ABSTRACT
The delivery of elective care needs to be reimagined to tackle the increasing demand for services that is currently outstripping the available capacity; a problem exacerbated by the impact of the COVID-19 pandemic.
This article highlights key strategies to improve the delivery of elective care combined with local and national examples of best practice. It is based on key recommendations from the Getting It Right First Time (GIRFT) programme: the UK's largest healthcare quality improvement programme operating across 42 clinical specialties. GIRFT has visited every integrated care system in England over the last 12 months to discuss elective recovery and the learning from these visits is captured in this article.
Rethinking the delivery of elective care, utilising advances in technology, and harnessing the power of data to identify unwarranted variation and targeted areas for improvement, will dramatically change the future delivery of elective care for the better.
KEYWORDS: elective care, GIRFT, pathway standardisation, productivity, workforce
Introduction
In January 2022, there were 6,104,056 patients waiting for consultant-led non-urgent treatment.1 The pandemic has led to increased waiting times in all specialties as elective care was postponed to manage the influx of acute medical patients presenting with COVID-19. From March 2020 to March 2021, the number of patients waiting for elective treatment increased by 17%, and those waiting for more than 52 weeks increased from 3,097 to 436,127. Although most patients are waiting for surgical treatment, there are over 1.8 million adults waiting for elective treatment in a medical specialty.
Prior to the pandemic, waiting lists had been increasing month on month since April 2012, and the NHS has not met the operational standard for 92% of patients receiving treatment within 18 weeks of referral since November 2015.2,3 The NHS, as part of its elective recovery programme, has published ambitious targets stating that no patient will wait more than 1 year for treatment by March 2025.4 Herein, we showcase major initiatives that will transform the delivery of elective care in the NHS in England.
We focus on how to improve patient care and experience, maximise use of existing resources, improve service resilience (maintaining services during peaks of demand) and manage the surge in patients waiting for treatment. Case studies are used to demonstrate best practice from a range of medical and surgical specialties and help to visualise the future delivery of elective services.
The strategies outlined in this article are based on learning from the Getting It Right First Time (GIRFT) programme in England; a clinically-led, data-driven quality improvement programme operating across 42 clinical specialties. To date, GIRFT has conducted over 4,000 hospital visits: meeting with local clinicians and managers to discuss areas of unwarranted variation and use outcome metrics to identify improvement opportunities to transform the quality of care.
Improving patient care and experience
Unwarranted variation: identifying the issues
Geographical variation in healthcare outcomes has long been reported in England and beyond.5–7 The inconsistencies can sometimes be appropriate and deliberate as care is tailored to the local population. A problem arises when this variation is unwarranted, which is defined as ‘variation that cannot be explained on the basis of illness, medical evidence, or patient experience’.8 Public Health England has produced atlases of variation since 2010, showcasing the scale of unwarranted variation across the NHS, thereby influencing discussion, policy and spending.
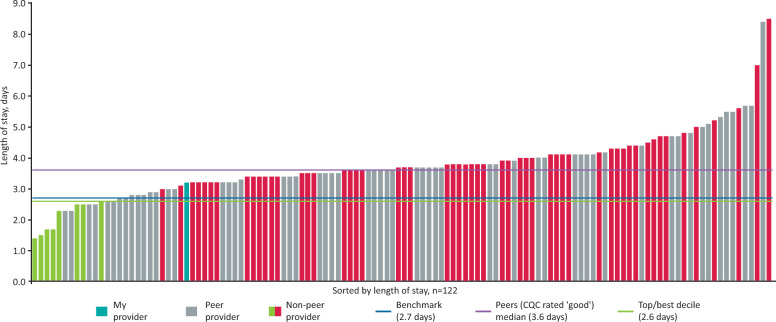
The GIRFT programme specifically works to reduce variation in the delivery of healthcare services. Fig 1 demonstrates variation in the length of stay for a primary hip replacement, which ranges from 1.4 to 8.5 days. A 500% difference in the average length of stay between two providers for the same procedure raises issues and warrants further investigation.9 GIRFT has demonstrated similar variation in outcomes, activity and value across all 42 specialties. The future of elective care depends on reducing the gap between the best and worst performing providers.
Fig 1.
The length of stay for adult patients receiving elective primary hip replacement. Each bar represents an NHS provider in England. An example of data available to each NHS provider on the Model Health System. Adapted with permission from NHS. The Model Health System. NHS. www.england.nhs.uk/applications/model-hospital
Every provider must instigate the necessary outcome improvement measures to ensure their performance for each metric is equivalent (or better) than the average of the top 10% of providers. This is termed ‘top decile’ performance and supports continual quality improvement; for example, the incidence of surgical site infection (SSI) following elective hip or knee arthroplasty ranges from 0.5% to 4% across the NHS. Tackling this variation by adhering to best practice principles could reduce 6,000 SSIs and save the NHS £300 million per year.5
Using data to drive improvement
GIRFT has developed gateway frameworks for each specialty that are a series of key metrics, allowing providers to benchmark performance against GIRFT standards and compare performance with every trust in the country. GIRFT clinical leads discuss these metrics with clinicians and managers during trust visits to identify targeted opportunities for improvement and uncover areas of exemplar practice that can be cascaded through the health service and included in national pathways.
The Model Health System (MHS) will revolutionise the ability to measure quality and efficiency across care pathways.9 It is a dashboard accessible to all healthcare professionals displaying key performance metrics for every specialty in each NHS hospital. For the first time, freely available data covering the whole NHS is available in one place and refreshed regularly. Elective care in the future will be transformed by expanding the data points available on MHS, and increasing engagement with the system. As electronic patient record systems are developed, MHS will be able to collect data in real time, aiding data interpretation and usefulness by eliminating lag time. These interventions are critical for reducing unwarranted variation and improving the quality of elective care.
Pathway standardisation
When pathways of care are not clearly defined, they can be complex to navigate and inefficient.10,11 In response to the elective backlog, GIRFT's High Volume Low Complexity (HVLC) programme created end-to-end patient pathways for 29 surgical procedures. They outline optimal evidence-based clinical and operational practice to improve quality of care and ensure efficient resource use. These 29 standardised process maps include procedures from six of the largest surgical specialties, representing 63% of waiting list activity and over 70% of patients waiting 52 weeks or more for surgery.12,13
These procedure process maps have been designed to tackle variation in practice and promote widespread adoption of best practice relating to patient outcomes and value. Pathways enable providers and systems to perform gap analyses between their current practice and the optimal process, thus helping to identify new ways of working. Furthermore, standardised procedure pathways across a region or integrated care system tailored to local needs can assist with mutual aid between providers and encourages knowledge sharing to solve issues and optimise service delivery.
Standardised pathways will be a fundamental facet of elective recovery and will create capacity by helping promote widespread improvement in patient outcomes and utilisation of resources; for example, providers that have successfully implemented the spinal HVLC pathway have reduced the number of perioperative outpatient attendances and reduced the number of interventions required (Fig 2).12 The number of standardised pathways now needs to be expanded at pace across medical and surgical specialties as a tool to improve outcomes, reduce the backlog and deliver value.
Fig 2.
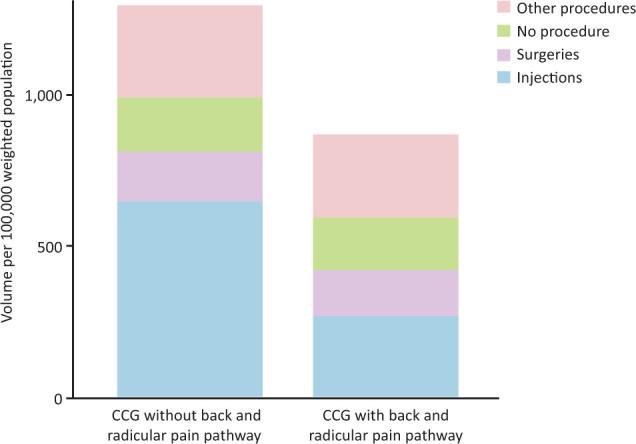
The number of spinal procedures between clinical commissioning groups with and without a back and radicular pain pathway. Analysed using Hospital Episode Statistics data. CCG = clinical commissioning group. Adapted with permission from Getting It Right First Time. Elective recovery high volume low complexity (HVLC) guide for systems, 2nd edition. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/12/GIRFT_HVLC_Guide_Edition_2_FINAL.pdf
Clinical leadership
The future of elective care can only be delivered with clinicians, executives and operational leads working ‘shoulder to shoulder’. Clinicians with an interest in leadership and management need to be supported to lead local transformation work.12,13 High-quality leadership in healthcare has been shown to deliver improved quality and efficiency.5 Cheshire and Merseyside Health and Care Partnership has developed a clinically-led, operationally supported, elective restoration and transformation programme to ensure the adoption of best practice within its system driven by specialty-level clinical networks.12
The increased demand in elective care has seen a reduction in the leadership time within consultant job plans, and consultants are spending more of their time delivering direct patient care. Although this was required during the pandemic, leadership time in consultant job plans needs to be restored and invested in for elective care to develop and improve.14
Efficient use of resources and service resilience
Day-case procedures
The British Association Of Day Surgery directory lists over 200 procedures that should be performed as a zero-night stay. The future of elective care should see 80%–85% of all elective surgery default to a day-case pathway. There is potential to increase the number of procedures performed as a day case in many specialties. This will help improve patient experience, reduce cancellations due to bed pressures at times of peak demand (eg winter pressures) and increase inpatient bed availability for more complex procedures. In gastroenterology, if every provider increased the proportion of endoscopic retrograde cholangiopancreatography (ERCP) done as a day case and met the best quartile target of 6.3% overnight stays, 1,700 admissions would be avoided, and the notional financial opportunity would be £1.67 million.16
Clinicians and managers need to look for opportunities to move procedures down the ‘intensity gradient’ from inpatient to day-case settings, and from day-case theatres to outpatient clinics.15 The GIRFT national report in dermatology describes how local anaesthetic surface surgery is being undertaken in general-anaesthetic-equipped operating theatres rather than outpatient procedure rooms despite there being no evidence that outcomes in dermatology are improved by carrying out procedures in more complex settings.14
Innovative enhanced recovery pathways and a change in culture implemented at South Warwickshire NHS Foundation Trust have enabled the delivery of day-case total hip replacements for selected patients with excellent patient reported outcomes.17 Day-case arthroplasty is pushing the boundaries of possibility in relation to day-case surgery. Calderdale and Huddersfield NHS Foundation Trust is utilising wearable technology to facilitate its elective day-case knee replacement pathway. The device monitors and guides patients postoperative rehabilitation, enabling them to maximise self-directed therapy, thus enhancing recovery and improving outcomes.18
Virtual wards are a new alternative to bedded care, where patients can receive monitoring, acute care and treatment enabled by technology in their own home.19 During the COVID-19 pandemic, virtual wards were a vital tool in freeing up in hospital bed capacity.20 This new method of healthcare delivery now needs to be adapted to support the provision of elective care as day case.
Maximising productivity
A major barrier to improving access to elective care is the availability of operating theatres, clinic rooms and other highly specialised estate. While we wait for new facilities to be built, the quickest and most economical solution to increasing capacity is to maximise the use of current resources. The ‘new normal’ will see creative job planning, services operational for 6–7 days per week, 2.5–3.0 session days and clinicians working across sites with staff passports.21
As we move towards more standardised pathways of elective care, productivity levels need to be recognised. In gastroenterology, one trust with five endoscopy rooms is performing more endoscopies than another trust with 12 rooms.14 Although there are many reasons why this could be, there is significant variation nationally in endoscopy activity. To address this, GIRFT has published productivity standards for the number of cases expected during a 4-hour session for certain uncomplicated procedures. Examples include 10 cataract procedures for a non-training list (eight for a training list), and two total hip or knee replacements on a half day list or their equivalent.12,13 These numbers are achieved not by completing the actual procedures more quickly, instead, what needs to change is the operational and organisational performance that often prevents clinicians from completing their jobs efficiently.
Following the pandemic, we have seen examples of trusts transforming their services to tackle the elective backlog and maximise resources. This has been demonstrated by the Barking, Havering and Redbridge University Hospitals NHS Trust, which completed 135 joint replacements in 1 week, and Moorfields Eye Hospital NHS Foundation Trust, which performed 713 cataract operations in 1 week as part of elective drive events.22,23
Outpatient appointments
There continues to be unwarranted variation in outpatient follow-up rates impacting capacity to see new patients. The reasons for the observed variation are multifactorial, however, there is evidence to suggest that high follow-up rates can be related to inexperienced clinicians having uncertainty of their diagnosis or treatment and experienced clinicians wanting certainty prior to discharge.16
Follow-ups should be benchmarked for each specialty and there needs to be universal agreement defining which patients can be discharged with patient-initiated follow-up. For this to work, appropriate safety netting is required with a robust process to urgently review patients failing to progress. University Hospital Southampton NHS Foundation Trust developed a regional strategy to manage neurology follow-ups and published a consensus statement developed by consultants that remains a departmental guideline. This has clearly been useful in teaching trainees and managing patients' expectations.24
Additionally, we need to break the traditional cycle of investigation where a patient is reviewed, then sent for investigation and then re-reviewed etc. When clinicians review patients for the first time, they should have the results of the necessary investigations available so a complete assessment can be undertaken. This will be achieved by developing more one-stop clinics or triaging referrals and sending patients for investigation prior to clinical review (Fig 3).24 Imperial College Healthcare NHS Trust developed a male lower urinary tract one-stop outpatient clinic and reduced their follow-up rate by 55%.25
Fig 3.
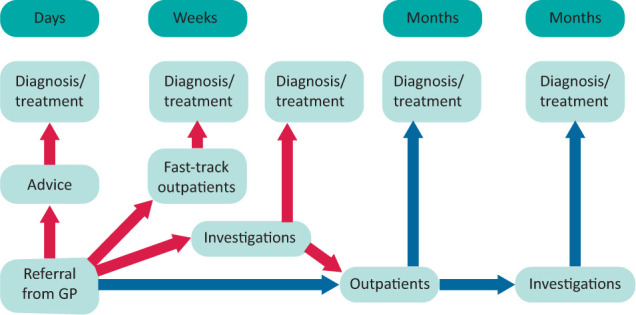
Active assessment of referrals to secondary care (red arrows) provides earlier diagnosis and treatment in comparison to conventional processes (blue arrows). GP = general practitioner. Adapted with permission from Getting It Right First Time. Neurology: GIRFT programme national speciality report. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2022/06/Neurology-Sept21g.pdf
Elective recovery also depends on reducing the number of patients who do not turn up to clinical appointments that continues to be a problem across specialties. Nationally, 7.3 million outpatient appointments were missed in 2021; generally the highest did not attend (DNA) rates are in hepatology and diabetic medicine.14,26 The cause of DNA is multifactorial and requires a combined generic and specialty-specific approach; for example, gastroenterology patients with digestive conditions may find it physically challenging to attend hospital appointments. Clinicians need to consider such challenges and personalise care planning to patients' needs by providing appropriate local facilities and more community and virtual appointments.14
Managing the demand
Workforce and training
Workforce challenges are a barrier to the growth of every specialty. The Royal College of Anaesthetists estimates there is a deficit of 1,400 anaesthetists, preventing 1 million operations from taking place per annum.27 Rethinking roles, developing new ones, and supporting the workforce will be crucial to the future of elective care.
Trainees need to be supported to access training opportunities (eg daytime theatre and clinic sessions) to prevent delays in completion of training and to ensure tomorrow's consultants have the requisite skillset. The Joint Committee on Surgical Training has made it clear that every operation should be a training operation.28 The GIRFT and Royal College of Ophthalmologists guidance on high-flow all-complexity cataract surgery clearly defines how training should be undertaken on these lists and demonstrates how it is possible to train junior doctors while simultaneously increasing service capacity to manage the elective backlog.29,30
The future of elective care will see all healthcare professionals working at the top of their licence, utilising the breadth of their experience and knowledge, to enable career development, help with staff retention, and support developing elective services. In high-flow cataract surgery, patients are admitted, operated and discharged within 60 minutes.31 This is only possible by upskilling ophthalmic nurses to help with every part of the patient pathway, eg confirming consent and marking the eye pre-procedure. In ophthalmology, the ophthalmic practitioner programme was developed to upskill non-medical eyecare professionals to develop new competencies through a nationally recognised programme to help improve capacity.32 Many trusts now offer non-medically-led services such as University Hospitals of Leicester NHS Trust, which developed a cardioversion service led by advanced practitioners. The results of which have been proven to be safe and efficient.21
Managing referrals
All referrals to a secondary care service should be triaged, by an appropriately qualified individual, to ensure patients receive the correct care the first time.14 Vetting referrals ensures patients are booked into the correct specialist clinic or managed in the community with appropriate specialist advice.21 Clinical triage of referrals helps improve waiting times, increase the number of patients discharged following their first appointment and provide patients with clinical input earlier. St Helens and Knowsley Teaching Hospitals NHS Trust set up a consultant-led virtual referral triaging clinic that runs every day. This has seen the number of patients discharged after their first gastroenterology clinic appointment increase to 51% (double the national average).14
A close working relationship with primary care colleagues is essential to facilitate managing patients in the community and supporting referral to secondary services. In north-west London, a clinical decision making tool has been embedded into primary care software for urology referrals; thus, effectively automating the triaging process. The software prompts general practitioners (GPs) to answer a series of set questions and self-populates key information from the patient's electronic record (eg blood results). Local urology pathways are embedded into the software and, where appropriate, specialist advice is provided to GPs in real time to support treatment in the community. If a referral to secondary care is necessary, the software will automatically generate a referral letter saving the GP time. The tool is an example of how technology can be used to reduce variation in secondary care referrals, provide patients with information quickly and help ensure that patients are treated in the right place at the right time.33
Elective care hubs
Peaks in demand for acute medical services, as seen during busy winter periods, directly impact the delivery of elective care. Elective hub sites are a solution to this issue. They are ring-fenced elective surgical facilities separated from emergency and acute care. This hot/cold split was first introduced by GIRFT in orthopaedics where separating elective and trauma surgery was shown to improve clinical outcomes and performance and, importantly, patient safety and staff morale.
Elective care hubs will help increase capacity, and as they are separated from acute services, will continue to operate during peaks of acute and emergency care. Hubs can be standalone elective facilities or created within existing acute sites. Hubs also provide an opportunity to address inequities of access and promote collaborative working across regions. During the pandemic, many regions successfully created cancer treatment hubs with ring-fenced capacity and workforce to treat patients despite the COVID-19 challenges in secondary care.34
Across London, elective hubs have demonstrated increased productivity levels, reduced on-the-day cancellations, improved staff and patient experience, better financial position, and higher quality of care. The future will see clinicians in appropriate specialties undertaking more of their elective workload at new elective care hubs.34
Conclusion
The delivery of elective care is highly complex. Here, we provided an overview of areas that can be transformed to improve future services and, most importantly, the quality of care. Clearly, diagnostics, outpatient services and perioperative care are all essential components to elective care and are explored further in other articles in this edition.
This article demonstrates that there are shared issues in the delivery of elective medical and surgical care, showing that a collaborative approach and shared learning will help transform services. Changes to ingrained ways of working and implementation of new practices will be challenging and relies upon clinicians, executives and operational managers working in close partnership.
There was rapid development and learning in response to the pandemic. Advances such as the introduction of virtual consultations and virtual wards occurred at pace, demonstrating what can be achieved. It is important that this momentum of transformation continues as we recover from the effects of the pandemic. The collective energy and resource now focused on elective recovery will ensure the elective backlog is taken care of and elective care delivery in the medium to long term is improved.
GIRFT has conducted detailed analysis on the impact of introducing the HVLC programme's standardised pathways and concepts as described in this article. It has shown that adhering to HVLC standards for the 29 procedures (that the HVLC programme currently covers) will free up theatre sessions and beds to address the elective backlog. Vitally, the freed-up theatres are fully staffed and can be used to tackle backlogs for non-HVLC procedures. This supports implementation of the HVLC programme and provides hope that, despite continued workforce and financial pressures, the transformation of elective services is possible.
References
- 1.NHS England . Consultant-led referral to treatment waiting times. NHS. www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times [Google Scholar]
- 2.Department of Health & Social Care . The NHS constitution for England. DHSC, 2021. www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england [Google Scholar]
- 3.NHS England, NHS Improvement . Referral to treatment (RTT) waiting times statistics for consultant led care: 2019/20. NHS. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/11/RTT-Annual-Report-2019-20-2.pdf [Google Scholar]
- 4.NHS England . Delivery plan for tackling the COVID-19 backlog of elective care. NHS, 2022. www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2022/02/C1466-delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care.pdf [DOI] [PubMed] [Google Scholar]
- 5.Lord Carter of Coles . Operational productivity and performance in English NHS acute hospitals: unwarranted variations. Department of Health, 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/499229/Operational_productivity_A.pdf [Google Scholar]
- 6.Public Health England, NHS Right Care . The 2nd Atlas of variation in risk factors and healthcare for respiratory disease in England. NHS, 2019. https://fingertips.phe.org.uk/profile/atlas-of-variation [Google Scholar]
- 7.Dartmouth Atlas Project . The Dartmouth Atlas of Health Care. Dartmouth Atlas Project. www.dartmouthatlas.org [Accessed 20 May 2022]. [Google Scholar]
- 8.Wennberg J. Tracking medicine: A researcher's quest to understand health care. Oxford University Press, 2010. [Google Scholar]
- 9.NHS . The Model Health System. NHS. www.england.nhs.uk/applications/model-hospital [Accessed 20 May 2022]. [Google Scholar]
- 10.Antonacci G, Lennox L, Barlow J, et al. Process mapping in healthcare: a systematic review. BMC Health Serv Res 2021;21:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute for Healthcare Improvement . QI essential toolkit: Flowchart. IHI, 2017. www.in.gov/health/files/Flowchart.pdf [Google Scholar]
- 12.Getting It Right First Time. Elective recovery high volume low complexity (HVLC) guide for systems, 2nd edition. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/12/GIRFT_HVLC_Guide_Edition_2_FINAL.pdf [Google Scholar]
- 13.Getting It Right First Time . Elective recovery high volume low complexity (HVLC) guide for systems. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/05/GIRFT-HVLC-Guide-Final-V6.pdf [Google Scholar]
- 14.Oates B. Gastroenterology: GIRFT Programme National Speciality Report. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/10/Gastroenterology-Oct21v.pdf [Google Scholar]
- 15.Getting It Right First Time, Centre for Perioperative Care, British Association of Day Surgery . National day surgery delivery pack. NHS, 2020. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2020/10/National-Day-Surgery-Delivery-Pack_Sept2020_final.pdf [Google Scholar]
- 16.Getting It Right First Time . Dermatology national speciality report. NHS, 2021. https://future.nhs.uk/connect.ti/GIRFTNational/view?objectId=112160933 [Google Scholar]
- 17.Saunders P, Smith N, Syed F, et al. Introducing a day-case arthroplasty pathway significantly reduces overall length of stay. Bone Jt Open 2021;2:900–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh G. Delivering digital day case knee replacement with BPM pathway. YouTube, 2020. www.youtube.com/watch?v=8dSrHm8w35c [Accessed 20 May 2021]. [Google Scholar]
- 19.NHS England . Supporting information for ICS leads: Enablers for success: virtual wards including hospital at home. NHS, 2022. www.england.nhs.uk/wp-content/uploads/2022/04/B1382_supporting-information-for-integrated-care-system-leads_enablers-for-success_virtual-wards-including-hos.pdf [Google Scholar]
- 20.Schiff R, Oyston M, Quinn M, Walters S, McEnhill P, Collins M. Hospital at Home: another piece of the armoury against COVID-19. FHJ 2022;9:90–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Getting It Right First Time . Cardiology national speciality report. NHS, 2021. https://future.nhs.uk/GIRFTNational/view?objectId=112034597 [Google Scholar]
- 22.Vemulapalli K. BONES: BHRUT Orthopaedic NHS Elective Surgery project. Barking, Havering and Redbridge University Hospitals NHS Trust, 2021. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fwww.gettingitrightfirsttime.co.uk%2Fwp-content%2Fuploads%2F2021%2F09%2FBHRUT-BONES-Week-HVLC-summary-2021-08-27.pptx&wdOrigin=BROWSELINK [Google Scholar]
- 23.Wickham L, Reinink M. Moorfields: The cataract drive and beyond... UK Ophthalmology Alliance, 2021. https://uk-oa.co.uk/wp-content/uploads/2021/01/Moorfields-The-Cataract-Drive-Loiusa-Wickham-Merel-Reinink.pdf
- 24.Getting It Right First Time. Neurology: GIRFT programme national speciality report. NHS, 2021. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2022/06/Neurology-Sept21g.pdf [Google Scholar]
- 25.Getting It Right First Time. Getting it right in urology: Innovations, good practice and guidelines for establishing a urology area network. NHS, 2019. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2020/09/GIRFT-Urology-Innovations-OCT2020.pdf [Google Scholar]
- 26.NHS Digital . Provisional monthly hospital episode statistics for admitted patient care, outpatient and accident and emergency data, April 2021 – December 2021. NHS, 2022. www.gov.uk/government/statistics/provisional-monthly-hospital-episode-statistics-for-admitted-patient-care-outpatient-and-accident-and-emergency-data-april-2021-december-2021 [Google Scholar]
- 27.Royal College of Anaesthetists . The anaesthetic workforce: UK state of the nation report. RCoA, 2022. www.rcoa.ac.uk/sites/default/files/documents/2022-02/State-Nation2022.pdf [Google Scholar]
- 28.Joint Committee on Surgical Training, The Association of Surgeons in Training, British Orthopaedic Trainees Association, Confederation of Postgraduate Schools of Surgery . COVID-19 recovery – Training any time, any place, every case – no excuses. JCST, 2021. [Google Scholar]
- 29.Getting It Right First Time . High flow all complexity cataract surgery pathway. NHS, 2022. [Google Scholar]
- 30.The Royal College of Ophthalmologists . Cataract surgical training in high volume cataract settings. RCOphth, 2022. www.rcophth.ac.uk/wp-content/uploads/2021/12/Cataract-Training-Report-1.pdf [Google Scholar]
- 31.The Royal College of Ophthalmologists . High flow cataract surgery, version 2.0. RCOphth, 2022. www.rcophth.ac.uk/wp-content/uploads/2022/02/High-Flow-Cataract-Surgery_V2.pdf [Google Scholar]
- 32.The Royal College of Ophthalmologists . Ophthalmic practitioner training. RCOphth. www.rcophth.ac.uk/training/ophthalmic-practioner-training [Accessed 20 May 2022]. [Google Scholar]
- 33.Ayres B, Gnanapragasam, Magallanes A, Reynolds W. Elective Surgery Recovery and Transformation: Urology. YouTube, 2022. www.youtube.com/watch?v=HcamXVHr11g [Accessed 20 May 2022]. [Google Scholar]
- 34.Getting It Right First Time . Design and layout of elective surgical hubs: A guide for NHS systems and regions to support planning of effective surgical hubs. NHS, 2022. www.gettingitrightfirsttime.co.uk/wp-content/uploads/2022/04/HVLC_2022-04-05_Guide_Design-and-layout-of-elective-surgical-hubs.pdf [Google Scholar]