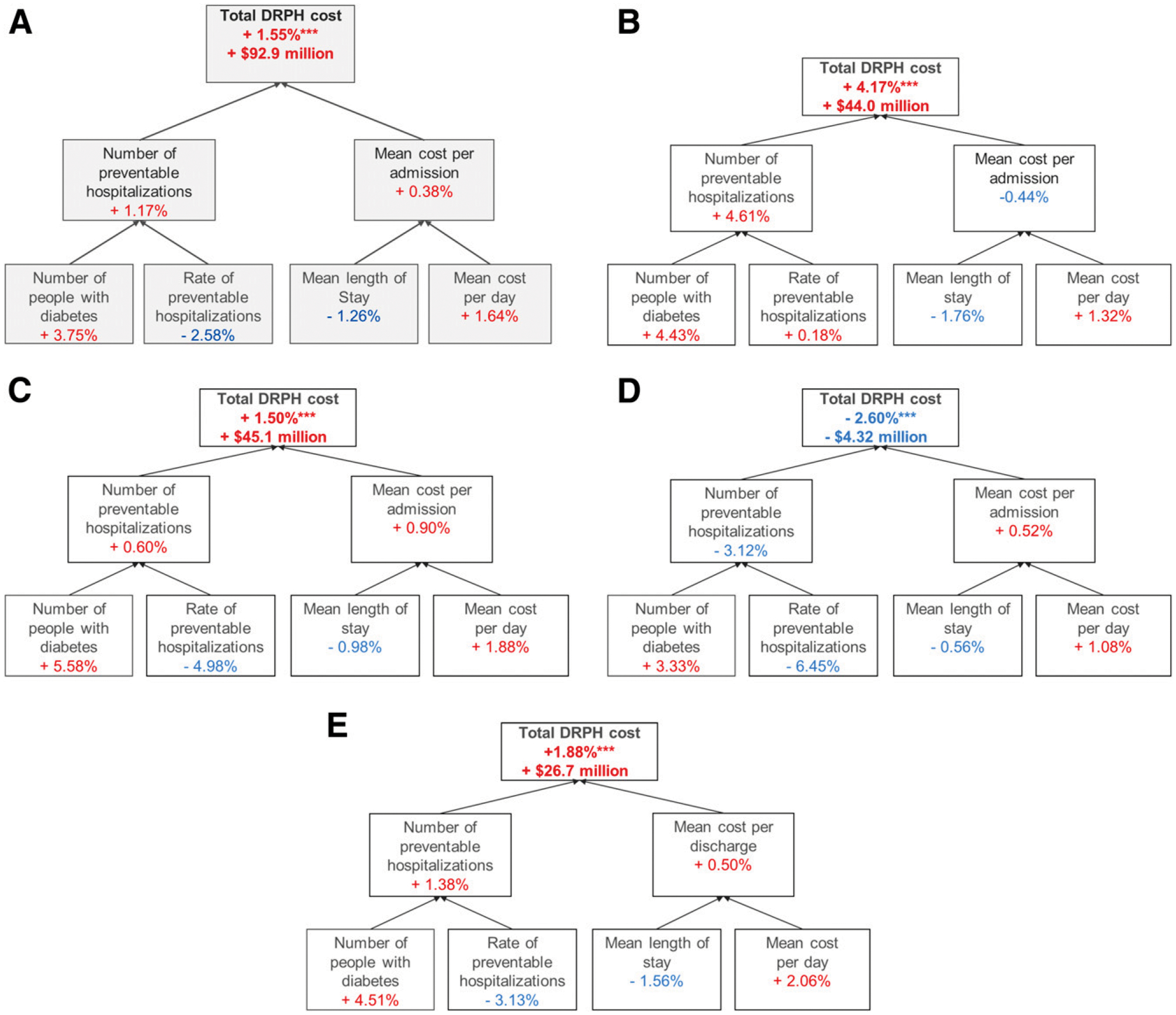
Table 1—
Estimates and trends in total diabetes-related preventable hospitalization costs and contributing factors overall and by condition (2001–2014)
| Annual average trends, 2001–2014 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimates | 95% CI | 95% CI | ||||||||
| Condition | Year 2001 | Year 2014 | Amount | LL | UL | P | Percent | LL | UL | P |
| Total cost (in million USD) | ||||||||||
| Any condition | 4,513 | 5,873 | 92.9 | 68.5 | 117 | *** | 1.55 | 1.16 | 1.93 | *** |
| Short-term complications | 789 | 1,355 | 44 | 38.4 | 49.6 | *** | 4.17 | 3.77 | 4.58 | *** |
| Long-term complications | 2,662 | 3,319 | 45.1 | 24.5 | 65.6 | *** | 1.5 | 0.41 | 2.6 | ** |
| Uncontrolled diabetes | 253 | 173 | −4.32 | −7.58 | −1.05 | * | −2.6 | −3.89 | −1.29 | *** |
| Lower-extremity amputation | 1,620 | 2,123 | 26.7 | 12.9 | 40.4 | *** | 1.88 | 0.58 | 3.19 | *** |
| No. of preventable hospitalizations | ||||||||||
| Any condition | 450,025 | 530,190 | 6,648 | 4,997 | 8,299 | *** | 1.19 | 0.93 | 1.45 | *** |
| Short-term complications | 106,854 | 187,390 | 6,245 | 5,452 | 7,038 | *** | 4.41 | 3.88 | 4.94 | *** |
| Long-term complications | 247,919 | 268,985 | 1,702 | −57 | 3,460 | 0.06 | 0.59 | −0.19 | 1.38 | 0.14 |
| Uncontrolled diabetes | 56,133 | 31,935 | −1,299 | −1,869 | −729 | *** | −4.14 | −6.82 | −1.39 | *** |
| Lower-extremity amputation | 82,335 | 100,045 | 1,042 | 271 | 1,814 | * | 1.28 | 0.16 | 2.42 | * |
| Mean cost per admission (USD) | ||||||||||
| Any condition | 10,027 | 11,077 | 44.49 | 15.6 | 73.38 | ** | 0.39 | 0.17 | 0.62 | *** |
| Short-term complications | 7,387 | 7,230 | −14.13 | −42.04 | 13.79 | 0.29 | −0.41 | −0.77 | −0.04 | * |
| Long-term complications | 10,738 | 12,338 | 95.37 | 69.11 | 121.6 | *** | 0.89 | 0.68 | 1.11 | *** |
| Uncontrolled diabetes | 4,507 | 5,426 | 52.04 | 31.17 | 72.91 | *** | 0.71 | 0.3 | 1.13 | *** |
| Lower-extremity amputation | 19,672 | 21,223 | 8.67 | −74.56 | 91.9 | 0.82 | 0.46 | −0.16 | 1.09 | 0.14 |
| No. of people with diabetes (in thousands) | 13,006 | 21,872 | 772.1 | 679.7 | 864.6 | *** | 4.35 | 3.76 | 4.94 | *** |
| Rate of preventable hospitalizations (%) | ||||||||||
| Any condition | 3.46 | 2.42 | −0.09 | −0.11 | −0.07 | *** | −2.89 | −3.36 | −2.43 | *** |
| Short-term complications | 0.82 | 0.86 | 0 | −0.01 | 0.01 | 0.94 | 0.17 | −0.58 | 0.92 | 0.66 |
| Long-term complications | 1.91 | 1.23 | −0.06 | −0.07 | −0.05 | *** | −3.73 | −4.15 | −3.31 | *** |
| Uncontrolled diabetes | 0.43 | 0.15 | −0.02 | −0.02 | −0.02 | *** | −7.92 | −10.96 | −4.78 | *** |
| Lower-extremity amputation | 0.63 | 0.46 | −0.02 | −0.02 | −0.01 | *** | −2.91 | −4.3 | −1.5 | *** |
| Mean length of stay (days) | ||||||||||
| Any condition | 6.12 | 5.23 | −0.09 | 0.01 | −0.1 | *** | −1.38 | 1.67 | −1.1 | *** |
| Short-term complications | 4.19 | 3.44 | −0.06 | 0 | −0.07 | *** | −1.59 | −1.85 | −1.33 | *** |
| Long-term complications | 6.58 | 5.85 | −0.07 | 0.01 | −0.09 | *** | −0.97 | −1.24 | −0.7 | *** |
| Uncontrolled diabetes | 3.64 | 3.21 | −0.05 | 0 | −0.06 | *** | −1.11 | −1.74 | −0.48 | *** |
| Lower-extremity amputation | 11.98 | 9.66 | −0.21 | 0.01 | −0.24 | *** | −1.68 | −2.03 | −1.33 | *** |
| Mean cost per day (USD) | ||||||||||
| Any condition | 1,639 | 2,120 | 38.88 | 34.21 | 43.55 | *** | 1.83 | 1.49 | 2.16 | *** |
| Short-term complications | 1,762 | 2,103 | 29.62 | 22.28 | 36.95 | *** | 1.21 | 0.86 | 1.56 | *** |
| Long-term complications | 1,632 | 2,107 | 38.78 | 34.73 | 42.84 | *** | 1.89 | 1.6 | 2.19 | *** |
| Uncontrolled diabetes | 1,237 | 1,689 | 36.12 | 30.09 | 42.14 | *** | 2.19 | 1.53 | 2.84 | *** |
| Lower-extremity amputation | 1,642 | 2,196 | 40.63 | 35.17 | 46.09 | *** | 2.26 | 1.57 | 2.96 | *** |
Types of data as described in the leftmost column apply to the columns entitled “Estimates.” All costs were adjusted to 2014 USD using gross domestic product deflator. Trends for annual average amounts were estimated using ordinary least squares regression. Trends for annual average percentage changes were estimated using joinpoint regression. Amount, absolute value; LL, lower limit; UL, upper limit.
P <0.05;
P <0.01;
P <0.001.
Of the 1.6% annual increase in total costs, most (75% of 1.6% increase [or 1.2%]) were attributable to an increase in the number of diabetes-related preventable hospitalizations, while the remainder (25% of 1.6% increase in total [or 0.4%]) was due to increases in mean cost per admission (Fig. 3A and Supplementary Table 1). With these costs further decomposed into secondary factors, the 1.2% annual increase in the number of diabetes-related preventable hospitalizations was due to a 3.8% annual increase in the number of people with diabetes, countered by a 2.6% average annual decline in their rate of hospitalizations. The 0.4% annual increase in mean cost per admission was the net effect of a 1.3% annual decline in the mean length of stay and a 1.6% annual increase in mean cost per day.
The relative contribution of decomposition factors was generally similar across the four diabetes-related conditions, with some notable exceptions (Fig. 3B–E and Supplementary Table 1). For short-term complications, the increase in total cost was attributed to a large increase in the number of preventable hospitalizations (4.6% annually) offset by a slight decrease in mean cost per admission (−0.4% annually). The hospitalization rates remained nearly constant (0.2% increase) rather than decreasing, while the number of people with diabetes increased, contributing to a larger increase in the total number of preventable hospitalizations. The decrease in cost per admission was the net effect of larger decreases in length of stay (−1.8% annually) compared with increases in cost per day (1.3% annually). For uncontrolled diabetes, the overall decrease in cost was due to a 3.1% decline in the total number of hospitalization, as the annual decline in hospitalization rate (−6.5%) was greater than the increase in the size of the population with diabetes.
CONCLUSIONS
To our knowledge, this study is the first to decompose the increasing trends in total costs associated with diabetes-related preventable hospitalizations attributable to trends of the underling contributing factors. During 2001–2014, the total cost for diabetes-related preventable hospitalizations increased substantially, from 4.5 to 5.9 billion USD, corresponding to annual increases of 92.9 million USD or 1.6%. A similar pattern was also observed for specific diabetes-related conditions (short-term complications, long-term complications, and lower-extremity amputations) with the exception of uncontrolled diabetes, which was of much lower magnitude to begin with and decreased by 2.6% annually. The overall increases were driven by increases in the size of the population with diabetes and the mean cost per day, which were larger than simultaneous decreases in hospitalization rates and lengths of stay. The contributions of underlying factors to the trends were relatively consistent across the conditions. For example, for all conditions, the growth of the population with diabetes was the largest increasing factor: cost per day was increasing, and length of stay was decreasing. Hospitalization rates decreased for all conditions except short-term complications, although the relative decrease was much larger for uncontrolled diabetes than for long-term complications and lower-extremity amputations.
Our results of declining trends in hospitalization rates are consistent with those from prior studies (20,21). Similar results have also been observed for diabetes-related preventable hospitalizations overall (22) and for nontraumatic lower-extremity amputations (23). Our results of declining preventable hospitalization rates among the diabetes population are also consistent with results from earlier studies; the preventable hospitalization rate per general population was previously shown to increase for short-term complications (8,24) but decrease for uncontrolled diabetes (23,24), long-term complications (23), and lower-extremity amputations (24). This pattern of overall decline in preventable hospitalization rates could be attributed to improvements in risk factors and diabetes management. For example, prior studies show that diabetes education visits in primary care settings (25) and persistent use of antidiabetes medication may be associated with a decline in hospitalization rates (26,27). The lower rate of hospitalization across the complications could also be associated with other factors such as better scheduled primary care access and glycemic control as shown by Calderón-Larrañaga et al. (28) in England. Another reason for the decline could be the growing penetration of private managed care, which has been associated with a decline in ambulatory care hospitalization rates (29,30) and an overall decline in the rate of inpatient stays (31).
The decrease in length of stay for diabetes-related preventable hospitalization is consistent with a recent estimate using 2005–2014 data (8) and results for overall hospitalizations (16) and for other specific conditions, such as heart failure and surgeries (21,32–34). These changes may reflect advancement in clinical medical technology, as well as changes in health policy that discourage long inpatient hospital stays. The reduction in length of stay for diabetes-related preventable hospitalization could also be attributed to improved glucose management in hospital settings (35).
Despite the reduction in the length of stay, the average cost per admission remained roughly stable (for short-term complications and lower-extremity amputations), or increased (overall and for long-term complications and uncontrolled diabetes), due to the offsetting effect of increases in mean cost per day. This was especially true for long-term complications, for which increase in the cost per day was the primary cause of overall cost increases. The reasons for this pattern are not clear. It is generally assumed that reducing average length of stay will result in big cost savings. However, improvement in length of stay may not necessarily translate into proportionately lower per-admission cost, as the cost of hospitalization tends to be lower toward end of a patient’s stay (36). Ironically, therefore, decreases in length of stay can result in increases in mean cost per day. Improvements in diabetes self-management and ambulatory care, and the resulting improved control and reduction of complications, may help reduce the severity of hospitalization cases and thereby lower the cost per admission.
The finding that increases in diabetes-related preventable hospitalization costs (overall and for short-term complications and lower-extremity amputations) were primarily due to increases in the number of people with diabetes reinforces the importance of continued type 2 diabetes prevention efforts, despite a decline in incidence of type 2 diabetes in recent years (37,38).
Our study has several limitations that must be considered while interpreting the results. First, we were not able to distinguish diabetes by type. Trends in preventable hospitalization outcomes and costs could differ between type 1 and type 2 diabetes because of differences in natural courses and management of the disease. Because type 2 diabetes accounts for ~95% of adults with diabetes in the U.S. (39), our results are likely to predominantly reflect trends in preventable hospitalization outcomes for type 2 diabetes. Second, the results are subject to potential inaccuracy of diagnostic codes. Third, the categories of diabetes-related preventable hospitalization were defined based on experts’ consensus. Different classification based on empirical evidences could be used if such classification was available. Finally, the data may not be representative of noncommunity hospitals, such as Veterans Administration hospitals, Indian Health Service, and psychiatric, substance abuse, and long-term care hospitals.
During 2001–2014, the total costs associated with diabetes-related preventable hospitalizations increased by 92.9 million USD or 1.6% annually. These increases occurred despite substantial improvements in the rate of preventable hospitalizations and reduced lengths of stay, which were offset by larger increasing trends in mean costs per day and, more importantly, increases in the size of the diabetes population. While costs for uncontrolled diabetes decreased, the burden increased overall and for short-term complications, lower-extremity amputations, and long-term complications. Our results highlight the importance of stemming the tide in the type 2 diabetes epidemic and of improving ambulatory care and diabetes management to reduce preventable hospitalizations and their costs.
Supplementary Material
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-1078/-/DC1.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017 [Internet], 2017. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Available from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 31 July 2017 [Google Scholar]
- 2.American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018;41:917–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hogan P, Dall T, Nikolov P; American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care 2003;26:917–932 [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality. AHRQ qQuality Indicators. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Version 3.1. Rockville, MD, Agency for Healthcare Research and Quality, 2001. (AHRQ publ. no. 02-R0203). Available from http://www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V31/pqi_guide_v31.pdf. Accessed 21 September 2016 [Google Scholar]
- 5.Kruzikas DT, Jiang HJ, Remus D, Barrett ML, Coffey RM, Andrews R. Preventable Hospitalizations: A Window Into Primary and Preventive Care, 2000. Rockville, MD, Agency for Healthcare Research and Quality, 2004. (AHRQ publ. no. 04–0056) [Google Scholar]
- 6.Russo A, Jiang HJ, Barrett M. Trends in potentially preventable hospitalizations among adults and children, 1997–2004. Statistical brief #36. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 7.Torio CM, Elixhauser A, Andrews RM. Trends in potentially preventable hospital admissions among adults and children, 2005–2010. Statistical brief #151. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 8.Rubens M, Saxena A, Ramamoorthy V, et al. Trends in diabetes-related preventable hospitalizations in the U.S., 2005–2014. Diabetes Care 2018;41:e72–e73 [DOI] [PubMed] [Google Scholar]
- 9.Agency for Healthcare Research and Quality. 2013 Introduction to the NIS. Healthcare Cost and Utilization Project (HCUP) [Internet], 2016. Available from www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2013.jsp. Accessed 22 September 2016 [Google Scholar]
- 10.Agency for Healthcare Research and Quality. Prevention Quality Indicators Technical Specifications-Version 5.0 [Internet], 2015. Available from https://www.qualityindicators.ahrq.gov/Modules/PQI_TechSpec_ICD10.aspx. Accessed 22 September 2016
- 11.Houchens R, Ross D, Elixhauser A, Jiang J. Nationwide Inpatient Sample (NIS) Redesign Final Report [Internet], 2014. HCUP Methods Series Report # 2014–04 ONLINE. April 4, 2014. U.S. Agency for Healthcare Research and Quality. Available from https://www.hcup-us.ahrq.gov/reports/methods/2014-04.pdf. Accessed 11 November 2018 [Google Scholar]
- 12.Agency for Healthcare Research and Quality. HCUP NIS Trend Weights. Health Care Cost and Utilization Project (HCUP) [Internet], 2015. Available from www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp. Accessed 12 May 2015 [Google Scholar]
- 13.Houchens RL, Ross D, Elixhauser A. Using the HCUP National Inpatient Sample to Estimate Trends [Internet], 2015. HCUP Methods Series Report # 2006–05 ONLINE. January 4, 2016. U.S. Agency for Healthcare Research and Quality. Available from https://www.hcup-us.ahrq.gov/reports/methods/2006_05_NISTrendsReport_1988-2004.pdf. Accessed 11 November 2018 [Google Scholar]
- 14.Agency for Healthcare Research and Quality. Cost-to-Charge Ratio Files. Healthcare Cost and Utilization Project (HCUP). Rockville, MD, Agency for Healthcare Research and Quality, 2015. Available from www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed November 12 2015 [Google Scholar]
- 15.Pfuntner A, Levit K, Elixhauser A. Components of cost increases for inpatient hospital procedures, 1997–2009. Statistical brief #133. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 16.Pfuntner A, Wier LM, Elixhauser A. Overview of hospital stays in the United States, 2011. Statistical brief #166. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 17.Bureau of Economic Analysis. National data. Section 1, domestic product and income. Table 1.1.4, price indexes for gross domestic product [Internet], 2016. Available from https://apps.bea.gov/histdata/fileStructDisplay.cfm?HMI=7&DY=2016&DQ=Q2&DV=Third&dNRD=September-29-2016. Accessed 21 September 2016
- 18.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med 2009; 28:3670–3682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dunn A, Liebman EB, Shapiro A. Decomposing medical-care expenditure growth [Internet]. Cambridge, MA, National Bureau of Economic Research, 2017. Available from http://www.nber.org/papers/w23117.pdf. Accessed 6 November 2017 [Google Scholar]
- 20.Wang J, Imai K, Engelgau MM, Geiss LS, Wen C, Zhang P. Secular trends in diabetes-related preventable hospitalizations in the United States, 1998–2006. Diabetes Care 2009;32: 1213–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stranges E, Friedman B. Potentially preventable hospitalization rates declined for older adults, 2003–2007. Statistical brief #83. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 22.Moy E, Chang E, Barrett M; Centers for Disease Control and Prevention (CDC). Potentially preventable hospitalizations - United States, 2001–2009. MMWR Suppl 2013;62: 139–143 [PubMed] [Google Scholar]
- 23.Li Y, Burrows NR, Gregg EW, Albright A, Geiss LS. Declining rates of hospitalization for nontraumatic lower-extremity amputation in the diabetic population aged 40 years or older: U.S., 1988–2008. Diabetes Care 2012; 35:273–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fingar KR, Barrett ML, Elixhauser A, Stocks C, Steiner CA. Trends in potentially preventable inpatient hospital admissions and emergency department visits. Statistical brief #195. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 25.Robbins JM, Thatcher GE, Webb DA, Valdmanis VG. Nutritionist visits, diabetes classes, and hospitalization rates and charges: the Urban Diabetes Study. Diabetes Care 2008; 31:655–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lo-Ciganic WH, Donohue JM, Jones BL, et al. Trajectories of diabetes medication adherence and hospitalization risk: a retrospective cohort study in a large state Medicaid program. J Gen Intern Med 2016;31:1052–1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stuart BC, Simoni-Wastila L, Zhao L, Lloyd JT, Doshi JA. Increased persistency in medication use by U.S. Medicare beneficiaries with diabetes is associated with lower hospitalization rates and cost savings. Diabetes Care 2009;32:647–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calderón-Larrañaga A, Soljak M, Cecil E, et al. Does higher quality of primary healthcare reduce hospital admissions for diabetes complications? A national observational study. Diabet Med 2014;31:657–665 [DOI] [PubMed] [Google Scholar]
- 29.Backus L, Moron M, Bacchetti P, Baker LC, Bindman AB. Effect of managed care on preventable hospitalization rates in California. Med Care 2002; 40:315–324 [DOI] [PubMed] [Google Scholar]
- 30.Basu J Preventable hospitalizations and Medicare managed care: a small area analysis. Am J Manag Care 2012;18:e280–e290 [PubMed] [Google Scholar]
- 31.Weiss AJ, Elixhauser A. Overview of hospital stays in the United States, 2012. Statistical brief #180. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, Agency for Healthcare Research and Quality, 2006 [PubMed] [Google Scholar]
- 32.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA 2010;303:2141–2147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alosh H, Li D, Riley LH III, Skolasky RL. Health care burden of anterior cervical spine surgery: national trends in hospital charges and length of stay, 2000–2009. J Spinal Disord Tech 2015;28: 5–11 [DOI] [PubMed] [Google Scholar]
- 34.Cary MP Jr., Baernholdt M, Merwin EI. Changes in payment regulation and acute care use for total hip replacement: trends in length of stay, costs, and discharge, 1997–2012. Rehabil Nurs 2016;41:67–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahmann A Reduction of hospital costs and length of stay by good control of blood glucose levels. Endocr Pract 2004;10(Suppl. 2):53–56 [DOI] [PubMed] [Google Scholar]
- 36.Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg 2000;191: 123–130 [DOI] [PubMed] [Google Scholar]
- 37.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA 2014;312:1218–1226 [DOI] [PubMed] [Google Scholar]
- 38.Diagnosed diabetes [Internet]. Available from https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html. Accessed 4 May 2018
- 39.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2014: Estimates of Diabetes and Its Burden in the United States [Internet]. Atlanta, GA, U.S. Department of Health and Human Services. Available from https://www.cdc.gov/diabetes/pdfs/data/2014-report-estimates-of-diabetes-and-its-burden-in-the-united-states.pdf. Accessed 11 November 2018 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


