Abstract
Background
While [18F]-fluordeoxyglucose ([18F]FDG) uptake is associated with arterial inflammation, [18F]-sodium fluoride ([18F]NaF) is a marker for arterial micro-calcification. We aimed to investigate the prospective correlation between both PET markers over time and whether they are prospectively ([18F]FDG) and retrospectively ([18F]NaF) related to progression of systemic arterial disease in a longitudinal study in patients with type 2 diabetes mellitus (T2DM).
Methods
Baseline [18F]FDG PET/Low Dose (LD) Computed Tomography (CT) scans of ten patients with early T2DM without cardiovascular history (70% men, median age 63 years) were compared with five-year follow-up [18F]NaF/LDCT scans. Systemic activity was expressed as mean target-to-background ratio (meanTBR) by dividing the maximal standardized uptake value (SUVmax) of ten arteries by SUVmean of the caval vein. CT-assessed macro-calcifications were scored visually and expressed as calcified plaque (CP) score. Arterial stiffness was assessed with carotid-femoral pulse wave velocity (PWV). Five-year changes were expressed absolutely with delta (Δ) and relatively with %change.
Results
Baseline meanTBR[18F]FDG was strongly correlated with five-year follow-up meanTBR[18F]NaF (r = 0.709, P = .022). meanTBR[18F]NaF correlated positively with ΔCPscore, CPscore at baseline, and follow-up (r = 0.845, P = .002 and r = 0.855, P = .002, respectively), but not with %change in CPscore and PWV.
Conclusion
This proof-of-concept study demonstrated that systemic arterial inflammation is an important pathogenetic factor in systemic arterial micro-calcification development.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12350-021-02781-w.
Keywords: Inflammation, diabetes, atherosclerosis, PET, CT, vascular imaging
Background
Inflammation and progressive calcification are the hallmarks of atherosclerosis, resulting in arterial stiffness and development of cardiovascular diseases.1,2 Although these processes are closely related, clinical data on their association over time are limited. With positron emission tomography (PET), detailed molecular imaging of the active processes of atherosclerosis can be visualized.3 [18F]-fluorodeoxyglucose ([18F]FDG) and [18F]-sodium fluoride ([18F]NaF) PET scans are suitable for assessment of respectively arterial inflammation and micro-calcification, and are proven useful for detection of cardiovascular disease in the clinical research setting.3 Arterial [18F]FDG uptake is linked to Pulse Wave Velocity (PWV)-assessed arterial stiffness and has shown to predict future cardiovascular events.4,5 Furthermore, [18F]FDG may also serve as a marker for endothelial dysfunction and as a precursor of arterial calcification, which are important characteristics of the development of cardiovascular disease. Patients with T2DM are at increased cardiovascular risk, with increased arterial inflammation on [18F]FDG PET and more progressive arterial calcification.6 Ex vivo studies suggest a close relation between PET-assessed arterial inflammation and calcification, but this has yet to be confirmed in clinical studies.7,8 Importantly, in a cross-sectional study, focal arterial [18F]FDG uptake did not correlate with [18F]NaF uptake.9 Furthermore, arterial [18F]FDG PET uptake was not associated with calcification progression on computed tomography (CT) and specific sites of increased [18F]FDG uptake and calcification rarely overlapped.10 However, since inflammation is the precursor of calcification development and previous studies observed that both processes are not present simultaneously,9,11 we hypothesize that [18F]FDG-assessed arterial inflammation may be associated with [18F]NaF-assessed arterial micro-calcification over time. The primary aim of this proof-of-concept study is the assessment of the prospective association of baseline systemic arterial [18F]FDG activity with systemic [18F]NaF PET during five years of follow-up in asymptomatic patients with T2DM. The secondary aim was to correlate arterial PET activity with CT-assessed macrocalcification and arterial stiffness and changes in these markers over five years.
Methods and Results
Study Design and Population
For this study, ten participants from the RELEASE trial were included (NCT02015299).5,12 The study design and selection of participants have been reported previously.5 In short, patients with early T2DM, without using glucose lowering drugs, and without severe cardiovascular history (i.e., stable coronary artery disease or acute coronary syndrome, stroke, or transient ischemic attack, peripheral artery disease) were included. Baseline assessments (including [18F]FDG PET/CT scan, clinical, laboratory, and cardiovascular assessments), were conducted between April 2014 and April 2015 and the follow-up visit (including [18F]NaF PET/CT scan, clinical, laboratory, and cardiovascular assessments) took place between January 2019 and June 2019. Both studies (baseline and follow-up) were reviewed and approved by the Medical Ethical Institutional Review Board of the UMCG (METC numbers 2013-080 and 2018-456, respectively). Both studies were performed in compliance with the principles of the Declaration of Helsinki.
Clinical and Laboratory Assessments
At baseline and follow-up visit and a detailed medical history were evaluated. Height and weight were measured to determine body mass index (BMI). Blood samples were obtained in the morning after at least 8 hour of overnight fasting for the measurements of plasma glucose, HbA1c, and lipid profile. To determine arterial stiffness, carotid-femoral pulse wave velocity (PWV) and blood pressure measurements were performed at baseline and follow-up visit. Measurements were performed as described previously.5
PET/CT Imaging
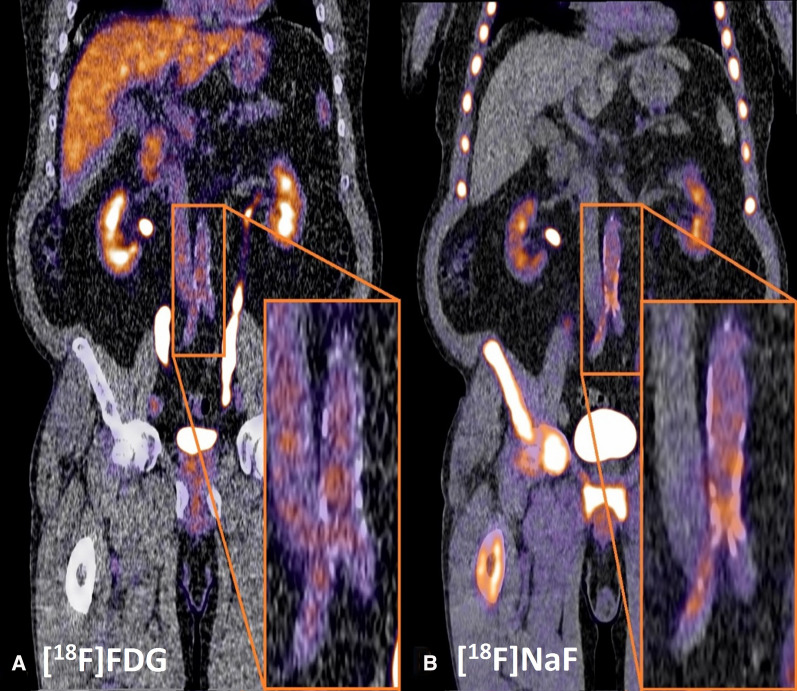
At baseline, [18F]FDG PET/Low Dose (LD) CT imaging was performed on a Siemens Biograph 64-slice PET/CT scanner (Siemens Healthineers, Knoxville, TN), 60 minutes after intravenous injection of 3 MBq⋅kg [18F]FDG. Follow-up [18F]NaF PET/CT images were obtained on a Siemens Vision scanner (Siemens Healthineers, Erlangen, Germany), 90 minutes after an intravenous injection of 2.0 MBq⋅kg [18F]NaF (maximum dosage: 200 MBq). A baseline [18F]FDG and follow-up [18F]NaF PET/LD CT of one participant with abdominal aorta tracer uptake is shown in Figure 1. Participants were instructed to fast overnight for at least 8 hours and drink 1 L water 1-3 hours before and 0.5 L water after injection of the radiopharmaceutical. Before PET imaging started, a continuous breathing LD CT (80-120 kV, 20-35 mAs, and 5 mm slice thickness) was performed for visualization of anatomical structures and used as attenuation correction map. PET acquisitions were obtained with 2-3 minutes per bed position in 3D setting. Images were reconstructed according to the European Association of Nuclear Medicine guidelines,13 using a time of flight iterative reconstruction method (3 iterations, 21 subsets, and voxel-size 3.18 × 3.18 × 2 mm) with point spread function correction. Images were corrected for random coincidences, scatter and attenuation, and were smoothed with a Gaussian filter of 6.5 mm in full width at half maximum.
Figure 1.
[18Fluor]fluordeoxyglucose ([18F]FDG) and five-year follow-up [18Fluor]SodiumFluoride ([18F]NaF) positron emission tomography/low dose computed tomography in a patient with type 2 diabetes mellitus. A Metabolic active cells are visualized by [18F]FDG uptake can be found in the liver, heart, and more focal in arterial tissue (pop-up). In arterial tissue, [18F]FDG uptake is a marker for inflammation which is considered an important factor in the development of CVD. B [18F]NaF uptake demonstrates skeletal activity and, next to that, this tracer also visualizes micro-calcification formation in the arterial wall (pop-up). Both nuclear tracers are excreted via the kidneys, ureters, and bladder. For image processing and analysis Affinity 2.0 was used (Hermes Medical Solutions)
Image Analysis
The method of systemic arterial tracer PET activity analysis used in this study, was performed as described previously.5,12 Briefly, ten arteries were divided into four anatomical segments: carotid arteries (segment 1), ascending aorta and aortic arch (segment 2), descending thoracic and abdominal aorta (segment 3), and iliac and femoral arteries (segment 4). First, the maximal standardized uptake value (SUVmax) per segment was calculated. Second, by averaging the SUVmax of the four individual segments, the meanSUVmax was calculated. The SUVmax values for [18F]FDG scans were normalized for fasting pre-scan glucose. Regional arterial target-to-background ratios (meanTBR) for both [18F]FDG and [18F]NaF per segment were calculated by dividing the SUVmax by the (in duplex measured) SUVmean derived from the blood pool in the superior caval vein (for segments 1-2) or inferior caval vein (for segments 3-4). meanTBR was calculated by averaging the four segments, as measurement for the whole aortic tree for both [18F]FDG and [18F]NaF. In addition to the per-patient association, a regional analysis between tracers was analyzed including 4 segments in 10 patients, resulting in a comparison of 40 segments. Analyses of [18F]NaF and [18F]FDG were separated by time and [18F]NaF scans were blinded and coded by study number and scan date.
Arterial Calcification
Based on LD CT-scans, arterial macro-calcification was quantified visually. According to the method of Rominger et al.,4 a visual score was assigned for the above mentioned ten arteries. Presence of macro-calcification was scored as 0 (no visual calcification), 1 (plaque covered < 10% of vessel circumference), 2 (plaque covered 10%-25% of vessel circumference), 3 (plaque covered 25%-50% of vessel circumference), or 4 (plaque covered > 50% of vessel circumference). For the calcified plaque (CP) score, the sum of the plaque scores of ten arterial segments was calculated and further in the analysis and manuscript addressed as CPscore.
Statistical Analysis
Discrete variables are presented as numbers with percentages. Quantitative variables with a normal distribution are presented as median with interquartile range (IQR). Univariate associations were investigated with Spearman’s correlation coefficient (R). Wilcoxon’s matched signed rank test was used to asses differences between baseline and follow-up visit. CT-assessed macro-calcification and PWV changes between baseline and follow-up visit were calculated absolutely as [value follow-up]-[value at baseline] and expressed as Delta’s (Δ), relative changes were calculated as ([value follow-up]-[value at baseline])/[value at baseline] and expressed as %change. All statistical analyses were performed with IBM Statistical Package for Social Sciences (SPSS) version 23. P < .05 was considered statistically significant.
Results
Ten patients (seven males, three females), with a median age of 63 [59-69] years at baseline, participated in this substudy. Patient characteristics at baseline and follow-up visit are presented in Table 1 and did not differ significantly from the baseline characteristics of the entire RELEASE cohort.5,12 HbA1c increased significantly over five years (46 [42-48] vs 52 [44-56] mmol⋅mol (P = .012). After five-year follow-up, CPscore had increased significantly (16.0 [5.0-19.5] vs 20 [7.5-24.5] (P = .007), with a CPscore %change of 24% [19-33], whereas PWV remained stable (7.98 [6.95-9.29] vs 8.65 [7.79-9.70] m⋅s (P = .203), with a PWV %change of 7.2% [− 9.0 to 27] as did other parameters (SBP, BMI, lipids, C-reactive protein, and kidney function (estimated glomerular filtration rate, albumin-creatinin ratio)). Baseline age correlated significantly with meanTBR[18F]NaF and PWV (r = 0.746, P = .013, and r = 0.654, P = .040, respectively).
Table 1.
Characteristics at baseline and at five-year follow-up
| N = 10 | Baseline | Five-year follow-up | P value |
|---|---|---|---|
| Age (years) | 63 [59–69] | 69 [63–73] | |
| Male (%) | 70% | 70% | |
| Statin use (%) | 60% | 70% | |
| BMI (kg⋅m2) | 31 [27–36] | 31 [28–34] | .799 |
| SBP (mmHg) | 138 [127–149] | 138 [127–149] | .953 |
| HbA1c (mmol⋅mol) | 46 [42–48] | 52 [44–56] | .012 |
| Total cholesterol (mmol⋅L) | 4.85 [4.15–5.33] | 4.15 [3.68–5.10] | .106 |
| LDL-cholesterol (mmol⋅L) | 3.00 [2.55–3.90] | 2.70 [2.35–3.80] | .476 |
| HDL-cholesterol (mmol⋅L) | 1.20 [1.10–1.23] | 1.10 [0.98–1.33] | .168 |
| Triglycerides (mmol⋅L) | 1.45 [1.11–1.99] | 1.49 [1.35–1.69] | .760 |
| C-reactive protein (mg⋅L) | 1.15 [0.78–2.40] | 1.15 [0.83–2.03] | .812 |
| Estimated glomerular filtration rate (ml⋅min*1.73m2) | 85 [80–101] | 87 [84–93] | .878 |
| Albumin-creatinin ratio (mg⋅mmol) | 0.45 [0.00–0.80] | 0.35 [0.25–0.75] | .646 |
| PWV (m⋅s) | 7.98 [6.95–9.29] | 8.65 [7.79–9.70] | .203 |
| CT-assessed arterial calcified plaque score | 16.0 [5.0–19.5] | 20.0 [7.5–24.5] | .007 |
| Arterial [18F]-FDG uptake (meanTBR) | 2.12 [1.82–2.49] | ||
| Arterial [18F]-NaF uptake (meanTBR) | 2.20 [2.03–2.97] |
Predictive Value of PET and PWV-Assessed Arterial Disease
Baseline meanTBR[18F]FDG demonstrated a strong positive correlation with five-year follow-up meanTBR[18F]NaF (r = 0.709, P = .022, Figure 2). Also, the regional association between [18F]FDG and [18F]NaF showed a significant correlation over five years (r = 0.523, P = .001). Baseline meanTBR[18F]FDG did not correlate with age (r = 0.306, P = .390), baseline CPscore (r = 0.334, P = .345), follow-up CPscore (r = 0.345, P = .328), follow-up PWV (r = − 0.103, P = .777), ΔCPscore (r = 0.389, P = .267) or ΔPWV (r = − 0.442, P = .200). CPscore at baseline and follow-up were strongly correlated (r = 0.960, P < .001). Follow-up meanTBR[18F]NaF did correlate with ΔCPscore and CPscore at baseline and follow-up (r = 0.735, P = .016, r = 0.845, P = .002 and P = 0.855, P = .002 (Figure 3), respectively), while it was not associated with CPscore %change (r = − 0.152, P = .675), PWV %change (r = − 0.406, P = .244) and ΔPWV (r = − 0.285, P = .425). Furthermore, follow-up meanTBR[18F]NaF showed a trend toward a significant positive association with baseline PWV (r = 0.588, P = .074) but not with follow-up PWV (r = − 0.018, P = .960). Also, baseline and follow-up PWV did not correlate with CPscore at baseline (r = 0.377, P = .283 and r = 0.079, P = .828, respectively) or at follow-up (r = 0.527, P = .117 and r = 0.285, P = .425, respectively).
Figure 2.
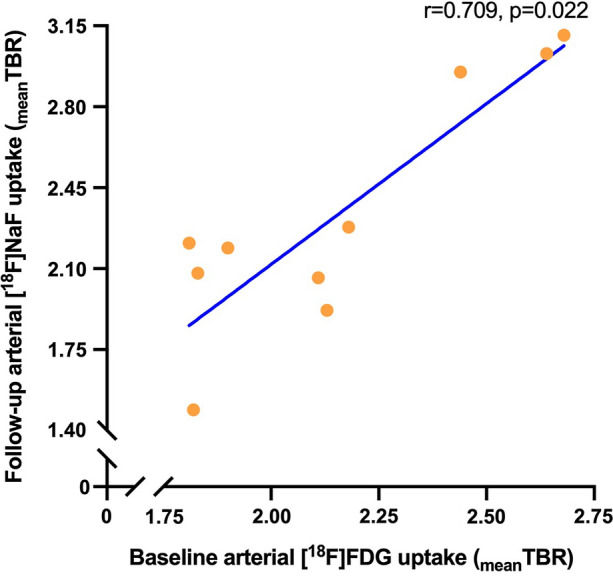
Baseline systemic arterial inflammation is related to five-year follow-up systemic arterial micro-calcification. Correlation between arterial [18F]-fluordeoxyglucose ([18F]FDG) uptake at baseline and arterial [18F]-sodium fluoride ([18F]NaF) uptake at five-year follow-up, expressed as target-to-background ratio (TBR). TBR was calculated by dividing the maximal standardized uptake value (SUVmax) of the arteries by the mean standardized uptake value (SUVmean) of the caval veins (blood pool)
Figure 3.
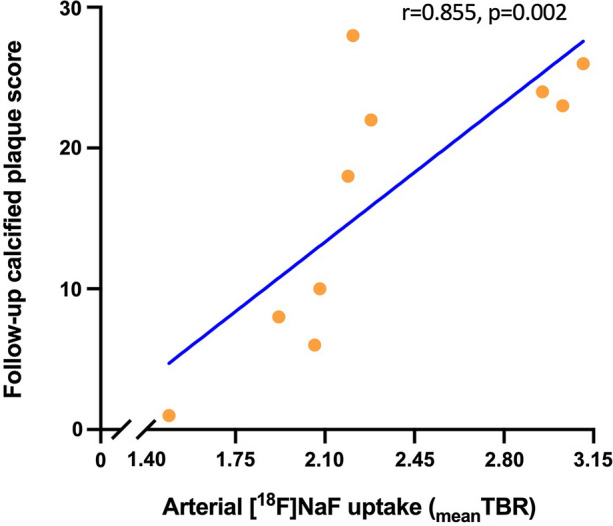
Systemic arterial micro-calcification was related to systemic arterial macro-calcification over five years. Correlation between systemic positron emission tomography-assessed arterial [18F]-sodium fluoride ([18F]NaF) uptake (expressed as meantarget to background ratio (TBR), calculated by averaging ten TBRs (maximal standardized uptake value (SUVmax) divided by the mean standardized uptake value (SUVmean) of the blood pool)) and follow-up low dose computed tomography-assessed arterial macro-calcification (expressed as calcified plaque score, measured in whole aortic tree4)
Discussion
In this five-year follow-up study, baseline arterial [18F]FDG uptake correlated positively with follow-up arterial [18F]NaF uptake as interrelated molecular imaging markers of development of systemic arterial disease in patients with early T2DM without overt cardiovascular disease. Arterial [18F]NaF uptake demonstrated a significant positive correlation with the CT-assessed whole aortic tree macro-calcification burden. After five years of follow-up we observed that, compared with baseline, CPscore increased significantly, while PWV did not. This suggests that, without significantly affecting arterial stiffness, systemic arterial disease increased in five years in patients with early T2DM and that the development of atherosclerosis seems to progress from systemic arterial inflammation to systemic arterial micro-calcification over time.
Although our cohort has a limited sample size, we believe these observations add significance to the understanding of arterial [18F]FDG uptake in T2DM. To the best of our knowledge, no similar follow-up studies with arterial [18F]FDG and [18F]NaF uptake have been reported in patients with T2DM. However, previous studies did investigate the relation between arterial [18F]FDG and [18F]NaF uptake at the same time. Derlin et al. observed in vivo colocalized uptake of both [18F]FDG and [18F]NaF in only 6.5% of focal arterial lesions in carotid arteries and aorta.14 This limited relation between [18F]FDG and [18F]NaF uptake might be explained by the fact that PET images were performed simultaneously after separate administration while these tracers are markers of a different stage of development of atherosclerosis.3 An additional import distinction is that the current study focused on the whole aortic tree, reflecting a more systemic measurement approach of arterial tracer uptake. This is important, since atherosclerosis is generalized arterial disease and not limited to specific sites. A similar approach was used in patients with pseudoxanthoma elasticum, in which a relation between arterial [18F]FDG and [18F]NaF uptake was not observed.9 In this latter study, PET scans were performed within a very short time interval of just a few days. The observation that arterial [18F]FDG and [18F]NaF uptake do not colocalize in parallel PET scans emphasizes that these tracers reflect a different stage of arterial disease and appear not to coincide in an arterial lesion.3 By demonstrating a correlation of arterial [18F]FDG with [18F]NaF uptake over a time frame of five years, the current study sheds light on the potential temporal arterial disease progression from arterial inflammation to arterial micro-calcification, but not macro-calcification. This accentuates the importance of inflammation as risk factor in the development of atherosclerotic diseases.1 In contrast to our brief report results, other studies did show a correlation between arterial [18F]FDG and macro-calcification, maybe due to low power in the current study.15
Our data suggest that micro-calcifications appear related to the retrospective and concurrently measured burden of arterial macro-calcification, but not with the relative change in calcification over five years. Few clinical studies have been performed on aortic [18F]NaF uptake in relation to arterial disease progression. We and others previously demonstrated that focal [18F]NaF uptake is a reliable marker to identify active atherosclerotic calcification formation.16,17 In these studies it was observed that calcification patterns of [18F]NaF and CT are different, revealing a different stage of the calcification process. Next to that, in patients with aortic stenosis it was demonstrated that baseline aortic valve [18F]NaF uptake correlated with the progression of calcium content after one year.18 This result is in line with our current study, in which systemically assessed arterial [18F]NaF activity was related to the five-year increase of macrocalcification, highlighting [18F]NaF as a marker of active calcium buildup. In contrast, in a study among postmenopausal women, in which a [18F]NaF PET scan was performed for the assessment of bone mineralization, baseline aortic [18F]NaF uptake did not predict aortic calcification and its four-year progression.19 However, the authors had adequately addressed that they only included women without cardiovascular risk factors and that results may not be directly generalizable to men or other (high risk) populations, which we particularly included in our study. With the current study we underline previous conclusions that systemic arterial [18F]NaF uptake reveals arterial macro-calcification in high risk patients with T2DM. Although speculatively, these data underline that atherosclerotic progression already takes place at an early stage of T2DM and progression from arterial inflammation into micro-calcification on a systemic level already occurs in five years.
This long-term follow-up study also has some limitations. First, our proof-of-concept study is limited by the small sample size, resulting in an inability to adjust for additional parameters (such as sex and drug use) which potentially could have influenced our outcomes. Second, we could not assess changes over time in arterial [18F]FDG and [18F]NaF uptake because no [18F]NaF PET scan was performed at baseline and no [18F]FDG PET scan was repeated at the follow-up visit. Third, while [18F]NaF uptake was related to the preceding and concurrent macro-calcification cross-sectionally we did not study the role of [18F]NaF uptake in predicting macrocalcification progression since baseline [18F]NaF PET scans was not performed. Finally, more advanced methods of PET image analyses were developed in the previous years between our baseline and follow-up analyses. For instance, blood pool measurements in the right atrium seem more reproducible and quantification of aortic whole vessel PET tracer uptake has improved.20 However, even with this small sample size, we already observed correlations of systemic arterial [18F]NaF uptake with the active process of the arterial disease progression with molecular imaging. These results prompts to perform similar analyses in larger cohorts.
Conclusion
In this study it was demonstrated for the first time that, in patients with early T2DM without overt cardiovascular disease, systemic arterial inflammation is prospectively related to systemic arterial micro-calcification after five-year follow-up, as measured with arterial [18F]FDG and [18F]NaF uptake, respectively. This implicates that arterial disease is present in an early phase of T2DM and that this arterial disease leads to a significant increase of arterial calcification. Although larger cohort studies are needed to investigate whether these changes on PET are related to T2DM parameters and are predictive for clinical outcomes, we believe that the current study contributes to the current understanding of the temporal interrelation of these tracers in arterial disease.
New Knowledge Gained
In cardiovascular high risk patients with type 2 diabetes mellitus, PET-assessed systemic arterial [18F]FDG uptake is positively and prospectively associated with five-year follow-up systemic arterial [18F]NaF uptake.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
Ethical approval
All authors have agreed for authorship, read and approved the manuscript, and given consent for submission and subsequent publication of the manuscript. This work was supported in part by an unconditional grant of Siemens Healthineers. The sponsor had no role in the conceptualization, interpretation of findings, writing or publication of the article.
Abbreviations
- [18F]FDG
[18F]-fluordeoxyglucose
- [18F]NaF
[18F]-sodium fluoride
- CP
Calcium plaque
- CT
Computed tomography
- LD
Low dose
- PET
Positron emission tomography
- PWV
Pulse wave velocity
- SUV
Standard uptake value
- T2DM
Type 2 diabetes mellitus
- TBR
Target to background ratio
Footnotes
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 2.Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM. Role of smooth muscle cells in vascular calcification: Implications in atherosclerosis and arterial stiffness. Cardiovasc Res. 2018;114:590–600. doi: 10.1093/cvr/cvy010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKenney-Drake ML, Moghbel MC, Paydary K, Alloosh M, Houshmand S, Moe S, et al. (18)F-NaF and (18)F-FDG as molecular probes in the evaluation of atherosclerosis. Eur J Nucl Med Mol Imaging. 2018;45:2190–2200. doi: 10.1007/s00259-018-4078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rominger A, Saam T, Wolpers S, Cyran CC, Schmidt M, Foerster S, et al. 18F-FDG PET/CT identifies patients at risk for future vascular events in an otherwise asymptomatic cohort with neoplastic disease. J Nucl Med. 2009;50:1611–1620. doi: 10.2967/jnumed.109.065151. [DOI] [PubMed] [Google Scholar]
- 5.de Boer SA, Hovinga-de Boer MC, Heerspink HJ, Lefrandt JD, van Roon AM, Lutgers HL, et al. Arterial stiffness is positively associated with 18F-fluorodeoxyglucose positron emission tomography-assessed subclinical vascular inflammation in people with early type 2 diabetes. Diabetes Care. 2016;39:1440–1447. doi: 10.2337/dc16-0327. [DOI] [PubMed] [Google Scholar]
- 6.Raggi P. Screening for atherosclerotic cardiovascular disease in patients with type 2 diabetes mellitus: Controversies and guidelines. Can J Diabetes. 2020;44:86–92. doi: 10.1016/j.jcjd.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Kerwin WS, Caldwell JH, Ferguson MS, Hippe DS, Alessio AM, et al. High resolution FDG-microPET of carotid atherosclerosis: Plaque components underlying enhanced FDG uptake. Int J Cardiovasc Imaging. 2016;32:145–152. doi: 10.1007/s10554-015-0739-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masteling MG, Zeebregts CJ, Tio RA, Breek JC, Tietge UJ, de Boer JF, et al. High-resolution imaging of human atherosclerotic carotid plaques with micro 18F-FDG PET scanning exploring plaque vulnerability. J Nucl Cardiol. 2011;18:1066–1075. doi: 10.1007/s12350-011-9460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Omarjee L, Mention PJ, Janin A, Kauffenstein G, Pabic EL, Meilhac O, et al. Assessment of inflammation and calcification in pseudoxanthoma elasticum arteries and skin with 18F-FluroDeoxyGlucose and 18F-sodium fluoride positron emission tomography/computed tomography imaging: The GOCAPXE trial. J Clin Med. 2020;9:3448. doi: 10.3390/jcm9113448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meirelles GS, Gonen M, Strauss HW. 18F-FDG uptake and calcifications in the thoracic aorta on positron emission tomography/computed tomography examinations: Frequency and stability on serial scans. J Thorac Imaging. 2011;26:54–62. doi: 10.1097/RTI.0b013e3181d9c9f9. [DOI] [PubMed] [Google Scholar]
- 11.Shioi A, Ikari Y. Plaque calcification during atherosclerosis progression and regression. J Atheroscler Thromb. 2018;25:294–303. doi: 10.5551/jat.RV17020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Boer SA, Heerspink HJ, Lefrandt JD, Hovinga-de Boer MC, van Roon AM, Juárez Orozco LE, et al. Effect of linagliptin on Arterial (18)F-fluorodeoxyglucose positron emission tomography uptake: A randomized controlled trial (RELEASE) J Am Coll Cardiol. 2017;69:1097–1098. doi: 10.1016/j.jacc.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: Version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–354. doi: 10.1007/s00259-014-2961-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derlin T, Tóth Z, Papp L, Wisotzki C, Apostolova I, Habermann CR, et al. Correlation of inflammation assessed by 18F-FDG PET, active mineral deposition assessed by 18F-fluoride PET, and vascular calcification in atherosclerotic plaque: A dual-tracer PET/CT study. J Nucl Med. 2011;52:1020–1027. doi: 10.2967/jnumed.111.087452. [DOI] [PubMed] [Google Scholar]
- 15.Abdelbaky A, Corsini E, Figueroa AL, Fontanez S, Subramanian S, Ferencik M, et al. Focal arterial inflammation precedes subsequent calcification in the same location: A longitudinal FDG-PET/CT study. Circ Cardiovasc Imaging. 2013;6:747–754. doi: 10.1161/CIRCIMAGING.113.000382. [DOI] [PubMed] [Google Scholar]
- 16.Hop H, de Boer SA, Reijrink M, Kamphuisen PW, de Borst MH, Pol RA, et al. (18)F-sodium fluoride positron emission tomography assessed microcalcifications in culprit and non-culprit human carotid plaques. J Nucl Cardiol. 2018;26:1064. doi: 10.1007/s12350-018-1325-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bellinge JW, Francis RJ, Lee SC, Phillips M, Rajwani A, Lewis JR, et al. (18)F-sodium fluoride positron emission tomography activity predicts the development of new coronary artery calcifications. Arterioscler Thromb Vasc Biol. 2021;41:534–541. doi: 10.1161/ATVBAHA.120.315364. [DOI] [PubMed] [Google Scholar]
- 18.Joshi NV, Vesey AT, Williams MC, Shah AS, Calvert PA, Craighead FH, et al. 18F-fluoride positron emission tomography for identification of ruptured and high-risk coronary atherosclerotic plaques: A prospective clinical trial. Lancet. 2014;383:705–713. doi: 10.1016/S0140-6736(13)61754-7. [DOI] [PubMed] [Google Scholar]
- 19.Cecelja M, Moore A, Fogelman I, Frost ML, Blake GM, Chowienczyk P. Evaluation of aortic (18)F-NaF tracer uptake using PET/CT as a predictor of aortic calcification in postmenopausal women: A longitudinal study. JRSM Cardiovasc Dis. 2019;8:2048004019848870. doi: 10.1177/2048004019848870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fletcher AJ, Lembo M, Kwiecinski J, Syed MBJ, Nash J, Tzolos E, et al. Quantifying microcalcification activity in the thoracic aorta. J Nucl Cardiol. 2021 doi: 10.1007/s12350-020-02458-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.