ABSTRACT
Older adults may experience a number of physiological changes that influence how acute pain is perceived, diagnosed and managed by healthcare professionals. Understanding these differences enables the identification, assessment and treatment of acute pain in older adults. Combining careful selection of pain medications with appropriate titration and monitoring allows the analgesic needs of this group to be met.
KEYWORDS: analgesia in older patients, pain assessment scales, polypharmacy, Abbey Pain Score, acute pain
Key points
Both quantitative and qualitative methods of assessing pain are helpful in determining the choice of analgesia in the older adults.
Multiple factors determine the choice of analgesia prescribed for older adults including physiological changes, psychological issues, existing medications and cognitive function.
Under- or overtreatment of pain can have significant consequences, such as delirium and falls, so this must be considered when prescribing for older adults with acute pain.
Older adults should be given the lowest analgesic dose for the shortest possible time to adequately manage their pain: starting low and titrated cautiously.
Formally reassess the pain in older people to help guide the effectiveness of both the initial and ongoing treatments.
Introduction
Pain is the subjective experience of noxious stimuli and, in its acute form, is defined as pain lasting up to 3 months.1 Older adults may experience several physiological changes that influence how acute pain is experienced, as well as how it is diagnosed and managed by healthcare professionals. Acute pain is highly prevalent for all patients seen in both primary and secondary care, with estimates suggesting that more than 50% of hospital inpatients experience significant pain during their hospitalisation and that the prevalence of pain has been found to increase with age, particularly for those with a history of musculoskeletal problems and depression.2 This article aims to outline the age-related changes in physiology relating to pain that may alter the way pain is perceived for older adults, and outline the adjustments required when assessing and treating this pain.
Changes in ageing regarding nociception and perception of pain
There are a number of physiological changes that take place in the older adult that can affect their experience of pain. Nerve fibres, particularly the myelinated A-delta nerve fibres that produce the sensation of sharp localised pain decrease with age.1 Neurons in older adults do not regenerate and are replaced by proliferating non-neuronal glial cells reducing the response to pain. Further changes, including the loss of proprioception and altered peripheral nerve conductivity, increase the risk of injury leading to a higher likelihood of developing pain.1,3
Older adults are also more likely to experience multi-morbidity leading to an accumulation of potentially painful diseases as the prevalence of certain conditions linked to pain increases with age. These include conditions such as Parkinson's disease, post-stroke pain, degenerative spinal disease, arthritis and diabetic neuropathy.3 Older adults are also more likely to develop cognitive impairment, including dementia, which may result in an altered sensation of pain.4
Impact of pain in older adults
The impact of pain on an individual is wide ranging and is especially so in the older adult. Pain can result in functional impairment, sleep disturbance, reduced socialisation, depression, reduced mobility, and impaired or slowed rehabilitation. Studies have shown a 70%–80% reduction in the ability of older adults to perform activities of daily living for those with pain compared with those without pain, as well as decreased gait speed, weaker grip strength and decreased self-reported physical ability.5 Older adults, especially those with frailty, may have reduced functional reserves meaning that pain-related impairments may have a more profound impact on mobility, cognition and independence.
Assessing pain in older adults
Pain is a subjective phenomenon and cannot be directly measured. As a result, self-reporting pain measurement tools are used to quantify pain, including simple verbal rating scales, visual analogue scales and pictorial pain scales as well as more complex assessment tools such as the McGill Pain Questionnaire or the Brief Pain Inventory.6,7
It is important that pain is proactively explored with patients as they, and their carers, may underestimate pain by attributing it to the ‘normal’ ageing process, leading to under-reporting and, therefore, under-treatment. Patients and carers may also be concerned about the side effects or polypharmacy associated with analgesia and hence avoid reporting pain to healthcare professionals.3,8 It should also be recognised that the majority of older adults who experience pain will experience pain at multiple sites, and this must be considered when assessing pain. In one study, a fifth of older adults over 65 years old reported pain at four or more sites.5
The most valid assessment of pain is self-reported, although this can be influenced by numerous factors (including mood, lethargy and sedating medications).9,10 It is also recognised that documentation of pain during inpatient admissions can be poor and higher pain scores may not necessarily result in the administration of more analgesic medications.11 In older adults, the assessment of pain may be further complicated as a consequence of cognitive impairment (such as dementia or delirium) or communication issues (such as aphasia), which may limit the reporting of pain and reduce the accuracy of these tools. For these patients, pain may be unreported and under-recognised. As a result, observational pain assessment tools have been devised that look at non-verbal behaviour (such as facial expression and changes in body language) combined with physiological changes associated with pain (such as tachycardia) to help elicit the level of pain. An example of such a tool is the Abbey Pain Scale (Fig 1) designed to measure pain in people with dementia who cannot verbalise.12
Fig 1.
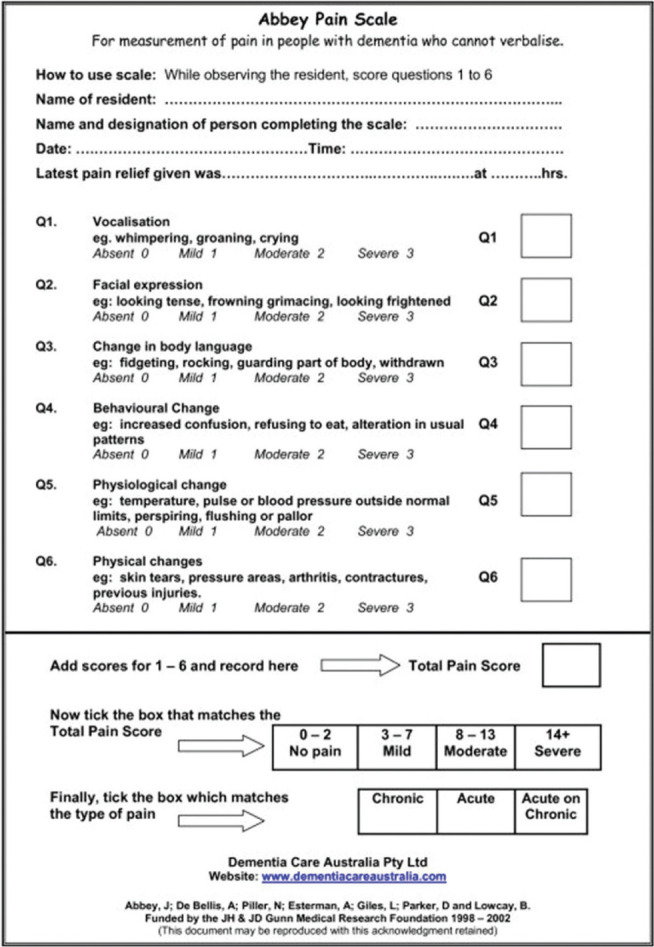
The Abbey Pain Scale. Designed to assess pain for patients who cannot verbalise their pain. Reproduced with permission from Abbey J, De Bellis A, Piller N et al. Abbey Pain Scale. Funded by the JH & JD Gunn Medical Research Foundation 1998–2002.
Effects of analgesia in the older adult
Older adults may experience the effects of analgesia differently to their younger counterparts for multiple reasons. Firstly, there are a number of age-related metabolic changes that alter the pharmacokinetics of analgesic medications. In the older adult, there is a decrease in total body water, meaning that water soluble medications (such as morphine) will have a smaller volume of distribution. There is also a decrease in lean muscle mass and an increase in body fat meaning that medications will have a smaller muscle volume of distribution and lipid soluble medications will accumulate. Further physiological changes include a reduction in hepatic and renal size, and blood flow, altering the potency, duration and clearance of analgesic medications.
Older adults are also more likely to experience multi-morbidity and polypharmacy. This may alter the impact of medications prescribed for pain due to the increased risk of drug–drug interactions and side effects.13–15 In clinical practice, this necessitates careful drug choice, dose adjustments and close monitoring of the effects of analgesics when they are prescribed for older adults. Specific impacts for the different categories of analgesia are outlined in Table 1.1–3,16,17
Table 1.
Specific impacts for different categories of analgesia
| Class of drug | Mechanism of action and indication | Common side effects | Considerations in the older person |
|---|---|---|---|
| Paracetamol (acetaminophen) | Inhibits prostaglandin synthesis. | Generally well tolerated with minimal side effects. | Renal impairment: in the older person there is glomerulosclerosis and renal cortical atrophy, consequently, there is a decrease in the glomerular filtration rate (GFR) and a decreased clearance of medications and a reduced renal reserve to recover from nephrotoxic medications. Hepatic impairment: older adults have fewer hepatocytes so there is a decreased hepatic metabolism. |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | Inhibits cyclooxygenase enzymes. | Gastrointestinal bleeding. Asthma. Renal failure. |
Generally avoided in older people who are frail. If used, a short course with a definite stop date is advised. Renal impairment: reduced renal reserves means a higher risk of renal injury; in addition, older adults may be taking a number of other potentially nephrotoxic medications (such as diuretics and ACE inhibitors). The addition of NSAIDs can, therefore, exacerbate existing kidney damage. Gastrointestinal bleeds: NSAIDs can cause gastrointestinal mucosal injury resulting in gastrointestinal bleeding and/or gastritis. Thrombotic events: the risk of thrombotic events is increased in older adults due to the inhibition of substances such as thromboxanae A2, which is an anti-throbotic. |
| Opioids | Used in conjunction with other analgesia such as paracetamol when these alone have been ineffective. Moderate pain: codeine phosphate and tramadol. Moderate to severe pain: morphine, oxycodone and hydromorphine (causes less pruritus compared with other opioids). Patient-controlled analgesia (PCA) in those who are cognitively intact. |
Confusion. Constipation. Respiratory depression. |
Certain metabolites within opiates can cross the blood brain barrier resulting in delirium (especially for those with an existing vulnerable brain), respiratory depression and falls. This occurs to a greater extent in older adults. Older adults are more prone to constipation (primarily due to slowed gut transit and medications), which can be exacerbated by opiates. The majority of opioids are renally excreted, therefore, renal changes in the older adult (such as a reduced GFR) can lead to an accumulation of opioids. |
| Topical analgesia | Capsasin: causes a brief initial sensitisation followed by a prolonged desensitisation of the local pain nerves. Topical NSAIDS eg diclofenac. |
Muscle spasms. Palpitations. Peripheral oedema. |
The side effects of these medications include localised irritation, erythema and swelling. Topical NSAIDs can cause complications, such as stomach ulcers |
| Anticonvulsants | Gabapentin and pregabalin: blocks voltage-gated calcium channels. Carbamazepine: blocks voltage-gated sodium channels. All effective for neuropathic pain. |
Arthralgia. Confusion. Headache. Drowsiness. Dizziness. Dry mouth. |
Through their effects on the central nervous system, anticonvulsants can cause oversedation. There are a number of consequences of this, such as falls and cognitive impairment. |
| Tricyclic antidepressants (TCAs) | Amitriptyline: blocks noradrenaline and serotonin transporters. Effective for neuropathic pain. |
Cardiac arrhythmias. Drowsiness. |
Certain considerations in older adults include anticholinergic effects, such as urinary retention, blurred vision and a dry mouth. TCAs can also cause cardiac arrhythmias in various ways, such as blocking noradrenaline reuptake. TCAs can increase intraocular pressure and cause narrow angle glaucoma |
| Ketamine | Blocks the N-methyl-D-aspartate (NMDA) receptor. | Confusion. Hallucinations. |
Ketamine can cause a number of side effects (such as delirium and night terrors) and is rarely used for older adults. |
| Lignocaine | Hyperpolarisation and decreased excitability of postsynaptic spinal dorsal horn neurones. | Anxiety. Atrioventricular block. |
Lignocaine can cause allergic reactions, such as anaphylaxis, nausea, vomiting and changes in heart rate. |
| Regional anaesthesia | Spinal anaesthesia. Epidural anaesthesia. Nerve blocks along the distribution of the nerve. Helpful perioperatively. |
Spinal haematoma. Headache. Infection. Nerve block: bleeding and itching. |
Regional anaesthesia can be anatomically challenging to perform in the older adult due to problems such as degenerative bone disease and vertebral joint disease. Both the intervertebral and epidural spaces decrease with ageing along with calcification of the ligamentum flavum. |
| Duloxetine | This inhibits the reuptake of serotonin and noradrenaline in the central nervous system. Helpful in the treatment of neuropathic pain, such as diabetic neuropathy. |
Headache. Diarrhoea. Dry mouth. Insomnia. |
Duloxetine is to be used cautiously in the older person as it can cause a number of problems (such as drug-induced movement disorders, confusion and hypertension) due to their noradrenergic effects. |
Treatment of pain in older patients
There are many non-pharmacological treatment modalities for acute pain management including the application of heat or ice, massage therapy, physiotherapy, and alternative therapies (such as acupuncture). In view of the issues outlined earlier regarding the challenges that prescribing medications for older adults present, non-pharmacological treatments tend to have fewer side effects and should generally be considered as a first-line therapy. However, these measures may not be sufficient, and so, analgesia often forms the cornerstones of treatment options for pain.2 The selection of analgesia is underpinned by the principles outlined in the World Health Organization (WHO) pain ladder (Fig 2).18
Fig 2.
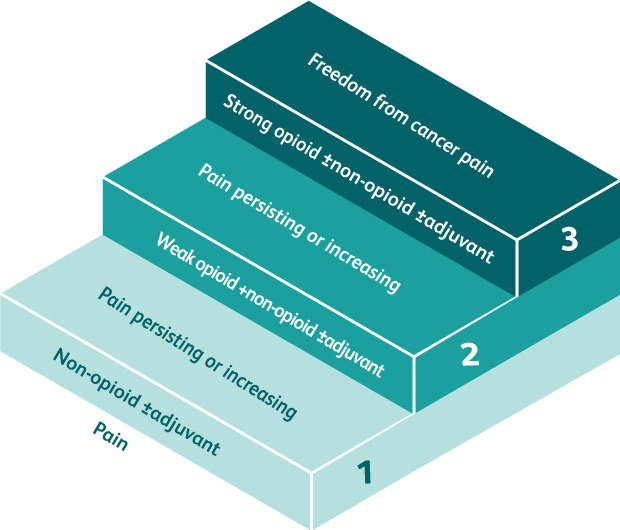
The World Health Organization pain ladder. Adapted with permission from World Health Organization. Cancer pain relief. WHO, 1986:19.
However, there are a number of considerations that are needed when analgesia is prescribed for the older person (Table 1).1–3 Specific regional forms of analgesia may be particularly effective in selective acute settings, such as the use of femoral nerve blocks following a neck of femur fracture. These have the advantage of reducing adverse systemic effects (such as cognitive dysfunction and sedation) but can be more challenging to administer for older adults.1,2 They may also require specialist training to administer and may not always be available.
Conclusion
Providing adequate analgesia for older adults in the acute setting can be challenging as a result of changes to physiology, polypharmacy, multi-morbidity and altered processing of medications combined with under-reporting and under-recognition of pain. Actively asking about pain and incorporating additional methods to accurately assess pain can be important, particularly for those who cannot communicate effectively. Combined with careful selection, titration and monitoring of analgesia, this will allow the analgesic needs of this patient group can be successfully met.
References
- 1.Schofield P. The assessment of pain in older people: UK national guidelines. Age Ageing 2018;47:i1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Behrends M, Rajan J. Acute pain in older adults. recommendations for assessment and treatment. Anesthesiology Clin 2019;37:507–20. [DOI] [PubMed] [Google Scholar]
- 3.Lin RJ, Siegler EL. Acute pain management in older adults. In: Cordts GA, Christo PJ. (eds). Effective treatments for pain in the older patient. Springer, 2019:35–52. [Google Scholar]
- 4.Baluch A, Kaye AD, Scott JT. Pain management in the elderly population: A review. Ochsner J 2010;10:179–87. [PMC free article] [PubMed] [Google Scholar]
- 5.Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the united states: findings from the 2011 national health and aging trends study. Pain 2013;154:10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melzack R. The McGill pain questionnaire: from description to measurement. Anesthesiology 2005;103:199–202. [DOI] [PubMed] [Google Scholar]
- 7.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap 1994;23:129–38. [PubMed] [Google Scholar]
- 8.Rudy TE, Weiner DK. Attitudinal barriers to effective treatment of persistent pain in nursing home residents. J Am Geriatr Soc 2002;50:2035–40. [DOI] [PubMed] [Google Scholar]
- 9.Melzack R, Katz J. Pain measurement in persons in pain. In: Wall PD, Melzack R. (eds). Textbook of pain. London: Churchill Livingstone, 1994. [Google Scholar]
- 10.Peter E, Watt-Watson J. Unrelieved pain: an ethical and epistemological analysis of distrust in patients. Canadian Journal of Research 2002;34:2,65–80. [PubMed] [Google Scholar]
- 11.Watt-Watson J, Stevens B, Garfinkel P, Streiner D, Gallop R. Relationship between nurses' knowledge and pain management outcomes for their postoperative cardiac patients. J Adv Nurs 2001;36:535–45. [DOI] [PubMed] [Google Scholar]
- 12.Gregory J. Assessing pain in patients with cognitive impairment in acute care. Nursing Times 2017;113:10,18–21. [Google Scholar]
- 13.Guy-Alfandary S, Rochon PA, Sternberg SA. Prescribing cascades in older adults. CMAJ 2021;193:E215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turnheim K. When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol 2003;38:843–53. [DOI] [PubMed] [Google Scholar]
- 15.Hein C, Forgues A, Piau A, et al. Impact of polypharmacy on occurrence of delirium in elderly emergency patients. J Am Med Dir Assoc 2014;15:850.e11–5. [DOI] [PubMed] [Google Scholar]
- 16.Mann C, Pouzeratte Y, Eledjam JJ. Postoperative patient-controlled analgesia in the elderly: risks and benefits of epidural versus intravenous administration. Drugs Aging 2003;20:337–45. [DOI] [PubMed] [Google Scholar]
- 17.National Institute for Health and Care Excellence. British National Formulary (BNF). NICE. https://bnf.nice.org.uk [Accessed 20 June 2022]. [Google Scholar]
- 18.World Health Organization. Cancer pain relief. WHO, 1986:19. https://apps.who.int/iris/bitstream/handle/10665/43944/9241561009_eng.pdf [Google Scholar]


