ABSTRACT
Physiological changes that occur during ageing can affect the incidence, experience and treatment of pain in older adults. This article reviews these physiological changes and how they can affect the best approach to management.
KEYWORDS: pain, ageing, neuropathic, nociceptive, pharmacodynamics
Key points
While difficult to estimate, pain prevalence increases with age, with a higher incidence in women and institutionalised patients.
Assessment of pain can be challenging due to cognitive and sensory impairment and under-reporting.
An understanding of the pathophysiology of different pain syndromes can aid analgesic choice.
Changes in body systems resulting from ageing lead to different responses to pain and treatments.
Presence of pain has been shown to have a significant impact and to be associated with negative outcomes.
Introduction
As the population ages, physicians are increasingly likely to be required to manage pain in older adults, particularly as longer life expectancy does not necessarily correspond to an increase in the number of pain-free years. The International Association for the Study of Pain has identified research on pain in relation to ageing as a priority, with the aim of understanding how the ageing process affects pain perception and the treatment options available.1 Achieving adequate pain control is notoriously difficult in older adults, particularly those with multiple health conditions, due to the associated polypharmacy and propensity for side effects. This article examines some of the causes of pain in older adults, the impact of ageing on pain processing and how this affects pain management.
Incidence and prevalence of pain in older adults
Although it is recognised that pain is extremely common in older adults, substantial differences in the populations studied and methods and definitions used in published research make it challenging to compare across studies and determine the definitive prevalence of pain in older people.2 It has consistently been found that institutionalised adults have higher levels of pain than community-dwelling adults, and that raised body mass index, lower levels of education and socioeconomic deprivation are associated with increased rates of pain.3,4 There also appear to be gender differences, with older women consistently having a higher reported prevalence of pain than older men, and also demonstrating less concordance with medications.2
Assessment of pain in older individuals represents a significant challenge for a number of reasons, including cognitive impairment, communication issues (such as aphasia) and sensory impairments, which are more common in older adults, as well as under-reporting, with many feeling that pain is ‘just a normal part of ageing’. However, acute pain is not an inevitable consequence of ageing and is commonly a result of pathology, such as trauma, disease or degeneration.5 This is consistent with research evidence suggesting that pain is both under-reported and under-assessed in older adults, and makes the clinical assessment of pain in this demographic, particularly for patients with cognitive impairment, important.6 As such, there has been significant work into the best assessment tools to use, particularly for those who are unable to verbally express pain, with specific guidelines available.7
Causes of pain in older adults
While the normal ageing processes do not necessarily guarantee pain, older adults are more likely than their younger counterparts to have developed conditions that can lead to pain. Some examples of these conditions are outlined in Table 1, although this is by no means an exhaustive table, and multiple other conditions lead to pain in older adults.5,8–11 The main sites of pain in older adults been found consistently to be the back/hip/knee and other joints.5 Studies have also consistently shown that older adults may experience pain at multiple sites, with one showing that a fifth of adults older than 65 years had pain at four or more sites when thoroughly assessed.2 This information should be taken into account when making a pain assessment, especially with those who are unable to verbalise their pain. Understanding the condition and the type of pain it causes is important as it will guide the selection of appropriate agents for treatment.
Table 1.
Conditions leading to pain in older adults with pathology, type of pain and epidemiology
| Condition | Pathology | Type of pain | Epidemiology |
|---|---|---|---|
| Osteoarthritis | Progressive loss or destruction of articular cartilage leading to inflammation, resulting in impaired joint mobility and progressive pain | Nociceptive and neuropathic | Estimated to affect 50% of adults aged over 65 years5 |
| Post-herpetic neuralgia | Reactivation of varicella-zoster virus in the dorsal root ganglion, causing damage to peripheral and central neurons | Neuropathic | Frequency and severity increases with age; estimated to occur in 30% of those aged over 80 years who have had acute herpes zoster8 |
| Diabetic neuropathy | Hyperglycaemia leading to changes in blood supply of peripheral nerves causing a progressive loss of fibres along the autonomic and somatic divisions9 | Neuropathic | 10%–26% of the diabetic population9 |
| Lower back pain: spondylosis and radiculopathies | Chronic degeneration of articular surfaces leading to inflammation and narrowing that can result in radiculopathy | Nociceptive and neuropathic | Incidence of spondylosis increases with age, with almost all individuals showing spondylosis by the age of 79 years5 |
| Post-stroke pain (PSP) | Central PSP, peripheral neuropathic pain, pain secondary to spasticity, and joint subluxation10 | Nociceptive and neuropathic | 10.6% of ischaemic strokes experience some chronic PSP10 |
| Parkinson's disease | Musculoskeletal (40%–90%); altered processing of the somatosensory information in the basal ganglia results in reduced pain threshold and increased pain sensitivity, ‘off state pain’11 | Nociceptive and neuropathic | 45%–60% in patients with Parkinson's disease, with variations in gender found11 |
Impact of pain
The presence of pain has been shown to be associated with functional impairment, decreased appetite, impaired sleep, depression and social isolation in older adults.5 It has been found that treating depression early reduces the perception of pain, potentially improving quality of life and reducing the need for prescription of significant or prolonged courses of analgesia. Recognising and treating pain is also an important part of the management of depression.12
Changes in pain perception and experience with ageing
Ageing affects the experience of pain in a number of different ways, some of which are not yet fully understood.13 First, ageing leads to presbyalgos, a reduced ability to detect harmful signals related to loss in the structure and function of peripheral and central nervous system pathways implicated in the processing of painful stimuli.5,14 This occurs due to a decrease in the number of delta nerve fibres that detect the signals of sharp localised pain and a proliferation of non-neuronal glial cells replacing pain transmitting neurons. Further changes, including the loss of proprioception and altered peripheral nerve conductivity, increase the risk of injury leading to a higher likelihood of developing pain.3,15
Altered responses to thermal pain have also been shown to occur in the middle insular cortex and the primary somatosensory cortex.13 These changes in pain perception and processing may compromise the protective biological function of pain, placing older adults at an increased risk of injury and potentially delaying the diagnosis of diease.14 A common example of this is that chest pain seems to be a less prominent presenting feature for older adults with myocardial infarction.14
The threshold at which pain is experienced has been shown to increase with age; this finding has been found to be more prominent in women. This means a higher stimulus is required to induce pain and, thus, a reduced sensitivity to mild pain is observed with advancing age, a finding that has been found particularly for thermal pain stimuli.14 Conversely, the maximal intensity of a pain a person is able to tolerate has been found to be either unchanged or reduced with ageing, regardless of the type of pain stimulus.5,14 This might suggest a reduction in the ability to withstand pain at higher intensities, perhaps because endogenous pain inhibitory systems have been found to be less effective.14 Finally, neuroplasticity, the ability to recover from injury and the resolution of pain, appears to be slowed with ageing. Older adults have longer periods of hyperalgesia following painful stimuli.14 Combined with slower healing after injury, this may lead to prolonged periods of discomfort and functional impairment.16
Clearly the changes associated with pain processing in ageing are complex. As pain pathways diminish, it might be expected that patients feel and report less pain, but studies have also shown older adults are less able to tolerate higher intensities of pain and experience a longer period of hyperalgesia.14
Clinical impacts of changes in ageing and implications for pain management
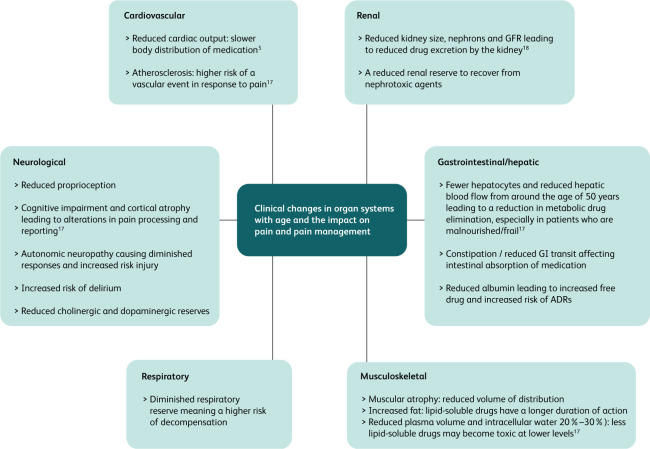
As outlined earlier, there are a number of physiological changes with ageing that alter the perception of pain. The impact of analgesic medications has also been found to be altered in older adults as a result of many of the physiological changes in various body systems (Fig 1).5,17,18 As a result of these changes, drug effects may be blunted, and adverse drug reactions may be more debilitating and occur at an increased frequency. Age-related changes in pharmacodynamics occur at the receptor or signal transduction level and homeostatic mechanisms may be attenuated, with more time being required to regain the steady state.18 There is also a significant heterogeneity of drug response in older adults, meaning the effects can vary vastly between individuals.18 Cautious prescribing is, therefore, required for older adults, with careful choice of analgesic medication and the potential need for lower starting doses, slow titration and careful monitoring for side effects.
Fig 1.
Clinical changes in organ systems with age and the impact on pain and pain management. ADR = adverse drug reaction; GFR = glomerular filtration rate; GI = gastrointestinal.
Conclusion
Changes that occur as part of the ageing process increase the susceptibility to pain, affect the ability to tolerate pain and the capacity to recover from injury when it occurs. This is compounded by the accumulation of multiple potentially pain-causing health conditions, as well as by polypharmacy and altered pharmacodynamics, which may limit treatment options. Management of pain needs to take into consideration the changes that occur in various body systems and the effect this has on the response to treatment including adverse drug reactions. Assessment of pain and its management needs to be individualised as there is a heterogeneity of age-related changes and response to treatments in older adults.
References
- 1.Patel KV, Guralnik JM, Dansie EJ, Turk DC, et al. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain 2013;154:2649–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdulla A, Adams A, Bone M, et al. Guidance on the management of pain in older people. Age Ageing 2013;42:S1–57. [DOI] [PubMed] [Google Scholar]
- 3.Gibson SJ, Lussier D. Prevalence and relevance of pain in older persons. Pain Med 2021;13:S23–6. [DOI] [PubMed] [Google Scholar]
- 4.Lacey RJ, Belcher J, Croft PR. Does life course socio-economic position influence chronic disabling pain in older adults? A general population study. Eur J Public Health 2013;23:534–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones MR, Ehrhardt KP, Ripoll JG, et al. Pain in the elderly. Curr Pain Headache Rep 2016;20:23. [DOI] [PubMed] [Google Scholar]
- 6.Herr KA, Garand L. Assessment and measurement of pain in older adults. Clin Geriatr Med 2001;17:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schofield P. The assessment of pain in older people: UK National Guidelines. Age Ageing 2018;47:i1–i22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mallick-Searle T, Snodgrass B, Brant JM. Postherpetic neuralgia: epidemiology, pathophysiology and pain management pharmacology. J Multidiscip Healthc 2016;9:447–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schreiber AK, Nones CFM, Reis RC, Chicorro JG, Cunha JM. Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes 2015;6:432–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Treister AK, Hatch MN, Cramer SC, Chang EY. Demystifying poststroke pain: from etiology to treatment. PM R 2017;9:63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skogar O, Lokk J. Pain management in patients with Parkinson's disease: challenges and solutions. J Multidiscip Healthc 2016;9:469–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gloth M. Pain management in older adults: prevention and treatment. J Am Geriatr Soc 2001;49:188–99. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez-Roldan AM, Terrasa JL, Sitges C, et al. Age-related changes in pain perception are associated with altered functional connectivity during resting state. Front Aging Neurosci 2020;12:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadjistavropoulos T, Herr K, Prkachin KM, et al. Pain assessment in elderly adults with dementia. Lancet Neurology 2014;13:1216–27. [DOI] [PubMed] [Google Scholar]
- 15.Gagliese L, Melzack R. Age differences in Nociception and pain behaviours in the rat. Neurosci Biobehav Rev 2000;24:843–54. [DOI] [PubMed] [Google Scholar]
- 16.Gerstein AD, Phillips TJ, Rogers GS, Gilchrest BA. Wound healing and aging. Review Dermatol Clin 1993;11:749–57. [PubMed] [Google Scholar]
- 17.Rajan J, Behrends M. Acute pain in older adults: recommendations for assessment and treatment. Anesthesiol Clin 2019;37:507–20. [DOI] [PubMed] [Google Scholar]
- 18.Turnheim K. When drug therapy gets old: Pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol 2003;38:843–53. [DOI] [PubMed] [Google Scholar]