ABSTRACT
Introduction
Breathing pattern disorders (BPDs) are a common cause of chronic breathlessness, including after acute respiratory illnesses such as COVID pneumonia. BPD is however underdiagnosed, partly as a result of difficulty in clinically assessing breathing pattern. The Breathing Pattern Assessment Tool (BPAT) has been validated for use in diagnosing BPD in patients with asthma but to date has not been validated in other diseases.
Methods
Patients undergoing face-to-face review in a post-COVID clinic were assessed by a respiratory physician and specialist respiratory physiotherapist. Assessment included a Dyspnoea-12 (D12) questionnaire to assess breathlessness, physiotherapist assessment of breathing pattern including manual assessment of respiratory motion, and BPAT assessment. The sensitivity and specificity of BPAT for diagnosis of BPD in post-COVID patients was assessed.
Results
BPAT had a sensitivity of 89.5% and specificity of 78.3% for diagnosing BPD in post-COVID breathlessness. Patients with a BPAT score above the diagnostic cut-off had higher levels of breathlessness than those with lower BPAT scores (D12 score mean average 19.4 vs 13.2).
Conclusion
BPAT has high sensitivity and moderate specificity for BPD in patients with long COVID. This would support its use as a screening test in clinic, and as a diagnostic tool for large cohort studies.
KEYWORDS: long COVID, dysfunctional breathing, breathlessness, sequalae, follow-up
Introduction
There is increasing awareness across the field of respiratory medicine of the importance of breathing pattern disorders (BPD) as a cause of chronic breathlessness. In the last 10 years there has been a renewed focus on the classification of BPD, its evidence-based diagnosis and management.1 In clinical practice BPD is usually diagnosed by specialist physiotherapists after clinical assessment of the patient using questionnaires and manual assessment of respiratory motion (MARM) physical examination.2 However, the subjective nature of diagnosis by standard clinical assessment is a limitation, particularly for research studies where objective structured diagnosis of disease is important to ensure reproducibility and translatability of findings. Todd and colleagues have therefore recently developed a structured tool for diagnosis of breathing pattern disorders – the Breathing Pattern Assessment Tool.3 BPAT was developed for diagnosis of BPD in patients with asthma, and validated in this context by Bondarenko and colleagues,4 but to the best of our knowledge has not been validated in other conditions.
Persistent breathlessness is one of the commonest symptoms reported by patients suffering from long COVID.5–7 Many of these patients also report symptoms of autonomic dysfunction and there is increasing interest in the association between autonomic dysfunction and breathing pattern disorders.8,9 Recent reports of long COVID patient cohorts have noted that many of these patients have BPD.7,10 Assessing the prevalence of BPD within these cohorts, however, is difficult without a validated objective diagnostic tool. Our post-COVID service staffing included specialists re-deployed from our severe asthma service and routine patient assessment included use of BPAT. We report here our experience of using BPAT to diagnose BPD in patients with long COVID. In particular, we have examined whether BPAT has good sensitivity and specificity for diagnosing breathing pattern disorders in long COVID.
Methods
Patients
Patients admitted across Barts Health NHS Trust for presumed or confirmed COVID-19 pneumonia were electronically referred to the After COVID Clinic and underwent asynchronous virtual review.10 Additional referrals of patients were accepted from the community where the GP had ongoing concerns after 12 weeks following confirmed or suspected COVID infection in the community. At virtual review, those patients with more severe post-COVID symptoms, or where there were other concerns, were triaged for face-to-face review by a consultant respiratory physician and a specialist respiratory physiotherapist. Further tests and validated questionnaires, including the Dyspnoea-12 (D12) questionnaire,11 were undertaken in this clinic. Physiotherapist review included MARM and BPAT assessments. BPAT assessment was undertaken after the patient had agreed to physiotherapist review and took 60 seconds to conduct whilst the patient was completing the clinical breathlessness questionnaires.
Service evaluation
The results reported here are from a further analysis of data from a local service evaluation (Barts Health NHS Trust CEU ID 11166) by the clinical team.10 Consecutive patients completing respiratory physiotherapist review (as described above) were included in the evaluation. Statistics were analysed in R (version 4.0.2; www.r-project.org) using the following additional packages: dplyr, eeptools, gplots, pROC. Clinical data was extracted from electronic medical records.
Results
Sixty-five patients underwent clinical and specialist respiratory physiotherapy face-to-face review in our post-COVID clinic, with complete assessment including physical examination, D12 questionnaire and BPAT assessment, over the period of our previous service evaluation.10 These patients were selected for face-to-face review after triage by virtual review raised clinical concerns regarding their recovery after COVID infection. On clinical assessment by a specialist respiratory physiotherapist, 19 of the 65 patients were diagnosed with clinically significant BPD as a component of their post-COVID syndrome.
Comparing clinical assessment to BPAT score with receiver operating characteristics (ROC) analysis, the area under the curve (AUC) was 0.906 (95% CI 0.810–1.000), showing a strong performance of BPAT in diagnosis of BPD (Fig 1). Taking the previously established cut-off BPAT score of ≥4 as positive for BPD, BPAT had a sensitivity of 89.5% and specificity of 78.3%. Of the 19 patients identified as having a breathing pattern disorder by clinical physiotherapy assessment, 17 had a BPAT score of ≥4.
Fig 1.
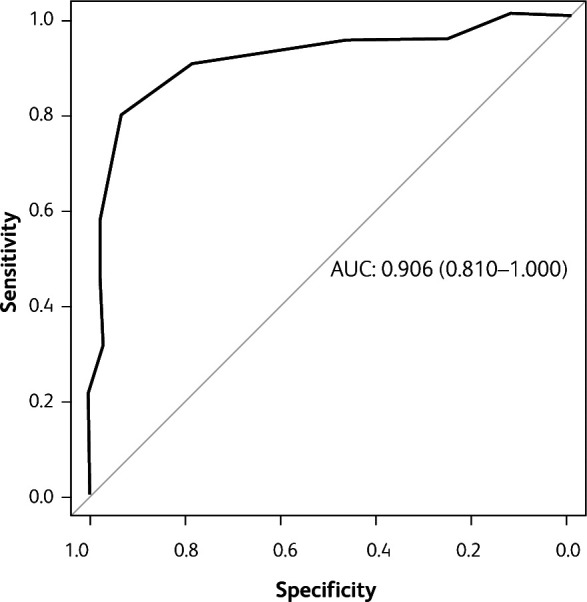
AUC ROC curve for use of BPAT to diagnose breathing disorder.
Comparing patients with positive and negative BPAT scores, patient characteristics were similar (Table 1). Both groups were predominantly female and included patients of different severities of initial acute COVID infection. Patients with positive BPAT had significantly higher D12 scores (mean (SD) D12 score 19.4 (8.6) vs 13.2 (8.7); p=0.0099, Wilcoxon-Mann-Whitney test) indicative of higher levels of breathlessness (Fig 2). However, breathlessness as rated by the patient on a 10-point scale did not significantly differ between patients with and without positive BPAT scores. Similarly, neither fatigue rated on a 10-point scale nor total symptom score were significantly different between patients with and without positive BPAT scores.
Table 1.
Patient demographics
| BPAT positive | BPAT negative | |
|---|---|---|
| Number, n | 27 | 38 |
| Gender | ||
| Female, n | 14 | 21 |
| Male, n | 13 | 17 |
| Age, years, mean (standard deviation) | 54.1 (13.7) | 50.4 (14.2) |
| Ethnicity | ||
| White, n | 8 | 9 |
| Black, n | 1 | 7 |
| Asian, n | 1 | 8 |
| Mixed/other, n | 1 | 0 |
| Not stated, n | 16 | 14 |
| Recovery period, weeks, mean (standard deviation) | 16.8 (5.7) | 14.7 (3.6) |
| Severity of acute COVID-19 | ||
| Severe (requiring hospitalisation with ICU admission and/or CPAP and/or HFNO), n | 6 | 9 |
| Moderate (requiring hospitalisation but not higher-level respiratory support), n | 5 | 15 |
| Mild (not requiring hospitalisation), n | 16 | 14 |
CPAP = continuous positive airway pressure; HFNO = high-flow nasal oxygen; ICU = intensive care unit.
Fig 2.
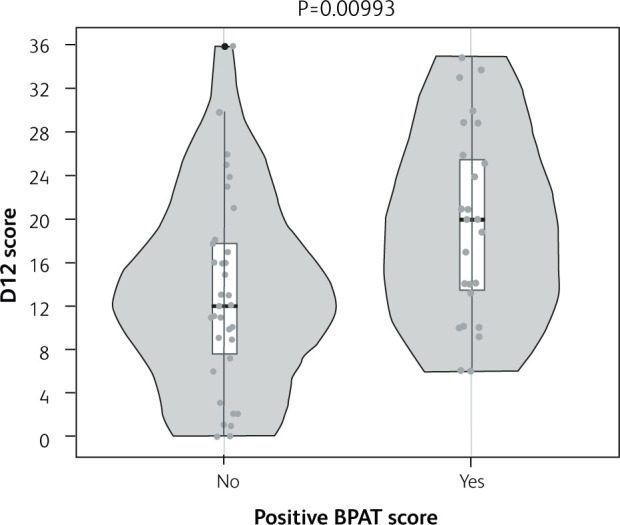
D12 questionnaire scores for breathlessness in patients with/without positive BPAT score indicative of likely breathing pattern disorder. Violin with box-and-whisker plots of D12 questionnaire scores for patients with BPAT score ≥4, positive for likely breathing pattern disorder, and those patients with BPAT score <4, negative for likely breathing pattern disorder. P value for Wilcoxon-Mann-Whitney test.
Analysing BPAT score as a continuous variable, there was a significant positive association between higher BPAT score and higher D12 score (r=0.39, p=0.00133, Pearson's test; Fig 3).
Fig 3.
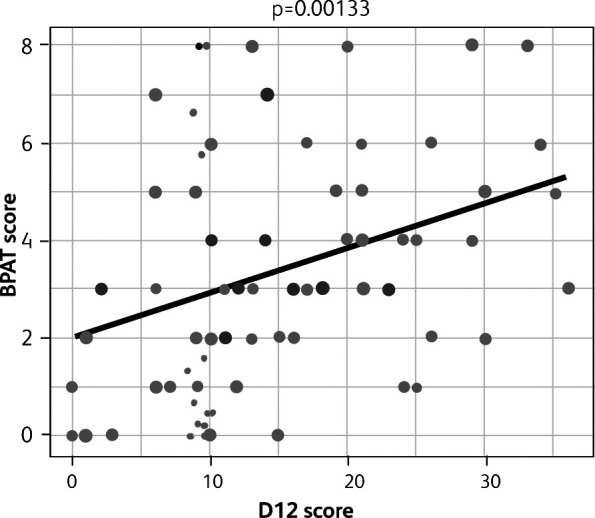
Association between BPAT scores and D12 questionnaire scores for breathlessness. Scatter plot with trend line. P value for correlation coefficient.
Discussion
Breathing pattern disorders were common in our cohort of patients reporting significant breathlessness following COVID infection, and evident in patients with different severities of initial acute COVID infection. BPAT had an excellent sensitivity and good specificity for dysfunctional breathing. Those patients with a BPAT score indicative of BPD had significantly higher levels of breathlessness on the D12 questionnaire than those without BPD. However, there was no difference between the groups on a 10-point breathlessness scale, which may reflect the limitations of a simple 10-point scale to assess any complex symptom.
BPAT is a standard part of our assessment of patients with unexplained breathlessness and a limitation of our study is that the physiotherapists who conducted the BPAT assessments also decided, based on their overall clinical assessment, whether a patient had a breathing pattern disorder or not. The physiotherapist making the diagnosis was not ‘blinded’ to the BPAT score, and vice-versa.
Breathing pattern disorders are increasingly being categorised into different types such as hyperventilation syndrome, periodic deep sighing and thoracic dominant breathing (examples from the Boulding classification).1 Whether the BPAT tool has similar sensitivity and specificity at detecting these different types of dysfunctional breathing is unknown, as is the proportion of patients with post-COVID breathing pattern disorders of each type. There was only a modest correlation between D12 scores and BPAT scores on a continuous scale – whether the absolute BPAT score has additional value in triaging which patients may benefit most from specialist breathing pattern physiotherapy is uncertain. Notably, the sensitivity of BPAT was better than its specificity, suggesting it could be used as a quick screening test to identify patients needing further specialist respiratory physiotherapy review.
A limitation in studies of clinical assessment of breathing pattern, including this evaluation, is the lack of an accepted, objective gold-standard for diagnosis of all forms of BPD. While MARM is an accepted clinical standard, it is a subjective assessment. There is increasing interest in use of cardio-pulmonary exercise testing (CPET) to objectively assess breathing pattern. In particular, CPET can detect chronic hyperventilation syndrome and ventilatory irregularity (corresponding to periodic deep sighing in the Boulding classification) as limitations to exercise capacity.12,13 CPET studies of patients post-COVID have similarly shown a high prevalence of BPD,14,15 but CPET is resource-intensive, limiting its use in the assessment of large numbers of patients in long COVID clinics.
Why some people, including many patients after COVID pneumonia, develop breathing pattern disorders remains very uncertain. One possibility is that abnormal breathing patterns develop during acute respiratory insults as an adaptive response to the pathology, eg as responses to hypoxaemia or basal lung consolidation, but pathologically persist after resolution of the acute respiratory insult. There is also a complex interplay between stress, anxiety, breathing pattern and breathlessness.16 Specific to COVID, there has also been a suggestion the virus may be able to directly affect brainstem respiratory centres.17
Conclusion
BPAT looks likely to be a useful tool in assessing patients for breathing pattern disorders post-COVID. Further research is now needed examining the clinical response of these patients to specialist respiratory physiotherapy.
Summary
What is known?
Breathlessness is a frequent symptom in long COVID.
Breathing pattern disorders (BPDs) are a common cause of chronic breathlessness, but often difficult to diagnose.
What is the question?
Does the Breathing Pattern Assessment Tool (BPAT) have good sensitivity and specificity for diagnosing breathing pattern disorders in long COVID?
What was found?
Using the established cut-off, BPAT had a sensitivity of 89.5% and specificity of 78.3% for diagnosing breathing pattern disorders in patients with long COVID.
What is the implication for practice now?
BPAT is a useful tool for identifying patients with BPD among those presenting with post-COVID breathlessness.
Conflicts of interest
Paul E Pfeffer, Hannah Hylton and Richa Singh are co-investigators on an NIHR-funded grant NIHR132243 – Supported remote rehabilitation post Covid-19: development, deployment and evaluation of a digitally enabled rehabilitation programme. There is no conflict of interest between that grant and this research.
References
- 1.Boulding R, Stacey R, Niven R, Fowler SJ. Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev 2016;25:287–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Courtney R, van Dixhoorn J, Cohen M. Evaluation of breathing pattern: comparison of a Manual Assessment of Respiratory Motion (MARM) and respiratory induction plethysmography. Appl Psychophysiol Biofeedback 2008;33:91–100. [DOI] [PubMed] [Google Scholar]
- 3.Todd S, Walsted ES, Grillo L, Livingston R, Menzies-Gow A, Hull JH. Novel assessment tool to detect breathing pattern disorder in patients with refractory asthma. Respirology 2018;23:284–90. [DOI] [PubMed] [Google Scholar]
- 4.Bondarenko J, Hew M, Button B, et al. Reliability of the breathing pattern assessment tool for in-person or remote assessment in people with asthma. Clin Exp Allergy 2021;51:1218–20. [DOI] [PubMed] [Google Scholar]
- 5.Evans RA, McAuley H, Harrison EM, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study. Lancet Respir Med 2021;9:1275–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mandal S, Barnett J, Brill SE, et al. ‘Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2020. 76:396–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heightman M, Prashar J, Hillman TE, et al. Post-COVID-19 assessment in a specialist clinical service: a 12-month, single-centre, prospective study in 1325 individuals. BMJ Open Respir Res 2021;8:e001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dani M, Dirksen A, Taraborrelli P, et al. Autonomic dysfunction in ‘long COVID': rationale, physiology and management strategies. Clin Med 2021;21:e63–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reilly CC, Floyd SV, Lee K, et al. Breathlessness and dysfunctional breathing in patients with postural orthostatic tachycardia syndrome (POTS): The impact of a physiotherapy intervention. Auton Neurosci 2020;223:102601. [DOI] [PubMed] [Google Scholar]
- 10.Taylor RR, Trivedi B, Patel N, et al. Post-COVID symptoms reported at asynchronous virtual review and stratified follow-up after COVID-19 pneumonia. Clin Med 2021;21:e384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yorke J, Moosavi SH, Shuldham C, Jones PW. Quantification of dyspnoea using descriptors: development and initial testing of the Dyspnoea-12. Thorax 2010;65:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bansal T, Haji GS, Rossiter HB, Polkey MI, Hull JH. Exercise ventilatory irregularity can be quantified by approximate entropy to detect breathing pattern disorder. Respir Physiol Neurobiol 2018;255:1–6. [DOI] [PubMed] [Google Scholar]
- 13.Ionescu MF, Mani-Babu S, Degani-Costa LH, et al. Cardiopulmonary exercise testing in the assessment of dysfunctional breathing. Front Physiol 2020;11:620955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mancini DM, Brunjes DL, Lala A, et al. Use of Cardiopulmonary Stress Testing for Patients With Unexplained Dyspnea Post-Coronavirus Disease. JACC Heart Fail 2021;9:927–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frésard I, Genecand L, Altarelli M, et al. Dysfunctional breathing diagnosed by cardiopulmonary exercise testing in ‘long COVID' patients with persistent dyspnoea. BMJ Open Respir Res 2022;9:e001126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barker N, Everard ML. Getting to grips with ‘dysfunctional breathing’. Paediatr Respir Rev 2015;16:53–61. [DOI] [PubMed] [Google Scholar]
- 17.Gandhi S, Srivastava AK, Ray U, Tripathi PP. Is the collapse of the respiratory center in the brain responsible for respiratory breakdown in COVID-19 Patients? ACS Chem Neurosci 2020;11:1379–81. [DOI] [PubMed] [Google Scholar]


