Abstract
Background
Firefighters may experience high environmental temperatures or carry out intensive physical tasks, or both, which leads to increased core body temperature and risk of fatalities. Hence there is a need to remotely and non-invasively monitor core body temperature.
Methods
Estimated (heart rate algorithm) and actual core body temperature (ingested telemetric pill) measures were collected simultaneously for comparison during training exercises on 44 firefighter volunteers.
Results
Prediction of core body temperature varied, with no specific identifiable pattern between the algorithm values and directly measured body core temperatures. Group agreement of Lin's Concordance of 0.74 (95% Upper 0.75, lower CI 0.73), was deemed poor.
Conclusion
From individual agreement data Lin's Concordance was variable (Min 0.11, CI 0.13–0.01; Max 0.83, CI 0.86–0.80), indicating that the heart rate algorithm approach was not suitable for core body temperature monitoring in this population group, especially at the higher more critical core body temperatures seen.
Keywords: Firefighter, Heart rate estimation, Internal temperature, Kalman filter
Abbreviations: CBTm, actual core temperature; BA, breathing apparatus; CI, confidence intervals; CBT, core body temperature; CT, core temperature; CBTest, estimated core temperature; HR, heart rate; LOA, limits of agreement; PARQ, physical activity readiness questionnaire; PPE, personal protective equipment; SEM, sensor electronics module
1. Introduction
Modern firefighting involves a diverse range of activities that often take place in abnormal environmental temperatures. At the extremes, this can include the need for maximal levels of physical exertion in extreme temperatures while wearing breathing apparatus (BA) and full personal protective equipment (PPE). This presents a unique challenge to the firefighter's physiology, particularly their ability to thermo-regulate. The combination of internal metabolic heat production and external heat transfer from the environment, combined with an inability to remove heat, results in rapid rises in core body temperature that impacts the firefighter's physical capacity, their awareness and decision-making ability, and ultimately, their safety [1].
Although there is a highly individualised response to elevated temperatures, the margin for safety is small. A rise of as little as 1–2°C above the normal core temperature of ∼37°C can result in detriments to mental and physical performance, while a rise of 3°C is almost certainly a threat to safety. There is, therefore, a need to be able to monitor the core temperature and physiology of firefighters.
Previously, core body temperature assessment has been undertaken using a range of methods; however, these are either impractical in an operational setting (rectal and oesophageal) or unreliable (tympanic) [1]. To be operationally practical, any method of temperature assessment has to be non-invasive and unobtrusive. This means that it must be easy to administer, not restrict movement, and must not interfere with communication or ambient noise. This has led researchers to investigate indirect methods such as heat flux and heart rate parameters to estimate core temperature from non-invasive measures [[2], [3], [4], [5]].
Buller and co-workers [6] presented a method to estimate CT from the time series observations of HR under steady-state conditions. Using data from ten laboratory and field trials (involving 52,000 matched data sets drawn mainly from well-trained young athletes or military personnel), 95% (2 SD) of all core temperature estimates fell within 0.63°C with an overall bias of –0.03 ± 0.32°C. Within this data set, there were outliers (approximately 5% of the population) for whom the model did not provide a good predictor of CT. This appears to be specific to the individual rather than the conditions.
While the approach used by Buller appears to be a suitable predictor of CT in this population under steady-state conditions, it is unknown how well this method will work across a more diverse population (male/female; untrained/trained; younger/older) and under more varied work conditions (short/long; continuous/intermittent; static/dynamic). More specifically, it is unknown how well this method will work in a firefighter population exposed to firefighter specific activities under typical environmental conditions.
Hence the aim of this study was to determine the level of agreement between the estimated core temperature CBTest (determined via time-series HR observations) and actual core temperature CBTm (determined from a swallowed telemetric pill) in firefighters exposed to live-fire exercises.
2. Methods
2.1. Participants
All volunteers monitored during their live-fire training exercises were recruited from the UK fire and rescue service via convenience sampling. Prior to recruitment, potential participants at local fire stations were given a presentation to enable them to understand the study and decide to take part or not. Written informed consent was then given by all those willing to participate in the study. All human testing was approved by the local ethics committee and was carried out in accordance with resolution 466/2012 of the National Health Council and to the updated Declaration of Helsinki 2013 – ethical principles for research involving humans.
2.2. Equipment
Estimated and actual core temperature measures were collected using the Equivital EQO2Life monitor, VitalSense core temperature pill, and Black Ghost software (Hidalgo, Cambridge, UK). Data were logged on the sensor electronics module (SEM) and also transmitted in real time via Bluetooth to the Equivital app on a smartphone (Samsung G4) and onward, via 4G, to the Equivital black ghost server. Estimation of core temperature occurred remotely on the Equivital server and was displayed in real time and logged (every 5 seconds) via access to the Black Ghost website using a laptop computer. Estimation of CBT (CBTest) was determined in the Equivital black ghost software using a HR algorithm [6,7] and displayed in real time, along with simultaneous telemetric pill measured CBT (CBTm) and HR.
2.3. Protocols
Approximately 5 hours prior to monitoring, participants swallowed the VitalSense pill. This was to allow sufficient time for the pill to pass through the stomach and into the gut and reduce the chance of the readings being affected by ingestion of food or drink. Participants were then fitted with the life monitor sensor harness just prior to the beginning of the live-fire exercises. The sensor harnesses are sized from 1–9 and were fitted such that they were tight but comfortable on the middle of three adjustment settings. This was to ensure optimum contact for heart rate measurement.
At this point, the phone was paired with the SEM, and all readings were checked via the Equivital app on the phone. Once the actual core temperature (and correct pill ID) and heart rate were displayed on the phone, this was then placed in the inside pocket of the PPE jacket. From this point on, data were transmitted and collected in parallel on the SEM and on the Black Ghost server.
Estimated core temperature, HR, and actual core temperature were then displayed in real time on the laptop computer. Entry and exit times for all participants were recorded for their live-fire exercise and used to trim the data set for analysis.
We monitored and recorded CBTest, HR, and CBTm during a range of typical firefighter training scenarios. These included: hot and humid burn room sessions, operational license training for serving firefighters (house fire exercises), and supervisory and training activities by firefighter instructors under operational license or hot and humid conditions. Typical temperatures ranged from (120–250 0C) and task duration (10–40 minutes).
These conditions were deemed by the fire service to represent the range of activities and environments (including duration, activity type, and environmental conditions) commonly encountered during operational firefighter duties that require PPE and BA.
2.4. Analysis
In order to examine the ‘agreement’ for each individual's estimated vs. the actual core temperature measurement, it was intended to apply the approach developed by Bland and Altman that has been widely utilised by other similar studies [8]. Here the limits of agreement (LOA) plot would indicate any bias and spread of the compared methods to determine body core temperature. Underlying this approach, however, are certain assumptions that relate to data normality and homoscedasticity across the data range. Normality was examined in SPSS (ver 25) via the Shapiro Wilks test and homoscedasticity via the Koenker test (custom syntax code). Both normality and homoscedasticity were seen to be violated in a number of cases that rendered this approach unsuitable for the purposes of this research. Therefore, in order to analyse the whole data set in a consistent way, alternate approaches were utilised. Data were expressed as median, and interquartile range, along with ranges for comparison. To examine the agreement, Lin's Concordance [9] was used, expressed as an r value (with 95% CI). To further examine the variability in patterns of agreement, participants' data were divided into upper, mid, and lower bandings (tertiles) for age and body mass.
3. Results
Forty-four firefighters (8 female; 36 male) took part in the present study, with age ranges from 19–50 years and body mass ranging from 48–110 kg. Physical characteristics (age, body mass and height ± SD) for the firefighters are presented in Table 1. Table 1 shows the division of subjects by age and weight into three subgroups. These subgroup data were then analysed as for the pooled group data to determine if body mass or age showed any specific patterns of estimated to measured core body temperature.
Table 1.
Tertile data ranges of age, body mass and height for the subjects. (Data expressed as mean ± SD)
| Tertile data (age) | ||
|---|---|---|
| Age (Years) | Body Mass (kg) | Height (cm) |
| 19–29 (24 ± 3.5) n = 14 | 78.4 ± 14.3 | 175.0 ± 7.5 |
| 30–40 (35 ± 3.4) n = 19 | 84.6 ± 11.8 | 179.4 ± 7.3 |
| 41–50 (44.7 ± 3.0) n = 11 |
86.5 ± 10.9 |
178.4 ± 6.8 |
| Tertile data (Body mass) | ||
| Body mass (kg) |
Age (Years) |
Height (cm) |
| 48–68 (61.3 ± 7.2) n = 6 | 29.3 ± 8.2 | 166.7 ± 7.7 |
| 69–89 (79.8 ± 5.7) n = 23 | 34.3 ± 9.6 | 176.1 ± 5.3 |
| 90–110 (95.9 ± 6.0) n = 15 | 37.1 ± 6.2 | 183.8 ± 3.3 |
The general agreement between the CBTm and the CBTest was examined by the determination of Lin's Concordance. Here all individual data (n = 44) were pooled and entered into the analysis. Fig. 1 shows the group scatter plot of measured core body temperature (CBTm) against estimated core body temperature (CBTest). The Lin's Concordance r value of 0.742, according to the suggested scales of Lin, was poor. Here, at the upper end of the body core temperatures, it can be seen that the estimated core temperatures are underestimating the measured core temperatures by approx 0.75 0C.
Fig. 1.
Group Scatter plot of CBTest against CBTm. Lin's concordance (r) = 0.742 (CI = upper = 0.749; lower = 0.734). Red lines = 95% prediction intervals; blue lines = 95% CI for line fit. Estimated Core temp = 0.708 × Measured Core Temp +10.996; r2 = 0.584.
Fig. 2(a–c) shows the agreement between CBTm and CBTest with Lin's concordance r values for each plot. As for the group data, the Lin's Concordance r values of 0.78, 0.62 and 0.67 for the tertile groups by age were all poor for agreement between the measured and estimated core temperature values. Data split by age (a = 19–29; b = 30–40; and c = 41–50 yrs).
Fig. 2.
Scatter plots of CBTest vs. CBTm for the tertile groups by age, 19–29 yrs (n = 14); 30–40 yrs (n = 19) and 41–50 yrs (n = 11). Lin's concordance (r) 0.78 (CI upper = 0.79; lower = 0.77); (r) = 0.62 (CI upper = 0.63; lower = 0.61); and (r) = 0.67, (CI upper = 0.68; lower = 0.65) for a, b and c respectively. Red lines = 95% prediction intervals; blue lines = 95% CI for line fit. (a) Estimated Core temp = 0.819 x Measured Core Temp + 6.727; r2 = 0.692. (b) Estimated Core temp = 0.679 x Measured Core Temp + 11.907; r2 = 0.569. (c) Estimated Core temp = 1.121 x Measured Core Temp –4.621; r2 = 0.542.
For examining if any pattern existed between the estimated and measured core body temperature, the data were split by body mass tertiles (See Fig. 3). Data were split by body mass (48–68 kg; 69–89 kg; and 90–110 kg) for graphs (a–c), respectively. Lin's Concordance results (r = 0.66, 0.66, 0.74 respectively) suggest poor agreement between the measured and estimated core body temperature values.
Fig. 3.
Scatter plots of CBTest vs. CBTm for the tertile groups by body mass, 48–68 kg (n = 6); 69–89 kg (n = 23) and 90–110 kg (n = 15). Lin's concordance (r) = 0.66 (CI upper = 0.68; lower = 0.64); (r) = 0.66 (CI upper = 0.67; lower = 0.65); and (r) = 0.74 (CI upper = 0.75; lower = 0.73) for a, b, and c respectively. Red lines = 95% prediction intervals; blue lines = 95% CI for line fit. (a) Estimated Core temp = 0.875 x Measured Core Temp + 4.420; r2 = 0.729. (b) Estimated Core temp = 0.750 x Measured Core Temp + 9.373; r2 = 0.489. (c) Estimated Core temp = 0.756 x Measured Core Temp + 9.037; r2 = 0.709.
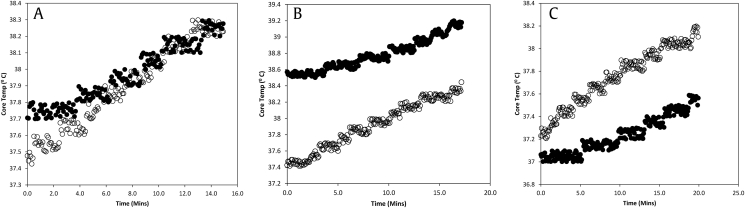
Examples of the variation in agreement observed between the measured and heart rate estimated core body temperatures can be seen in Fig. 4. Large individual differences can be seen from the plots, with approximately up to a degree underestimation at the upper temperatures (Fig. 4b), and approximately 0.7 of a degree overestimation at the upper temperatures (Fig. 4c).
Fig. 4.
Individual firefighter scatter plots illustrating good (a), under (b) and over (c) estimation of the CBTm. Lin's Concordance values of r = 0.83, CI upper 0.86; lower 0.80; r = 0.12, CI upper 0.14; lower 0.0.09; r = 0.21, CI upper 0.24; lower 0.18, for a, b and c respectively. (●) represents measured core temperature, (○) represents estimated core temperature.
4. Discussion
Overall, the general agreement between the CBTest and CBTm indicated that the heart rate algorithm method was not a valid solution to monitor the immediate physiology of firefighters under the conditions tested here. Relatively large discrepancies could be seen at the critical higher core body temperatures, with up to 1.7 0C variation between the estimated and the actual core temperatures seen. The inter-individual variations in the agreement were evident even when describing the data by way of age and body mass tertiles (See Fig. 2, Fig. 3). This lack of certainty in terms of the pattern of agreement rendered the estimation approach invalid as a method to determine core body temperature.
There are clear safety or operational issues resulting from either underestimation or overestimation of CBT. From a firefighter safety perspective, any underestimation presents a problem whereby the incident commander will be receiving information that does not represent the true level of thermal strain to which the firefighter is exposed. From an operational decision-making perspective, any overestimation could lead to a firefighter being withdrawn from the fire on safety grounds when they were not in any danger, thus requiring additional firefighters and time to complete any given task.
Moreover, in this study, there also appears to be no pattern related to any particular firefighting activity. (It is likely, however, that even within the range of firefighter activities tested, very few would have approximated the steady-state conditions under which Buller and co-workers [6] developed the algorithm). Importantly, most of the activities undertaken in this study were intermittent in nature, requiring a combination of static and dynamic work of varying intensities with a range of muscular and physiological stressors. This alone may be a major factor relating to the discordance between the estimated and actual core body temperature measures. Each firefighter would have performed different tasks, requiring intermittent muscle action and work of both a dynamic and static nature, possibly further complicating and confounding the ability of the algorithm to estimate core body temperature from HR.
Previous work by Welles and colleagues [10] have shown the approach used here to be a suitable method for monitoring the core body temperatures in military personnel. However, there are not only distinct differences between both the cohorts used here and those in the work by Welles et al but also, and possibly more importantly, the work carried out by the firefighters in this study was reflective of typical firefighter tasks and not steady state working as described above. This would likely result in varying cardiac requirements for any given amount of work (varied by type of muscular action, for example), and it could be suggested that this varying cardiac response would differentially affect the work/heart rate relationship, both within individuals and across individuals, thus potentially explaining the variety in patterns seen here.
Other important observations here relate to considerations of the apparent decoupling of HR and temperature under conditions where the firefighter is no longer undertaking physical activity in the heat (data not shown). This manifests as a discrepancy between the CBTest and CBTm on leaving the fire, a situation which generally saw CBTm rise and CBTest remain relatively constant or fall.
There are a number of possible explanations for the patterns observed. The continued rise in CBTm that was often observed post-fire may be due to passive heating from continued PPE wear and continued metabolic heat being returned to the core from the muscles, immediately post-fire. Where this occurs at the same time as a reduced activity level, it may present competing drivers for heart rate. Indeed in work carried out by Weippert and co-workers [11], where heart rate was fixed, and contraction mode was varied. It was observed that perceived ratings of exertion and blood pressure were higher for the isometric condition compared to the dynamic condition, leading them to conclude that cardiovascular control may be different between the contraction modalities.
We were unable to control for differential patterns of work, heat exposure, and time in the fire. This was largely due to the authenticity that was designed into the live fire exercises by the instructors, where firefighters had differing and varying roles within it. It is important to note, however, that the aim of this research was to investigate the suitability of the HR approach in a commercial device, in real world conditions, and as such, it is important that it works for all situations, including being practical during varied work tasks, typical of firefighter activities.
Because we were testing operational firefighters under normal training activities, we recruited volunteers from those firefighters who had already been deemed fit enough to undertake live fire exercises. Although we made no specific attempt to control for medication, rather tested a convenience sample from the pool of available firefighters, we did, however, exclude those on beta-blockers as identified in the PARQ. We do recognise that other medications may have affected the relationship between CBTm and CBTest.
Although the algorithm used in this study did not appear to provide a suitable estimate of core body temperature within the population tested and in the tasks undertaken, there may be a case for the development of individualised algorithms (i.e., the algorithm used here but ‘calibrated’ to each individual). Unlike the approach taken here, where the aim was to use a generalised algorithm, based on fairly homogenous military data under mostly steady-state conditions, it may be possible to investigate an approach where the algorithm is informed by more individualised task specific data. Moreover, there may be some benefit in combined approaches as explored by Xu et al [12]. For example, Welles et al, [13] estimated CBT from a combination of HR, skin temperature and heat flux using a Kalman Filter approach.
Funding
This work was supported by The Greater Manchester Fire and Rescue Service.
Ethical approval
This work was approved by the local University ethics committee.
Consent to participate
All firefighters gave their written consent after reviewing a participant information sheet.
Consent for publication
All data are anonymised and publication was agreed/reviewed as part of the ethical approval process.
Authors contributions
All named authors were involved in specific aspects of planning/approval of the project, subject recruitment and collecting data and data analysis, writing of the manuscript.
Conflicts of interest
None.
Acknowledgments
Thanks go to Greater Manchester Fire and Rescue Service who provided funding and logistical support for this work.
References
- 1.Lim C.L., Byrne C., Lee J.K. Human thermoregulation and measurement of body temperature in exercise and clinical settings. Ann Acad Med Singapore [Internet] 2008 Apr;37(4):347–353. http://www.ncbi.nlm.nih.gov/pubmed/18461221 [cited 2018 Oct 28]. Available from: [PubMed] [Google Scholar]
- 2.Fox R.H., Solman A.J., Isaacs R., Fry A.J., MacDonald I.C. A new method for monitoring deep body temperature from the skin surface. Clin Sci. 1973 Jan;44(1):81–86. doi: 10.1042/cs0440081. [DOI] [PubMed] [Google Scholar]
- 3.Fox R.H., Solman A.J. A new technique for monitoring the deep body temperature in man from the intact skin surface. J Physiol. 1971 Jan;212(2):8P–10P. [PubMed] [Google Scholar]
- 4.Kitamura K.-I., Zhu X., Chen W., Nemoto T. Development of a new method for the noninvasive measurement of deep body temperature without a heater. Med Eng Phys. 2010 Jan;32(1):1–6. doi: 10.1016/j.medengphy.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Tachibana S., Chida Y., Yamakage M. Using the Bair Hugger TM temperature monitoring system in neck and chest regions: a pilot study. JA Clin Reports. 2019 May;5(1):32. doi: 10.1186/s40981-019-0252-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buller M.J., Tharion W.J., Cheuvront S.N., Montain S.J., Kenefick R.W., Castellani J., et al. Estimation of human core temperature from sequential heart rate observations. Physiol Meas [Internet] 2013 Jul 1;34(7):781–798. doi: 10.1088/0967-3334/34/7/781. http://stacks.iop.org/0967-3334/34/i=7/a=781?key=crossref.8c1701eaf2975a48c9f4e6ac1576bc99 [cited 2018 Mar 2]. Available from: [DOI] [PubMed] [Google Scholar]
- 7.Buller M.J., Tharion W.J., Duhamel C.M., Yokota M. Real-time core body temperature estimation from heart rate for first responders wearing different levels of personal protective equipment. Ergon [Internet] 2015 Nov 2;58(11):1830–1841. doi: 10.1080/00140139.2015.1036792. http://www.tandfonline.com/doi/full/10.1080/00140139.2015.1036792 [cited 2018 Mar 2]. Available from: [DOI] [PubMed] [Google Scholar]
- 8.Feng J., Zhou C., He C., Li Y., Ye X. Development of an improved wearable device for core body temperature monitoring based on the dual heat flux principle. Physiol Meas [Internet] 2017 Apr 1;38(4):652–668. doi: 10.1088/1361-6579/aa5f43. http://stacks.iop.org/0967-3334/38/i=4/a=652?key=crossref.ae487a50ff09ff581d9bf824f9542f7c [cited 2018 Mar 2]. Available from: [DOI] [PubMed] [Google Scholar]
- 9.Lin L.I., McBride G., Bland J.M., Altman D.G. A proposal for strength-of-agreement criteria for Lin’s Concordance Correlation Coefficient. NIWA Client Rep. 2005;45(1):307–310. [Google Scholar]
- 10.Welles A.P., Buller M.J., Margolis L., Economos D., Hoyt R.W., Richter M.W. Thermal-work strain during marine rifle squad operations in Afghanistan. Mil Med [Internet] 2013 Oct 1;178(10):1141–1148. doi: 10.7205/MILMED-D-12-00538. https://academic.oup.com/milmed/article/178/10/1141-1148/4352250 [cited 2018 Mar 2]. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Weippert M., Behrens M., Gonschorek R., Bruhn S., Behrens K. Muscular contraction mode differently affects autonomic control during heart rate matched exercise. Front Physiol [Internet] 2015;6:156. doi: 10.3389/fphys.2015.00156. https://www.frontiersin.org/article/10.3389/fphys.2015.00156 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu X., Karis A.J., Buller M.J., Santee W.R. Relationship between core temperature, skin temperature, and heat flux during exercise in heat. Eur J Appl Physiol [Internet] 2013 Sep 18;113(9):2381–2389. doi: 10.1007/s00421-013-2674-z. http://link.springer.com/10.1007/s00421-013-2674-z [cited 2018 Oct 28]. Available from: [DOI] [PubMed] [Google Scholar]
- 13.Welles A.P., Xu X., Santee W.R., Looney D.P., Buller M.J., Potter A.W., et al. Estimation of core body temperature from skin temperature, heat flux, and heart rate using a Kalman filter. Comput Biol Med. 2018 Aug;99:1–6. doi: 10.1016/j.compbiomed.2018.05.021. [DOI] [PubMed] [Google Scholar]