Abstract
Objectives
Data on work participation impairment and related societal costs for patients with hand osteoarthritis (OA) are scarce. Therefore, we aimed to investigate the association of hand OA with work limitations and costs of productivity loss in paid and unpaid work.
Methods
We used data from the Hand Osteoarthritis in Secondary Care cohort, including patients with hand OA diagnosed by their treating rheumatologist. Using the validated Health and Labour Questionnaire, we assessed experienced unpaid and paid work restrictions, unpaid work replacement by others and inefficiency and absence during paid work related to hand OA over the last 2 weeks. Societal costs (€) per hour of paid and unpaid work were estimated using Dutch salary data in 2019.
Results
381 patients were included (mean age 61 years, 84% women, 26% high education level, 55% having any comorbidity). Replacement of unpaid work by others due to hand OA was necessary for 171 out of 381 patients (45%). Paid work was reported by 181/381 patients (47%), of whom 13/181 (7%) reported absenteeism, 28/181 (15%) unproductive hours at work and 120/181 (66%) paid work restrictions due to hand OA.
Total estimated work-related societal costs per patient with hand OA (381 patients) were €94 (95% CI 59 to 130) per 2 weeks (€2452, 95% CI 1528 to 3377 per year).
Conclusions
Hand OA is associated with impairment in paid and unpaid work participation, which translates into substantial societal costs of lost productivity. These results highlight the importance of adequate hand OA treatment.
Keywords: osteoarthritis, economics, epidemiology
What is already known about this subject?
Several rheumatic musculoskeletal diseases have been shown to impact paid and unpaid work participation.
What does this study add?
This study reveals the impact of hand osteoarthritis (OA) on work, as well as high associated societal costs.
This study calls for attention for the work status of patients with hand OA.
How might this impact on clinical practice or further developments?
This study shows the economic and societal importance of adequate hand OA management.
Introduction
Osteoarthritis (OA) is a highly prevalent chronic disorder that can affect any joint.1 It results in symptoms of pain, disability, weakness and stiffness of the joints leading to loss of quality of life and participation.2–4 Also, these OA symptoms can cause work restrictions. OA symptoms not only can affect paid work leading to absenteeism (absence from paid work due to disease), experience of impediments at work (presenteeism)5 and change in or loss of occupation,6 7 but also can affect unpaid work.8 This may result in the necessity of replacement of unpaid work by others, such as relatives or a paid housekeeper. Studies have indeed shown that OA leads to performing less paid or unpaid work, which can be defined as productivity loss.6 9 10
Various studies have demonstrated that productivity loss by patients with OA leads to societal costs.9–12 A recent study estimated societal costs at US$4274 (€3406 at 2019 price levels) per American patient with OA per year at 2019 price levels, using income loss as a surrogate for societal costs of lost productivity.11 Another study estimated €1526 per Italian patient with knee OA per year of societal costs due to productivity loss at 2019 price levels.12 Similar studies done in Canada and Portugal also indicated that OA is associated with societal costs through work due to productivity loss.9 10
These studies mostly concern OA of the lower extremities and do not specifically concern hand OA. The hands consist of many joints, in which OA frequently occurs.13 14 As the hands are required for most activities in daily life,13 it is likely that hand OA also results in productivity loss and associated costs. However, data on productivity loss for specifically hand OA are scarce. In one study, no association was found between hand OA and early exit from paid work,9 but no information on presenteeism and societal costs was provided. This knowledge is crucial for gaining insight in the impact of hand OA on individuals and society, as well as in establishing the potential economic benefit of adequate treatment.
Therefore, we aimed to investigate the association of hand OA with restrictions in paid and unpaid work, related productivity loss and societal costs, as well as the patient and disease characteristics related to productivity loss.
Materials and methods
Study population
Data from the Hand Osteoarthritis in Secondary Care (HOSTAS) were used. This is an ongoing cohort on primary hand OA.15 Baseline data of the cohort were used for this study, including patients who filled in the Health and Labour Questionnaire (HLQ) (collected from January 2011 to October 2015).16 Written informed consent was obtained from all participants.
Presence of primary hand OA was defined by the treating rheumatologist. Distal interphalangeal (DIP), proximal interphalangeal (PIP), interphalangeal (IP), metacarpophalangeal (MCP), and first carpometacarpal (CMC1) hand joints were physically assessed for presence of bony swelling, soft swelling and tenderness on palpation (range 0–30).15 Fulfilment of the American College of Rheumatology (ACR) criteria for hand OA was defined.17 Self-reported hand pain and function were assessed with the Australian Canadian Hand OA Index (AUSCAN).18 Conventional dorsal–volar radiographs of the hands were scored according to the Kellgren-Lawrence system with good reliability.15 19 Erosive hand OA was defined as a joint in Verbruggen-Veys anatomical phases E (‘erosive’) or R (‘remodelling’).20 21 Comorbid diseases were recorded with a modified Charlson index22 (including osteoporosis) (range 0–18). Depression–anxiety was defined as a Hospital Anxiety and Depression Scale (HADS) score of ≥16 (range 0–42).23–25 Patients with an university degree were classified as having a high education level.
Work characteristics and costs
Physical and mental intensity of paid work was assessed using the classification by de Zwart et al,26 which is a spectrum from 1 (solely mentally demanding work) up to 6 (solely physically demanding).
The HLQ was used to acquire self-reported quantitative and qualitative data on the impact of hand OA on paid and unpaid work in the last 2 weeks.16 It divides the consequences of hand OA into three modules: absenteeism (defined as sick leave from paid work), presenteeism (in this study consisting of two aspects, namely, ‘unproductive hours while present at work’ and ‘work restrictions’, the latter described in the HLQ as ‘hinder at paid work’) and unpaid work impairment (consisting of replacement of unpaid work by others and hinder). Unproductive hours are measured by self-reported extra hours work that would be required to catch up unfinished tasks due to hand OA, and paid work restrictions are quantified using a hinder score (range 6–24) comprising several hand OA-related paid work impediments, such as loss of concentration and impaired decision making. For paid work absenteeism, patients are required to fill in at which date the absenteeism started and how many mornings and afternoons per 2 weeks are lost due to absence. Unpaid work is subdivided into household activities, groceries, chores and taking care of own children.
The societal costs of paid labour productivity loss were estimated by quantifying lost hours due to paid work absenteeism and presenteeism (in the form of extra hours to catch up with unproductive hours at work) caused by hand OA. Societal costs per hour of work lost were estimated based on the average gross salary per hour of the general country-specific population of the same age category and sex, converted to price levels of 201927 (online supplemental appendix 1 for price level conversion). Using a weight factor from Statistics Netherlands, this salary was converted to societal costs.28 Societal costs per hour multiplied by the hours of work lost resulted in total costs related to absenteeism and unproductive hours at work due to hand OA. If data on age, sex or hours per week of work were missing, no costs related to absenteeism or unproductive hours at work could be calculated, in which case these were counted as missing. All societal costs were assessed using a partial human-capital approach, which accounts for sick leave without accounting for possible replacement by a new employee after a set amount of time (the ‘friction period’).29 The societal costs of unpaid labour loss were estimated by multiplying the hours of unpaid labour lost by the replacement costs. These replacement costs were defined as the gross hourly salary of a paid Dutch household help in 2019 (€12.50 per hour).30
rmdopen-2022-002367supp001.pdf (86.4KB, pdf)
We also collected the self-reported salary and working hours of patients with paid work and compared this with the average net Dutch hourly salary stratified for age, sex and education level.28 In order to further estimate the impact of hand OA on paid work, we compared the salary of our cohort with the estimated salary of the Dutch general population having the same age (categorised per ten years), sex and working hours as our cohort.28
Statistical analysis
All outcomes solely regarded patients for whom information on the concerning outcome was available. Summed scores were regarded as missing in case of any missing component, or in case of more than one missing (AUSCAN pain and AUSCAN function) or two missing components (HADS). In these cases, the value of the missing component was counted as the mean of the non-missing components. The number of missing values for all outcomes was collected in online supplemental appendix 2 and did not exceed 5% except for ‘hand OA symptom duration’ and ‘predominantly manual profession’.
rmdopen-2022-002367supp002.pdf (93.4KB, pdf)
Outcomes were summarised as mean (SD). For the estimation of costs, 95% CI was used, as this was deemed more informative. In case of non-normally distributed or ordinal variables, median (IQR) was used. We compared our outcomes of hours of work with the Dutch general population data of the year 2013 adjusted for age and sex of our cohort, as 2013 is the mean year that our patients were assessed. All costs were adjusted to values for 2019 using consumer price indices from Statistics Netherlands27 (online supplemental appendix 1). Costs per 2 weeks were extrapolated to costs per year by using a conversion factor of 26.09.31 In a sensitivity analysis, analyses were repeated for those under state pension age on which Dutch persons usually retire (65 years), in order to allow comparison with other studies that investigate patients of working age. SPSS software for Windows V.25.0 was used.
Results
Study population
Between January 2011 and October 2015, 388 patients were included in the HOSTAS cohort, of whom 7 patients did not fill in the HLQ or a substantial part of it. Therefore, 381 patients were included in the present study. Characteristics of the study population are shown in table 1.
Table 1.
Characteristics of our present study population and of patients with and without paid work
| Total study population (N=381) | Patients with paid work (47%, n=181) | Patients without paid work (53%, n=200) | |
| General patient characteristics | |||
| Age (years) | 61 (8) | 55 (6) | 66 (7) |
| Sex, women, n (%) | 319 (84) | 150 (83) | 169 (85) |
| BMI (kg/m2) | 27.6 (4.9) | 27.5 (4.9) | 27.8 (5.0) |
| Living with a partner, n (%) | 312 (82) | 152 (84) | 160 (80) |
| Education, high,* n (%) | 101 (26) | 57 (31%) | 44 (21%) |
| Hand-specific characteristics | |||
| Fulfilling ACR hand OA criteria, n (%) | 344 (90) | 153 (85) | 191 (95) |
| Erosive hand OA, n (%) | 113 (30) | 35 (20) | 78 (39) |
| Symptom duration (years)† | 5.5 (2.1–13.0) | 4.3 (1.6–9.3) | 7.2 (2.8–17.7) |
| AUSCAN hand pain (0–20) | 9 (4) | 9 (5) | 10 (4) |
| AUSCAN hand function (0–36) | 16 (8) | 15 (9) | 17 (10) |
| Tender joint count (0–30)* | 3 (1–6) | 3 (1–6) | 4 (2–8) |
| KL summated score (0–120)† | 16 (8–29) | 13 (5–21) | 22 (11–37) |
| General burden | |||
| Any comorbidity present, n (%) | 209 (55) | 88 (49) | 121 (61) |
| Amount of comorbidities† | 1 (0–1) | 0 (0–1) | 1 (0–1) |
| Fulfilling ACR hip OA criteria, n (%) | 30 (8) | 9 (5) | 21 (6) |
| Fulfilling ACR knee OA criteria, n (%) | 127 (33) | 53 (29) | 74 (37) |
| HADS total score (0–42)† | 7 (4–12) | 7 (3–10) | 7 (4–12) |
| Work characteristics | |||
| Retired, n (%) | 116 (31) | – | 116 (58) |
| Full work disability, n (%) | 24 (6) | 5 (3) | 19 (12) |
| Full work disability due to hand OA, n (%) | 6 (2) | 6 (3) | 0 (0) |
| Partial work disability, n (%) | 12 (3) | 8 (4) | 4 (2) |
| Partial work disability due to hand OA, n (%) | 6 (2) | 4 (2) | 2 (1) |
| Predominantly manual profession, n (%)‡ | 26 (9) | 11 (17) | 15 (8) |
Numbers represent mean (standard deviation) unless otherwise specified.
*Defined as having completed university-level education.
†Median (IQR).
‡Defined as a score of 5 or 6 on the scale by de Zwart et al.26
ACR, American College of Rheumatology; AUSCAN, Australian Canadian Osteoarthritis Hand Index; BMI, body mass index; HADS, Hospital Anxiety and Depression Scale; KL, Kellgren-Lawrence; OA, osteoarthritis.
Paid work
In our cohort, 181 patients (47% of all patients, 69% of patients below Dutch retiring age) had paid work, on which a mean of 25.9 hours (SD 11.8) per week was spent. Paid work characteristics are shown in table 2. Of patients with paid work, 13 (7%) reported absenteeism due to hand OA in the last 2 weeks, with a median of 42 hours (IQR 24–52). Extra hours to catch up work due to hand OA were reported by 28 (15%) out of 181 patients with paid work, with a median of 4 hours (IQR 2–6). Presenteeism (‘unproductive hours’ or ‘work restrictions’) was reported by 137 (76%) out of 181. Of all working hours in the cohort, 5.6% were lost due to hand OA absenteeism and 1.4% to hand OA unproductive hours at work. Any paid work productivity loss (absenteeism or unproductive hours at work) occurred for 36 patients (20% of patients with paid work). Any paid work restrictions due to hand OA were reported by 120 (66%) out of 181 patients (table 2). Needing to slow down work pace was the most frequent reported form of hinder, as 17 patients (9% of patients with paid work) experienced this often or always at work.
Table 2.
Paid work outcomes of the Health and Labour Questionnaire concerning the last 2 weeks for patients having paid work (181 out of 381 patients)
| Hours of paid work per week | 25.9 (11.8) |
| Absenteeism due to hand OA | |
| Any absenteeism, n (%) | 13 (7) |
| Hours of absenteeism, if any* (n=13) | 42 (24–54) |
| Hours of absenteeism, total group (n=181) | 3 (14) |
| Unproductiveness at work due to hand OA | |
| Any unproductive hours at work, n (%) | 28 (15) |
| Hours of unproductiveness at work, if any* (n=28) | 4 (2–6) |
| Hours of unproductiveness, total group (n=181) | 1 (2) |
| Overall work productivity loss due to hand OA (=absenteeism and unproductive hours) | |
| Any work productivity loss, n (%) | 35 (19) |
| Hours of work productivity loss due to hand OA, if any (n=38) | 11 (4–35) |
| Hours of unproductiveness due to hand OA, total group (n=181) | 4 (14) |
| Activity restrictions at work due to hand OA | |
| Any form of paid work restrictions due to hand OA, n (%) | 120 (66) |
| Any presenteeism (=hinder or unproductive hours) due to hand OA | 137 (76) |
| Hinder score for complaints at work (6–24)* | 7 (6–8) |
| Impaired concentration due to hand OA (often or always), n (%) | 3 (2) |
| Needing to slow down work pace due to hand OA (often or always), n (%) | 17 (9) |
| Needing to seclude oneself due to hand OA (often or always), n (%) | 2 (1) |
| Difficulties in making decisions due to hand OA (often or always), n (%) | 0 (0) |
| Inability to complete work due to hand OA (often or always), n (%) | 2 (1) |
| Needing assistance at work due to hand OA (often or always), n (%) | 7 (4) |
Numbers represent mean (SD) unless otherwise specified.
*Median (IQR).
OA, =osteoarthritis.
Patients having paid work productivity loss due to absenteeism or unproductive hours at work because of hand OA (n=36) did not differ statistically significantly in patient and disease characteristics from those without productivity loss (n=145) (table 3).
Table 3.
Comparison of patients with and without productivity loss due to hand OA
| Patients with paid work (n=181) | All patients (N=381) | |||
| Paid work productivity loss (n=36) | No paid work productivity loss (n=145) | Unpaid work productivity loss (n=171) | No unpaid work productivity loss (n=210) | |
| General patient characteristics | ||||
| Age (years) | 55 (6) | 56 (6) | 61 (8) | 61 (9) |
| Sex (female), n (%) | 28 (78) | 122 (84) | 159 (93) | 161 (76) |
| BMI (kg/m2) | 28.2 (7.5) | 27.3 (4.8) | 28.6 (5.6) | 26.9 (4.2) |
| Living with a partner, n (%) | 28 (78) | 124 (76) | 144 (84) | 168 (80) |
| Education, high,§ n (%) | 11 (31) | 46 (32) | 34 (19) | 67 (32) |
| Hand-specific characteristics | ||||
| Fulfilling ACR hand OA criteria, n (%) | 29 (81) | 124 (86) | 157 (92) | 187 (88) |
| Erosive hand OA, n (%) | 8 (23) | 27 (19) | 43 (25) | 70 (33) |
| Symptom duration (years)* | 4.3 (1.2–11.6) | 4.2 (1.6–8.2) | 6.1 (1.6–14.6) | 4.8 (2.1–10.4) |
| AUSCAN hand pain (0–20) | 11 (4) | 8 (5) | 11 (4) | 8 (4) |
| AUSCAN hand function (0–36) | 19 (8) | 13 (8) | 19 (8) | 13 (8) |
| Tender joint count (0–30)* | 6 (2–9) | 2 (1–5) | 6 (2–9) | 3 (1–6) |
| KL summated score (0–120)* | 13 (5–21) | 12 (5–21) | 13 (5–21) | 17 (8–9) |
| General burden | ||||
| Any comorbidity present, n (%) | 19 (53) | 69 (48) | 109 (64) | 100 (47) |
| Amount of comorbidities* | 1 (0–1) | 1 (0–1) | 1 (0–2) | 0 (0–1) |
| Fulfilling ACR hip OA criteria, n (%) | 5 (14) | 4 (3) | 14 (8) | 16 (8) |
| Fulfilling ACR knee OA criteria, n (%) | 15 (42) | 38 (26) | 57 (34) | 70 (33) |
| HADS total score (0–42)* | 7 (5–12) | 6 (3–11) | 7 (4–14) | 6 (3–10) |
| Work characteristics | ||||
| Retired, n (%) | – | – | 46 (28) | 70 (33) |
| Full work disability, n (%) | 3 (8) | 2 (1) | 6 (3) | 3 (1) |
| Full work disability due to hand OA, n (%) | 0 (0) | 0 (0) | 3 (2) | 3 (2) |
| Partial work disability, n (%) | 3 (8) | 5 (3) | 6 (3) | 6 (3) |
| Partial work disability due to hand OA, n (%) | 1 (3) | 3 (2) | 2 (1) | 4 (2) |
| Unpaid work replacement, n (%) | 20 (56) | 53 (37) | – | – |
| Paid work productivity loss, n (%) | – | – | 16 (9) | 20 (10) |
| Predominantly manual profession†, n (%) | 1 (3) | 10 (7) | 7 (4) | 19 (9) |
Numbers represent mean (standard deviation) unless otherwise specified.
*Median (IQR).
†Defined as a score of 5 or 6 on the scale by de Zwart et al.26
§Defined as having completed university level education
ACR, American College of Rheumatology; AUSCAN, Australian Canadian Osteoarthritis Hand Index; BMI, body mass index; HADS, Hospital Anxiety and Depression Scale; KL, Kellgren-Lawrence; OA, osteoarthritis.
Unpaid work
All 381 patients reported unpaid work in the last 2 weeks, and they spent a median of 44 hours (30–64) on various types of unpaid work (table 4). The necessity of unpaid work tasks being replaced by others was reported by 171 out of 381 patients (45%), with a median of 3 hours replaced (2–7). Any unpaid work hinder due to hand OA was perceived by 221 out of 381 patients (58%). The category of doing groceries provided the highest number of patients experiencing hinder (155 out of 381 patients (41%)) (table 4).
Table 4.
Outcomes of the Health and Labour Questionnaire for all patients (N=381), concerning unpaid work in the last 2 weeks
| Activities | Hours performed | Perceived hinder due to hand OA, n (%) |
Patients needing replacement, n (%) | Hours replaced in case of replacement |
| Total | 44 (30–64) | 297 (78%) | 171 (45%) | 3 (2–7) |
| Housekeeping | 28 (16–40) | 271 (72%) | ||
| Groceries | 8 (4–10) | 216 (57%) | ||
| Chores | 4 (0–10) | 210 (55%) | ||
| Activities with own children | 2 (0–8) | 80 (31%) |
Numbers represent median (IQR) unless specified otherwise.
OA, osteoarthritis.
We compared our patients with unpaid work replacement by others due to hand OA (n=171, 45%), with those without any replacement (n=210, 55%). This showed that patients with unpaid work replacement statistically significantly were more often female (p=0.02) and had a higher body mass index (p<0.01) (table 3).
Societal costs of hand OA
Four patients had missing data on total paid work costs. Over the total cohort (N=381), a mean of €49 (95% CI 16 to 82) per 2 weeks per patient with hand OA was lost due to hand OA absenteeism from work (table 5). This can be extrapolated to €1284 (95% CI 426 to 2142) per patient per year (figure 1). Mean costs per patient due to unproductiveness at work (defined in the HLQ as hours needed to catch up with lost productivity at work) was estimated to be €12 per patient (95% CI 6 to 18) per 2 weeks, or €313 (95% CI 168 to 458) per year. The mean estimated costs of paid work productivity loss per patient (sum of the costs of absenteeism and unproductive hours at work) was €61 (95% CI 27 to 96) per 2 weeks.
Table 5.
Societal costs of paid and unpaid work due to hand OA (€)
| Cause of costs | All patients (N=381) | Patients with paid work (n=181) | Patients under 65 years of age (n=263) |
| Absenteeism | |||
| Mean costs per 2 weeks | 45 (13 to 78) | 96 (28 to 163) | 72 (24 to 120) |
| Mean costs per year | 1186 (348 to 2024) | 2496 (738 to 4253) | 1865 (622 to 3108) |
| Median costs per 2 weeks only for patients generating any costs* (amount of patients) | 1229 (623 to 2567)* (n=11) | 1229 (623 to 2567)* (n=11) | 1229 (623 to 2567)* (n=11) |
| Unproductive hours at paid work | |||
| Mean costs per 2 weeks | 11 (6 to 16) | 23 (12 to 33) | 16 (8 to 23) |
| Mean costs per year | 282 (150 to 415) | 594 (320 to 868) | 409 (219 to 600) |
| Median costs per 2 weeks only for patients generating any costs* (€) (amount of patients) | 126 (61 to 186)* (n=28) | 126 (61 to 186)* (n=28) | 126 (61 to 186)* (n=28) |
| Paid work productivity loss (=absenteeism+unproductive hours at work) | |||
| Mean costs per 2 weeks | 56 (23 to 90) | 119 (49 to 188) | 87 (38 to 136) |
| Mean costs per year | 1470 (600 to 2342) | 3096 (1278 to 914) | 2279 (991 to 3566) |
| Median costs per 2 weeks only for patients generating any costs* (€) (amount of patients) | 186 (66 to 619)* (n=36) | 186 (66 to 619)* (n=36) | 186 (70 to 742)* (n=36) |
| Total unpaid work replacement by others | |||
| Mean costs per 2 weeks | 33 (27 to 40) | 30 (17 to 41) | 33 (24 to 43) |
| Mean costs per year | 853 (669 to 1038) | 754 (443 to 1064) | 868 (626 to 1109) |
| Median costs per 2 weeks only for patients generating any costs* (€) (amount of patients) | 50 (25 to 88)* (n=170) | 38 (25 to 88)* (n=75) | 38 (28 to 50)* (n=116) |
| Total paid and unpaid work productivity loss | |||
| Mean costs per 2 weeks | 90 (56 to 125) | 148 (75 to 220) | 121 (70 to 172) |
| Mean costs per year | 2452 (1528 to 3377) | 3844 (1964 to 5724) | 3142 (1813 to 4471) |
| Median costs per 2 weeks only for patients generating any costs* (€) (amount of patients) | 63 (38 to 125)* (n=186) | 38 (25 to 50)* (n=91) | 88 (28 to 187)* (n=130) |
Numbers represent mean (95% CI).
*Median (IQR).
Figure 1.
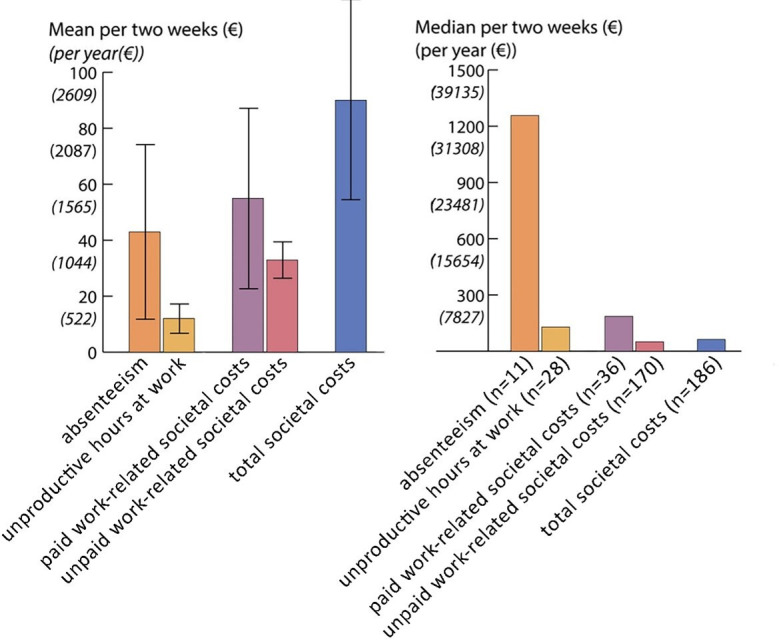
Left: societal hand osteoarthritis-related costs per patient in our cohort, with 95% confidence interval. Right: median societal costs per patient for those having costs larger than zero on the concerning outcome.
Costs of unpaid work replacement were present for 171/381 patients (45%), for whom mean costs were €33 (95% CI 27 to 40) for the total cohort (table 5 and figure 1) per 2 weeks. Mean societal costs of paid and unpaid work per 2 weeks for all 381 patients were €94 (95% CI 59 to 130). This can be extrapolated to €2452 (95% CI 1528 to 3377) per year. Of all hand OA work-related costs estimated by the HLQ, 48% was due to absenteeism, 13% due to unproductive hours at paid work and 39% due to unpaid work replacement. For patients having paid work, mean total societal costs were €148 (95% CI 75 to 220) per 2 weeks or €3844 (95% CI 1964 to 5724) per year. Assessing solely patients that had any paid or unpaid work productivity loss (n=188), mean total costs were €63 (95% CI 38 to 125) per patient per 2 weeks (table 5) or €1630 (95% CI 717 to 3261) per year. Analyses limited to the subgroup with paid work (n=181) revealed that mean costs per patient were €96 (95% CI 28 to 163) per 2 weeks for absenteeism and €23 (95% CI 12 to 33) for unproductive hours at work (table 5, figure 1). Mean unpaid work replacement costs in this group were €30 (95% CI 17 to 41). Investigating solely those under 65 years of age (n=263, online supplemental appendix 3), we found higher mean hours of productivity loss (3.7 (SD 14.4) in 2 weeks), and higher mean associated costs (€121 (95% CI €70 to 172) in 2 weeks) compared with our complete study population.
rmdopen-2022-002367supp003.pdf (91.8KB, pdf)
Work and salary comparison with the general Dutch population
Full work disability due to hand OA was reported by 16 patients (4.4% of all 360 patients aged 15–75 years, 6.1% of 263 patients below Dutch retiring age), and full work disability due to any cause was reported by 24 patients (6.7% of all patients 15–75 years, 9.1% of those below retiring age). This is higher than the all-cause full work disability number in The Netherlands, which has been stable over the years around 6.3% of those aged 15–75.32 33 Absenteeism due to hand OA composed 5.6% of all hours worked in our cohort, which is similar to the mean absenteeism due to any disease in the Dutch population aged 55–65 in 2013 (5.2%).34
Out of 181 patients with paid work, 109 provided their self-reported net salary, which was a mean of €14 (SD 12) per hour. This is 14% lower than the mean estimated hourly salary in the general Dutch population with similar age, sex and working hours (mean (95% CI) €17.16 17 28 Mean weekly hours worked per person was similar for the patients with hand OA and the general Dutch working population in 2013 adjusted for age and sex of our cohort (25.9 (SD 11.8) vs 25.8).35 36 Educational level did not differ between our cohort and the general Dutch population aged 55–65 in 2013 (both 27% high education).36
Based on the self-reported salary information, patients with paid work earned an estimated mean salary of €19 746 (95% CI 10872 to 25599). This is approximately 13% lower than estimated for the general Dutch population with the same working hours, education level and sex as our cohort (€22770 (21041;24499). It is approximately 50% of the average net yearly salary for Dutch persons aged 55–65 years in 2019 (€39800).28
Discussion
In this study on the paid and unpaid work-related disease burden experienced by patients with hand OA, we found that hand OA is associated with substantial paid and unpaid work restrictions, productivity loss (due to absenteeism, unproductive hours at paid work and replacement of unpaid work) and related societal costs associated with productivity loss.
Previous studies concerning other rheumatic and musculoskeletal diseases than hand OA showed outcomes of evident absenteeism, presenteeism and associated costs, which is in line with our study.5 10 37 A Canadian study investigated presenteeism (defined in the study as productivity loss while at work), in 250 patients having paid work and OA (without specifying which joint was affected) or rheumatoid arthritis.10 Four different questionnaires were used. Mean lost hours per 2 weeks due to unproductiveness at work ranged from 1.6 (HLQ) to 14.2 (Work Productivity and Impairment questionnaire, WPAI) hours depending on the questionnaire used, which is higher than the 0.7 (HLQ) hours in our cohort. Related estimated costs were therefore also higher, ranging from €26 (HLQ) to €245 (WPAI) adjusted for 2019 price levels, vs €23 in our study. These outcomes support the association we found between hand OA and impairment in paid work participation but also imply dependence of outcomes on the measurement instrument used. Furthermore, the difference in presenteeism and societal costs between our study and this Canadian study might be explained by the latter investigating different rheumatic and musculoskeletal diseases than our study. Another study assessed 233 Japanese patients with self-reported OA in any joint, of which 27% had hand OA, and paid work using the WPAI.37 The number of patients reporting any absenteeism due to OA was in line with our cohort (both 11% of all working patients). However, presenteeism (defined as a score of worse than 0 on a Visual Analogue Scale for impairment at paid work) was more frequent than in our cohort, being 71% of all patients and 68% of patients with hand OA, vs 15% of working patients in our cohort. The difference could be explained in two ways. First, the HLQ we used showed to be more conservative than the WPAI in estimating working hours lost due to presenteeism.10 Second, there are possibly large differences in organisational culture at work between Japan and The Netherlands, leading to different work consequences of illness.
In this study, we found impaired unpaid work participation in hand OA. This is in line with studies concerning other rheumatic and musculoskeletal diseases than hand OA, being ankylosing spondylitis and rheumatoid arthritis.5 38 However, the Dutch patients with ankylosing spondylitis needed more hours of replacement per patient than in our study, and relatively more Finnish patients with rheumatoid arthritis experienced household activity hinder or needed assistance for these activities. This discrepancy might be due to differences in disease burden from the underlying diseases. Whether differences in gender and age between the groups could explain the difference in not clear. These evident unpaid work impairment outcomes indicate further attention for adequate household support for hand OA.
We found unpaid work productivity loss being more common in our cohort than paid work productivity loss (75 (41%) vs 35 (19%) out of 181), which might be due to several reasons. First, absenteeism is low (13 patients), possibly due to the fact that patients with severe hand OA experience paid work restrictions and retire earlier than those without hand OA, thus evading absenteeism. Second, patients experiencing hand complaints might switch to an occupation that involves less hand labour, preventing hand OA absenteeism. For these reasons, our results may underestimate the true association of hand OA with paid work impairment. A third reason for this relatively high unpaid work productivity loss is that household activities are often physically heavy,39 while paid work in our cohort was seldom predominantly physical (13 patients, 9%). Finally, it could possible that patients prefer household activity replacement over absenteeism or unproductive hours at work in case of reduced physical capacity due to hand OA. This might be caused by social expectations or risk of occupation loss. Although productivity loss was more prevalent for unpaid work than for paid work, the mean associated costs were lower for unpaid work. This discrepancy can be explained by the replacement costs per hour in The Netherlands being lower than the societal costs per hour of most paid work.28 30
Our study has several strengths. It is the first to our knowledge that investigates paid and unpaid work productivity loss, hinder, associated costs and income loss in patients with hand OA specifically and provides extensive information on these outcomes. Also, it has a large study group, likely containing most hand OA disease stages except for the earliest. Furthermore, we performed a separate analysis for patients below the Dutch state pension age (online supplemental appendix 3), which provides information concerning specifically patients of working age. Besides these strengths, our study also has some limitations. First, the self-reported data are prone to response biases, such as recall bias.40 However, as questions concerned a short and recent period, this effect should be limited. Second, the self-reported data are also prone to dependence on the method of quantification. Zhang et al10 demonstrated this by finding large differences in unproductive hours at paid work and associated costs between different questionnaires for the same patient group. However, the outcomes of unproductive hours and associated societal costs provided by the HLQ showed in this study to be more conservative than the estimates provided by the other questionnaires. Therefore, these outcomes would probably be even higher using another questionnaire than the HLQ. Third, the generalisation of hours and cost estimates is limited. As different countries have different cultures and social welfare systems,41 consequences of performing no or less work differ between countries. Salaries also differ between countries,42 which means that associated societal costs of hand OA are likely to differ as well. Fourth, the separate analysis of patients below Dutch retiring age might not be fully accurate, as the actual retiring age might be earlier than 65 years of age for some patients, which is possible in the Dutch system. This might especially be the case if these patients experience paid work hinder due to disease such as hand OA.
In conclusion, hand OA is associated with substantial impairment in paid and unpaid work participation, which translates into substantial societal costs. This highlights the social and economic importance of the development of adequate hand OA treatments. It also highlights the importance of investigating work impairment experienced by patients with hand OA visiting the outpatient clinic for potentially more tailored treatment.
Acknowledgments
We thank the patients of the HOSTAS cohort for participation in this study and research nurses B. van Schie-Geyer, A. Wongsodihardjo and M. Janson, data managers J. van Krol-Berkel and C. Kromme and technicians in the Radiology Department of the LUMC for support in data collection.
Footnotes
Twitter: @fritsrosendaal, @OAKloppenburg
Correction notice: This article has been corrected since it was first published online. The author names Sietse E S Terpstra, Lotte A. van de Stadt and Frits R. Rosendaal have been updated.
Contributors: All authors contributed to the planning, conduct and reporting of the work described in the manuscript. S. Terpstra is the guarantor of this manuscript.
Funding: The HOSTAS study was supported by a grant from the Dutch Arthritis Foundation, which had no involvement in the study design, collection, analysis and interpretation of the data, in writing the manuscript or in the decision to submit the manuscript for publication.
Competing interests: AB received a research grant from Abbvie and consultancy fees to her department from Novartis, Lilly, Galapagos and Abbvie. MK received grants/research support for the submitted work, all paid to the institution.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. However, some aspects of the data can be shared on reasonable request to the corresponding author.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
This study involves human participants and was approved by Leiden University Medical Center Ethical Committee (number P09.004). Written informed consent was obtained from all participants. The participants gave informed consent to participate in the study before taking part.
References
- 1.Safiri S, Kolahi A-A, Smith E, et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis 2020;79:819–28. 10.1136/annrheumdis-2019-216515 [DOI] [PubMed] [Google Scholar]
- 2.Kwok WY, Vliet Vlieland TPM, Rosendaal FR, et al. Limitations in daily activities are the major determinant of reduced health-related quality of life in patients with hand osteoarthritis. Ann Rheum Dis 2011;70:334–6. 10.1136/ard.2010.133603 [DOI] [PubMed] [Google Scholar]
- 3.WHO . International classification of functioning, disability and health (ICF), 2021. Available: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health
- 4.Tenti S, Ferretti F, Gusinu R, et al. Impact of thumb osteoarthritis on pain, function, and quality of life: a comparative study between erosive and non-erosive hand osteoarthritis. Clin Rheumatol 2020;39:2195–206. 10.1007/s10067-020-04982-z [DOI] [PubMed] [Google Scholar]
- 5.Boonen A, Brinkhuizen T, Landewé R, et al. Impact of ankylosing spondylitis on sick leave, presenteeism and unpaid productivity, and estimation of the societal cost. Ann Rheum Dis 2010;69:1123–8. 10.1136/ard.2009.116764 [DOI] [PubMed] [Google Scholar]
- 6.Muchmore L, Lynch WD, Gardner HH, et al. Prevalence of arthritis and associated joint disorders in an employed population and the associated healthcare, sick leave, disability, and workers' compensation benefits cost and productivity loss of employers. J Occup Environ Med 2003;45:369–78. 10.1097/01.jom.0000063621.37065.26 [DOI] [PubMed] [Google Scholar]
- 7.Kingsbury SR, Gross HJ, Isherwood G, et al. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatology 2014;53:937–47. 10.1093/rheumatology/ket463 [DOI] [PubMed] [Google Scholar]
- 8.Kjeken I, Dagfinrud H, Slatkowsky-Christensen B, et al. Activity limitations and participation restrictions in women with hand osteoarthritis: patients' descriptions and associations between dimensions of functioning. Ann Rheum Dis 2005;64:1633–8. 10.1136/ard.2004.034900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laires PA, Canhão H, Rodrigues AM, et al. The impact of osteoarthritis on early exit from work: results from a population-based study. BMC Public Health 2018;18:472. 10.1186/s12889-018-5381-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang W, Gignac MAM, Beaton D, et al. Productivity loss due to presenteeism among patients with arthritis: estimates from 4 instruments. J Rheumatol 2010;37:1805–14. 10.3899/jrheum.100123 [DOI] [PubMed] [Google Scholar]
- 11.United States Bone and Joint Initiative . The burden of musculoskeletal diseases in the United States (BMUS) fourth edition, 2019. Available: https://www.boneandjointburden.org/fourth-edition/iiia40/economic-burden-aorc
- 12.Leardini G, Salaffi F, Caporali R, et al. Direct and indirect costs of osteoarthritis of the knee. Clin Exp Rheumatol 2004;22:699–706. [PubMed] [Google Scholar]
- 13.Kloppenburg M, Kwok W-Y. Hand osteoarthritis--a heterogeneous disorder. Nat Rev Rheumatol 2011;8:22–31. 10.1038/nrrheum.2011.170 [DOI] [PubMed] [Google Scholar]
- 14.Haugen IK, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham osteoarthritis study. Ann Rheum Dis 2011;70:1581–6. 10.1136/ard.2011.150078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Damman W, Liu R, Kroon FPB, et al. Do comorbidities play a role in hand osteoarthritis disease burden? data from the hand osteoarthritis in secondary care cohort. J Rheumatol 2019;46:1659–66. 10.3899/jrheum.170208.C1 [DOI] [PubMed] [Google Scholar]
- 16.Hakkaart-van Roijen L, Essink-Bot MLE. Manual health and labour questionnaire, 2000. Available: http://hdl.handle.net/1765/1313
- 17.Altman R, Alarcón G, Appelrouth D, et al. The American College of rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthritis Rheum 1990;33:1601–10. 10.1002/art.1780331101 [DOI] [PubMed] [Google Scholar]
- 18.Bellamy N, Campbell J, Haraoui B, et al. Dimensionality and clinical importance of pain and disability in hand osteoarthritis: development of the Australian/Canadian (AUSCAN) osteoarthritis hand index. Osteoarthritis Cartilage 2002;10:855–62. 10.1053/joca.2002.0837 [DOI] [PubMed] [Google Scholar]
- 19.KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verbruggen G, Veys EM. Numerical scoring systems for the anatomic evolution of osteoarthritis of the finger joints. Arthritis Rheum 1996;39:308–20. 10.1002/art.1780390221 [DOI] [PubMed] [Google Scholar]
- 21.Kortekaas MC, Kwok W-Y, Reijnierse M, et al. In erosive hand osteoarthritis more inflammatory signs on ultrasound are found than in the rest of hand osteoarthritis. Ann Rheum Dis 2013;72:930–4. 10.1136/annrheumdis-2012-201458 [DOI] [PubMed] [Google Scholar]
- 22.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 24.Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychol Med 1997;27:363–70. 10.1017/S0033291796004382 [DOI] [PubMed] [Google Scholar]
- 25.Axford J, Butt A, Heron C, et al. Prevalence of anxiety and depression in osteoarthritis: use of the hospital anxiety and depression scale as a screening tool. Clin Rheumatol 2010;29:1277–83. 10.1007/s10067-010-1547-7 [DOI] [PubMed] [Google Scholar]
- 26.de Zwart BC, Broersen JP, van der Beek AJ, et al. Occupational classification according to work demands: an evaluation study. Int J Occup Med Environ Health 1997;10:283–95. [PubMed] [Google Scholar]
- 27.Cb voor de statistiek. consumer prices. statistics Netherlands. Available: https://www.cbs.nl/en-gb/figures/detail/83131eng
- 28.Lonen en loonkosten . De arbeidsmarkt in cijfers 2019, 2019. Available: https://longreads.cbs.nl/dearbeidsmarktincijfers-2019/lonen-en-loonkosten/
- 29.van den Hout WB. The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis 2010;69 Suppl 1:i89–91. 10.1136/ard.2009.117150 [DOI] [PubMed] [Google Scholar]
- 30.Uurtarief.tips . Tarief huishoudelijke hulp. Vergelijk uurloon en prijzen. Available: https://uurtarief.tips/nl/zzp/schoonmaak/tarief-huishoudelijke-hulp
- 31.Convert week to year - Conversion of Measurement Units. Available: https://www.convertunits.com/from/week/to/year
- 32.Huidige situatie incidentie arbeidsongeschiktheid naar leeftijd en geslacht. Available: https://www.volksgezondheidenzorg.info/onderwerp/arbeidsongeschiktheid/cijfers-context/huidige-situatie#node-incidentie-arbeidsongeschiktheid-naar-leeftijd-en-geslacht-1
- 33.Centraal bureau voor Statistiek – Arbeidsongeschiktheid: trends. Available: https://www.volksgezondheidenzorg.info/onderwerp/arbeidsongeschiktheid/cijfers-context/trends#!node-trend-arbeidsongeschiktheid
- 34.CBS . Ziekteverzuim. Available: https://www.cbs.nl/nl-nl/visualisaties/dashboard-arbeidsmarkt/werkenden/ziekteverzuim
- 35.Statline: werkuren Nederland. Available: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82647NED/table?fromstatweb
- 36.Statline: Bevolking; onderwijsniveau; geslacht, leeftijd en migratieachtergrond, 2021. Available: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82275NED/table?fromstatweb
- 37.Nakata K, Tsuji T, Vietri J, et al. Work impairment, osteoarthritis, and health-related quality of life among employees in Japan. Health Qual Life Outcomes 2018;16:64. 10.1186/s12955-018-0896-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leino M, Tuominen S, Pirilä L, et al. Effects of rheumatoid arthritis on household chores and leisure-time activities. Rheumatol Int 2015;35:1881–8. 10.1007/s00296-015-3313-2 [DOI] [PubMed] [Google Scholar]
- 39.Timmermans EJ, de Koning EJ, van Schoor NM, et al. Within-Person pain variability and physical activity in older adults with osteoarthritis from six European countries. BMC Musculoskelet Disord 2019;20:12. 10.1186/s12891-018-2392-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Furnham A. Response bias, social desirability and dissimulation. Pers Individ Dif 1986;7:385–400. 10.1016/0191-8869(86)90014-0 [DOI] [Google Scholar]
- 41.Heymann J, Rho H, Schmitt J. Contagion nation: a comparison of paid sick day policies in 22 countries. center for economic and policy research (CEPR), CEPR reports and issue Briefs 2009.
- 42.PayScale . Search salaries by country. Available: https://www.payscale.com/research/Country
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2022-002367supp001.pdf (86.4KB, pdf)
rmdopen-2022-002367supp002.pdf (93.4KB, pdf)
rmdopen-2022-002367supp003.pdf (91.8KB, pdf)
Data Availability Statement
No data are available. The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. However, some aspects of the data can be shared on reasonable request to the corresponding author.


