Abstract
OBJECTIVE
The association between structural racism, as captured by historic residential redlining practices under the Home Owners’ Loan Corporation (HOLC), and present-day diabetes mortality, and years of life lost (YLL), remains unknown.
RESEARCH DESIGN AND METHODS
Age-standardized mortality and YLL data were combined with historic HOLC redlining data for the city of Seattle, WA (a sample of 109 census tract–level observations) for each of the years 1990 through 2014 (25 years). Spatial autoregressive regression analyses were used for assessment of the association between an area’s historic HOLC redlining score and diabetes (and all-cause) mortality and YLL.
RESULTS
Spatial autoregressive model estimates indicate that an area’s HOLC redlining score explains 45%–56% of the variation in the census tract–level diabetes mortality rate and 51%–60% of the variation in the census tract diabetes YLL rate between the years of 1990 and 2014. For 2014, estimates indicate that areas with a unit-higher HOLC grade are associated with 53.7% (95% CI 43.3–64.9; P < 0.01) higher diabetes mortality rates and 66.5% (53.7–80.4; P < 0.01) higher diabetes YLL rate. Magnitudes of marginal effects were consistently larger for diabetes than for all-cause outcomes.
CONCLUSIONS
Results indicate sizable, and statistically significant, associations between historic redlining practices and present-day diabetes mortality and YLL rates. In addition, the persistence of these associations across the 1990–2014 period highlight a need for targeted action to undo the impact of historical redlining on current health.
Introduction
There are more than 34 million adults in the U.S. with diabetes, approximately 10.2% of the population (1). Diabetes disproportionately impacts racial/ethnic minoritized groups, with non-Hispanic Black adults having a prevalence of 16.4% and Hispanic/Latino adults of 14.7% compared with 11.9% for non-Hispanic White adults (2). Non-Hispanic Black and Hispanic/Latino adults are more likely to have uncontrolled diabetes and to suffer from diabetes-related complications like being hospitalized, having lower-limb amputations, and experiencing retinopathy and are more likely to die as a result of the disease compared with their White counterparts (1,3,4).
There is emerging evidence that structural racism, or the ways in which societies foster discrimination through mutually reinforcing inequitable systems, is a major contributor to poor health outcomes for racial/ethnic minoritized groups (5–8). Structural racism captures upstream historic racist events (such as slavery, black code, and Jim Crow laws) and more recent state-sanctioned racist laws in the form of redlining. Redlining, formalized in 1934 by the Federal Housing Administration (and later prohibited under the Fair Housing Act of 1968), refers to the practice of systematically denying various services to residents of specific neighborhoods/communities, often based on race/ethnicity. Examples included denial of credit access and insurance for borrowers in neighborhoods with worse housing conditions, lower housing prices, and deprived surrounding areas that were inhabited by primarily racial/ethnic minoritized groups (9–11). The term redlining was adopted from the maps created by the Home Owners’ Loan Corporation (HOLC) that included a grading system of A, “best” and characterized as green; B, “still desirable” and marked as blue; C, “declining” and marked as yellow; or D, “hazardous” and marked as red. Neighborhoods made up of primarily racial/ethnic minoritized families were graded as D, hazardous, and marked as red. While redlining was formally prohibited in 1968, the racial segregation created through these practices persist to present time and were compounded by the informal practices that continued after redlining was prohibited through White flight, blockbusting, and more recently gentrification.
Given that redlining represents a more recent legal manifestation of historic racist events/laws, it is an important surrogate for structural racism. Recent research suggest that areas with exposure to residential redlining are to this day disproportionately inhabited by residents who are unduly subject to worse social risk factors (including discrimination, mass incarceration, poverty, residential segregation, substance abuse, housing instability, poor educational attainment, and poor employment opportunities) and that redlining may present an important link between historic structural racism and present-day racial/ethnic inequalities in health outcomes, disability, and, more broadly, human capital (5–7,12). In summary, historic redlining may affect present day health and mortality outcomes both directly and via its impact on social risk factors that present mediating channels between redlining and present day health and mortality outcomes. Given the multiple potential channels linking historic redlining with health and mortality outcomes, it is important to assess whether individuals with high medical and cost burdens are disproportionately negatively affected by these historic structural inequities.
In this study we examine the association of residential redlining with rates of age-standardized mortality and years of life lost (YLL) in the period of 1990–2014 caused by diabetes. We focused on diabetes-specific causes of death because people with diabetes represent an exemplar (high cost and high burden) study population that may be at elevated risk of death from exposure to historic structural racist policies. For the sake of benchmarking associations related to diabetes deaths, we also examined all-cause mortality and YLL outcomes. Our hypothesis was that areas with exposure to worse HOLC grading are associated with higher mortality rate and more YLL, and we also hypothesized that this association will be stronger for diabetes-related outcomes than for all-cause outcomes. Second, we further evaluated the persistence of these associations over the course of these 25 years and examined whether associations persist, with the hypothesis being that associations between historic redlining and present-day mortality and YLL outcomes would diminish with time.
Research Design and Methods
Study Sample
We combined three sets of data to establish this study sample. First, cause-specific YLL and mortality data from King County in the state of WA were used. These data were sourced from the Institute for Health Metrics and Evaluation (13). Second, a digitized copy of the HOLC map for the city of Seattle, which is located within King County, WA, was used. This data was sourced from the Mapping Inequality project (14). Lastly, census tract shapefiles from the U.S. Census Bureau’s 2010 TIGER/Line Shapefiles were used (15). The resulting sample consisted of 109 census tracts, for each of the 25 years of outcomes data (1990–2014).
Study Variables
Outcome Measures
The main outcome measures included rates (per 100,000 population) of age-standardized mortality and YLL. These rates were based on death registration data, across all ages, from the WA state Department of Health Center for Health Statistics and population data from the WA state Office of Financial Management and were constructed by Dwyer-Lindgren et al. (2017) (16) using the method described by Wang et al. (2017) (13,17). In particular, age-standardized YLL rates, for each census tract, were constructed as follows: 1) Multiplication of the age-specific mortality rate by life expectancy at the average age of death in each age-group from the reference life table of the study of Wang et al. (17). 2) These age-specific YLL rates were then age standardized with use of the U.S. 2010 decennial census population as the standard (13,16,17). We examined the data on all-cause deaths and those caused by diabetes, defined on the basis of the cause definitions of the Global Burden of Disease Study 2015 (17). Details on the exact ICD-9 and ICD-10 codes used to define the cause of death to be by diabetes can be found in Supplementary Appendix A.
Exposure Measure
A continuously constructed HOLC score served as the primary exposure measure. We constructed this on the census tract level using the following steps. First, the proportion of a census tract contained within a given HOLC neighborhood was computed. Second, HOLC neighborhood rating was given a numeric classification with A = 1, B = 2, C = 3, and D = 4; these letter grades correspond to historic HOLC grades where A designated the “best” areas, B the “still desirable” areas, C the “definitely declining” areas, and D the “hazardous” or redlined areas. Third, for census tracts that overlap multiple HOLC neighborhoods, a weighted average census tract level redlining score was constructed based on the area overlaps (this weighting allowed for assigning greater relative weight to HOLC neighborhood scores of areas that had greater area overlap with the specific census tract). The resulting HOLC grade score was thus a continuous measure between 1 (best) and 4 (fully redlined).
As a secondary, robustness check measure, we also used a binary HOLC grade measure that takes the value of 0 for neighborhoods rated as either A or B (i.e., those with HOLC grade score between 1.0 and 2.5) and the value of 1 for neighborhoods rated as either C or D (those with HOLC grade score between 2.5 and 4.0).
Statistical Analysis
Spatial autoregressive models were used to investigate the association of historic residential redlining practices with present day age-standardized mortality and YLL rates. The two outcomes (age-standardized mortality rate and YLL rate) were assessed separately (with use of their logarithms), and the two HOLC grading measures (a continuous HOLC score between 1 and 4 and a binary HOLC grade of 0 and 1) were also assessed separately as the primary independent variable. These methods allowed us to account for potential spatial lags within our outcome measure, and within our HOLC score measure, across adjacent census tracts. Our main analyses were stratified across the years of 1990, 2000, 2010, and 2014; estimation was performed with the generalized spatial two-stage least squares estimator; and the total marginal effects were reported (i.e., the sum of direct and indirect effects) (18). Additional analyses consisted of 1) scatterplot fitted lines based on the simple (unadjusted) regression results and 2) reporting of temporal trends of the coefficient of determination (obtained from temporally stratified spatial autoregressive model estimates across each of the years 1990–2014). Stata MP, version 17, was used for all analyses.
Results
Descriptive Characteristics Across HOLC Rating Score and Year
This sample consisted of 109 census tracts, for the years 1990–2014. Of these census tracts, 53 were classified as HOLC grade A or B (on the basis of numeric HOLC grade between 1.0 and 2.5) and the remaining 56 were classified as HOLC grade C or D (numeric HOLC grade between 2.5 and 4.0). Table 1 provides descriptive characteristics (means and SDs) across low and high HOLC rating areas (low = A or B, high = C or D) across the years of 1990, 2000, 2010, and 2014. The descriptive characteristics are provided across mortality rates (per 100,000) and YLL rates (per 100,000) for each of our four mortality causes.
Table 1.
Summary statistics for main outcome variables (per 100,000) by year, HOLC grade grouping, and death cause
| HOLC grades | Diabetes | All cause | ||
|---|---|---|---|---|
| Mortality | YLL | Mortality | YLL | |
| Year 1990 | ||||
| A or B | 16.41 (4.08) | 300.92 (74.61) | 914.34 (113.38) | 16,048.45 (2,330.08) |
| C or D | 26.78 (10.47) | 523.75 (214.45) | 1,141.19 (222.61) | 23,019.26 (6,387.03) |
| Year 2000 | ||||
| A or B | 17.11 (4.4) | 294.78 (76.7) | 751.07 (96.00) | 12,262.23 (1,795.94) |
| C or D | 28.94 (10.27) | 531.95 (199.43) | 935.09 (158.61) | 17,550.35 (4,119.66) |
| Year 2010 | ||||
| A or B | 12.7 (3.56) | 221.51 (63) | 577.43 (79.16) | 9,556.78 (1,521.81) |
| C or D | 20.91 (7.49) | 397.78 (149.98) | 721.5 (142.1) | 13,640.63 (3,258.12) |
| Year 2014 | ||||
| A or B | 12.68 (3.87) | 217.57 (66.79) | 547.17 (75.25) | 9,033.6 (1,467.63) |
| C or D | 21.47 (8.51) | 403.39 (168.13) | 695.53 (148.24) | 13,089.29 (3,329.08) |
Data are means (SD). Two-way t tests indicate that mean differences across A/B and C/D HOLC grade areas are significant at P < 0.001 level across all years and causes. Mean difference tests performed with use of spatial autoregressive models that allow for spatial correlation across the outcomes and HOLC grade score measures also resulted in significant mean differences (P < 0.001 for all). (Details on these estimates can be found in Supplementary Appendix B2.) Total number of observations is 109 census tracts; of these, 53 are contained in the A or B HOLC grade group and 56 in the C or D HOLC grade group.
Table 1 indicates that mortality and YLL rates decreased across both low and high HOLC rating areas for diabetes and all-cause mortality between 1990 and 2014. Disparity gaps persisted across the 25-year period, and two-way t tests of mean differences across low and high HOLC rating areas were significant at P < 0.0001 across all outcomes, years, and causes. We also assessed these mean differences using a spatial autocorrelation model to allow for spatial correlation across both the outcome and HOLC rating measures; this yielded results qualitatively similar to those obtained with a t test (i.e., P < 0.001). Additional estimation result details can be found in Supplementary Appendix B2.
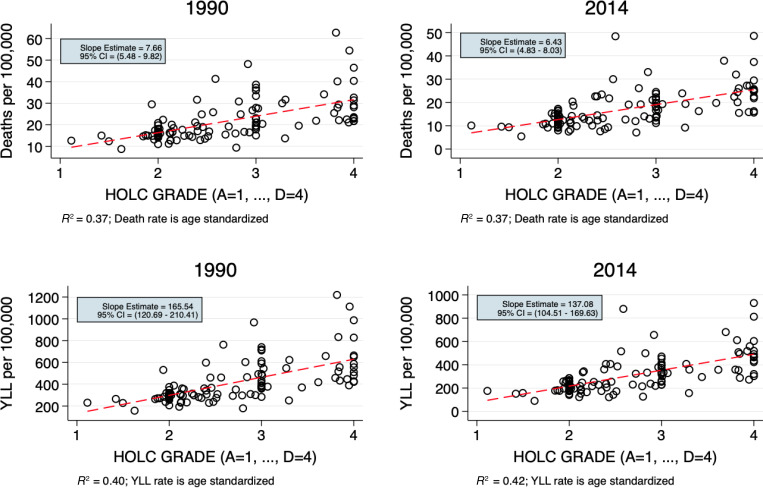
Figure 1 provides information on the relationship between census tract HOLC rating and diabetes mortality and YLL rates for the years of 1990 and 2014. Looking at the linear fitted lines (red dashed lines), we note clear trends, with areas with higher HOLC grades associated with higher mortality and YLL rates. Given the 25-year span between the left column figures and the right column figures (in Fig. 1), it is important to emphasize that these associations persisted across this period. In looking at the YLL plots between 1990 and 2014 the association between YLL and the HOLC grading strengthened over this period of time (the coefficient of variation increased from 0.40 in 1990 to 0.42 in 2014).
Figure 1.
Scatterplots with fitted simple regression lines (red dashed line) indicating the association between HOLC grade scores and diabetes mortality rates and YLL rates across 1990 and 2014. For 1990 deaths per 100,000 R2 = 0.37; death rate is age standardized. For 2014 deaths per 100,000 R2 = 0.37; death rate is age standardized. For 1990 YLL per 100,000 R2 = 0.40; YLL rate is age standardized. For 2014 YLL per 100,000 R2 = 0.42; YLL rate is age standardized.
For further examination of the temporal persistence of these structural disparities, Supplementary Fig. 1 showcases the coefficient of determination trajectories across each of the 25 years of data. Each dot within these figures is obtained from the year-specific (and cause-specific) coefficient of variation from each spatial autoregressive model, which allowed for spatial correlation across the outcomes and the HOLC grade exposure measure. These trajectories indicate great persistence in the noted associations across time, with little to no discernable decay between 1990 and 2014. (Results of pooled regression analyses that further support this conclusion can be found in Supplementary Appendix B3.)
Regression Analyses
Table 2 presents the spatial autoregressive model regression results at the stratified time periods of 1990, 2000, 2010, and 2014. The top section of Table 2 presents results for the continuous HOLC grade score, and the bottom section presents results for the binary HOLC classification. Estimates are provided for diabetes and all-cause mortality rates, and these estimates represent the total marginal change of the mortality rate associated with a unit change in the exposure. Given that the outcomes are measured in logarithms, these results are reported as percentage changes within the main text calculated with the following formula: (exponential(total marginal effect estimate) − 1). Reporting results as percentage changes allows for results to be more interpretable; however, it also means that there are some differences between estimates reported within the main text and those seen within the Tables 2 and 3, as the latter report the raw “total marginal effect estimates.”
Table 2.
Spatial autoregressive model regression results across cause-specific mortality rates for the years 1990, 2000, 2010, and 2014
| Diabetes | All cause | |||||||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2000 | 2010 | 2014 | 1990 | 2000 | 2010 | 2014 | |
| Continuous HOLC exposure | ||||||||
| HOLC grade (score 1–4) | 0.37 (0.29– 0.45)*** | 0.44 (0.37– 0.50)*** | 0.41 (0.35– 0.48)*** | 0.43 (0.36– 0.50)*** | 0.19 (0.13– 0.24)*** | 0.18 (0.14– 0.23)*** | 0.17 (0.12– 0.21)*** | 0.17 (0.12– 0.22)*** |
| No. of observations | 109 | 109 | 109 | 109 | 109 | 109 | 109 | 109 |
| Pseudo R2 | 0.48 | 0.55 | 0.47 | 0.45 | 0.40 | 0.40 | 0.34 | 0.32 |
| Binary HOLC exposure of A/B vs. C/D | ||||||||
| HOLC grade (A/B vs. C/D) | 0.67 (0.56– 0.79)*** | 0.73 (0.62– 0.84)*** | 0.67 (0.56– 0.79)*** | 0.70 (0.57– 0.82)*** | 0.29 (0.22– 0.37)*** | 0.28 (0.21– 0.35)*** | 0.26 (0.19– 0.33)*** | 0.27 (0.19– 0.34)*** |
| No. of observations | 109 | 109 | 109 | 109 | 109 | 109 | 109 | 109 |
| Pseudo R2 | 0.49 | 0.53 | 0.44 | 0.42 | 0.38 | 0.38 | 0.31 | 0.31 |
The outcome measure is age standardized (across all ages) and in logarithms. Robust 95% CIs are reported within the parentheses. Significance is denoted as follows:
P < 0.01.
Table 3.
Spatial autoregressive model regression results across cause-specific YLL rates for the years 1990, 2000, 2010, and 2014
| Diabetes | All cause | |||||||
|---|---|---|---|---|---|---|---|---|
| 1990 | 2000 | 2010 | 2014 | 1990 | 2000 | 2010 | 2014 | |
| Continuous HOLC exposure | ||||||||
| HOLC grade (score 1–4) | 0.44 (0.36– 0.53)*** | 0.50 (0.43– 0.57)*** | 0.49 (0.41– 0.56)*** | 0.51 (0.43– 0.59)*** | 0.30 (0.24– 0.37)*** | 0.30 (0.25– 0.36)*** | 0.29 (0.24– 0.34)*** | 0.30 (0.24– 0.35)*** |
| No. of observations | 109 | 109 | 109 | 109 | 109 | 109 | 109 | 109 |
| Pseudo R2 | 0.53 | 0.59 | 0.53 | 0.51 | 0.54 | 0.58 | 0.52 | 0.51 |
| Binary HOLC exposure of A/B vs. C/D | ||||||||
| HOLC grade (A/B vs. C/D) | 0.75 (0.63– 0.87)*** | 0.81 (0.69– 0.92)*** | 0.78 (0.65– 0.90)*** | 0.81 (0.67– 0.94)*** | 0.48 (0.39– 0.58)*** | 0.47 (0.39– 0.56)*** | 0.45 (0.37– 0.53)*** | 0.46 (0.37– 0.54)*** |
| No. of observations | 109 | 109 | 109 | 109 | 109 | 109 | 109 | 109 |
| Pseudo R2 | 0.53 | 0.55 | 0.50 | 0.48 | 0.49 | 0.52 | 0.47 | 0.45 |
The outcome measure is age standardized (across all ages) and in logarithms. Robust 95% CIs are reported within the parentheses. Significance is denoted as follows:
P < 0.01.
Starting with diabetes mortality rates, within the top section of Table 2, results show that areas with a 1-unit-higher HOLC grade (e.g., those with a D rather than C grade) are associated with a 44.8% (95% CI 33.6–56.8; P < 0.01) higher rate of diabetes mortality in 1990 and a 53.7% (43.3–64.9; P < 0.01) higher rate in 2014. Second, for deaths due to all causes, results show that areas with a 1-unit-higher HOLC grade are associated with a 20.9% (13.9–27.1; P < 0.01) higher mortality rate in 1990 and an 18.5% (12.7–24.6; P < 0.01) higher mortality rate in 2014.
The bottom section of Table 2 shows results based on the binary HOLC grade measure demonstrating that areas with a C or D grade (rather than A or B grade) are associated with a 95.4% (95% CI 75.1–120.3; P < 0.01) higher rate of diabetes mortality in 1990 and a 101.4% (76.8–127.1; P < 0.01) higher rate in 2014. For deaths due to all causes, areas with a 1-unit higher HOLC grade are associated with a 33.6% (24.6–44.8; P < 0.01) higher mortality rate in 1990 and a 31.0% (20.9–40.5; P < 0.01) higher mortality rate in 2014.
Table 3 presents the spatial autoregressive model regression results with YLL used as the outcome measure. The results from these analyses are qualitatively similar. For the top section of Table 3, areas with 1-unit-higher HOLC grades are associated with 55.3%–66.5% higher YLL from diabetes rate (depending on the year), and 33.6%–35.0% higher YLL from all causes rate, again depending on the year. All of these association are, again, significant at a P < 0.01 level.
Conclusions
Results from this study indicate that an area’s HOLC redlining score explains between 45% and 56% of the variation in the census tract–level age-adjusted diabetes mortality rate and between 33% and 47% of the variation in the census tract age-adjusted all-cause mortality rate between the years of 1990 and 2014. These results also show that areas with a 1-unit-higher HOLC grade (e.g., those with a D rather than C grade) are associated with a 44.8% (P < 0.01) higher rate of diabetes mortality in 1990 and a 53.7% (P < 0.01) higher rate in 2014. For deaths due to all causes, areas with a 1-unit-higher HOLC grade were associated with a 20.9% (P < 0.01) higher mortality rate in 1990 and an 18.5% (P < 0.01) higher mortality rate in 2014. These findings indicate great persistence between areas’ historic HOLC gradings and more recent mortality and YLL due to diabetes and all causes. Estimates were found to be qualitatively similar across years and are robust to the use of alternative exposure measure definitions. In addition, these associations indicate consistently higher marginal effects of HOLC redlining exposure on diabetes mortality rates than on all-cause mortality rates. This finding is important to highlight, as it suggests that populations with chronic and elevated medical burdens, and medical cost burdens, such as those with a diagnosis of diabetes, may be at elevated risk of death from exposure to historic structural racist policies.
These results highlight the persistent impact of structural racism on health. Despite the fact that redlining policies were legally prohibited in 1968, the impact on mortality and YLL due to diabetes can be seen in a major metropolitan area of the U.S. across the years of 1990–2014. Additionally, these gaps represent not only statistically significant but also clinically meaningful differences in mortality rates and YLL. These findings contribute to a body of recent work where investigators have sought to use digitized copies of the HOLC maps to document the persistent negative impact from redlining on present-day factors such as residential segregation, economic inequity, and health disparities (19–21), mental health (9), risk of experiencing a preterm birth (22), emergency department visits due to asthma (23), and coronavirus disease 2019 outcomes (24,25). Here, we contribute to the body of evidence with the results of our study of cause-specific mortality and YLL pertaining to diabetes and documentation of a clear persistence of the association between historic redlining and mortality across the 25-year period of our data.
The findings documented here present an urgent call for further research into the linkage between structural racism and health outcomes and for interventions that can help reduce this influence. As seen in the persistence of impact, a lack of policies to intentionally reverse structural racism results in the perpetuation and, possibly, in the widening of disparity gaps across mortality and YLL based on an individual’s area of residence. The prevailing approach to addressing disparity gaps has been focused on improving social conditions, such as affordable food and housing, or increasing access to health care. However, as policies initiated the redlining measured in this study, it is necessary to target policies that are perpetuating the impact of historical practices, which is currently seen in disparities in mortality and morbidity. This study also highlights the important role that our living environment, which may be shaped by historic racist policies such as residential redlining, has on population health and diabetes outcomes.
Study Limitations
For this study we used an observational study design, and as such, results should be interpreted as associations and not as causal effects. Secondly, vital registration records have been noted to understate the contribution of diabetes to mortality (26), and accuracy of characterizing ill-defined death relies on the proficiency of the garbage code redistribution methods used. As such, this study drew on mortality and YLL data from Dwyer-Lindgren et al. (16), who used validated methods (Wang et al. [17]) for the computation of these measures and for the careful redistribution of garbage codes. Third, the fact that census tracts do not perfectly map into historic HOLC redlining maps presents a problem pertaining to how to best compute this metric at a census tract level. To evaluate the sensitivity of our exposure measure we used two (one continuous and one binary) measures within our main analyses. Additional sensitivity checks that only included counties that overlapped with at most one HOLC area were further found to yield qualitatively similar results, suggesting a level of robustness for our measure. (Details on the sensitivity analyses can be found in Supplementary Appendix C). Lastly, these data sources represent the state of WA, and findings may not be generalizable to other states or regions of the U.S. However, given the consistent use of HOLC redlining maps across the U.S., we believe these results represent a first step in understanding the impact of structural racism through redlining on diabetes-specific mortality.
Conclusion
Results indicate sizable, and statistically significant, associations between historic redlining practices and present day diabetes mortality and YLL rates.
In addition, the persistence of these associations across the 1990–2014 period highlights a need for targeted action to undo the impact of historical redlining on current health. These findings highlight a tangible influence of structural racism on health outcomes for adults with diabetes and call for meaningful action to mitigate this impact.
Article Information
Funding. Effort for this study was partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases (K24DK093699, R01DK118038, R01DK120861 [Principal Investigator (PI) L.E.E.], and K01DK131319 [PI J.A.C.]) and the National Institute on Minority Health and Health Disparities (R01MD013826 [PIs R.J.W. and L.E.E.]).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. S.L. and L.E.E. designed the study. S.L. acquired and analyzed data. S.L. drafted the manuscript. R.J.W., J.A.C., and L.E.E. reviewed and revised the manuscript. All authors critically revised the manuscript for intellectual content and approved the final manuscript. S.L. and L.E.E. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.19694947.
This article is featured in a podcast available at diabetesjournals.org/journals/pages/diabetes-core-update-podcasts.
References
- 1. Centers for Disease Control and Prevention . Diabetes. Atlanta, GA, National Center for Health Statistics, 2020 [Google Scholar]
- 2. Centers for Disease Control and Prevention . Prevalence of Both Diagnosed and Undiagnosed Diabetes, 2020. Accessed 12 January 2021. Available from https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html
- 3. Office of Minority Health . Diabetes and African Americans. Rockville, MD, U.S. Department of Health and Human Services, 2019. Accessed 28 November 2021. Available from https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=18
- 4. Office of Minority Health . Diabetes and Hispanic Americans, 2019. Rockville, MD, U.S. Department of Health and Human Services, 2019. Accessed 28 November 2021. Available from https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=63
- 5. Egede LE, Walker RJ. Structural racism, social risk factors, and Covid-19 - a dangerous convergence for Black Americans. N Engl J Med 2020;383:e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bailey ZD, Feldman JM, Bassett MT. How structural racism works - racist policies as a root cause of U.S. racial health inequities. N Engl J Med 2021;384:768–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453–1463 [DOI] [PubMed] [Google Scholar]
- 8. Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015;10:e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richardson J, Meier HCS, Mitchell BC, Edlebi J, Lynch E. The lasting impact of historic “redlining” on neighborhood health: higher prevalence of COVID-19 risk factors, 2020. Accessed 12 January 2021. Available from https://ncrc.org/holc-health
- 10. Rothstein R. The Color of Law: A Forgotten History of How Our Government Segregated America. Liveright Publishing Corporation, New York, 2017 [Google Scholar]
- 11. Lee EK, Donley G, Ciesielski TH, et al. Health outcomes in redlined versus non-redlined neighborhoods: a systematic review and meta-analysis. Soc Sci Med 2022;294:114696. [DOI] [PubMed] [Google Scholar]
- 12. Egede LE, Walker RJ, Campbell JA, Dawson AZ, Davidson T. A new paradigm for addressing health disparities in inner-city environments: adopting a disaster zone approach. J Racial Ethn Health Disparities 2021;8:690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Institute for Health Metrics and Evaluation . United States - King County, Washington life expectancy and cause-Specific mortality by census tract 1990-2014, 2017. Accessed 12 January 2021 Available from https://ghdx.healthdata.org/record/ihme-data/united-states-king-county-washington-census- tract-life-expectancy-cause-specific-mortality- 1989-2014
- 14. Nelson RK, Winling L, Marciano R, Connolly N. Mapping Inequality, 2021. Accessed 10 December 2021. Available from https://dsl.richmond.edu/panorama/redlining/#loc=5/39.1/-94.58
- 15. U.S. Census Bureau . TIGER/Line Shapefiles 2010, 2021. Accessed 21 February 2022. Available from https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.2010.html
- 16. Dwyer-Lindgren L, Stubbs RW, Bertozzi-Villa A, et al. Variation in life expectancy and mortality by cause among neighbourhoods in King County, WA, USA, 1990-2014: a census tract-level analysis for the Global Burden of Disease Study 2015. Lancet Public Health 2017;2:e400–e410 [DOI] [PubMed] [Google Scholar]
- 17. Wang H, Naghavi M, Allen C, et al.; GBD 2015 Mortality and Causes of Death Collaborators . Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459–1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Badinger H, Egger P. Estimation of higher-order spatial autoregressive cross-section models with heteroscedastic disturbances. Pap Reg Sci 2011;90:213–235 [Google Scholar]
- 19. Faber JW. Redlined yesterday and redlined today: the Home Owners Loan Corporation’s long shadow, 2017. Accessed 12 January 2021. Available from https://paa.confex.com/paa/2018/mediafile/ExtendedAbstract/Paper19071/Redlined%20yesterday%20and%20redlined% 20today%20-%20PAA.pdf
- 20. Mitchell B, Franco J. HOLC “redlining” maps: the persistent structure of segregation and economic inequality, 2020. Accessed 12 January 2021. Available from https://ncrc.org/holc/
- 21. Aaronson D, Faber J, Hartley D, Mazumder B, Sharkey P. The long-run effects of the 1930s HOLC “redlining” maps on place-based measures of economic opportunity and socioeconomic success. Reg Sci Urban Econ 2021;86:103622. Accessed 12 January 2021. Available from https://www.sciencedirect.com/science/article/abs/pii/S0166046220303070?via%3Dihub
- 22. Krieger N, Van Wye G, Huynh M, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013-2017. Am J Public Health 2020;110:1046–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nardone A, Chiang J, Corburn J. Historic redlining and urban health today in U.S. cities. Environ Justice 2020;13:109–119 [Google Scholar]
- 24. Bertocchi G, Dimico A. COVID-19, race, and redlining, 2020. Accessed 12 January 2021. Available from https://docs.iza.org/dp13467.pdf
- 25. Choi Y, Unwin J. Racial impact on infections and deaths due to COVID-19 in New York City. 9 July 2020 [preprint]. arXiv:2007.04743 [Google Scholar]
- 26. Stokes A, Preston SH. Deaths attributable to diabetes in the United States: comparison of data sources and estimation approaches. PLoS One 2017;12:e0170219. [DOI] [PMC free article] [PubMed] [Google Scholar]