Abstract
We tested the feasibility and acceptability of a group therapy treatment that addresses the intersecting stigma-related stressors theorized to drive elevated mental health risk, sexual health risk, and their co-occurrence among Black and Latino gay, bisexual, and other men who have sex with men (GBM). First, we modified an existing 10-week, one-on-one, cognitive-behavioral treatment addressing co-occurring health risks among GBM to develop a group-based, intersectionally informed treatment for GBM of color. Then, an open pilot was conducted (n = 21, across two cohorts) with young Black and Latino GBM. An evaluation of feasibility metrics (e.g., eligibility-enrollment ratio, session attendance, rate of retention) supported overall treatment feasibility. Qualitative data suggest high acceptability of the treatment length, format, and content—and revealed a powerful theme: The treatment and group composition led participants to feel less alone as GBM of color. To further evaluate acceptability, baseline and 3-month post-treatment assessments and exit interviews were used to examine the treatment’s impact on stigma coping, mental health, and sexual health. Expected changes were found for: (a) stigma coping, as demonstrated by decreases in perceived sexual minority stress, racial minority stress, and intersectional stress; (b) mental health, including depression, anxiety, stress, and suicidality, but not alcohol use; and (c) sexual health, including condom use efficacy, sexual compulsivity, and PrEP uptake; with partial support for decreased human immunodeficiency virus (HIV) transmission risk acts. This study lays the groundwork for a group treatment to address intersectional stigma, mental health, and HIV risk among young Black and Latino GBM in the US.
Keywords: intersectionality, stigma-related stress and coping, mental health, HIV risk, cultural adaptation
Black and Latino gay, bisexual, and other men who have sex with men (GBM), represent one of the highest-risk groups for human immunodeficiency virus (HIV) infection both in the U.S. and globally (Centers for Disease Control and Prevention [CDC], 2016; Millett et al., 2006). Despite marked improvements in HIV screening, diagnosis, and viral load suppression within the US overall, progress on these metrics has been less pronounced among GBM of color (CDC, 2020; Dailey et al., 2017). At current rates, one in two Black GBM and one in four Latino GBM in the US will become infected with HIV in their lifetimes (CDC, 2016). Although GBM of color do not engage in greater rates of sexual risk behaviors compared with White GBM (Millett et al., 2007), their HIV infection rate is nearly four times the rate of White GBM and over 40 times the rate of US men overall. The disproportionate HIV burden that characterizes this already-vulnerable population is long-standing and, among some populations (e.g., young Latino GBM; CDC, 2017), increasing—underscoring the urgent need for of population-tailored preventive health interventions.
Stigma has been identified as a clear and persistent driver of this health inequity (Ayala et al., 2012; Díaz et al., 2004; Millett et al., 2012). Multiple forms of stigma (e.g., racism, xenophobia, homophobia, biphobia) manifesting at multiple levels (e.g., individual, interpersonal, structural) are thought to synergistically drive health disparities affecting GBM of color (Ayala et al., 2012; Díaz et al., 2001). Stigma related to race and sexual orientation predict poorer sexual health among Black and Latino GBM (Levy et al., 2014; Reisen et al., 2013), including HIV-risk behavior, lack of testing, lack of status disclosure, and among those living with HIV, a lack of antiretroviral adherence (Arnold et al., 2014; Ayala et al., 2012). Research suggests that multiple forms of stigma can have a compounded association with sexual health (Díaz et al., 2004). For instance, Latino GBM who report experiences of both racism and homophobia—as opposed to racism only, homophobia only, or neither—are more likely to report recent condomless receptive anal intercourse with a casual sex partner and be living with HIV (Mizuno et al., 2012).
The link between stigma and health extends beyond sexual health outcomes, as racism and homophobia are associated with numerous psychiatric symptoms, including anxiety, depression, and suicidality among GBM of color (Díaz et al., 2001; Hightow-Weidman et al., 2011; Reisen et al., 2013). Unless adequately coped with, stress related to one’s racial and sexual minority status may interact to drive mental health risk among GBM of color longitudinally. Perceived racism and sensitivity to rejection based on sexual orientation interact to predict subsequent difficulties with emotion regulation, depression, anxiety, and alcohol use among Black and Latino GBM (English et al., 2018). Further, in a probability sample of HIV-negative GBM, psychological distress was only associated with lower odds of HIV testing, condom use, and knowledge of pre-exposure prophylaxis (PrEP)—a medication that substantially reduces one’s risk of HIV infection—when perceived homophobia was elevated (Krueger et al., 2020). This accumulating research suggests that the interrelations between stigma, stress, mental health, and HIV risk are no mere co-occurrence, but rather, may represent syndemic psychosocial health processes.
Conceptual models of stigma and health, such as minority stress theory (Meyer, 2003), have attempted to highlight pathways that explain these links between stigma-related events in one’s environment (i.e., distal stressors) and health. Research building upon this framework suggests that living in a hostile, discriminatory context may trigger internal, health-eroding stress processes related to individuals’ minority status (i.e., proximal stressors), including identity concealment, anxious expectations of rejection, and internalized stigma (Hatzenbuehler, 2009). Internalized homophobia indeed predicts co-occurring elevations in mental health problems (i.e., anxiety/depression) and sexual health risk (i.e., sexual compulsivity) among HIV-positive GBM longitudinally (Rendina et al., 2017). Proximal stress, such as rejection sensitivity, also explain the link between distal stress and mental health among sexual minorities (Feinstein et al., 2012).
Intersectionality (Collins, 1990; Crenshaw, 1989) posits that multiple axes of power interlock to produce unique, often overlooked, experiences of oppression. Black and Latino GBM endure distinct types of stigma, beyond the general forms of homophobia endured by White GBM and racism endured by heterosexual people of color (Jackson et al., 2020; Sarno et al., 2015). Not only do GBM of color endure unique stereotypes (Calabrese et al., 2018), but they face intra-community stigma due to their subordinated position within two minority groups (Balsam et al., 2011). Specifically, GBM of color face (a) homophobia, religious persecution against lesbian, gay, bisexual, transgender (LGBT) people, and culturally bound gender norms in their majority heterosexual racial/ethnic communities (Ramirez-Valles, 2007; Sarno et al., 2015) and (b) racism, race-based sexual rejection and exotification, and Eurocentric norms within the majority White GBM community (Díaz et al., 2004; Han, 2007; Wilson et al., 2009). Experiences of intra-community rejection and betrayal are associated with identity adjustment difficulties, mental health problems, and sexual health risk (Balsam et al., 2011; Gómez, 2019; Han et al., 2015).
How might one adopt an intersectional framework to identify new treatment targets for GBM of color? Recent experience sampling research using a daily diary methodology suggests that negative intersectional experiences predict day-to-day distress among Black sexual minorities (Jackson et al., 2020)—and this fluctuation is mediated by identity conflict (i.e., one’s internal sense that their racial and sexual identities are incompatible; Sarno et al., 2015). These and other findings linking intersectional stressors to mental and sexual health (Balsam et al., 2011; Han et al., 2015) raise an intriguing prospect: GBM of color’s ability to cope with intersectional stress—in addition to traditional racial or sexual minority stress—can serve as a promising treatment target to improve their mental and sexual health. We relied upon this literature to imagine an emergent conceptual model of stigma-related stress and health among GBM of color (Figure 1).
Figure 1. Theoretical Model of Intersectional Stigma-Related Stress and Health Among GBM of Color.
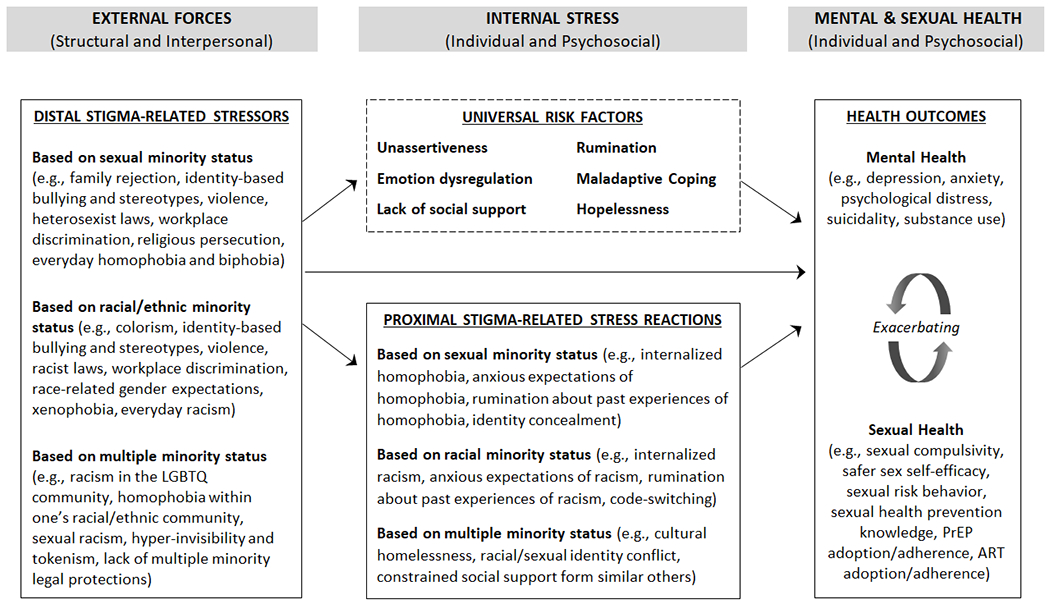
Note. This model was adapted from existing models (Hatzenbuehler, 2009; Meyer, 2003, 2015; Pachankis, 2015) to address the confluence of racial, sexual orientation, and intersectional stressors. To conserve space, universal risk factors were not examined as mechanisms within the present investigation. GBM = gay, bisexual, and other men who have sex with men; LGBTQ = lesbian, gay, bisexual, transgender, queer; PrEP = preexposure prophylaxis; ART = antiretroviral therapy.
If, as evidenced above, (a) racism, homophobia, and their intersection lead to internal experiences of stigma-related stress and (b) these factors drive mental health risk and HIV risk behavior among Black and Latino GBM, addressing stigma is critical to supporting the health and well-being of GBM of color. Although health equity cannot be achieved for GBM of color without the dismantling of structural oppression—a primary driver of HIV disparities—disrupting individual-level variables linking stigma and health may partially relieve the health burden endured by this group. It is therefore imperative to develop culturally-attuned treatments that empower GBM of color by supporting adaptive coping skills and resilience against these barriers.
Evidence suggests that health interventions can buffer against the health risks of stigma when tailored to address the experiences of homophobia among sexual minorities (Pachankis et al., 2015, 2020) and racism among people of color (Graham-LoPresti et al., 2017; Lee et al., 2011; Reid et al., 2014; Williams et al., 2009). Among interventions for GBM of color, however, few focus on racial stigma and none seek to build stigma coping to address the syndemic occurrence of mental and sexual health risk (Fish et al., 2016; Maulsby et al., 2013). A recent systematic review of sexual minority health interventions identified no treatments that assessed intersectional stigma or examined multiple forms of stigma within the same model (Layland et al., 2020). Treatments informed by intersectionality that address the established and emergent pathways between stigma, mental health, and HIV risk (Pachankis, 2014; Pan et al., 2020; Safren et al., 2011) may pose particular promise for addressing the syndemic health of Black and Latino GBM.
The Present Study
Due in part to experiences of stigma, US GBM of color are at disproportionate sexual health risk as compared to White GBM (CDC, 2017) and disproportionate mental health risk as compared to heterosexual men of color (Rodriguez-Seijas et al., 2019). To address these inequities, we piloted a 10-session intersectionally informed group therapy treatment that promotes Black and Latino GBM’s resilience to three types of stigma-related stress—racial minority stress, sexual minority stress, and intersectional stress—to address mental health risk, HIV-transmission risk, and their co-occurrence. The treatment was developed by modifying an existing one-on-one treatment to specifically address the unique needs, barriers, and contextual factors that drive mental and sexual health risk among young GBM of color.
Method
Treatment Adaptation
Guided by theoretical models of stigma-related stress (Hatzenbuehler, 2009; Meyer, 2003; Pachankis, 2014) and supported by empirical evidence (Pachankis, 2014; Pachankis et al., 2015), the original treatment—Effective Skills to Empower Effective Men (ESTEEM)—is a manualized, cognitive behavioral therapy (CBT) treatment developed to address stigma coping, mental health problems, and HIV risk among GBM (Burton et al., 2017; Pachankis et al., 2015). This treatment model is transdiagnostic in that it is designed to address young GBM’s co-occurring maladaptive behavioral patterns, including mental health and health-risk behavior, by disrupting the pathways through which stigma impairs health. The treatment was designed to be implemented by a therapist across 10 individually-delivered treatment modules, with home practice assignments between sessions.
Originally adapted from the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (Barlow et al., 2017), the ESTEEM treatment develops skills among GBM through a variety of CBT techniques, including motivation enhancement, emotion exposure, cognitive restructuring, mindfulness, and self-monitoring (Pachankis, 2015). A focus on sexual minority stress is infused into each technique, including the clinician’s didactic strategies (e.g., teaching the client about sexual minority stress), in-session experiential exercises (e.g., mindfulness about sexual minority stress reactions), and home practice (e.g., monitoring sexual minority stress reactions; Burton et al., 2017).
The original treatment was tested in a waitlist controlled trial among 63 GBM reporting depression, anxiety, and condomless anal sex (Pachankis, 2014; Pachankis et al., 2015), making it one of the few treatments to use CBT to improve GBM’s health by addressing their cognitive, affective, and behavioral reactions to sexual minority stress. One strength of the treatment is its ability to address multiple mental health conditions and behavioral health risks by building support against the very universal risk factors (e.g., social support, emotion regulation) and sexual minority stressors hypothesized to underlie these co-occurring outcomes (Pachankis, 2015). The ESTEEM treatment model did not directly target race-related stress or intersectional stress. Therefore, the present study aimed to assess the feasibility and acceptability of an adapted version of the treatment aiming to reduce the multiple stigma-related stress reactions relevant to GBM of color (Figure 1). Additionally, this treatment was originally delivered in one-on-one settings; however, group treatment modalities can help promote healthy peer norms, role modeling, and social connections that might be especially important in the social and sexual networks of GBM of color (Carlos et al., 2010; Young et al., 2018), who report smaller social networks and fewer dimensions of support than White GBM (Frost et al., 2016; Meyer et al., 2008).
Sources of Adaptation Guidance
The body of research on group treatments for Black and Latino GBM, though sparse, features promising developments and certain limitations that guided our work. For example, Many Men, Many Voices (Wilton et al., 2009) is a well-established, six-session group intervention that has been shown to reduce sexual risk among Black HIV negative or status unknown GBM and includes a session that helps participants “recognize how racism and homophobia are related to sexual and substance use risk behaviors” (p. 535). Siempre Seguiré (Bogart et al., 2021) is a more recent cognitive-behavioral group intervention that improved anti-retroviral treatment adherence and decreased medical mistrust and negative religious coping in response to stigma among HIV-positive Latino GBM. Regarding limitations, somewhat understandably, existing treatments for GBM of color tend to focus heavily on reducing HIV risk, but in doing so, may overlook the mental health problems that often accompany and exacerbate sexual risk. Second, many health interventions for GBM of color are limited to a single GBM subgroup based on race/ethnicity and serostatus (e.g., Black HIV-positive GBM; Bogart et al., 2018), which likely offer high cultural specificity and group cohesion, but may also result in a restricted scope of impact. Finally, many individual-level treatments for GBM of color focus on sexual health promotion and do not simultaneously highlight the external drivers of health disparities among GBM of color (Fish et al., 2016); such treatments may unintentionally contribute to a narrative that Black and Latino GBM are somehow at fault for the health inequities they face (Matthews et al., 2016).
Inspired by prior empirically supported group treatments for GBM of color (e.g., Wilton et al., 2009) and guidance on psychotherapy for individuals who are both racial and sexual minorities (Adames et al., 2018; Greene, 1997; Morales, 1989), we modified the original ESTEEM treatment to create a new pilot group treatment. Addressing the aforementioned limitations, this new CBT group treatment model (a) is designed to be flexible and responsive to participants’ lived experiences, allowing it to be implemented among various GBM of color subgroups (e.g., regardless of racial composition, serostatus, or cisgender/transgender status), (b) not only addresses sexual health problems, but also transdiagnostic mental health problems, and the intersection of these domains of risk, and (c) underscores to GBM of color that the drivers of their health disparities are located outside of themselves (e.g., racism, homophobia, intersectional stigma), while empowering them with agency, pride, and stigma resiliency.
Additionally, we reviewed literature on the unique needs and barriers of GBM, including GBM of color, in racially diverse urban areas with high rates of HIV infection among GBM of color. We also drew from qualitative interview data from 29 local GBM (n = 16 GBM of color) regarding experiences of stigma and community (Keene et al., 2017; White Hughto et al., 2017). This review led us to adapt the existing treatment to: 1) build skills related to coping with racial and sexual orientation stigma, 2) consider the ways that racism and homophobia can interlock to produce intersectional stress, and 3) take advantage of the ability of group-based treatments to reduce social isolation and foster healthy norms through peer support and modeling. These adaptations and corresponding justifications are expanded below.
Adaptation 1. Incorporating Race-Related Stress and Resiliency
Although approximately half of the participants in the original treatment trial were GBM of color, the treatment did not target all sources of stigma that GBM of color face. The pathways through which sexual orientation stigma impair health (Hatzenbuehler, 2009; Pachankis et al., 2008; Wang & Pachankis, 2016) are many of the same pathways generated by racial stigma (Graham et al., 2016; Mendoza-Denton et al., 2002). Therefore, we adapted all aspects of the original treatment protocol that focus on the effects of homophobia to also address racial stigma. Modifications included integrating content on race-related stress into the therapist manual (e.g., background research, training vignettes) and session materials (e.g., participant handouts, home practice). Because the effects of racial and sexual stigma represent syndemic precursors to HIV risk (Arnold et al., 2014; Ayala et al., 2012; Hatzenbuehler, 2009), targeting both forms of stigma could help reinforce GBM of color’s defenses against HIV transmission.
Adaptation 2. Addressing Intersectional Stress and Resiliency
Considering the distinct experiences, stressors, and strengths of GBM of color helped ensure that our treatment was culturally relevant. We adapted treatment elements that previously focused solely on the effects of homophobia (e.g., vignettes on minority stress, practice exercises, coping strategies) to encompass intra-community stress, the distinct stereotypes of GBM of color, and intersectional forms of proximal stress (e.g., identity conflict, intra-community invisibility, cultural homelessness). Also, whereas the original curriculum highlighted the strengths, creativity, and perseverance of GBM and lesbian, gay, bisexual, transgender, queer (LGBTQ) people, we updated these moments to underscore the contributions and resilience of Black and Latino GBM, and LGBTQ people of color across history (e.g., during the civil rights movement, Stonewall riots, and HIV/AIDS epidemic; Bost, 2018; Phillips & Olugbala, 2006). Finally, the therapists delivering this new model were required to have knowledge of intersectionality, including the ways racism and homophobia interlock to produce stigma-related stress among Black and Latino GBM.
Adaptation 3. Shifting to a Group-Based Treatment Modality
Modifications were made to transform the ESTEEM treatment into a group-based intervention. Select session components were revised for the group-based modality, such as adding opportunities for participants to share their perspectives, set goals, or discuss challenges with home practice assignments within pairs or trios. We also worked to mitigate privacy issues associated with group-based treatments (e.g., selecting the physical space for treatment delivery, allowing pseudonyms, emphasizing confidentiality at the start of each session). Group norms were developed and presented at the start of each meeting to support effective communication, build trust, and support balanced participation across group members. Finally, the original session duration was extended from 60 to 90 minutes to accommodate treatment aspects that would take longer to implement within a group context (e.g., review of home practice).
Participants
Study eligibility criteria required that participants: 1) identify as men, regardless of sex assigned at birth, 2) be 18 to 35 years old, given than young Black and Latino GBM have the highest rates of HIV infection (CDC, 2017), 3) expect residential stability within the study geographic area for six months, 4) identify as gay, bisexual, or queer, or report past-12-month sex with a man, 5) identify as Black and/or Hispanic/Latino, and 6) speak fluent English. Given the primary aims to study feasibility and acceptability, this study relied upon a non-clinical sample (i.e., eligibility for this pilot did not include mental health problems and sexual risk behavior).
The sample was composed of 21 GBM of color at baseline (Table 1), of which 17 (80.95%) completed the 3-month follow-up assessment (Figure 2). Participants received treatment across two sequential cohorts (n = 12 and n = 9, respectively). Their ages ranged from 18 to 34 years (M = 26.50, SD = 5.12). The sample was predominantly gay (n = 16; 76.19%), Hispanic/Latino (n = 17; 80.95%), cisgender (n = 20; 95.24%), and HIV negative (n = 19; 90.48%). Most participants reported an income of less than $20,000 per year (n = 14; 57.14%).
Table 1.
Demographic Characteristics of Study Participants (N = 21)
| Variable | n | % |
|---|---|---|
| Age | ||
| 18-23 | 4 | 19.05 |
| 24-29 | 11 | 52.38 |
| 30-35 | 6 | 28.57 |
| Gender | ||
| Cisgender man | 20 | 95.24 |
| Transgender man (FtM) | 1 | 4.76 |
| Sexual orientation | ||
| Gay | 16 | 76.19 |
| Bisexual | 3 | 14.29 |
| Queer | 2 | 9.52 |
| Race/ethnicity | ||
| Latino/Latinx (Hispanic) | 7 | 33.33 |
| White (Hispanic) | 5 | 23.81 |
| Black (Hispanic) | 5 | 23.81 |
| Black (non-Hispanic) | 4 | 19.05 |
| HIV status | ||
| Negative | 19 | 90.48 |
| Positive | 2 | 9.52 |
| Income | ||
| Less than $10,000 | 10 | 47.62 |
| $10,000 - $19,999 | 2 | 9.52 |
| $20,000 - $29,999 | 2 | 9.52 |
| $30,000 - $39,999 | 3 | 14.29 |
| $40,000 - $49,999 | 3 | 14.29 |
| $50,000 - $74,999 | 1 | 4.76 |
| Education | ||
| Some high school | 1 | 4.76 |
| High school diploma or GED credential | 2 | 9.52 |
| Some college or associates degree | 5 | 23.81 |
| Currently enrolled in college | 2 | 9.52 |
| 4-year college degree | 6 | 28.57 |
| Currently enrolled in graduate school | 3 | 14.29 |
| Graduate degree | 2 | 9.52 |
Note. FtM = female to male; HIV = human immunodeficiency virus; GED = General Educational Development.
Figure 2.
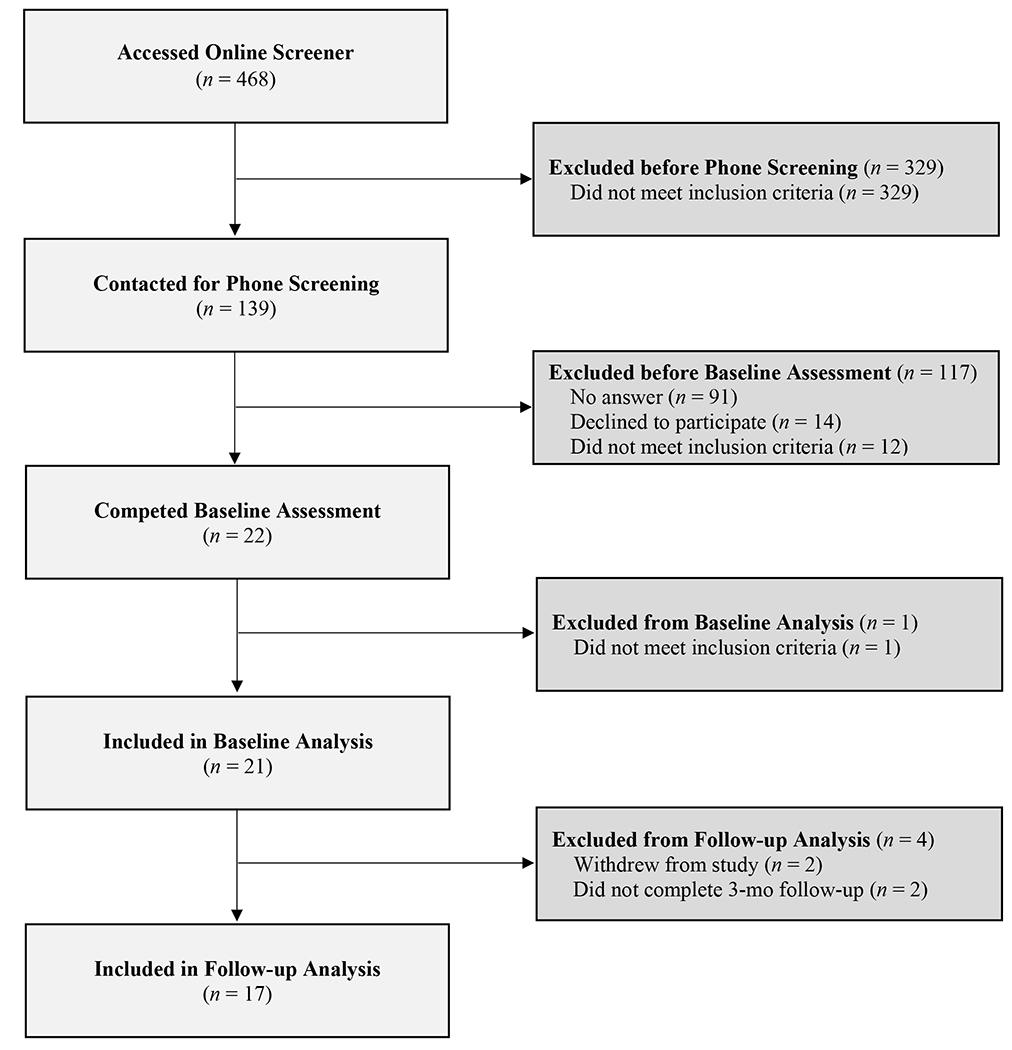
Flow diagram of participants’ progress through the study phases.
Recruitment and Procedures
We recruited for the study between September 2018 and February 2019 through local community organizations (e.g., flyers posted at community health clinics, LGBTQ community organizations, university LGBTQ centers) and online (i.e., advertisements posted to Grindr and LGBTQ Facebook groups). Potential participants received a link to a secure online eligibility survey. A research assistant called preliminarily eligible participants to describe study requirements, confirm eligibility, and gauge interest. Potential participants were informed that study participation included completing weekly 90-minute group treatment sessions over 10 weeks, assessments at baseline and three months post-treatment, and an exit interview. We screened 139 potential participants by phone; 21 enrolled in the study and provided informed consent (Figure 2). We conducted baseline and 3-month post-treatment assessments for each participant consisting of a phone interview and online, self-administered surveys regarding stigma-related stress, mental health, and sexual health. Within seven days of completing the 3-month post-treatment assessment, participants completed an exit interview about their experience.
The treatment was delivered across 10 sessions. Identical to the original ESTEEM format, sessions 1-2 introduced participants to the concept of stigma-related stress (in this case, sexual minority stress, racial minority stress, and intersectional stress), sessions 3-6 focused on emotion regulation and cognitive restructuring techniques that can help one cope with stigma (e.g., mindfulness, cognitive flexibility), and sessions 7-10 promoted behavioral skills to mitigate the effects of stigma-related stress (e.g., assertiveness practice, situation-based emotion exposures; Burton et al., 2017; Pachankis et al., 2015). At the end of each session, participants received a summary of the topics covered, skills learned, and home practice assignment; this summary was emailed to absent participants. Sessions were delivered in the evening at a predominantly Latino-serving federally qualified health center (FQHC) providing HIV-prevention and care services. Early career clinical psychologists delivered the treatment, including a Black queer man (cohort 1) and a Latinx gay man (cohort 2). Therapists were selected based on their (a) theoretical and practical knowledge of CBT, (b) experience leading group therapy, (c) clinical work with GBM of color, and (d) knowledge of intersectionality and theories of stigma-related stress. To support treatment fidelity within this pilot, treatment delivery was supervised by a clinical psychologist (last author and treatment developer) and a counseling psychologist (first author).
Research assistants coordinated all sessions—including signing in participants, setting up audio recorders and snacks, providing session materials (e.g., handouts, pens). They also contacted absent participants to assess the reason for their absence and encouraged participants to identify and troubleshoot barriers to treatment attendance, as appropriate. Participants were provided up to $340 for completing all study assessments and the exit interview, and to cover transportation to the sessions. The Yale Human Subjects Committee approved the study, which was preregistered at clinicaltrials.gov (NCT03464422).
Measures
We collected participant demographic information, including age, sex/gender, race, ethnicity, HIV status, income, and education. Participants also completed self-administered, psychometrically valid measures of stigma-related stress, mental health, and sexual health (Table 2). We derived the internal consistency for each measure, included in Table 2, by averaging the Cronbach’s alpha calculated at baseline and follow-up.
Table 2.
Pre-Post Changes in Study Outcomes
| Outcomes | Baseline Mean (SD)(n = 21) | 3-mo follow-up Mean (SD)(n = 17) | T-Test Effect Size Hedges’s g | Change in the expected direction |
|---|---|---|---|---|
| Mental health outcomes | ||||
| Depressive symptomsa | 22.10 (11.89) | 20.35 (12.01) | .15 | ✓ |
| Depression severityb | 11.00 (4.79) | 10.53 (6.07) | .09 | ✓ |
| Anxietyc | 12.05 (3.54) | 11.88 (6.07) | .03 | ✓ |
| Psychological distressd | 2.12 (0.87) | 2.05 (1.03) | .07 | ✓ |
| Suicidal ideatione | 4.33 (9.63) | 3.41 (8.20) | .10 | ✓ |
| Alcohol usef | 16.90 (6.57) | 17.53 (8.77) | .08 | --- |
| Sexual health outcomes | ||||
| Condom use self-efficacyg | 48.05 (16.33) | 49.24 (14.32) | .08 | ✓ |
| Sexual compulsivityh | 18.38 (7.11) | 18.18 (8.89) | .02 | ✓ |
| Recent PrEP usei | 0.31 (0.48) | 0.33 (0.49) | .04 | ✓ |
| Recent HIV-risk acts (baseline risk group)j | 13.67 (15.24) | 12.67 (11.84) | .07 | ✓ |
| Recent HIV-risk acts (full sample)k | 4.10 (10.12) | 8.29 (11.38) | .38 | --- |
| Identity-related stress mechanismsl | ||||
| Sexual minority stressors | ||||
| Sexual orientation rejection sensitivitym | 10.73 (5.66) | 9.92 (5.97) | .14 | ✓ |
| Sexual orientation concealmentn | 2.15 (0.97) | 2.01 (0.95) | .14 | ✓ |
| Internalized homophobiao | 1.53 (0.68) | 1.53 (0.78) | .00 | --- |
| Racial minority stressors | ||||
| Race-related anticipatory stressp | 5.26 (1.05) | 5.00 (1.39) | .21 | ✓ |
| Race-related ruminationq | 3.37 (1.54) | 3.06 (1.50) | .20 | ✓ |
| Race-related vigilancer | 3.29 (1.39) | 3.24 (1.30) | .04 | ✓ |
| Intersectional stressors | ||||
| Homophobia in racial communitys | 1.94 (1.70) | 1.82 (1.50) | .07 | ✓ |
| Racism in LGBT communityt | 2.02 (1.49) | 1.99 (1.49) | .02 | ✓ |
| Racism in close LGBT relationshipsu | 2.29 (1.56) | 1.95 (1.53) | .22 | ✓ |
Note. PrEP = preexposure prophylaxis; HIV = human immunodeficiency virus; LGBT = lesbian, gay, bisexual, transgender; GBM = gay, bisexual, and other men who have sex with men.
Center for Epidemiological Studies-Depression Scale (Radloff, 1977); α = .92.
Overall Depression Severity and Impairment Scale (Bentley et al., 2014); α = .91.
Overall Anxiety Severity and Impairment Scale (Norman et al., 2006); α = .90.
Brief Symptom Inventory (Derogatis & Melisaratos, 1983; Meijer et al., 2011); α = .95.
Suicidal Ideation Attributes Scale (Van Spijker et al., 2014); α = .89.
Alcohol Use Disorders Identification Test (Saunders et al., 1993); α = .93.
Safer Sex Self-Efficacy Questionnaire (Parsons et al., 2000); α = .96.
Sexual Compulsivity Scale (Kalichman & Rompa, 2001); α = .92.
Proportion of participants who reported any PrEP use over the past 3 months.
Past-90-day timeline follow-back interview (Sobell & Sobell, 1992). HIV-risk behavior was calculated as the number of past-90-day sex acts in which key harm-reduction strategies were not employed (e.g., condom, PrEP, viral load suppression).
Past-90- day timeline follow-back calculations restricted to participants reporting at least one sex act with HIV-transmission risk at baseline (n = 6).
Analyses restricted to HIV-negative participants at Time 1 (n = 19) and Time 2 (n = 15).
Gay-Related Rejection Sensitivity Scale (Pachankis et al., 2008); α = .94.
Self-Concealment Scale (Larson & Chastain, 1990) as previously modified for use with GBM (Schrimshaw et al., 2013); α = .89.
Internalized Homophobia Scale (Martin & Dean, 1992); α = .93.
Anticipatory Race-Related Stress—Psychological Subscale of the Prolonged Activation and Anticipatory Race-Related Stress Scale (Utsey et al., 2013); α = .73.
Perseverative Cognitive Subscale of the Prolonged Activation and Anticipatory Race-Related Stress Scale (Utsey et al., 2013); α = .89.
Racism-Related Vigilance Scale (Hicken et al., 2013); α = .94.
Heterosexism in Racial Ethnic Minority Communities Subscale of the LGBT People of Color (POC) Microaggression Scale (Balsam et al., 2011); α = .88.
Racism in LGBT Communities Subscale of the LGBT POC Microaggression Scale (Balsam et al., 2011); α = .88.
Racism in Dating and Close Relationships Subscale of the LGBT POC Microaggression Scale (Balsam et al., 2011); α = .88.
Exit Interviews
Trained research assistants conducted 90-minute semi-structured audio-recorded phone interviews, which included open-ended questions about barriers to participation, motivation for enrollment, and acceptability of treatment structure (e.g., session frequency, treatment duration, location; see interview guide within Supplemental Materials). Participants’ perspective on the content, home practice, and group modality were also assessed. Finally, we inquired about any benefits they attribute to participation (e.g., helpful learnings, new skills, behavioral changes).
Analytic Plan
To assess study feasibility, we examined the ratio of eligible-to-enrolled participants, rate of retention, number of sessions completed, and reasons provided for session absences. To assess treatment acceptability, we utilized codebook-based thematic analysis (Braun & Clarke, 2021) to guide our analytic method. First, all exit interviews were transcribed verbatim via a professional transcription service. Second, initial codes were generated via a multi-step process. The exit interview was designed to elicit responses about specific aspects of our treatment acceptability (e.g., “What things helped or interfered with you showing up to the sessions?”), targeted health outcomes (e.g., “How did the sessions influence on your sexual health behavior, such as condom use, talking about HIV status with your partners, sexual compulsivity, thinking about PrEP, talking to your doctor about your sexuality?”) and our theory of change (e.g., “How did the sessions influence how you cope with stress?” “How did the sessions influence the way you see yourself as a person of color?”). Thus, the majority of the thematic topic areas were pre-determined (i.e., most codes addressed a specific interview question), reflecting a deductive thematic analysis approach (Braun & Clarke, 2021). However, during the process of data familiarization in which the first and fourth authors reviewed all transcripts, additional emergent codes were identified and categorized into larger themes. The first author developed the final codebook, which included all necessary concept codes and a coding system to assess the prevalence of various participant sentiments. Third, transcripts were reviewed and double-coded, and the presence of each code was counted by the first, fourth, and fifth authors. Disagreements between coders were resolved as they arose. Fourth, the resulting themes were reviewed by the first and last author for their relevance to the acceptability of the pilot treatment. Consensus was achieved and all findings pertinent to treatment acceptability are reported below.
The researcher is neither a neutral nor objective player within the process of generating and transmitting scientific knowledge (Levitt et al., 2020; Starks & Brown Trinidad, 2007) and our research team is no exception. Even after implementing conventional protections against the influences of researcher bias (e.g., double coding of data, engagement in researcher reflexivity during analysis and interpretation), our team’s preconceived assumptions, personal values, unconscious biases, and cultural worldviews likely influenced qualitative coding and interpretation. This fact is not altogether problematic; when sufficiently identified, interrogated, and acknowledged, researcher subjectivity can enhance rather than detract from the rigor of scientific research (Tufford & Newman, 2012). Towards that goal, we acknowledge that our research team entered this work with a shared belief that (a) links between stigma and health can be attenuated via intervening at the individual level and (b) psychotherapy—and the ESTEEM model, in particular—has the potential to achieve this. Our team was predominantly composed of sexual minorities and can be described as highly educated and predominantly (Non-Hispanic) White. The delivery of the treatment as well as the process of data analysis, interpretation, and results compilation and presentation was led by a GBM of color. Our team members made explicit our core values, many of which can be described as feminist, anti-racist, sex positive, and/or decolonial in nature. Further, many team members have personal connections to aspects of this project (e.g., personal encounters with minority stress, experiences delivering or receiving therapy, residential history near the location of the pilot). These subjectivities and others undoubtedly supported and shaped how we appraised and coded qualitative results. The authors involved in each of the above steps had formal training and prior experience with qualitative research, which provided our team with the foundational tools and guiding principles to identify and reflect upon our individual and collective presuppositions regarding the study results.
Treatment acceptability was further assessed through analyses of quantitative data. After computing descriptive statistics of demographic and outcome variables, we performed t tests to assess changes in stigma-related stress—to capture any improvements in stigma coping—comparing mean baseline scores with mean 3-month post-treatment scores. We similarly examined pre-post changes in mental and sexual health. We focus our quantitative analysis on effect sizes and an examination of the overall pattern of changes, as this pilot investigation is not powered to detect significant treatment effects, does not rely on a clinical sample, and is not intended to serve as a test of treatment efficacy. When possible, we calculated Hedge’s g effect sizes to highlight the relative effect sizes across study outcomes because, unlike Cohen’s d, Hedge’s g provides unbiased estimates, even for smaller samples (n < 20; Lakens, 2013).
Results
Treatment Feasibility
We examined four metrics of treatment feasibility. First, we considered the eligibility-enrollment ratio: Of the 35 individuals deemed eligible for enrollment based on the information they provided during our online and phone screeners, the majority (n = 21; 60.00%) elected to participate in the treatment. Others declined due to not being interested in the treatment (n = 7; 20.00%), scheduling conflicts that prohibited participation (n = 5; 14.29%), concerns about the time commitment (n = 1; 2.68%), and the location being inconvenient (n = 1; 2.86%). Second, we calculated the number of sessions completed. Twenty of the 21 enrolled participants (95.24%) attended at least one of the ten treatment sessions. Most of these 20 individuals completed at least half of the treatment sessions (Mdn = 5; IQR = 7), with 10 (50.0%) attending eight or more sessions. Third, our high rate of retention provides evidence of feasibility: During the course of the study period, two participants withdrew, yielding 90.48% retention at 3-month follow-up. The present trial exceeds acceptable and expected rates of session attendance and retention in group therapies (Yalom & Leszcz, 2020), including with GBM of color (e.g., 81.6% retention at 4-month follow-up, 73.2% retention at 3-month follow-up; Bogart et al., 2021; Wilton et al., 2009).
Finally, to further probe treatment feasibility, we reviewed the reasons that group members provided for session absences. Nearly all absences were attributed to reasons unrelated to the treatment (e.g., illness, travel, work conflicts). That said, some barriers to participation were noted within the exit interviews. One member implied that guilt about missed sessions dissuaded him from returning to the group after absences, even though the session conflicts were pre-existing and made known to the group therapist. Another participant reported missing treatment sessions due to his discomfort with another participant, with whom he had a relationship. Finally, although compensation was provided for transportation, one participant reported being absent due to not having transportation access. Overall, barriers to participation were rare and those reported were not common across participants, suggesting that the treatment was highly feasible for this sample and setting.
Treatment Acceptability
Exit interviews, completed with 16 study participants (76.19%), were reviewed to assess overall treatment acceptability. Below, we summarize the findings pertaining to (a) motivation for enrollment, (b) treatment structure, and (c) cognitive-behavioral skill acquisition, supported by select participant quotes to exemplify informative participant perspectives. To indicate how many participants endorsed a particular theme, we use the terms (Chang et al., 2009): some (3-5 respondents); many (6-8 respondents), most (9-12 respondents); nearly all (13-15 respondents).
Engagement Motivated by Desire for Connection and Curiosity about Therapy
Qualitative data suggest participants were motivated to engage and that this motivation was driven by two overarching goals. The most common reason for enrollment, which was reported by most participants, was an interest in connecting with local peers for friendship and learning. For example, a 28-year old Black/Latino gay participant stated, “My initial intention was to learn more about how other gay men of color experience their lives and how do they deal with these two levels of prejudice.” Many participants shared that they were motivated by their curiosity about therapy, such as a 29-year-old Black/Latino gay man, who stated, “I’ve never been to therapy so I thought a group therapy situation like this would be a great entryway for me to sort of get over my anxiety about therapy and get my own therapist.”
Treatment Structure Was Deemed Appropriate and Supported Participation
Many participants reported that the treatment duration was ideal. Many others stated that they wished it was slightly longer, such as the 25-year-old Black gay man who reported, “it didn’t even feel like ten [weeks] because every week I was actually looking forward to it. So, I think it was either just enough or a little more would have been good because I enjoyed it.” Notably, no participants reported that the 10-session duration was too lengthy.
Regarding the length of each meeting, most participants reported that the 90-minute session duration was appropriate, as reflected by the response below.
I think [the length is] perfect. You don’t even get counseling that long, especially for something offered to you free […]. I think that was sweet and wonderful. With therapy, I go to therapy, it’s about an hour and to see a psychiatrist, they only give you 30 minutes. – Latino gay man, age 33
That said, some participants felt that decreasing the session length (e.g., to 60 or 75 minutes) might have been preferable.
Regarding session timing and frequency, our decision to hold treatment sessions once-per-week was deemed acceptable by many participants. For example, a 33-year-old Black/Latino gay man shared, “Once a week was good […] it worked out perfectly for me. Anything more might’ve been a little hard to get to, but I liked the amount of time we would spend in there.” Two participants noted potential benefits of having sessions twice per week (e.g., greater continuity) such as a 34-year-old Black gay man who stated, “seemed like [when meeting] once a week, there was always something new and then whatever we had to tackle with the last thing got forgotten or brushed away.”
Group Format and Composition Increased Learning and Decreased Loneliness
The benefits of in-group similarity and diversity.
Nearly all participants reported that the group format was beneficial, with most acknowledging the way this modality served to highlight key similarities and differences among the participating GBM of color.
We all came from different places. We were all doing different things and at different points in life, but we still have this same I guess thing that brought us together, so I thought it was cool hearing their stories, but not being the same kind of life. – Latino/White bisexual man, age 23
One 25-year-old Latino gay man noted how the group composition—composed of those who are similar, but also diverse—may have driven participants’ desire for the treatment to continue beyond 10 sessions, stating “I think by the end, the people […] like actually lamented leaving to an extent because of the connection that was shared, even through people sharing their experiences [were] from all these different backgrounds in one room.” Most participants noted that it was the mix of similarities and differences that they found helpful, suggesting that a group that is too homogenous or heterogeneous may have been less interesting and efficacious.
The group as an opportunity for peer-to-peer learning.
Most participants underscored how much they learned from other group members, noting that it was helpful to hear from group members who had faced—and often, overcome—the very struggles they were presently facing:
[Some participants] shared information about coming out to their parents, and this is something I have not done yet, and I was able to hear from other people about how it goes. […] I can remember there was one participant that was telling us that he came from a very conservative place, and that even his family is very conservative. He was saying that he was not out yet and he couldn’t find a way to do that. Of course, this is a very sad thing to think about. On the other hand, I remember that all the participants shared that they’ve come out and that coming out was hard at the start but that their families and friends got used to it over time. It was just good to hear. – Black/Latino gay man, age 28
Underscoring this impact of peer-to-peer learning, a 28-year-old Black/Latino gay man pointed out, “I learned more from the experiences of the other participants than with the sessions themselves, I mean with the therapist.”
The benefit of an intentionally intersectional treatment space: Feeling less alone.
We further examined if and how the group-based model improved the participants’ psychosocial well-being. The most consistent finding was that many participants felt less alone as a result of participation, with the many members mentioning this sentiment without prompting. A 28-year-old Black/Latino gay man shared this perspective, noting, “my perception that I’m not alone and that the problems I face sometimes, they are not unique to me is something that I really appreciate. That’s something I can say I learned.” Underscoring how this benefit would have been lost if this had been a one-on-one treatment, a 33-year-old Black/Latino gay man participant said, “I really liked listening to other people’s answers and responses and their problems, not just my problems. It made me feel less alone. It was pretty cool to see what other people had to say.” One participant provided an example of this learning.
I was talking about […] homophobia, since my family like they’re very, very bigoted, and like homophobic and racist, and all of that. I got the perspective of other Latino men […] they would say that oh, they were raised the exact same way […] it made me feel like I wasn’t alone. [Another participant] spoke about stuff that he had to deal with in the past […] his family […] hearing them talk about it in the group sessions was like really valuable to me. – Black/Latino bisexual man, age 18
Many participants highlighted how being around similar others led to positive affect and greater perceived ability to cope with intersectional stigma. For example, the below participant notes the benefit of seeing his challenges mirrored amongst others in the group.
Seeing different scenarios and different people talking about their situation definitely helped me maybe understand or maybe just feel better about my current situation. Not comparing myself in a bad way, but in a sense that I’m not alone. It just made me feel more comfortable. […] that I am LGBT and I am a person of color […] It’s something it’s helped me cope with. The [treatment] per se helped me cope with it. Seeing those other guys—other people struggling with it. – Latino gay man, age 27
This participant went on to share how the intersectional focus—and in particular, the group being composed of GBM of color—helped him feel a newfound sense of community connectedness.
I’m not very involved actively in the community. […] Putting myself out socially, it’s hard for me sometimes […] just because of myself, my own insecurities and stuff. But I am glad that there’s an active [city specified] LGBT community that is there to support. […] That made me feel better knowing that there’s a lot of people in [city specified] that are having a similar issue. […] What helped me be comfortable initially was the fact that they were all people that – LGBT people that – of color that made me feel more secure at being there and stuff. – Latino gay man, age 27
Drawbacks of group format.
Although feedback regarding the group format of the treatment was predominantly positive, some participants noted the challenges associated with this modality. For example, some participants reported feeling discomfort with one of their fellow group members based on factors such as the other member’s participation style or racial identity (i.e., presence of a White-identified Latino participant). Whereas the group made most members feel more connected to others, it left one participant feeling estranged from others. For example, one 34-year-old Latino/White gay man shared, “I felt like I didn’t belong there, so even though I was LGBTQ and Latino, when I was surrounded by that group, I felt like at times like, ‘What am I doing here?’” Additionally, many participants noted some difficulty participating in the group, such as participants who expressed feeling socially anxious and self-conscious.
I personally have a little bit of social anxiety […]. The group study was a little bit sometimes difficult for me to fully express what I’m feeling at the moment. There’s always that little wall: “What will people think of me?” or whatnot, which shouldn’t really matter, but I still felt in that scenario a little bit limited to say certain things […]. Sometimes it’s a little hard to express one’s self in a group setting. – Latino gay man, age 27
This participant went on to note, however, that the group became, “more comfortable during the weeks […]. At the beginning, it was more awkward and at the end, it was definitely more of a conversation with people that are in the same boat. It felt more comfortable at the end.”
Home Practice Facilitated Learning Outside of the Therapy Room
Overall, participants did not report finding the weekly home practice assignments to be burdensome. In fact, when asked about what they learned from the treatment, many participants mentioned learning from the assignments. For example, one 33-year-old Latino gay man participant reported, “I did [learn things], you guys gave study papers and things to talk about and experiences and real life situations and you can read it and put it together, think about situations you experienced, and figure it out.”
One participant reported that the home practice assignments were too simple and two found them too complex or burdensome, but these reports were outnumbered by feedback suggesting homework assignments were acceptable in terms of difficultly and required time.
[The homework] was not too much, but […] what we did have was challenging just emotionally or personal—on a personal level. It was interesting, but it was a good challenge. It wasn’t something completely—that I wasn’t capable of doing. […] I enjoyed sharing our homework. – Black/Latino gay man, age 33
Some participants appreciated that some learning took place outside of the group context. The aforementioned participant who discussed having social anxiety found the treatment’s home practice to be particularly beneficial.
[…] sometimes when they ask you a question and put you in the spotlight in the moment, it’s hard to put your thoughts together, especially in a group setting. I really did appreciate that they gave us time to write something down. They gave us a week for homework. That really helped me also understand myself better because most of those questions may help you with that, help us with that. Writing them down, what I felt and all of that really did help me a lot. I really appreciated that […]. – Latino gay man, age 27
Learning Cognitive-Behavioral Strategies Supported Emotion Regulation
Consistent with its theoretical framework, the treatment was successful in fostering the development of cognitive-behavioral skills among young Black and Latino GBM. As a result of the group, (a) most participants reported more emotional awareness, (b) most reported more mindful, present-focused awareness, and (c) some reported more cognitive flexibility, as reflected within the below quotes:
One thing that I still do is that we learned to, sometimes it’s best to say to yourself how you are feeling. So if you’re feeling nervous you accept the feelings that I’m nervous, I’m afraid, or something like that to help overcome the feeling. So, that’s what I do from time to time. – Black/Latino gay man, age 29
What really helped me was the mindfulness part. […] That really helped me and I still do it. I sometimes forget it to be honest, but I still do it and I remember mindfulness. It comes to my head and then I shut my thoughts down for a moment and my stress. Definitely it helped me with that, mindfulness. – Latino gay man, age 27
[…] the therapist taught us to interpret things in a different way, taught us that not always the first thing you think about something is the only possibility to interpret it. […] that was the one that got more of my attention. – Black/Latino gay man, age 28
These quotes suggest that CBT provided a suitable theoretical foundation and set of techniques through which to deliver a stigma resiliency treatment to young Black and Latino GBM.
Is this Treatment Aligned with Our Target Outcomes?
To further evaluate the acceptability of this pilot treatment, we examined our qualitative and quantitative data to assess participants’ self-reported changes concerning our main treatment targets: mental health, sexual risk, and stigma coping. To accomplish this, we again provide participant quotes to exemplify the themes derived from our qualitative analysis across each outcome domain. Within these domains, we also provide quantitative data results to corroborate the qualitative findings.
Table 2 summarizes participant scores across study outcomes at baseline and three months post-treatment, including effect sizes and whether outcomes changed in the expected direction. The overall trend is clear: 17 of the 20 study variables changed as expected. Although this trend is promising, our pilot study is not powered to test efficacy. Rather than presenting quantitative data as suggestive of reliable, significant change—as is typical within larger treatment studies—we instead provide this data to underscore treatment acceptability. All effects can be characterized as small or very small based on contemporary benchmarks (Sawilowsky, 2009). As the present study features a community sample of young Black and Latino GBM, effect sizes reported here are likely to be smaller—and less clinically meaningful—compared to the effect sizes one would expect to find among GBM of color at acute risk for co-occurring mental and sexual health problems.
Mental health improvements attributed to stigma coping and connection.
Nearly all participants reported perceived change across one or more mental health outcomes, including reductions in depression, anxiety, and general stress.
I felt happier when I left. I just felt more accomplished. I did feel like a better person […] like managing stress is a little easier now and I’m more aware and cognizant of things that stress me out. And how to deal with them and just knowing that it’s not the end of the world to be stressed […] that it’s manageable. –Black/Latino gay man, age 33
Two participants made a point to highlight that the treatment helped them reduce substance abuse.
I also have cut down on substance abuse because I am just sort of sitting with discomfort. Which was the reason why I abused. So that has helped. […] I definitely feel more comfortable sort of sitting with it instead of resorting to something that’s gonna like numb and like think of something else. I mean I still kinda do it a little bit, but I definitely am a bit more conscious of it and have chosen not to […]. – Black/Latino gay man, age 29
Many participants attributed their improved well-being to learning new ways to manage myriad, intersecting forms of stigma—and again, to learning that they are not alone in their experiences.
[…] us being minorities, African, Latino, male, being in White America, being judged upon being gay, being different, stuff like that. […] In a good way, [the treatment experience] lifted my spirit, made me think about things and how to manage now. I’ve always managed, but it gives you a different perspective […] like okay, I’m not the only one who thought of this. […] I’m better now. I can say, yeah, you guys released a lot for me. I needed someone to talk to and even if it was a group session, it still helped me cope with depression, anxiety, it took away […]. – Latino gay man, age 33
Between baseline and 3-month follow-up, participants demonstrated decreased depressive symptoms (g = 0.15), depression severity (g = 0.09), anxiety (g = 0.03), psychological distress (g = 0.07), and suicidality (g = 0.10). Contrary to expectation, mean alcohol use increased (g = 0.10) at three months post-treatment.
Sexual health improvements from a mental health treatment.
Most participants reported perceived change in their sexual health. Many reported decreased sexual risk behavior and increased intentions to engage in harm reduction, whereas some participants reported greater knowledge of PrEP and general sexual health.
My behaviors, sexually specifically, were better. Better as in I’m not out there trying to look for something else, trying to look for – expose myself maybe in situations that I don’t really wanna be in. Things that I’ve done in the past recklessly, I’m sure now that I won’t be able to – I won’t do. After the sessions, it helped me even more to calm down that sexual craziness that was going on in my life at one point. – Latino gay man, age 27
Oh, to be honest, the [therapist], he talked about STDs—was very interesting too and very useful. […] I didn’t know much about PrEP and he provided us information on PrEP and that was interesting. – Black/Latino gay man, age 28
Participants reported perceived change regarding open communication about sexual health with sexual partners and comfort with their sexuality.
After having participated in the survey, it was important for me to just kind of check in on my partner and say, “Hey, would you like to think about getting tested again together because I know it’s been a long time?” – Latino gay man, age 25
[…] they were very body-positive, very – also like the sex positive, you know they were like it’s not a problem. It’s not a bad thing to have sex and stuff. That made me feel about – feel about myself, a lot better. – Black/Latino bisexual man, age 18
Participant scores changed in the expected direction for condom use self-efficacy (g = 0.08) and sexual compulsivity (g = 0.02). We also saw changes in the expected direction for recent PrEP use (g = 0.04), such that more participants adopted PrEP (i.e., reporting past 90-day PrEP use at follow-up, but not baseline) than discontinued it (i.e., reporting past 90-day PrEP use at baseline, but not follow-up). Recent HIV-risk behavior decreased among those reporting past 90-day risk behavior at baseline (g = 0.07), but not among the full sample.
Increased pride and decreased stigma-related stress.
Many participants reported that the treatment helped them cope with internal and external manifestations of stigma. Notably, some discussed improvements in their ability to cope with sexual minority stress and some mentioned racial minority stigma coping:
[…] being in that group circle, I noticed a lot of the things that I was taught was incorrect, and it […] really helped me to let go of those like homophobic […] tendencies. […] I used to think that being gay was a bad thing, […] that I should be ashamed of myself, that I should try and be straight, and that I shouldn’t hang out with like other gay people, and yeah, now it’s like the exact opposite […] like a whole 180. […] I loved it and it helped me a lot with like me internalized homophobia, and […] I came out to my mom. I came out to a lot more friends, and now I’m not like quote-unquote in the closet. Now […] I’m just living my best life, as people say. The group really helped me with that too […] I’m [Latino heritage specified], I’m an openly gay man, and that group really helped me to be comfortable saying that. Like previously I would never say that to just anybody. It would be like a selective few people […] and nobody else. – Black/Latino bisexual man, age 18
You guys showed me to be proud, strong, and stand for who we are. I was a little ashamed, I’m a Latin male and especially with Trump in the realm and Republicans and the topic on Mexicans. We’re still all Hispanic Latin. We have to show we’re people—we have pride, we can persevere […]. – Latino gay man, age 33
Participants also responded positively to our intersectional approach to stigma. This focus seems to have provided valuable opportunities for many participants to better cope with stigma at the intersection of their sexual and racial identities.
There was another guy as well who talked about his experience in a [Latino nation specified] context […]. It was the comment that I could relate to the most as a [Latino ethnic heritage specified] person because I kind of understand like the elements of machismo and Latin culture and the family dynamic, I guess, of family members that are more heteronormative, I guess, or like homophobic, and have if anything, just less subtly implied prejudices that you have to navigate, as well as like religion as a component and all of that that comes to Latin culture and the gender role there. –Latino gay man, age 25
Our attention to intersectionality not only increased many participants’ sense of sexual and racial minority pride, respectively, but also supported a more integrated sense of racial/sexual identity.
It really did help me cope with the reality that I am LGBT and I am a person of color. […] I’m a minority of minorities. […] The study made me […] feel more comfortable in a way, because I saw the others that were there that were also people of color. It just made me feel more comfortable with myself. – Latino gay man, age 27
Quantitatively, participants demonstrated change in the expected direction for rejection sensitivity (g = 0.14) and concealment (g = 0.14); internalized homophobia was unchanged (g = 0.00). Participant scores decreased on all racial minority stress outcomes, including decreased anticipatory stress (g = 0.21), race-related rumination (g = 0.20), and race-related vigilance (g = 0.04). Assessments of intersectional stress also demonstrated decreases as expected: homophobia within one’s racial/ethnic community (g = 0.07), racism within the LGBT community (g = 0.02), and racism in dating and close relationships (g = 0.22).
Discussion
We adapted a manualized, transdiagnostic, CBT-based treatment (Pachankis et al., 2015) to create a group-based treatment to address stigma coping, mental health problems, and HIV risk among GBM of color. Qualitative and quantitative findings suggest that the treatment was feasible and acceptable—and possesses potential for efficacy upon further testing and implementation. Specifically, a review of key metrics (i.e., eligibility-enrollment ratio, session completion, reasons for session absences, rate of retention) suggests high treatment feasibility. Participant interviews revealed high acceptability regarding motivation for enrollment, treatment accessibility and structure, and cognitive-behavioral skill acquisition. Additionally, of the 20 study outcomes, 17 changed in the expected direction between baseline and 3-month follow-up. Although future research is needed to determine whether this trend is reliable and clinically significant among the target population, these data provide initial support for the acceptability of a new treatment to improve GBM of color’s mental and sexual health by building intersectional stigma coping skills.
Study findings build upon the promise of the original ESTEEM model, offering further evidence that CBT principles integrated within theories of stigma-related stress can be successfully used to empower individuals who face intersectional stigma. Indeed, exit interview data suggest that participants not only learned CBT skills, but that that these evidence-based techniques enhanced their ability to navigate general and stigma-related stressors within their everyday lives. This treatment builds upon the ESTEEM treatment and other health interventions that focus on minority status (Fish et al., 2016) by building stigma coping skills across multiple, intersecting domains of oppression within a single treatment—and may be the first studied stigma-coping intervention for sexual minorities to do so (Layland et al., 2020). Notably, the largest effect sizes demonstrated within this pilot concerned three race-related treatment targets that were added as a part of the treatment adaptation: race-related anticipatory stress, race-related rumination, and racism in close LGBTQ relationships. More generally, by including the multiple and unique forms of stigma that characterize the lives of GBM of color, this treatment provides participants with multiple ways to benefit from the treatment. Whereas some participants may have benefited most from learning to cope with homophobia, others may have found the most benefit in learning to cope with racism. Others still may have benefited from unique attention to the ways race and sexual orientation co-construct their lives and imbue oppression (i.e., intersectional stigma).
One innovation of the present treatment was its group-based delivery. Adopting a group format allowed us to benefit from many of Yalom’s therapeutic factors (e.g., interpersonal learning, imitative behavior, information giving; Yalom & Leszcz, 2020), as evidenced by participant reports that the group format helped promote peer support, role modeling, and social learning. Refinement of this group-based model can continue to consider how to best support the therapeutic experience of introverted and socially anxious group members and those who might feel disconnected from other group members. Additionally, future research can identify how to best navigate the potential for pre-existing relationships to produce barriers to treatment.
Participant feedback also suggests that group composition—which was restricted by age, race/ethnicity, and sexual orientation—may be a critical ingredient in building the resiliency of GBM of color. The unique opportunity to converse, take risks, and learn alongside other Black and Latino GBM—who were both similar to and different to one another—was likely the reason the group helped so many participants feel less alone. The prominence of this theme suggests that, in part, the treatment promoted well-being by leveraging the therapeutic factors of group cohesiveness, universality (e.g., a sense of relief due to feeling understood and similar to others, as opposed to an outsider), and installation of hope (Yalom & Leszcz, 2020). Although contact with others who share one’s stigmatized identity may be ameliorative for all individuals coping with stigma, it may be particularly helpful to those within a doubly marginalized community like GBM of color. Peer influences have been shown to be important to the sexual health of GBM of color (Young et al., 2018), who consistently report fewer supports than White GBM (Frost et al., 2016; Meyer et al., 2008). Thus, group models informed by intersectionality might provide the social mirroring and support many GBM of color desire. This need may be most pronounced in certain geographic locales, such as those that provide few venues catering to Black and Latino GBM clientele and whose GBM venues are sites of racial exclusion and elitism (Keene et al., 2017).
Limitations and Future Directions
The original ESTEEM protocol was developed via interviews with experts and community stakeholders to gain insight into treatment components to address sexual minority stress. This pilot, however, was developed, executed, and evaluated without the benefit of such outside input. As a result, every step of our research process (e.g., treatment adaptation and implementation, data collection and analysis, interpretation and dissemination of results) was highly dependent upon our team’s strengths and vulnerable to our limitations. Researcher positionality and subjectivity is neither uniformly an asset or liability (Tufford & Newman, 2012)—and a careful consideration of our team’s diversity, lived experiences, knowledge bases, and cultural worldviews yields both positives and negatives. The team that executed this pilot featured multiple Black GBM and multiple Latino GBM; was predominantly composed of sexual minority individuals; was highly attuned to issues of identity, stigma, and power; and featured multiple members with expertise on mental health, HIV prevention, intervention development, and intersectionality. On the other hand, collectively, our team (a) featured greater knowledge about sexual minority stress than racial minority stress and (b) did not mirror certain relevant aspects of the community we impacted—e.g., our team was, on average, older and more highly educated than the research sample; our final sample was predominantly Latino/Hispanic whereas our team is predominantly White and non-Latino/Hispanic. Greater overlap between the cultural identities of our research team and the target population may have yielded further community-resonant treatment adaptations. Also, although we did consult existing research evidence to guide adaptations from the original ESTEEM treatment, a more structured process (Wingood & DiClemente, 2008) might have yielded additional modifications and stronger initial effect sizes, as it has for adaptations of ESTEEM to other populations of GBM (Pan et al., 2020).
Our pilot was delivered at one facility in one small city in the Northeast. Small cities are shaped by unique structural barriers (e.g., fewer community resources and peer-level network factors), placing GBM in small urban areas at higher HIV risk (Rosenberg et al., 2016). Participants identified benefits of our specific treatment site (e.g., easy to travel to, broad community health mission was seen as non-stigmatizing and discreet), but also limitations (e.g., neighborhood reputation for elevated crime, high nearby foot-traffic that could undermine discretion). Future research should test treatment efficacy in larger cities or rural areas, within US regions with more structural stigma (e.g., the South), and across diverse treatment sites (e.g., LGBTQ community centers). We relied upon a non-clinical community sample for this pilot and included multiple incentives for participation. It therefore remains unclear to what extent our findings might be reproduced among Black and Latino GBM with greater mental health challenges or who do not benefit from the retention procedures featured within our study (e.g., payment for transportation, follow-up calls to troubleshoot barriers to treatment attendance). Also, our sample was disproportionately Latino, HIV-negative, cisgender, and fluent in English. Future research may examine treatment efficacy among GBM of color who are non-Hispanic, transgender/gender non-binary, or living with HIV. A question remains as to whether restricting the group by race/ethnicity, serostatus, or other personally relevant factors might strengthen or detract from the success of this model. Offering the treatment in other languages is warranted to increase accessibility. Future research might extend this model to exclusively Spanish-speaking Latino GBM, who face xenophobic stigma, linguistic barriers to GBM community connectedness, and other distinct health threats (Ramirez-Valles, 2007).
Other methodological features constrain the conclusions that can be drawn about this group treatment’s impact and theorized mechanisms (e.g., internalized homophobia). Pilot studies featuring small samples and significant attrition at follow-up are not adequately powered to detect significant effects. Second, the open pilot nature of this treatment prohibited our ability to establish causality. Future research with this treatment models ought to consider a randomized controlled trial, as no such trial exists of such a treatment with GBM of color. Beyond rigorously examining the efficacy of this treatment, such a trial could also investigate whether the group format translates into increased efficacy as compared to a one-on-one modality, as both offer distinct benefits (e.g., in individual treatment missed sessions do not result in missed content). Third, this study did not assess change in proximal (i.e., internal) manifestations of intersectional stigma. Future studies might assess whether this treatment decreases theorized intersectional manifestations of proximal stress (e.g., identity conflict, intra-community invisibility, cultural homelessness). Also, as this treatment seemed to build connections with similar others to reduce loneliness, measures of connection to GBM of color are warranted in future tests of this treatment. In fact, future trials may benefit from greater overall attention to change in positive aspects of well-being (e.g., life satisfaction, positive affect, social support, identity integration, meaning in life).
Although participants qualitatively report that the treatment reduced alcohol use and sexual risk behavior, the quantitative pre-post analyses partially contradict these findings. Perhaps frequency-based nature of the behavioral data, which is highly sensitive to extreme outliers in small samples, drove these inconsistent findings. Compounding this issue, sex risk was not required per study eligibility and only a minority of the sample (n = 6; 28.6%) reported one or more HIV-risk acts at baseline, constraining our ability to demonstrate improvement in HIV transmission acts in the full sample. Further, alcohol consumption and sexual behavior are vulnerable to seasonal effects—with increased drinking, sexual activity, and sexual risk during summer and/or autumn among some demographics (Carpenter, 2003; Shah et al., 2007; Wellings et al., 1999). This may explain why participants reported increased alcohol use and sexual risk at follow-up (in May and August) than at baseline (in November and February). Future treatment refinements or more targeted eligibility might enhance ability to address behavioral outcomes.
Together, these findings demonstrate the possibility for targeted treatments to support young Black and Latino GBM in navigating and coping with intersectional stigma in a manner that fosters their psychosocial health and well-being. Despite our belief in the promise of this intervention, any comprehensive public health effort to eradicate these health inequities must prioritize dismantling the unfair systems of power that drive and maintain them. Although our work to build Black and Latino GBM’s resiliency to stigma can equip them to better cope with stigma at the individual, interpersonal, and structural levels, this treatment does little to alter structural manifestations of racism and homophobia. The elimination of structural racism and homophobia would not only have a more robust and sustainable impact on health equity than building GBM of color’s capacity to cope with oppression—it would also avoid the injustice of burdening marginalized individuals with the task of building the resilience to endure oppressive systems that are not of their making. Future research should explore whether structural change and stigma resiliency can be blended to support the mental and sexual health of GBM of color, and how structural change and stigma resiliency might influence each other along the road to health equity (Cook et al., 2014).
Supplementary Material
Acknowledgments
This study was funded by a National Institute of Mental Health grant awarded to Yale University’s Center for Interdisciplinary Research on AIDS (P30MH062294) and the Fund for Lesbian and Gay Studies at Yale. This work was also supported by the Yale Center for Interdisciplinary Research on AIDS training program, funded by the National Institute of Mental Health (T32MH020031). The content contained herein is the authors’ own and does not necessarily reflect the views of the funders, including the National Institutes of Health. The authors would like to acknowledge the following individuals for their help with study coordination, data collection, and intervention development and delivery: Ricardo Albarran, Kriti Behari, Cal Brisbin, Erin McConocha, Benjamin Fetzner, Maxwell Richardson, TJ Sullivan, Cesar Villareal, Roxanne Winston, and the staff of Fair Haven Community Health Care. We also thank Eric Layland and Kobe Pereira for their feedback on an earlier version of this article.
References
- Adames HY, Chavez-Dueñas NY, Sharma S, & La Roche MJ (2018). Intersectionality in psychotherapy: The experiences of an AfroLatinx queer immigrant. Psychotherapy, 55(1), 73. [DOI] [PubMed] [Google Scholar]
- Arnold EA, Rebchook GM, & Kegeles SM (2014). ‘Triply cursed’: Racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Culture, Health & Sexuality, 16(6), 710–722. 10.1080/13691058.2014.905706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala G, Bingham T, Kim J, Wheeler DP, & Millett GA (2012). Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. American Journal of Public Health, 102 Suppl 2, S242–9. 10.2105/AJPH.2011.300641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsam KF, Molina Y, Beadnell B, Simoni J, & Walters K (2011). Measuring multiple minority stress: The LGBT People of Color Microaggressions Scale. Cultural Diversity and Ethnic Minority Psychology, 17(2), 163–174. 10.1037/a0023244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Sauer-Zavala S, Latin HM, Ellard KK, Bullis JR, Bentley KH, Boettcher HT, & Cassiello-Robbins C (2017). Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. Oxford University Press. [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, & Barlow DH (2014). Development and validation of the overall depression severity and imapairment scale. Psychological Assessment, 26(3), 815–830. 10.1037/a0036216 [DOI] [PubMed] [Google Scholar]
- Bogart LM, Barreras JL, Gonzalez A, Klein DJ, Marsh T, Agniel D, & Pantalone DW (2021). Pilot Randomized Controlled Trial of an Intervention to Improve Coping with Intersectional Stigma and Medication Adherence Among HIV-Positive Latinx Sexual Minority Men. AIDS and Behavior, 25(6), 1647–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Dale SK, Daffin GK, Patel K, Klein DJ, Mayer KH, & Pantalone DW (2018). Pilot Intervention for Discrimination-related Coping Among HIV-Positive Black Sexual Minority Men. Cultural Diversity & Ethnic Minority Psychology, 24(4), 541–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bost D (2018). Evidence of Being. University of Chicago Press. [Google Scholar]
- Braun V, & Clarke V (2021). One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 1–25. [Google Scholar]
- Burton CL, Wang K, & Pachankis JE (2017). Psychotherapy for the spectrum of sexual minority stress: Application and technique of the ESTEEM treatment model. Cognitive and Behavioral Practice, 26, 285–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese SK, Earnshaw VA, Magnus M, Hansen NB, Krakower DS, Underhill K, Mayer KH, Kershaw TS, Betancourt JR, & Dovidio JF (2018). Sexual stereotypes ascribed to Black men who have sex with men: An intersectional analysis. Archives of Sexual Behavior, 47(1), 143–156. 10.1007/s10508-016-0911-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlos J-A, Bingham TA, Stueve A, Lauby J, Ayala G, Millett GA, & Wheeler D (2010). The role of peer support on condom use among Black and Latino MSM in three urban areas. AIDS Education and Prevention, 22(5), 430–444. [DOI] [PubMed] [Google Scholar]
- Carpenter C (2003). Seasonal variation in self-reports of recent alcohol consumption: Racial and ethnic differences. Journal of Studies on Alcohol, 64(3), 415–418. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Half of black gay men and a quarter of Latino gay men projected to be diagnosed within their lifetime. Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. (2017). HIV Surveillance Report, 2016; vol. 28. Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Centers for Disease Control and Prevention. (2020). HIV Surveillance Report, 2018 (updated); vol. 31. Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Chang Y, Voils CI, Sandelowski M, Hasselblad V, & Crandell JL (2009). Transforming verbal counts in reports of qualitative descriptive studies into numbers. Western Journal of Nursing Research, 31(7), 837–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PH (1990). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Routledge. [Google Scholar]
- Cook JE, Purdie-Vaughns V, Meyer IH, & Busch JTA (2014). Intervening within and across levels: A multilevel approach to stigma and public health. Social Science & Medicine, 103, 101–109. 10.1016/j.socscimed.2013.09.023 [DOI] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 140, 139–167. [Google Scholar]
- Dailey AF, Hoots BE, Hall HI, Song R, Hayes D, Fulton P Jr, Prejean J, Hernandez AL, Koenig LJ, & Valleroy LA (2017). Vital signs: Human immunodeficiency virus testing and diagnosis delays—United States. MMWR. Morbidity and Mortality Weekly Report, 66(47), 1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13(3), 595–605. 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- Díaz RM, Ayala G, & Bein E (2004). Sexual risk as an outcome of social oppression: Data from a probability sample of Latino gay men in three U.S. cities. Cultural Diversity & Ethnic Minority Psychology, 10(3), 255–267. 10.1037/1099-9809.10.3.255 [DOI] [PubMed] [Google Scholar]
- Díaz RM, Ayala G, Bein E, Henne J, & Marin BV (2001). The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: Findings from 3 US cities. American Journal of Public Health, 91(6), 927–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Rendina HJ, & Parsons JT (2018). The effects of intersecting stigma: A longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychology of Violence, 8(6), 669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinstein BA, Goldfried MR, & Davila J (2012). The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of Consulting and Clinical Psychology, 80(5), 917–927. 10.1037/a0029425 [DOI] [PubMed] [Google Scholar]
- Fish J, Papaloukas P, Jaspal R, & Williamson I (2016). Equality in sexual health promotion: A systematic review of effective interventions for Black and minority ethnic men who have sex with men. BMC Public Health, 16(1), 810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost DM, Meyer IH, & Schwartz S (2016). Social support networks among diverse sexual minority populations. The American Journal of Orthopsychiatry, 86(1), 91–102. 10.1037/ort0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez JM (2019). What’s the harm? Internalized prejudice and cultural betrayal trauma in ethnic minorities. American Journal of Orthopsychiatry, 89(2), 237–247. 10.1037/ort0000367 [DOI] [PubMed] [Google Scholar]
- Graham JR, West LM, Martinez J, & Roemer L (2016). The mediating role of internalized racism in the relationship between racist experiences and anxiety symptoms in a Black American sample. Cultural Diversity and Ethnic Minority Psychology, 22(3), 369. [DOI] [PubMed] [Google Scholar]
- Graham-LoPresti JR, Gautier SW, Sorenson S, & Hayes-Skelton SA (2017). Culturally sensitive adaptations to evidence-based cognitive behavioral treatment for social anxiety disorder: A case paper. Cognitive and Behavioral Practice, 24(4), 459–471. [Google Scholar]
- Greene B (1997). Ethnic minority lesbians and gay men: Mental health and treatment issues. In Greene B (Ed.), Psychological perspectives on lesbian and gay issues: Vol. 3. Ethnic and cultural diversity among lesbians and gay men (pp. 216–239). Sage Publications, Inc. [Google Scholar]
- Han C (2007). They don’t want to cruise your type: Gay men of color and the racial politics of exclusion. Social Identities, 13(1), 51–67. 10.1080/13504630601163379 [DOI] [Google Scholar]
- Han C, Ayala G, Paul JP, Boylan R, Gregorich SE, & Choi K-H (2015). Stress and coping with racism and their role in sexual risk for HIV among African American, Asian/Pacific Islander, and Latino men who have sex with men. Archives of Sexual Behavior, 44(2), 411–420. 10.1007/s10508-014-0331-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken MT, Lee H, Ailshire J, Burgard SA, & Williams DR (2013). “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems, 5(2), 100–112. 10.1007/s12552-013-9095-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hightow-Weidman LB, Phillips G, Jones KC, Outlaw AY, Fields SD, & Smith JC (2011). Racial and sexual identity-related maltreatment among minority YMSM: Prevalence, perceptions, and the association with emotional distress. AIDS Patient Care and STDs, 25(S1), S39–S45. [DOI] [PubMed] [Google Scholar]
- Jackson SD, Mohr JJ, Sarno EL, Kindahl AM, & Jones IL (2020). Intersectional experiences, stigma-related stress, and psychological health among Black LGBQ individuals. Journal of Consulting and Clinical Psychology, 88(5), 416–428. 10.1037/ccp0000489 [DOI] [PubMed] [Google Scholar]
- Kalichman SC, & Rompa D (2001). The sexual compulsivity scale: Further development and use with HIV-positive persons. Journal of Personality Assessment, 76, 379–395. 10.1207/S15327752JPA7603_02 [DOI] [PubMed] [Google Scholar]
- Keene DE, Eldahan AI, White Hughto JM, & Pachankis JE (2017). ‘The big ole gay express’: Sexual minority stigma, mobility and health in the small city. Culture, Health & Sexuality, 19(3), 381–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger EA, Holloway IW, Lightfoot M, Lin A, Hammack PL, & Meyer IH (2020). Psychological distress, felt stigma, and HIV prevention in a national probability sample of sexual minority men. LGBT Health. 10.1089/lgbt.2019.0280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakens D (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4, 863. 10.3389/fpsyg.2013.00863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson DG, & Chastain RL (1990). Self-concealment: Conceptualization, measurement, and health implications. Journal of Social and Clinical Psychology, 9(4), 439–455. 10.1521/jscp.1990.9.4.439 [DOI] [Google Scholar]
- Layland EK, Carter JA, Perry NS, Cienfuegos-Szalay J, Nelson KM, Bonner CP, & Rendina HJ (2020). A systematic review of stigma in sexual and gender minority health interventions. Translational Behavioral Medicine, 10(5), 1200–1210. 10.1093/tbm/ibz200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CS, López SR, Hernández L, Colby SM, Caetano R, Borrelli B, & Rohsenow D (2011). A cultural adaptation of motivational interviewing to address heavy drinking among Hispanics. Cultural Diversity and Ethnic Minority Psychology, 17(3), 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt HM, Surace FI, Wu MB, Chapin B, Hargrove JG, Herbitter C, Lu EC, Maroney MR, & Hochman AL (2020). The meaning of scientific objectivity and subjectivity: From the perspective of methodologists. Psychological Methods. [DOI] [PubMed] [Google Scholar]
- Levy ME, Wilton L, Phillips G, Glick SN, Kuo I, Brewer RA, Elliott A, Watson C, & Magnus M (2014). Understanding structural barriers to accessing HIV testing and prevention services among Black men who have sex with men (BMSM) in the United States. AIDS and Behavior, 18(5), 972–996. 10.1007/s10461-014-0719-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JL, & Dean L (1992). Summary of measures: Mental health effects of AIDS on at-risk homosexual men [Unpublished manuscript]. Columbia University, Mailman School of Public Health. [Google Scholar]
- Matthews DD, Smith JC, Brown AL, & Malebranche DJ (2016). Reconciling epidemiology and social justice in the public health discourse around the sexual networks of black men who have sex with men. American Journal of Public Health, 106(5), 808–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, & Holtgrave D (2013). A systematic review of HIV interventions for black men who have sex with men (MSM). BMC Public Health, 13(1), 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer RR, de Vries RM, & van Bruggen V (2011). An evaluation of the brief symptom inventory-18 using item response theory: Which items are most strongly related to psychological distress? Psychological Assessment, 23(1), 193–202. 10.1037/a0021292 [DOI] [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, & Pietrzak J (2002). Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology, 83(4), 896–918. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, & Frost DM (2008). Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science & Medicine, 67(3), 368–379. 10.1016/j.socscimed.2008.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2015). Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity, 2(3), 209–213. 10.1037/sgd0000132 [DOI] [Google Scholar]
- Millett GA, Flores SA, Peterson JL, & Bakeman R (2007). Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS, 21(15), 2083–2091. 10.1097/QAD.0b013e3282e9a64b [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, Rourke SB, Heilig CM, Elford J, Fenton KA, & Remis RS (2012). Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet (London, England), 380(9839), 341–348. 10.1016/S0140-6736(12)60899-X [DOI] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Wolitski RJ, & Stall R (2006). Greater risk for HIV infection of black men who have sex with men: A critical literature review. American Journal of Public Health, 96(6), 1007–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Borkowf C, Millett GA, Bingham T, Ayala G, & Stueve A (2012). Homophobia and racism experienced by Latino men who have sex with men in the United States: Correlates of exposure and associations with HIV risk behaviors. AIDS and Behavior, 16(3), 724–735. [DOI] [PubMed] [Google Scholar]
- Morales ES (1989). Ethnic minority families and minority gays and lesbians. Marriage & Family Review, 14(3–4), 217–239. psyh. 10.1300/J002v14n03_11 [DOI] [Google Scholar]
- Norman SB, Cissell SH, Means-Christensen AJ, & Stein MB (2006). Development and validation of an overall anxiety severity and impairment scale (OASIS). Depression and Anxiety, 23(4), 245–249. 10.1002/da.20182 [DOI] [PubMed] [Google Scholar]
- Pachankis JE (2014). Uncovering clinical principles and techniques to address minority stress, mental health, and related health risks among gay and bisexual men. Clinical Psychology: Science and Practice, 4(21), 313–330. 10.1111/cpsp.12078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE (2015). A transdiagnostic minority stress treatment approach for gay and bisexual men’s syndemic health conditions. Archives of Sexual Behavior, 44(7), 1843–1860. 10.1007/s10508-015-0480-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Goldfried MR, & Ramrattan ME (2008). Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. Journal of Consulting and Clinical Psychology, 76(2), 306–317. 10.1037/0022-006X.76.2.306 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology, 83(5), 875–889. 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, McConocha EM, Clark KA, Wang K, Behari K, Fetzner BK, Brisbin CD, Scheer JR, & Lehavot K (2020). A transdiagnostic minority stress intervention for gender diverse sexual minority women’s depression, anxiety, and unhealthy alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 10.1037/ccp0000508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan S, Sun S, Li X, Chen J, Xiong Y, He Y, & Pachankis JE (2020). A pilot cultural adaptation of LGB-affirmative CBT for young Chinese sexual minority men’s mental and sexual health. Psychotherapy (Chicago, Ill.). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Bimbi D, & Borkowski T (2000). Perceptions of the benefits and costs associated with condom use and unprotected sex among late adolescent college students. Journal of Adolescence, 23(4), 377–391. 10.1006/jado.2000.0326 [DOI] [PubMed] [Google Scholar]
- Phillips L, & Olugbala S (2006). Fighting in he(r) heels: Sylvia Rivera, Stonewall, civil rights, and liberation. In Glisson S (Ed.), The human tradition and the civil rights movement, 1865–1980 (pp. 309–334). Rowman & Littlefield. [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Ramirez-Valles J (2007). “I don’t fit anywhere”: How race and sexuality shape Latino gay and bisexual men’s health. In Meyer IH & Northridge ME (Eds.), The health of sexual minorities: Public health perspectives on lesbian, gay, bisexual, and transgender populations. (pp. 301–319). Springer Science + Business Media; psyh. [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, & Johnson BT (2014). HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine (1982), 103, 118–125. 10.1016/j.socscimed.2013.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisen CA, Brooks KD, Zea MC, Poppen PJ, & Bianchi FT (2013). Can additive measures add to an intersectional understanding? Experiences of gay and ethnic discrimination among HIV-positive Latino gay men. Cultural Diversity and Ethnic Minority Psychology, 19(2), 208–217. 10.1037/a0031906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, & Parsons JT (2017). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 51(2), 147–158. 10.1007/s12160-016-9822-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Eaton NR, & Pachankis JE (2019). Prevalence of psychiatric disorders at the intersection of race and sexual orientation: Results from the National Epidemiologic Survey of Alcohol and Related Conditions-III. Journal of Consulting and Clinical Psychology, 87(4), 321–331. 10.1037/ccp0000377 [DOI] [PubMed] [Google Scholar]
- Rosenberg ES, Grey JA, Sanchez TH, & Sullivan PS (2016). Rates of prevalent HIV infection, prevalent diagnoses, and new diagnoses among men who have sex with men in US states, metropolitan statistical areas, and counties, 2012-2013. JMIR Public Health and Surveillance, 2(1). 10.2196/publichealth.5684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Blashill AJ, & O’Cleirigh CM (2011). Promoting the sexual health of MSM in the context of comorbid mental health problems. AIDS and Behavior, 15(Suppl 1), S30–S34. psyh. 10.1007/s10461-011-9898-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarno EL, Mohr JJ, Jackson SD, & Fassinger RE (2015). When identities collide: Conflicts in allegiances among LGB people of color. Cultural Diversity & Ethnic Minority Psychology, 21(4), 550–559. 10.1037/cdp0000026 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88, 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Sawilowsky SS (2009). New effect size rules of thumb. Journal of Modern Applied Statistical Methods, 8(2), 26. [Google Scholar]
- Schrimshaw EW, Siegel K, Downing MJ, & Parsons JT (2013). Disclosure and concealment of sexual orientation and the mental health of non-gay-identified, behaviorally bisexual men. Journal of Consulting and Clinical Psychology, 81(1), 141–153. 10.1037/a0031272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah AP, Smolensky MH, Burau KD, Cech IM, & Lai D (2007). Recent Change in the Annual Pattern of Sexually Transmitted Diseases in the United States. Chronobiology International, 24(5), 947–960. 10.1080/07420520701648325 [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow–back: A technique for assessing self–reported alcohol consumption. In Litten RZ & Allen JP (Eds.), Measuring alcohol consumption: Psychosocial and biological methods (pp. 41–72). Humana Press. [Google Scholar]
- Starks H, & Brown Trinidad S (2007). Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research, 17(10), 1372–1380. [DOI] [PubMed] [Google Scholar]
- Tufford L, & Newman P (2012). Bracketing in qualitative research. Qualitative Social Work, 11(1), 80–96. [Google Scholar]
- Utsey SO, Belvet B, Hubbard RR, Fischer NL, Opare-Henaku A, & Gladney LL (2013). Development and validation of the prolonged activation and anticipatory race-related stress scale. Journal of Black Psychology, 39(6), 532–559. 10.1177/0095798412461808 [DOI] [Google Scholar]
- Van Spijker BA, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, & Kerkhof AJ (2014). The Suicidal Ideation Attributes Scale (SIDAS): Community-Based validation study of a new scale for the measurement of suicidal ideation. Suicide and Life-Threatening Behavior, 44(4), 408–419. 10.1111/sltb.12084 [DOI] [PubMed] [Google Scholar]
- Wang K, & Pachankis JE (2016). Gay-related rejection sensitivity as a risk factor for condomless sex. AIDS and Behavior, 20(4), 763–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellings K, Macdowall W, Catchpole M, & Goodrich J (1999). Seasonal variations in sexual activity and their implications for sexual health promotion. Journal of the Royal Society of Medicine, 92(2), 60–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto JM, Pachankis JE, Eldahan AI, & Keene DE (2017). “You can’t just walk down the street and meet someone”: The intersection of social–sexual networking technology, stigma, and health among gay and bisexual men in the small city. American Journal of Men’s Health, 11(3), 726–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JK, Ramamurthi HC, Manago C, & Harawa NT (2009). Learning from successful interventions: A culturally congruent HIV risk–reduction intervention for African American men who have sex with men and women. American Journal of Public Health, 99(6), 1008–1012. 10.2105/AJPH.2008.140558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson PA, Valera P, Ventuneac A, Balan I, Rowe M, & Carballo-Diéguez A (2009). Race-based sexual stereotyping and sexual partnering among men who use the Internet to identify other men for bareback sex. Journal of Sex Research, 46(5), 399–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilton L, Herbst JH, Coury-Doniger P, Painter TM, English G, Alvarez ME, Scahill M, Roberson MA, Lucas B, & Johnson WD (2009). Efficacy of an HIV/STI prevention intervention for Black men who have sex with men: Findings from the Many Men, Many Voices (3MV) Project. AIDS and Behavior, 13(3), 532–544. [DOI] [PubMed] [Google Scholar]
- Wingood GM, & DiClemente RJ (2008). The ADAPT-ITT model: A novel method of adapting evidence-based HIV Interventions. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47, S40–S46. [DOI] [PubMed] [Google Scholar]
- Yalom ID, & Leszcz M (2020). The theory and practice of group psychotherapy. Hachette; UK. [Google Scholar]
- Young LE, Schumm P, Alon L, Bouris A, Ferreira M, Hill B, Khanna AS, Valente TW, & Schneider JA (2018). PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clinical Trials, 15(1), 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


