Abstract
Background
It remains unclear whether immunosuppressive agents are effective in patients with immunoglobulin A nephropathy (IgAN). We investigated the efficacy of a mycophenolate mofetil (MMF) and corticosteroid combination therapy in patients with advanced IgAN.
Methods
We conducted a multicenter, randomized, placebo-controlled, parallel-group study of 48 weeks administration of MMF and corticosteroids in biopsy-proven advanced IgAN patients with estimated glomerular filtration rate (eGFR) of 20–50 mL/min/1.73 m2 and urine protein-to-creatinine ratio (UPCR) of >0.75 g/day. The primary outcome was complete (UPCR < 0.3 g/day) or partial (>50% reduction of UPCR compared to baseline) remission at 48 weeks.
Results
Among the 48 randomized patients, the percentage that achieved complete or partial remission was greater in thecombination therapy group than in the control group (4.2% vs. 0% and 29.1% vs. 5.0%, respectively). Compared with the combination therapy group, eGFR in the control group decreased significantly from week 36 onward, resulting in a final adjusted mean change of –4.39 ± 1.22 mL/min/1.73 m2 (p = 0.002). The adjusted mean changes after 48 weeks were 0.62 ± 1.30 and –5.11 ± 1.30 mL/min/1.73 m2 (p = 0.005) in the treatment and control groups, respectively. The UPCR was significantly different between the two groups; the adjusted mean difference was –0.47 ± 0.17 mg/mgCr and 0.07 ± 0.17 mg/mgCr in the treatment and control group, respectively (p = 0.04). Overall adverse events did not differ between the groups.
Conclusion
In advanced IgAN patients with a high risk for disease progression, combined MMF and corticosteroid therapy appears to be beneficial in reducing proteinuria and preserving renal function.
Keywords: Corticosteroids, IgA nephropathy, Immunosuppressants, Mycophenolate mofetil, Proteinuria
Introduction
Immunoglobulin A nephropathy (IgAN) is the most common type of glomerulonephritis and is particularly prevalent among East Asian populations [1]. Although several pathogenetic mechanisms have been suggested, the precise mechanism of IgAN remains controversial. Overproduction of abnormal undergalactosylated IgA autoantibodies has been reported to play an important role in antibody deposition in the glomerular mesangium, leading to mesangial cell proliferation and matrix accumulation [2]. The prognosis of IgAN varies among patients, with the daily amount of proteinuria and kidney function at the time of diagnosis serving as important prognostic factors. The disease slowly progresses to end-stage kidney disease at 10 years after disease onset in approximately 27% of patients, and the prognosis for patients of Pacific Asian origin is worse than that of Western populations [3,4].
There is no definitive treatment for IgAN. The Kidney Disease: Improving Global Outcomes (KDIGO) 2020 guidelines for IgAN suggest that patients who remain at high risk of chronic kidney disease progression despite maximal supportive care be considered for a 6-month course of corticosteroid therapy [5], which is known to reduce IgA deposition and circulating IgA autoantibodies [6,7]. However, this recommendation is problematic due to the significant risk of toxicity associated with corticosteroid use, and risk stratification prior to administration is imperative.
In addition to corticosteroids, another immunosuppressant used in clinical practice is mycophenolate mofetil (MMF), although its role is controversial. Several studies investigating the efficacy of MMF have reported conflicting results. According to Beckwith et al. [8], in a prospective, randomized clinical trial involving 40 IgAN patients, MMF treatment resulted in statistically significant improvements in endocapillary hypercellularity and cellular crescents at 2-year follow-up after the initial biopsy, and stabilization of serum creatinine levels at three years. Although several additional studies investigating the efficacy of MMF have been conducted, studies have reported conflicting results [9–14]. According to the most recent KDIGO guidelines, MMF has been suggested as a potential steroid-sparing agent in Chinese patients [5]. As Chinese and Korean individuals have similar ethnic backgrounds, MMF could also be considered in Korean IgAN patients.
This study, a multicenter, randomized, open-label, parallel-group study of 48-weeks of MMF and corticosteroids in biopsy-proven advanced IgAN patients with estimated glomerular filtration rate (eGFR) of 20–50 mL/min/1.73 m2, was designed to demonstrate the efficacy of combination therapy in patients with advanced IgAN.
Methods
Study population
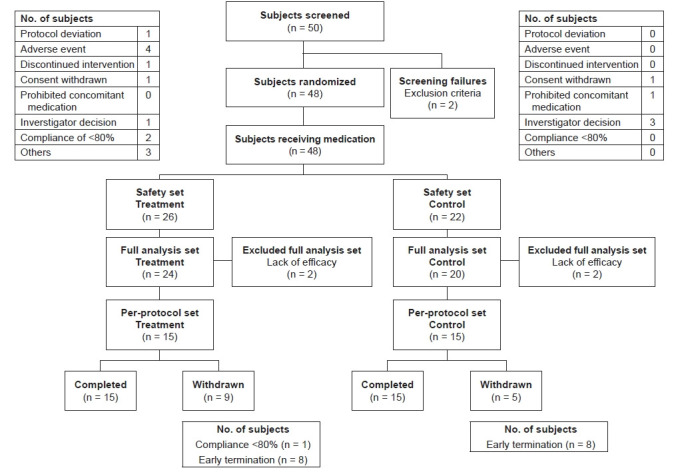
From September 2016 through July 2018, we screened 50 patients with biopsy-proven IgAN at seven tertiary institutions in Korea. After screening out two patients who failed the eligibility criteria, a total of 48 patients were enrolled in the present study (Fig. 1). The key eligibility criteria were biopsy-proven IgAN; age of 19 to 65 years; urine protein-to-creatinine ratio (UPCR) above 0.75 g/day; and an eGFR between 20 and 50 mL/min/1.73 m2 using the Modification of Diet in Renal Disease (MDRD) equation [15]. Major exclusion criteria were an eGFR lower than 20 mL/min/1.73 m2, systolic blood pressure above 160 mmHg or diastolic blood pressure above 100 mmHg, systemic inflammation or malignancy within the 5 years prior to screening, white blood cell count less than 3,000/mm3, or immunosuppression within 12 weeks prior to screening. During a 3-month run-in phase, all the patients received comprehensive supportive care, including renin-angiotensin-system (RAS) blockers.
Figure 1. Flow diagram for study participant enrollment and randomization.
The study was conducted in compliance with the Declaration of Helsinki, Good Clinical Practice guidelines, and standard operating procedures of the sponsor and was approved by the Institutional Review Board (IRB) of each participating center (host research institute, Yonsei University College of Medicine; IRB No. 4-2015-1199). Informed consent was obtained from each patient before the screening process.
Study design
This multicenter, randomized, open-labeled study was performed for 48 weeks (ClinicalTrial.gov NCT02981212; https://clinicaltrials.gov/ct2/show/NCT02981212). The eligible participants were randomized in a 1:1 ratio of MMF (Myrept, ChongKunDang Pharmaceutical, Seoul, Korea) and corticosteroid or control. The dose of MMF was 1,500 to 2,000 mg/day based on body weight. Prednisolone was prescribed at 0.5 mg/kg for 8 weeks and then tapered by 5 mg weekly until a final dose of 5 mg of prednisolone was maintained for the rest of the study period. Participants assigned to the control group received supportive care that included blood pressure management by prescription of maximally tolerated dose of RAS blockers and lifestyle modifications, consistent with treatment guidelines proposed by the KDIGO Glomerular Diseases Work Group [5].
Data collection
Demographic, medication, and laboratory data were collected at the time of study enrollment. Serum creatinine levels were determined using an isotope dilution mass spectrometry-traceable method at the central laboratories of each participating institution, with calibration against the reference. The eGFR was calculated using the MDRD creatinine equation [15]. Study participants visited the outpatient clinics of participating institutions every 12 weeks for a total of 48 weeks, where follow-up anthropometric, medication, and laboratory data (including blood chemistry tests and urinalysis), as well as safety data were collected at each visit.
Participant allocation
In this study, the size of the block was selected to be a multiple of two so that each subject was assigned a balanced allocation. Random number generation was performed using SAS version 9.3 (SAS Institute, Cary, NC, USA), and random assignment was carried out with a 1:1 allocation ratio between the treatment and control groups. A random identification number was assigned to each subject who met the inclusion and exclusion criteria using the Interactive Web Response System.
Efficacy and safety assessments
The primary outcome of the study was to evaluate the response rate of complete or partial remission at 48 weeks, defined as a UPCR less than 0.3 g/day and greater than 50% reduction of proteinuria compared to baseline, respectively. Additional study outcomes were response rates of complete and partial remission at 12, 24, and 36 weeks; changes in eGFR and UPCR at 24, 36, and 48 weeks; and the rate of kidney replacement therapy. The safety outcomes included adverse events including infections, gastrointestinal and hematological disorders, edema, and changes in vital signs and various laboratory parameters.
Statistical analyses
The proportion of remission in the treatment and the control group was set at 65% and 30%, respectively. The ratio of the groups was 1:1, and the level of significance (two-sided test) was 5% and 90%, respectively. As a result, it was necessary to include 40 subjects in each group, and assuming a dropout rate of 20%, an initial group size of 50 subjects. The total number of subjects required to be enrolled (treatment group plus control group) was calculated to be 100.
Survival curves and median survival time were estimated using the Kaplan-Meier method, and comparison between the groups was performed using the log-rank test. Continuous data were tested by an independent t test or Wilcoxon rank-sum test, and the results are presented as mean ± standard deviation or mean ± standard error. Categorical data were assessed using the chi-square test or Fisher exact test, and the results are presented as number and percentage. All analyses were conducted using STATA version 15 (STATA Corp., College Station, TX, USA).
Results
Baseline characteristics
Of the 48 randomized patients originally enrolled in the study, 44 were included in the full analyses, and 30 were included in the per-protocol analyses. The reasons for exclusion from the per-protocol analyses were major protocol violation (n = 1), adverse reaction (n = 4), no medication for more than 7 days (n = 1), withdrawal (n = 2), use of contraindicated medications (n = 1), study drug compliance <80% (n = 2), and other protocol violations (n = 7).
There were no statistically significant differences in baseline demographics or disease characteristics between the two groups (Table 1). At baseline, the mean age was 44.0 ± 10.6 years in the treatment group and 46.1 ± 7.8 years in the control group. The mean eGFR and UPCR were 36.3 ± 9.4 mL/min/1.73 m2 and 1.7 ± 0.6 mg/mgCr in the treatment group, respectively; and 33.0 ± 7.7 mL/min/1.73 m2 and 2.2 ± 1.0 mg/mgCr in the control group, respectively. All patients had taken RAS blockers for more than 3 months. No differences in physical examination or laboratory and electrocardiogram findings between the two groups were noted.
Table 1.
Baseline demographic and clinical characteristics of the study participants
| Characteristic | Treatment | Control |
|---|---|---|
| No. of patients | 24 | 20 |
| Demographic characteristic | ||
| Age (yr) | 44.0 ± 10.6 | 46.1 ± 7.8 |
| Male sex | 15 (62.5) | 10 (50.0) |
| Body mass index (kg/m2) | 24.5 ± 3.9 | 24.3 ± 3.5 |
| Clinical characteristic | ||
| SBP (mmHg) | 124.5 ± 10.6 | 129.5 ± 9.8 |
| DBP (mmHg) | 79.8 ± 9.03 | 78.7 ± 8.3 |
| Blood urea nitrogen (mg/dL) | 29.4 ± 10.3 | 30.6 ± 12.7 |
| Creatinine (mg/dL) | 2.0 ± 0.6 | 2.0 ± 0.5 |
| eGFR (mL/min/1.73 m2) | 36.3 ± 9.4 | 33.0 ± 7.7 |
| UPCR (mg/mgCr) | 1.7 ± 0.6 | 2.2 ± 1.0a |
Data are expressed as number only, mean ± standard deviation, or number (%).
DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; SBP, systolic blood pressure; UPCR, urine protein-to-creatinine ratio.
p = 0.02.
Of the 48 enrolled participants of this study, kidney biopsy results were available for 33, and their results are summarized in Supplementary Table 1 (available online). Kidney biopsy findings were similar among the two treatment groups.
Efficacy
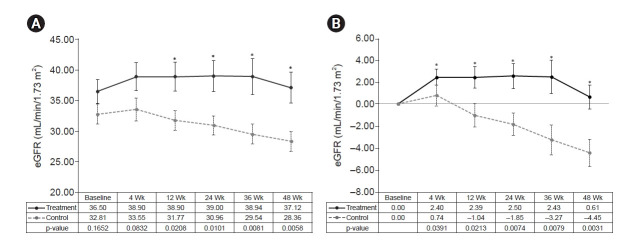
In the full analysis, the percentage of patients achieving remission at 48 weeks tended to be higher in the treatment group than in the control group (29.1% vs. 5.0% for partial remission, p = 0.05) (Table 2). One participant in the treatment group was in complete remission at 12 weeks after study enrollment. Changes in eGFR differed between the two groups. In the treatment group, the eGFR increased significantly at 4, 12, and 24 weeks after randomization compared to the baseline value (Fig. 2A). At 36 and 48 weeks, the adjusted mean changes were not significantly different compared to baseline, and the eGFRs were stable. In the control group, however, eGFR decreased significantly after 36 weeks; eGFR further decreased significantly at 48 weeks, resulting in an adjusted mean change of –4.39 ± 1.22 (p = 0.002). Comparing the results between the two groups, the treatment group was superior to the control with regard to adjusted mean change at 48 weeks (p = 0.01). The superiority was also significant at 12 weeks after randomization, and this effect was similar in the per-protocol analyses. Ultimately, the adjusted mean changes were 0.62 ± 1.30 and –5.11 ± 1.30 (p = 0.005) in the treatment and control groups at 48 weeks, respectively (Fig. 2B).
Table 2.
Primary outcomes among study participants at the end of the 48-week clinical trial
| Remission | Treatment (n = 24) | Control (n = 20) | p-value |
|---|---|---|---|
| Complete remission, n (%) | 1 (4.2) | 0 (0) | >0.99 |
| Duration to complete remission (wk) | 12.0 | ||
| Partial remission, n (%) | 7 (29.2) | 1 (5.0) | 0.05 |
| Duration to partial remission (wk) | 37.5 | 12.0 |
Figure 2. Time course of changes in eGFR in each group.
(A) Changes in eGFR (mean profile plot). (B) Adjusted mean changes in eGFR (mean difference vs. baseline).
eGFR, estimated glomerular filtration rate.
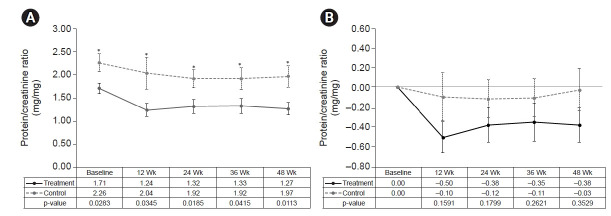
Although the percentage of patients achieving partial remission was marginally different between the two groups, the amount of proteinuria was significantly different (Table 3, Fig. 3). In the treatment group, the UPCR decreased significantly compared to baseline after 12 weeks (adjusted mean difference, –0.50 ± 0.69; p = 0.04), and this effect persisted until the end of the study period. However, there was no interval change in the UPCR in the control group. Overall, the UPCR differed significantly between the two groups, with adjusted mean differences of –0.47 ± 0.17 in the treatment group and 0.07 ± 0.17 in the control group (p = 0.04).
Table 3.
Urine protein-to-creatinine ratio at each visit
| Follow-up (wk) | Parameter | Treatment (n = 26) | Control (n = 22) | p-value |
|---|---|---|---|---|
| Baseline | Mean ± SD | 1.71 ± 0.56 | 2.26 ± 0.91 | 0.03 |
| 12 | Mean ± SD | 1.24 ± 0.64 | 2.04 ± 1.41 | 0.04 |
| Difference vs. baseline | –0.50 ± 0.69 | –0.10 ± 0.99 | 0.16 | |
| Adjusted mean difference ± SE | –0.52 ± 0.19 | –0.08 ± 0.21 | 0.14 | |
| 24 | Mean ± SD | 1.32 ± 0.67 | 1.92 ± 0.77 | 0.02 |
| Difference vs. baseline | –0.38 ± 0.72 | –0.12 ± 0.77 | 0.18 | |
| Adjusted mean difference ± SE | –0.47 ± 0.15 | –0.02 ± 0.17 | 0.06 | |
| 36 | Mean ± SD | 1.33 ± 0.68 | 1.92 ± 0.95 | 0.42 |
| Difference vs. baseline | –0.35 ± 0.80 | –0.11 ± 0.78 | 0.26 | |
| Adjusted mean difference ± SE | –0.43 ± 0.18 | –0.03 ± 0.19 | 0.14 | |
| 48 | Mean ± SD | 1.27 ± 0.52 | 1.97 ± 0.89 | 0.01 |
| Difference vs. baseline | –0.38 ± 0.68 | –0.03 ± 0.79 | 0.35 | |
| Adjusted mean difference ± SE | –0.47 ± 0.17 | 0.07 ± 0.17 | 0.04 |
SD, standard deviation; SE, standard error.
Figure 3. Time course of changes in urine protein-to-creatinine ratio in each group.
(A) Changes in urine protein-to-creatinine ratio (mean profile plot). (B) Adjusted mean changes in urine protein-to-creatinine ratio (mean difference vs. baseline).
No participants in either group had initiated kidney replacement therapy. No significant differences were noted between the two groups at 48 weeks with respect to clinical parameters, including blood pressure, heart rate, temperature, and weight, with the exception of white blood cell, eosinophil, and basophil counts (Table 4). The adjusted mean difference in white blood cell count was greater in the treatment group than in the control group (p = 0.02). The eosinophil and basophil counts were significantly reduced in the treatment group.
Table 4.
Laboratory parameters among study participants at 48 weeks
| Parameter | Treatment (n = 26) | Control (n = 22) | p-value |
|---|---|---|---|
| White blood cell (/µL) | 7,910 ± 1,580 | 6,980 ± 1,050 | 0.06 |
| Neutrophils (%) | 60.9 ± 8.9 | 56.3 ± 7.2 | 0.13 |
| Absolute neutrophil count | 4,840 ± 1,340 | 3,930 ± 750 | 0.08 |
| Lymphocytes (%) | 30.0 ± 8.0 | 33.2 ± 7.0 | 0.25 |
| Monocytes (%) | 7.6 ± 2.4 | 6.1 ± 1.4 | 0.04 |
| Eosinophils (%) | 1.1 ± 0.5 | 3.8 ± 2.8 | <0.001 |
| Basophils (%) | 0.4 ± 0.2 | 0.7 ± 0.3 | 0.02 |
| Hemoglobin (g/dL) | 13.4 ± 2.1 | 12.9 ± 2.1 | 0.53 |
| Platelets (109/L) | 245 ± 35 | 254 ± 54 | 0.56 |
| Blood urea nitrogen (mg/dL) | 28.5 ± 11.8 | 35.1 ± 13.7 | 0.09 |
| Total protein (g/dL) | 6.5 ± 0.5 | 6.8 ± 0.6 | 0.10 |
| Albumin (g/dL) | 4.1 ± 0.3 | 4.0 ± 0.3 | 0.27 |
| Glucose (mg/dL) | 98.4 ± 12.3 | 107.0 ± 23.4 | 0.22 |
| Sodium (mEq/L) | 141 ± 2 | 140 ± 3 | 0.59 |
| Potassium (mEq/L) | 4.4 ± 0.4 | 4.9 ± 0.2 | <0.001 |
| Chloride (mEq/L) | 105.9 ± 2.5 | 107.7 ± 2.6 | 0.11 |
Data are expressed as mean ± standard deviation.
Safety
There was no significant difference in overall adverse events between the two groups (Table 5), with 23 patients (88.5%) in the treatment group and 15 patients (68.2%) in the control group experiencing such events (p = 0.15). No significant difference in the incidence of severe adverse events was observed between the two groups. However, two serious adverse events occurred in both groups. In the treatment group, one patient experienced sudden death of unknown cause, and one patient experienced urinary tract infection. In the control group, one patient experienced foot fracture, and one patient experienced shoulder and cervical sprain.
Table 5.
Adverse events among study participants during the 48-week clinical trial
| Adverse event | Treatment (n = 26) | Control (n = 22) | p-value |
|---|---|---|---|
| Serious adverse event | |||
| Total | 2 (7.7) | 2 (9.1) | >0.99 |
| Type of serious adverse events | |||
| Death | 1 (3.8) | 0 (0) | |
| Adverse event | |||
| Overall | 23 (88.5) | 15 (68.2) | 0.15 |
| Drug-related adverse event | 12 (46.2) | 0 (0) | <0.001 |
| Type of adverse events | |||
| Infection | 9 (34.6) | 9 (40.9) | |
| Gastrointestinal disorder | 11 (42.3) | 2 (9.1) | |
| Hematologic disorder | 1 (3.8) | 0 (0) | |
| Edema | 3 (11.5) | 0 (0) | |
| Other disorders | 6 (23.1) | 0 (0) |
Data are expressed as number (%).
Drug-related adverse events in 12 patients (46.2%) of the treatment group included fatigue, abdominal pain, diarrhea, dysgeusia, gastritis, sinusitis, hypertension, urinary tract infection, esophagitis, dermatitis acneiform, dyspepsia, abdominal discomfort, vomiting, nausea, epigastric discomfort, facial edema, dry eye, and abdominal pain, all of which were tolerable. Drug compliance was good, at greater than 90% during the entire study period.
Discussion
The current study showed that the percentage of study participants achieving complete or partial remission of proteinuria was greater among those receiving MMF and corticosteroid combination therapy than in those receiving supportive care alone. We decided to stop this study due to ethical issues based on results of the interim analyses. Although the interim analyses revealed a marginally significant difference in primary outcome between the two groups, the secondary outcomes of eGFR and proteinuria were significantly different, with the difference in eGFR being greater at 48 weeks than at either 24 or 36 weeks. We also found changes in serum potassium, leukocyte, eosinophil, and basophil counts, where the increase in leukocytes and decrease in eosinophils and basophils might have been influenced by corticosteroids. The findings of this study add evidence to the current literature that MMF could potentially be prescribed as a steroid-sparing agent in patients with advanced IgAN.
The reported effects of combination therapy with corticosteroids and cytotoxic agents are inconsistent. In the STOP-IgA (Supportive Versus Immunosuppressive Therapy for the Treatment of Progressive IgA Nephropathy) trial, combination treatment with a corticosteroid and cyclophosphamide was not effective for changes in eGFR and proteinuria [16]. Furthermore, in another study, the addition of azathioprine to corticosteroids was not effective in IgAN patients [17]. However, combination therapy has shown beneficial effects in other studies; for example, coadministration of corticosteroids and cytotoxic agents stabilized eGFR in patients with IgAN in two prospective, randomized, controlled trials [18,19]. The results of our study are consistent with the findings of previous studies, demonstrating clinical remission and significant changes in eGFR and proteinuria among treatment groups. The eGFR improved with combination therapy at 12 weeks after treatment, and this beneficial effect was more prominent at 48 weeks. Proteinuria exhibited a pattern similar to that of eGFR, significantly decreasing in the treatment group but increasing in the control group.
It is unclear why the effects of combination therapy were different among groups, but one of several plausible explanations could be the effect of MMF. Indeed, inconsistent results have been documented for MMF monotherapy and combination therapy in several studies [9,10,19–22]. Among 33 children with steroid-resistant IgA nephropathy or nephrotic syndrome, 21 and six patients receiving combined MMF and corticosteroid therapy were able to achieve complete or partial remission of proteinuria, respectively [22]. Recent randomized clinical trials have indicated that combination therapy with MMF and corticosteroids had a similar effect on proteinuria reduction and fewer adverse events than full-dose corticosteroids in IgAN patients [13]. Overall, MMF has been reported to be superior to cyclophosphamide. Combination therapy using MMF and corticosteroids achieved a higher remission rate than combination therapy using cyclophosphamide and corticosteroid in patients with severe IgAN, and the MMF and corticosteroid combination reduced proteinuria and improved renal function. In addition, the incidence of adverse events was significantly lower in patients taking MMF than in those taking cyclophosphamide [12].
Immunosuppression-related adverse events represent one of the main obstacles for treatment of IgAN. The TESTING (Therapeutic Evaluation of Steroids in IgA Nephropathy Global) trial indicated that corticosteroids significantly reduced adverse renal outcomes; however, the rate of serious adverse events was 14.7% in the treatment group versus 3.2% in the control group [23]. As expected, adverse events in the present study occurred in a significantly greater percentage of participants in the combination therapy group. However, with the exception of one patient who died of an unknown cause, most of the side effects were tolerable. Given the lower incidence of side effects of combination therapy with MMF and corticosteroids than with high-dose corticosteroids alone [13], this combination regimen could be an alternative to high-dose corticosteroids in patients prone to drug-related side effects.
Some limitations of our study are worth noting. First, this study was not completed as scheduled; only 50% of subjects were randomized. As only patients with advanced IgA nephropathy, defined as those with eGFR of <50 mL/min/1.73 m2, were included, participant enrollment was more difficult than anticipated. A larger study population would have strengthened the findings of this study. Second, although kidney biopsy findings were available for 33 of 48 participants, more detailed findings, such as duration between pathologic diagnosis and initiation of immunosuppressant therapy, could have provided further insights into how different pathologic characteristics could affect treatment outcomes. Third, the dropout rate was high; only 30 of the 44 patients completed the study. Fourth, the control group had higher baseline proteinuria than the treatment group, which might account for the difference in outcomes of proteinuria. Nonetheless, the primary outcome of complete or partial remission tended to be significant, and the secondary outcomes were significantly beneficial in the MMF and corticosteroid combination therapy group.
In patients with advanced IgAN with a high risk of disease progression, combination therapy with MMF and corticosteroid appears to be beneficial in reducing proteinuria and preserving renal function, with relatively tolerable safety profiles. Although the results of this study suggest a potential benefit, further studies are warranted to validate the conclusion.
Acknowledgments
The authors thank the Medical Illustration & Design team within the Medical Research Support Services of Yonsei University College of Medicine for all artistic support related to this work.
Footnotes
Conflicts of interest
This study was sponsored by ChongKunDang Pharmaceutical. All authors have no conflicts of interest to declare.
Funding
The study received financial support from ChongKunDang Pharmaceutical.
Authors’ contributions
Conceptualization: BSK, BSC
Data curation: All authors
Formal analysis: SYH, CYJ, BSC, BSK
Funding acquisition: BSK
Investigation: All authors
Supervision: BSC, BSK
Writing–original draft: All authors
Writing–review & editing: All authors
All authors read and approved the final manuscript.
Supplementary Materials
References
- 1.Wyatt RJ, Julian BA. IgA nephropathy. N Engl J Med. 2013;368:2402–2414. doi: 10.1056/NEJMra1206793. [DOI] [PubMed] [Google Scholar]
- 2.Suzuki H, Kiryluk K, Novak J, et al. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22:1795–1803. doi: 10.1681/ASN.2011050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barbour SJ, Espino-Hernandez G, Reich HN, et al. The MEST score provides earlier risk prediction in lgA nephropathy. Kidney Int. 2016;89:167–175. doi: 10.1038/ki.2015.322. [DOI] [PubMed] [Google Scholar]
- 4.Barbour SJ, Cattran DC, Kim SJ, et al. Individuals of Pacific Asian origin with IgA nephropathy have an increased risk of progression to end-stage renal disease. Kidney Int. 2013;84:1017–1024. doi: 10.1038/ki.2013.210. [DOI] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021;100(4S):S1–S276. doi: 10.1016/j.kint.2021.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Floege J. The pathogenesis of IgA nephropathy: what is new and how does it change therapeutic approaches? Am J Kidney Dis. 2011;58:992–1004. doi: 10.1053/j.ajkd.2011.05.033. [DOI] [PubMed] [Google Scholar]
- 7.Cheng IK, Chan KW, Chan MK. Mesangial IgA nephropathy with steroid-responsive nephrotic syndrome: disappearance of mesangial IgA deposits following steroid-induced remission. Am J Kidney Dis. 1989;14:361–364. doi: 10.1016/s0272-6386(89)80168-4. [DOI] [PubMed] [Google Scholar]
- 8.Beckwith H, Medjeral-Thomas N, Galliford J, et al. Mycophenolate mofetil therapy in immunoglobulin A nephropathy: histological changes after treatment. Nephrol Dial Transplant. 2017;32(suppl 1):i123–i128. doi: 10.1093/ndt/gfw326. [DOI] [PubMed] [Google Scholar]
- 9.Tang S, Leung JC, Chan LY, et al. Mycophenolate mofetil alleviates persistent proteinuria in IgA nephropathy. Kidney Int. 2005;68:802–812. doi: 10.1111/j.1523-1755.2005.00460.x. [DOI] [PubMed] [Google Scholar]
- 10.Frisch G, Lin J, Rosenstock J, et al. Mycophenolate mofetil (MMF) vs placebo in patients with moderately advanced IgA nephropathy: a double-blind randomized controlled trial. Nephrol Dial Transplant. 2005;20:2139–2145. doi: 10.1093/ndt/gfh974. [DOI] [PubMed] [Google Scholar]
- 11.Maes BD, Oyen R, Claes K, et al. Mycophenolate mofetil in IgA nephropathy: results of a 3-year prospective placebo-controlled randomized study. Kidney Int. 2004;65:1842–1849. doi: 10.1111/j.1523-1755.2004.00588.x. [DOI] [PubMed] [Google Scholar]
- 12.Liu X, Dewei D, Sun S, et al. Treatment of severe IgA nephropathy: mycophenolate mofetil/prednisone compared to cyclophosphamide/prednisone. Int J Clin Pharmacol Ther. 2014;52:95–102. doi: 10.5414/CP201887. [DOI] [PubMed] [Google Scholar]
- 13.Hou JH, Le WB, Chen N, et al. Mycophenolate mofetil combined with prednisone versus full-dose prednisone in IgA nephropathy with active proliferative lesions: a randomized controlled trial. Am J Kidney Dis. 2017;69:788–795. doi: 10.1053/j.ajkd.2016.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Natale P, Palmer SC, Ruospo M, et al. Immunosuppressive agents for treating IgA nephropathy. Cochrane Database Syst Rev. 2020;3:CD003965. doi: 10.1002/14651858.CD003965.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 16.Rauen T, Eitner F, Fitzner C, et al. Intensive supportive care plus immunosuppression in IgA nephropathy. N Engl J Med. 2015;373:2225–2236. doi: 10.1056/NEJMoa1415463. [DOI] [PubMed] [Google Scholar]
- 17.Pozzi C, Andrulli S, Pani A, et al. Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. J Am Soc Nephrol. 2010;21:1783–1790. doi: 10.1681/ASN.2010010117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ballardie FW, Roberts IS. Controlled prospective trial of prednisolone and cytotoxics in progressive IgA nephropathy. J Am Soc Nephrol. 2002;13:142–148. doi: 10.1681/ASN.V131142. [DOI] [PubMed] [Google Scholar]
- 19.Chen X, Chen P, Cai G, et al. A randomized control trial of mycophenolate mofeil treatment in severe IgA nephropathy. Zhonghua Yi Xue Za Zhi. 2002;82:796–801. [PubMed] [Google Scholar]
- 20.Hogg RJ, Bay RC, Jennette JC, et al. Randomized controlled trial of mycophenolate mofetil in children, adolescents, and adults with IgA nephropathy. Am J Kidney Dis. 2015;66:783–791. doi: 10.1053/j.ajkd.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Roccatello D, Rossi D, Marletto F, et al. Long-term effects of methylprednisolone pulses and mycophenolate mofetil in IgA nephropathy patients at risk of progression. J Nephrol. 2012;25:198–203. doi: 10.5301/JN.2011.8452. [DOI] [PubMed] [Google Scholar]
- 22.Kang Z, Li Z, Duan C, et al. Mycophenolate mofetil therapy for steroid-resistant IgA nephropathy with the nephrotic syndrome in children. Pediatr Nephrol. 2015;30:1121–1129. doi: 10.1007/s00467-014-3041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lv J, Zhang H, Wong MG, et al. Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: the TESTING randomized clinical trial. JAMA. 2017;318:432–442. doi: 10.1001/jama.2017.9362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.