ABSTRACT
The English NHS outpatient service was handling over 1.6 million referrals per month before the COVID-19 pandemic, with numbers growing each year. There was a fall during the pandemic but by 2022, referrals were close to pre-pandemic levels. The GIRFT programme clinical leads from over 41 specialties visited each English hospital to identify unwarranted variation in care and identify good practice. A wealth of innovations covering the whole outpatient journey were identified in the national reports, which are published on the GIRFT website. Patient needs and demands vary greatly between infants and the elderly, between mental health, medical and surgical specialties. However, it was remarkable how common themes bridged age and illness to identify again and again how services could be improved. This report summarises the key themes identified by GIRFT to improve outpatient services in England as it moves forwards from the COVID pandemic.
KEYWORDS: outpatients, pathways, GIRFT, NHS, innovation
Introduction
NHS GIRFT is a clinically led, data-driven programme that aims to reduce unwarranted variation by identifying and sharing best practice in English NHS care. This paper includes recommendations relating to outpatient services made by the GIRFT specialist clinical leads, who are NHS consultants. The 41 specialty national reports that had been published by GIRFT by April 2022 were reviewed to identify key themes to improve quality and efficiency of outpatient services. This work is synergistic with work done by the NHS National Outpatient Transformation Project and supports the NHS Long Term Plan. The findings, summarised in Table 1,1–14 have relevance in the UK and abroad.
Table 1.
Key recommendations and actions to improve outpatient efficiency
| Change/recommendation | Notes on actions, benefits and examples | GIRFT report where change mentioned most often/examples given |
|---|---|---|
| Reorganise NHS hospitals to meet population need |
|
Multiple reports |
| Link secondary care networks to primary care networks |
|
Cardiology1 Rheumatology2 Urology3 Endocrinology4 Children's and young people's mental health services5 |
| Address workforce shortages to reduce geographic variations |
|
Rheumatology2 |
| Develop MDT |
|
Urology3 Cardiology1 Ear, nose and throat surgery6 Dermatology7 |
| Train specialty doctors locally to meet local needs |
|
Dermatology7 |
| Develop superclinics to see very large referral numbers |
|
Dermatology7 |
| Manage patient expectations of what NHS can provide |
|
Multiple reports |
| Reduce referrals due to fear of litigation |
|
Multiple reports |
| Introduce threshold policies to avoid inappropriate referrals |
|
Dermatology7 |
| Encourage patient self-management |
|
Gastroenterology8 |
| Develop whole system care models (will avoid destructive primary care/ secondary care behaviours) |
|
Geriatric medicine9 |
| Avoid targets which disadvantage some in greatest need |
|
Rheumatology2 Endocrinology4 |
| Working with patients |
|
Gastroenterology8 |
| Avoid wastage on high-cost locums |
|
Dermatology7 |
| Use pre-referral advice and guidance telemedicine wisely |
|
Neurology10 Dermatology7 |
| Develop effective community services |
|
Diabetes11 |
| Direct triage by telemedicine to services |
|
Gastroenterology8 Dermatology7 |
| Avoid duplication of secondary care services |
|
Geriatric medicine9 |
| Most efficient use of hospital facilities |
|
Gastroenterology8 |
| Link services to produce synergistic shorter pathways |
|
Dermatology7 Gastroenterology8 |
| Efficient transition from paediatric to adult services |
|
Diabetes11 |
| Develop one-stop services |
|
Multiple reports |
| Innovative clinic settings |
|
Ophthalmology12 |
| Reduce clinic DNAs |
|
Respiratory13 Neurology10 Dermatology7 |
| Reduce follow ups by discharge or when appropriate by open appointments |
|
Breast surgery14 Multiple reports |
| Avoid losing follow up patients with disabilities |
|
Ophthalmology12 |
| Efficient use of high-cost drugs |
|
Rheumatology2 Dermatology7 Gastroenterology8 |
NHS outpatient referral numbers and waiting times
There were approximately 1 million referrals from primary care, and 680,000 from other services, to English NHS outpatients in the month February 2020. Referrals dropped substantially during the COVID pandemic, but by February 2022 primary care referrals had returned to over 90% of pre-COVID levels.15 As NHS outpatient activity was reduced over the pandemic, despite the reduction in referrals, outpatient waiting times increased. In February 2022, 62.6% of those referred to outpatients had started treatment by 18 weeks16 compared with 83.2% in February 2020.17 This fall in performance was due to COVID-19-related workforce and workspace redeployment, staff sickness and burnout. To move forwards with the available NHS resources, change is required in outpatient service provision. The GIRFT national reports offer a framework for change, backed up by evidence and experience and with buy-in from NHS clinical staff.
Reviewing nineteenth-century NHS hospital infrastructure
Outpatient pathways in England are based around 200 national health service (NHS) hospital trusts serving 56 million people. Of these, about 50 are mental health trusts and the remainder are acute hospital trusts. They vary in size and services from small district general hospitals with annual budgets of €150 million to large city university NHS trusts, some with up to nine hospitals, with annual budgets of well over €1 billion. Many hospitals were located to serve the local needs of eighteenth- and nineteenth-century populations, and despite rebuilding and mergers, the NHS secondary care outpatient structure is often based on these historic institutions. Attempts to merge and close inefficient units are often resisted. Local communities are protective of the strong historic and cultural links, resisting change, even if health outcomes are poorer. Therefore, successful reconfiguration cannot be based only on data-driven logic but requires consultation and explanation to accommodate and respect the wishes of local communities.
Developing linked primary and secondary care outpatient networks
Teams led by specialist consultants, employed by hospitals, provide care in hospital wards and emergency departments in addition to their outpatient roles. This often ties outpatient services to historical hospital locations, reducing flexibility to reconfigure outpatient services based on patient need. Reconfiguration driven by patient need would, in the case of many conditions, lead to secondary care networks with close links to primary care networks, as recommended by some GIRFT reports.1–4 The best services in some specialties were able to offer multiagency joined-up care, enabling rapid responses to crises, without inpatient admission.5 However, NHS outpatient clinical staff shortages in other specialties may make it more efficient to keep staff in centralised multidisciplinary clinics, offering virtual advice to distant sites, than for them to travel between multiple, widely dispersed clinics.
Addressing outpatient workforce shortages with the multidisciplinary team
Addressing NHS workforce shortages is fundamental to developing a modern, flexible outpatient system, based on patient location and needs rather than on hospital location.
Imbalances between capacity and demand lead to considerable variation around England in referral to treatment times (RTT). For example, RTT in rheumatology varied from 5–30 weeks for serious conditions, such as vasculitis and lupus, which require rapid diagnosis and assessment to reduce morbidity and mortality.2
Use of the wider multidisciplinary team (MDT) not only increased efficiency, but improved quality.1 Examples include urology specialist nurses reducing unnecessary admissions and attendances, through telephone or electronic follow up and emergency triage systems. Quality was improved through their emphasis on patient safety and patient experience, and their ability to provide a caring environment.3 Nurses delivering post-operative care and chronic disease management freed up medical time and added quality to services.6,7 Many trusts developed the consultant nurse grade creating an aspirational career structure to help nurse retention and morale.7
The NHS medical workforce shortage is widespread. Small hospitals in more remote areas away from training centres are often short of doctors, who have settled with houses and schools in the large city-based training centres. GIRFT identified the benefits of small hospitals ‘home-growing’ medical staff outside of HEE training schemes, by setting up local medical training schemes (so-called CESR trainees). This was effective in repopulating doctors into outpatient clinics in some hospitals away from the large training centres.7
Address workforce morale to get genuine staff buy-in for change
Financial pressure may lead to the NHS focusing on process rather than on people when attempting to improve performance. A top-down managerial style and change process may reduce morale. The GIRFT programme involved face-to-face visits to individual units by the clinical leads, most of whom were active clinicians, to engage and agree a change programme at a personal level with the staff who would deliver change. This produced genuine buy-in from healthcare staff, delivering clinically led change at local and specialty levels.
Developing outpatient multidisciplinary ‘superclinics’
As it takes up to 15 years to train new doctors to be consultants, improving capacity in the outpatient clinical team also requires training of the MDT. Nurses, pharmacists, physician associates, physiotherapists and other paramedical staff can bring different professional skills to improve outpatient care.
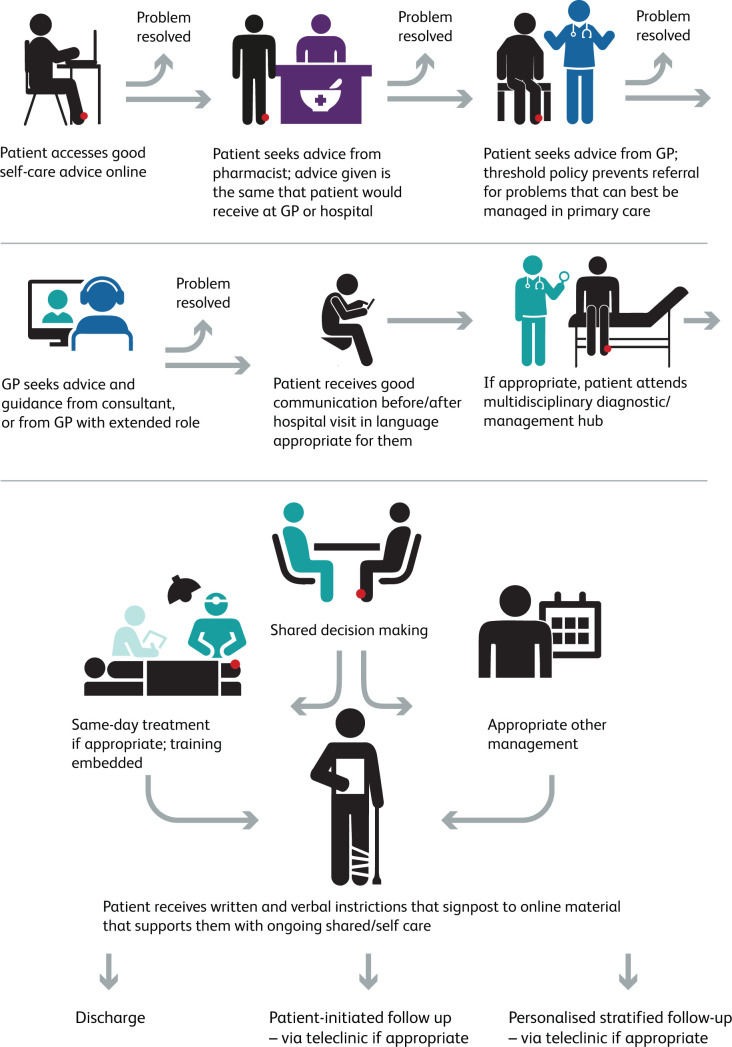
Fig 1.
Opportunities for improvement in the outpatient pathway. Some people with urgent, complex, or severe problems may omit some of these stages.
Some units have developed large outpatient ‘superclinics’ that are directly supervised by consultants but containing a combination of different team members. This model enables all patients to see somebody at their first outpatient visit who is competent to accurately diagnose and manage their problem.7 This avoids wasted time and resources for NHS staff and patients.
Managing factors increasing pressure on outpatients
Social media, electioneering promises, TV shows and inaccurate press reporting may lead to unrealistic expectations of the NHS outpatient service. Patients may demand outpatient referral from primary care, and treatment for less severe, lower-priority conditions in outpatients services. More surgical procedures are now day cases, which frees up hospital beds, reduces costs and may improve patient experience, but requires outpatient preparation and consent. There is pressure on primary care to refer cancer earlier. Fears of litigation regarding late or missed diagnosis increases pressure to refer to outpatients. The increasing complexity of healthcare increases the challenge of managing disease in primary care.
Managing pressure for outpatient referral with education and threshold policies
To ensure that the most appropriate people are referred to outpatient clinics, there should be effective referral threshold policies and education of patients and primary care staff.
Referral threshold policies list conditions which should not be referred unless there are exceptional reasons. Lists should be agreed between primary and secondary care with patient involvement. Threshold policies should be a shared responsibility for doctors and patients and adopted flexibly with common sense to avoid clinicians and patients expending resources trying to bypass them. A comprehensive range of threshold policies is on the Knowledge Anglia website.18 When first introduced, this was shown to reduce and stabilise outpatient referral numbers over several years.19
Clinicians should encourage patients to develop the skills, knowledge and confidence to self-manage their own conditions most effectively, which includes engaging with charities which provide patient education8 and appropriate web resources. Information given to patients in pharmacies should be better linked to that offered in primary and secondary care, to avoid mixed messaging.
Whole systems care models, and improving communication between primary and secondary care
Primary and secondary outpatient care can be divided by competitive funding systems, leading to inefficient ‘gaming’ attempts and poor communication. Whole-systems models in the elderly may reduce frailty progression and supported people to live well outside hospitals.9 Examples included community assessment hubs for ongoing assessment and treatment of frailty syndromes, crisis response hubs for events such as falls and the MDT working with GPs to support people at home.
Communication and joined-up care can be improved by GPs with extended roles who also work in hospital clinics, and by involvement of specialists in primary care education.7
Development of shared monitoring in primary and secondary care for people on long-term medication can move care back to the community, improve patient experience and reducing overall system costs – however, this requires sufficient primary care resource.
Balancing outpatient waiting list priorities
NHS cancer targets have improved access for people with cancer. However, targets in a setting of workforce shortages lead to reallocation of resources. This has worsened delays in some specialties such as endocrinology4 and rheumatology.2 GIRFT was advised (even before the pandemic) that, in some hospitals, some services for non-cancer patients had been suspended to enable hospitals to meet cancer targets.7
When routine waiting lists are long, some patients with a low risk of cancer access short cancer waiting lists. This shifts resources away from routine pathways, further lengthening waits for others without cancer. Systems should monitor how many of those referred with suspected cancer turn out to have cancer, to reduce inappropriate use of cancer pathways.
Working with patients
Shared decision making between clinicians and patients is likely to improve patient adherence to treatment, future attendance and identifying those who in future can be managed in a primary care setting.8
Locum agencies and outpatient waiting lists: short term gains – long term pain
Employing locum agencies to address long waiting lists is usually counterproductive. High pay to locum agencies incentivises NHS workers to leave the NHS. With a fixed-sized pool of workers, this worsens waiting times. Hospitals faced with workforce shortages pay external locums more than their own staff, incentivising more NHS staff to work for private locum agencies. Private locum agencies have lower costs as they invest less in education, training or research. This negative spiral was reported by hospital managers at some GIRFT visits; the managers concerned felt unable to break the cycle as there were penalties for not meeting targets.
Pre-referral activities to reduce pressure on outpatients
The NHS e-Referral service (e-RS) advice and guidance (A&G) system is widely used, although some hospitals have bought bespoke A&G systems. A&G is a telemedicine platform onto which primary care can upload requests for help from specialists with appropriate text, images and files. The specialist can offer advice, ask for more information or arrange for the patient to have a hospital clinic appointment, investigation or procedure. A&G enabled 8%– 23% of neurology referrals to be advised directly and promptly.10,20 There were some reports of A&G reducing referrals and provide patients with rapid help in primary care. However, there were some reports of A&G services increasing the total number of requests, with little impact on outpatient waits. Good quality research with unbiased data is needed to explore this further.
Effective community services can improve outcomes; for example, a community-based footcare protection service to screen people and help prevent diabetes-related problems, can help prevent the ulceration that leads to 80% of the 140 diabetes-related leg, foot and toe amputations that occur each week in the UK.11,21
Referral pathways for procedures or specific advice
Trusts should explore alternative pathways to access advice and treatment; examples include direct telemedicine triage of skin cancer surgery lists,7 and clinics led by specialist nurses, pharmacists or dieticians.8
Current rules for cancer referrals, mandating that all those referred should receive either a telephone or face-to-face appointment, reduce NHS efficiency. If the referral contains sufficient details to enable a clinician to confidently discharge without a consultation (eg an image of a suspected skin cancer that is obviously a wart), then if rules were changed, it would be possible to discharge some patients with a letter, without an unnecessary outpatient appointment or telephone consultation.7
Opportunities for increased efficiency in the outpatient appointment
Virtual outpatient appointments when clinically appropriate can offer advantages for the patient, who can avoid time and money spent travelling and parking, and for the hospital, which will require less parking, waiting areas and clinic space.
Some hospitals had duplicated pathways for people with the same condition; for example, some people with frailty were attending up eight separate clinics, often for brief assessments that did not require face-to-face contact.9
Seven-day outpatient services and three-session days optimise outpatient space use.8 These must be job planned and resourced so staff are not pressured to work ever longer hours.
Closer integration between outpatient services, such as between dermatology and plastic surgery,7 or gastroenterology and surgery,8 may enable shorter pathways with fewer appointments. If investigations and procedures can be undertaken at a one-stop appointment, this reduces hospital visits, provided complex issues around consent, appropriate patient selection and safety are considered.
Transition from paediatric to adult services can be optimised with a clear pathway between paediatric and 16–18 services, a named lead clinician for 16–18 patients, and a service for 19–25-year-olds.11
Clinic settings outside hospital
Faced with space shortages in many clinics, innovative approaches have been adopted, such as mobile units and clinics in community centres and shopping centres.12 While these can offer flexibility and easy access to some, other specialties reported that they fragment the service, making it more challenging to provide education and cross-cover for sickness and leading to clinicians spending time travelling rather than seeing patients.
Reducing outpatient ‘did not attends’
Long wait times contribute to high ‘did not attend’ (DNA) rates,13 as do appointment communications that are phrased in complex language, sent in English to non-English speakers, or sent in writing to those who cannot read or see.7 Communications around outpatients should consider diversity and disability. DNA referral rates in neurology services varied from 6% to 31%; it was calculated that reducing rates in the services with the highest rates to the average of 11.7% would result in 16,000 new and 42,000 follow-up neurology appointments being saved per year.10
Follow-up in outpatients
The MDT and virtual appointments should be utilised when appropriate. When discharge is impossible, open appointments systems, such as patient-initiated follow-up (PIFU),22 may reduce outpatient attendances. These enable appointment booking only when needed. However, booking of appointments for unrelated problems, instead of using primary care, must be prevented. Personalised stratified follow-up has been recommended after breast, prostate and colorectal cancer to free up time for those with greatest need14,23 and may be suitable for other cancers. Digital remote monitoring systems providing ‘call and recall’ and ‘right-results’ can ensure that patients are not lost and access outpatients when necessary.
More able clinicians are more likely to discharge a patient after their first appointment. Although it can be a useful quality measure,3 discharge on first appointment may not be a valid outcome measure, when considered in isolation, of a high-quality service.7 A clinic seeing a high proportion of people with less complex problems will find it easier to discharge more on the first appointment. Conversely, a service offering excellent advice and guidance (A&G), which reduces patients seen in clinic with simple problems, would have a low first discharge rate. GIRFT leads identified that services that employed locums or ‘insourced’ services to reduce waiting lists often reported fewer discharges after first appointment, higher rates of follow-up and more unnecessary investigations. This was attributed to the variable quality of some locum services.7
Patients lost to outpatient follow up or with delayed follow up was a major issue for progressive diseases such as retinal disease and glaucoma12 and for those on systemic drugs and cancer pathways. This risks avoidable problems such as blindness, drug toxicity and side effects and delayed cancer diagnosis. This worsened during COVID and has only partly been helped by use of technology.
Reducing variation in high-cost drugs used in outpatients
There has been a huge increase in effective but high-cost biologic, immunotherapy and small molecule drugs for cancer and inflammatory disease in outpatients.2,7,8 These are highly beneficial for many patients but present a challenge for controlling NHS costs, partially met by NICE guidelines. The pharmaceutical industry spends large sums on marketing. Commissioners vary in how they implement NICE guidance.7 Hospital pharmacies should report all use to the NHS DEFINE database of secondary care drug use. This should enable unwarranted variation in use of expensive drugs to be detected.
There was wide variation in access to effective drugs prescribed in outpatients. For example, belimumab, a major innovation for systemic lupus erythematosus, was in 2019 only used in 27 trusts for 143 patients, far short of the expected 300.2
Employment of consultant pharmacists within the outpatient team may improve hospital adherence to NICE guidelines, encourage appropriate use of biosimilar drugs and biologics in the most cost-effective sequence, reduce side effects and help deal with medication issues associated with surgery, vaccination, infections and pregnancy.7
Summary
After the COVID-19 pandemic, NHS outpatient staff and services face substantial challenges. The advent of new digital technology, new medicines for cancer and inflammatory disease, better understanding of the genetic basis for personalised medicine and the power of AI and big data, provide complex but unparalleled opportunities for NHS outpatient services and NHS staff. To unlock these opportunities consideration should be given to the recommendations for outpatients in the GIRFT national reports.
References
- 1.Clarke S, Ray S. GIRFT programme national specialty report for cardiology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 2.Kay L, Lanyon P, MacGregor A. GIRFT programme national specialty report for rheumatology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 3.Harrison S. GIRFT programme national specialty report for urology. GIRFT, 2018. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 4.Wass J, Lansdown M. GIRFT programme national specialty report for endocrinology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 5.Northover G. GIRFT programme national specialty report for children and young people's mental health services. GIRFT, 2022. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 6.Marshall M. GIRFT programme national specialty report for ear, nose and throat surgery. GIRFT, 2019. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 7.Levell N. GIRFT programme national specialty report for dermatology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 8.Oates B. GIRFT programme national specialty report for gastroenterology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 9.Hopper A. GIRFT programme national specialty report for geriatric medicine. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 10.Fuller G. GIRFT programme national specialty report for neurology. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 11.Rayman G, Kar P. GIRFT programme national specialty report for diabetes. GIRFT, 2020. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 12.MacEwen C, Davis A, Chang L. GIRFT programme national specialty report for ophthalmology. GIRFT, 2019. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 13.Allen M. GIRFT programme national specialty report for respiratory medicine. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 14.MacNeill F, Irvine T. GIRFT programme national specialty report for breast surgery. GIRFT, 2021. Available from www.gettingitrightfirsttime.co.uk/girft-reports/ [Accessed 19 April 2022]. [Google Scholar]
- 15.NHS England and NHS Improvement. Statistical press notice: NHS outpatient referrals February 2022. NHSEI, 2022. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/04/MRR-SPN-February-2022.pdf [Accessed 19 April 2022]. [Google Scholar]
- 16.NHS England and NHS Improvement. Statistical Press Notice: NHS referral to treatment (RTT) waiting times data February 2022. NHSEI, 2022. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/04/Feb22-RTT-SPN-publication-89824.pdf [Accessed 19 April 2022]. [Google Scholar]
- 17.NHS England and NHS Improvement. Statistical Press Notice: NHS referral to treatment (RTT) waiting times data February 2020. NHSEI, 2020. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2020/04/Feb20-RTT-SPN-publication-version.pdf [Accessed 19 April 2022]. [Google Scholar]
- 18.Knowledge Anglia. Clinical thresholds policy. www.knowledgeanglia.nhs.uk/KMS/NorthNorfolk/Home/ClinicalThresholdsPolicy.aspx [Accessed 19 April 2022].
- 19.Tan E, Levell NJ, Garioch JJ. The effect of a dermatology restricted-referral list upon volume of referrals. Clin Ex Dermatol 2007;32:114–5. [DOI] [PubMed] [Google Scholar]
- 20.Association of British Neurologists. ABN guidance on neurology active referral management (AKA advice and guidance). ABN executive and ABN service Committee 2019-20. ABN, 2021. www.theabn.org/resource/collection/65C334C7-30FA-45DB-93AA-74B3A3A20293/ABN_guidance_on_referralmanagement_02122020cmrdckrf.docx [Accessed 19 April 2022]. [Google Scholar]
- 21.Diabetes UK. Putting feet first. www.diabetes.org.uk/get_involved/campaigning/putting-feet-first [Accessed 26 April 2022].
- 22.NHS England and NHS Improvement. Patient initiated follow-up. www.england.nhs.uk/outpatient-transformation-programme/patient-initiated-follow-up-giving-patients-greater-control-over-their-hospital-follow-up-care/ [Accessed 26 April 2022].
- 23.NHS England and NHS Improvement. Implementing personalised stratified follow up pathways. NHSEI, 2020. www.england.nhs.uk/wp-content/uploads/2020/04/cancer-stratified-follow-up-handbook-v1-march-2020.pdf [Accessed 26 April 2022]. [Google Scholar]