Abstract
Background/Aims
The Gachon Regional Occupational Cohort Study (GROCS) is a large-scale longitudinal study of occupational safety and health data (covering Work Environment Monitoring, Workers' Health Surveillance, and Occupational Health Service) conducted by the Gachon University Gil Medical Center (GUGMC) in Incheon, Republic of Korea. We conducted GROCS to identify the health effects of workers’ occupational risks, behavior, socioeconomic status, and life style.
Methods
The GROCS includes data from Work Environment Monitoring, Workers’ Health Surveillance, and Occupational Health Service. The baseline year for all data collection was 2018. Work Environment Monitoring was conducted in 240 companies located in Incheon. General Health Examination and Special Health Examination were performed on 32,725 and 9,504 workers, respectively. Occupational Health Services were provided to 16,883 workers in 171 companies. These data have been collected and operated at an external data management institution and were provided as a retrospective cohort after removing personal identification information.
Results
In 2018, the total number of companies was 2,854, among which which 488 special Health Examination, 171 Work Environment Monitoring, and 240 Occupational Health Service. The proportion of companies undergoing Special Health Examination was 17.1%, the proportion of companies undergoing Work Environment Monitoring was 8.4%, and the proportion of Companies undergoing Occupational Health Service was 6.0%.
Conclusion
GROCS expects researchers to utilize its useful and reliable resource for occupational health and surveillance with for academic or political purposes to lead to improved workers’ health and working environment.
Keywords: Korea Occupational Health Service, Occupational safety, Surveillance, Work Environment Monitoring, Workers' Health Examination
1. Introduction
The Republic of Korea has enforced a plan to protect workers from exposure to hazardous materials and conditions since the 1970s [1]. The first step of this plan comprises a health surveillance of workers from large companies; the surveillance aims to detect not only health risks from occupational hazards but also tuberculosis and anemia, which were common during the Korean War [[2], [3], [4]]. Since then, Work Environment Monitoring has been performed nationwide irregularly. Both health surveillance and Work Environment Monitoring were authorized through the Occupational Safety and Health Act in 1982 [1,2,[5], [6], [7], [8]]. Since the enactment of this act, the annual results of these examinations have been published by the Ministry of Employment and Labor.
Subsequently, private occupational health agencies authorized by the Ministry of Employment and Labor have performed health surveillance and Work Environment Monitoring [9]. Annual health surveillance (medical examination) have been provided to all workers, including non-documented foreigners, since the 2000s [2,10,11]. Companies sometimes request more extended health profiles as one of welfare and prescreening lifestyle diseases and cancers other than official items provided by the National Health Insurance. All of the workers' health-related personal information is recorded before undergoing health surveillance. These data are kept as medical records and secured by the Personal Information Protection Act. The Gachon University Gil Medical Center (GUGMC), located in Incheon, is an authorized agency for keeping the records. Incheon is the first industrialized area in Korea, established as a post for the economic development of the 1970s. Residents in the Incheon area have been exposed to various occupational hazards at work or at home ever since. In the late 1980s, the Namdong National Industrial Complex was established in Korea according to the government's industry relocation plan.
The GUGMC provides Occupational Health Services to companies located in the Namdong Industrial Complex, which accommodates metallurgy, plating, electronics, machinery, chemicals, and autoparts factories. Workers in the Namdong Industrial Complex are exposed to metals, solvents, chemicals, fine dust, noise, and other occupational risks. Therefore, severely injured and ill workers have been treated at the GUGMC because it is the largest tertiary hospital, with approximately 1,400 beds and more than 30 medical specialties. Since 2015, all data from health surveillance and work environments can be merged into hospital records because workers who received Occupational Health Services were given the same hospital records. Based on this information, we conducted the Gachon regional occupational cohort study (GROCS) to identify the following health effects of workers' occupational risks, behavior, socioeconomic status, and lifestyle.
Due to its proximity with Seoul (which has several advantages, such as having a seaport and an international airport), Incheon hosts numerous types of companies, including manufacturers of various sizes. The GROCS is a large-scale occupational cohort study of workers from Incheon, and it includes data from Work Environment Monitoring, Workers' Health Surveillance, and Occupational Health Service. This study aims to provide researchers with reliable data on occupational health and medical surveillance for academic and political purposes.
The research topics of this study include the following:
-
(1)
Workplace health promotion,
-
(2)
Prevention of workplace accidents and injuries,
-
(3)
Acute chronic disease or illness in the workplace,
-
(4)
Effects of workers' socioeconomic status and lifestyle on their health, and
-
(5)
Effects of Occupational Health Services and management on workers' health.
2. Materials and methods
2.1. Who is in the cohort and how often were they followed up?
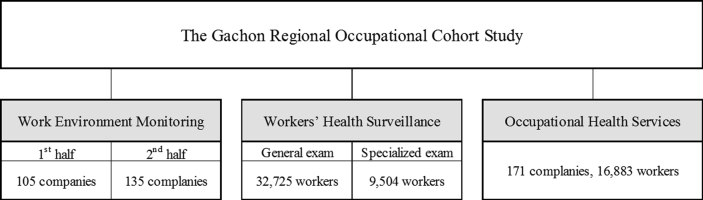
The GROCS includes data from Work Environment Monitoring, Workers' Health Surveillance, and Occupational Health Service. (Fig. 1). Under the legislation of occupational safety and health, companies located in Incheon require that these Occupational Health Services is provided by regional occupational health institutions [10,11]. The GUGMC has offered Occupational Health Service since 2015, while the baseline year for all data collection was 2018. In 2018, Work Environment Monitoring was conducted in 105 companies in the first half of the year and in 135 companies in the second half. General Health Examination and Special Health Examination were performed on 32,725 and 9,504 workers, respectively. Occupational Health Services were provided to 16,883 workers in 171 companies. Fig. 1 shows the number of companies and workers according to each category (Work Environment Monitoring, Workers' Health Examinations, and Occupational Health Service). The follow-up observations were performed either every 6 months or yearly.
Fig. 1.
Flow diagram of baseline recruitment for the Gachon Regional Occupational Cohort Study in 2018.
In Korea, employers are obligated to perform health surveillance (medical examination) on their employees, in accordance with the Occupational Safety and Health Act. There are two major types of Workers' Health Surveillances: General Health Examinations and Special Health Examinations [10]. Workers' General Health Examinations are for all employees subject to the Occupational Safety and Health Act. Office workers undergo a General Health Examination once every two years, while all other workers undergo a general examination annually [11]. In 2019, 8.5 million workers underwent General Health Examinations. Workers' Special Health Examinations, including preplacement health examinations, are for employees who are exposed to hazardous materials and/or conditions, such as chemicals, toxic metals, and noisy environments. As of 2019, there were 178 hazardous factors designated by law, including 161 types of chemicals, seven types of dust, eight physical factors, and two types of night-shift work [11]. In 2019, 2.3 million workers underwent Special Health Examinations.
Work Environment Monitoring, defined as gathering, analysis, and evaluation of samples conducted by an employer or business owner (who formulates a measurement plan for the relevant workers or the workplace) to understand the actual conditions of the working environment, is a mandatory procedure to protect workers' health from hazardous environments and to highlight possible improvements for the working environment. Every six months, employers assess the working environment of the company's premises for anything that may pose a health hazard [11]. The employer must notify their workers and record the measurement results of the workplace. Simultaneously, employees must report the findings of their assessment to the Ministry of Employment and Labor [10]. During assessments of the working environment, personal sampling must be performed to estimate workers' exposure to certain substances during their work duties. In addition, surrogates must be measured to evaluate workers' exposure to the hazadous substances. The most common surrogates are substance concentrations around the breathing zone (substances near the worker's nose and mouth) and noise levels in the hearing zone (near the ear). The measured concentration represents the potential exposure. Additionally, it is possible to perform area sampling depending on the situation.
Occupational Health Service requires the accumulation of long experience, high technology, high-tech facilities, and diverse professional manpower. In small and medium-sized workplaces, it is difficult to expect employers to take charge of health management on their own. It is a system that provides guidance and support for workplace health management by specialized health managers for small and medium-sized workplaces. It aims to protect workers' health and promote health, and for this purpose, it creates a healthy and safe working environment and conditions [[10], [11], [12]].
2.2. Data collection
We collected information on workers' gender, number of workers, number of companies, and the number of Special Health Examinations according to harmful agents at baseline in 2018. The 2019 data reflected changes in the information of the existing companies and workers in 2018, such as updates or additions. Similar distributions of harmful agents (ranging from abnormal air pressure, vibration, hazardous rays, acid–alkali gas, dust, noise, organic compounds, and metals) were observed in 2018 and 2019. The baseline characteristics of Workers' Health Examination data are summarized in Table 1. Each company and worker was assigned a unique number so that the collected data could be linked.
Table 1.
Baseline Characteristics of Workers' Health Surveillance Data
| 2018 (baseline) |
2019 (follow-up) |
|||
|---|---|---|---|---|
| N (%) | N (%) | |||
| Number of workers | 9,504 | 10,809 | ||
| Gender | ||||
| Male | 6,400 | (67.3) | 7,875 | (72.9) |
| Female | 3,104 | (32.7) | 2,934 | (27.1) |
| Number of companies | 488 | 568 | ||
| Harmful agent-specific health examination∗ | ||||
| Noise | 5,190 | (12.5) | 4,607 | (10.0) |
| Abnormal air pressure | 18 | (0.0) | 10 | (0.0) |
| Dust | 2,956 | (7.1) | 3336 | (7.2) |
| Organic compounds | 10,838 | (26.2) | 11,754 | (25.5) |
| Metals | 11,191 | (27.0) | 14,493 | (31.4) |
| Acid–alkali | 2,483 | (6.0) | 2746 | (6.0) |
| Vibration | 16 | (0.0) | 63 | (0.1) |
| Hazardous rays | 2,161 | (5.2) | 2284 | (5.0) |
| Others | 6,579 | (15.9) | 6803 | (14.8) |
Duplicate allowed.
Table 2 summarizes the baseline characteristics of workplace measurement data, including the number of companies, company size, and workplace hazards. Compared to the first half of 2018, the number of companies implementing Work Environment Monitoring gradually increased until the second half of 2019. Regarding company size, enterprises with 5 to 49 employees were the most common, while their distribution was similar in 2018 and 2019. Workplace hazards, including noise, dust, organic compounds, acid–alkali gas, metals, gases, permitted substances, heat, and oil mists, also showed a similar distribution in 2018 and 2019.
Table 2.
Baseline characteristics of Work Environment Monitoring data
| 2018 (baseline) |
2019 (follow-up) |
|||||||
|---|---|---|---|---|---|---|---|---|
| First half N (%) | Second half N (%) | First half N (%) | Second half N (%) | |||||
| Number of companies | 105 | 135 | 141 | 180 | ||||
| Company size∗ | ||||||||
| Less than 5 | 5 | (4.8) | 23 | (17.0) | 24 | (17.0) | 38 | (21.1) |
| 5–49 | 44 | (41.9) | 56 | (41.5) | 59 | (41.9) | 81 | (45.0) |
| 50–99 | 36 | (34.3) | 36 | (26.6) | 35 | (24.8) | 37 | (20.6) |
| 100–299 | 13 | (12.4) | 14 | (10.4) | 14 | (9.9) | 16 | (8.9) |
| 300–999 | 6 | (5.7) | 4 | (3.0) | 8 | (5.7) | 6 | (3.3) |
| 1000 or more | 1 | (0.9) | 2 | (1.5) | 1 | (0.7) | 2 | (1.1) |
| Workplace hazards† | ||||||||
| Noise | 78 | (74.3) | 100 | (74.1) | 98 | (69.5) | 14 | (7.8) |
| Dust | 51 | (48.6) | 63 | (46.7) | 74 | (52.5) | 93 | (51.7) |
| Organic compounds | 61 | (58.1) | 72 | (53.3) | 70 | (49.6) | 81 | (45.0) |
| Acid–alkali | 24 | (22.9) | 25 | (18.5) | 25 | (17.7) | 31 | (17.2) |
| Metals | 67 | (63.8) | 79 | (58.5) | 87 | (61.7) | 96 | (53.3) |
| Gases | 8 | (7.6) | 7 | (5.2) | 9 | (6.4) | 8 | (4.4) |
| Permitted substances | 2 | (1.9) | 1 | (0.7) | 0 | (0.0) | 0 | (0.0) |
| Heat | 3 | (2.9) | 1 | (0.7) | 5 | (3.5) | 2 | (1.1) |
| Oil mists | 29 | (27.6) | 40 | (29.6) | 51 | (36.2) | 44 | (24.4) |
Based on the number of workers.
Number of companies can be duplicated due to multiple workplace hazards.
The baseline data of the Occupational Health Service, including the number of workers, workers' gender, number of companies, and company size, are summarized in Table 3. Companies that received Occupational Health Service and the number of workers were greater in 2018 than in 2019. Regarding company size, enterprises with 5 to 49 employees were the most common in both 2018 and 2019.
Table 3.
Baseline characteristics of the Occupational Health Service data
| 2018 (baseline) |
2019 (follow-up) |
|||
|---|---|---|---|---|
| N (%) | N (%) | |||
| Number of workers | 16,883 | 17,698 | ||
| Gender | ||||
| Male | 11,301 | (66.9) | 12,329 | (69.7) |
| Female | 5,582 | (33.1) | 5,369 | (30.3) |
| Number of companies | 171 | 169 | ||
| Company size∗ | ||||
| Less than 5 | 25 | (14.6) | 33 | (19.5) |
| 5–49 | 92 | (53.8) | 73 | (43.2) |
| 50–99 | 49 | (28.7) | 57 | (33.7) |
| 100–299 | 5 | (2.9) | 6 | (3.6) |
Based on the number of workers.
3. Results
Owing to the difference in measurement objects, each Occupational Health Service has different measures of data. The measures obtained for the GROCS are summarized in Table 4. All Occupational Health Services share company information data. Industrial classification, main products, and enterprise size can be known. In 2018, the total number of companies was 2,854, among which 488 had Special Health Examination, 171 had Work Environment Monitoring and 240 had Occupational Health Service. The total number of companies includes not only those with Special Health Examination, Work Environment Monitoring, and Occupational Health Service but also those with General Health Examination. The proportion of companies undergoing Special Health Examination was 17.1%, the proportion of companies undergoing Work Environment Monitoring was 8.4%, and the proportion of companies undergoing Occupational Health Service was 6.0%. Compared to the total companies, the proportion of Special Health Examination, Work Environment Monitoring, and Occupational Health Service was 31.5%.
Table 4.
Summary of core variables collected in GROCS
| Service category | Data category | Measurements |
|---|---|---|
| Company information data | Characteristics of company | Industrial classification |
| Main products | ||
| Size of enterprise | ||
| Work Environment Monitoring | Occupational hazardous factors | Organic compounds |
| Acid–alkali gas | ||
| Metals | ||
| Gases | ||
| Permitted substances | ||
| Metalworking fluids | ||
| Physical factors | ||
| Dusts | ||
| Workers' Health Surveillance | Medical and social history data | Medical history |
| Family history | ||
| Occupation | ||
| Lifestyle data | ||
| Drinking habit | ||
| Smoking history | ||
| Physical activity | ||
| Anthropometric measures | Height and weight | |
| Waist circumference | ||
| Eye vision test | ||
| Audiometry (1 kHz) | ||
| Blood pressure | ||
| General blood test | Hemoglobin | |
| Liver function test | ||
| BUN/Creatinine | ||
| eGFR | ||
| Lipid profile | ||
| Urine test | Dipstick test | |
| Imaging Study | Chest X-ray | |
| Specialized questionnaire∗ | Self-reported symptom | |
| Self-reported sleep habit | ||
| Specialized test∗ | Electrocardiography | |
| Spirometry | ||
| Complete blood counts | ||
| Specific urine test | ||
| Biological exposure indicator | ||
| Blood peripheral smear | ||
| Audiometry | ||
| Occupational Health Service | Health checkup and consultation | Blood pressure |
| Blood sugar test | ||
| Company management | Safety and health education | |
| Work stress index | ||
| Risk assessments of cardiovascular disease | ||
| Health promotion program | ||
| Work-related injury/disease | Number of injuries/diseases | |
| Disease cause investigation | ||
| Work conformity assessments |
Acquired depending on hazards.
3.1. Workers' Health Surveillance
Workers' Health Surveillance comprised questionnaires, anthropometric measures, and clinical measurements. Medical and social history of occupation data were collected by the questionnaires. Data on lifestyle factors, such as drinking habits and smoking history were also collected. Unlike General Health Examinations, workers who underwent Special Health Examinations were asked additional questions about clinical symptoms and work-related symptoms. For night-shift workers, questionnaires regarding sleep habits were also collected. In particular, workers' socioeconomic status, lifestyle, and work patterns are important information that can affect chronic diseases such as high blood pressure, metabolic syndrome, diabetes, and hyperlipidemia.
The General Health Examination collected anthropometric data, such as height, weight, waist circumference, vision, audiometry (1 kHz), and blood pressure. Workers who underwent General Health Examinations underwent standard clinical measurements. In blood tests, serum hemoglobin, liver function test, BUN/creatinine ratio, and eGFR were measured. Urine dipstick tests were performed to check for proteinuria. Chest X-rays were also taken. The lipid profile was only available once every 4 years [11].
For Special Health Examinations, target organs are determined according to the health effects of specific risk factors. Based on their occupational health risks, workers underwent different kinds of tests, including blood tests, urine tests, pulmonary function tests, chest radiography, dental check-ups, and/or biological monitoring. For example, workers who were exposed to dimethylformamide, which may cause hepatic disorders and irritation of the mucous membrane, underwent blood tests for liver function, health examinations for irritation to the eyes and skin, and urinary N-methylformamide for the biological monitoring. Exposure to hazardous factors in the workplace can cause acute (e.g., acute encephalopathy or peripheral neuropathy by exposure to organic compounds) or chronic disease (e.g., blood cancer by benzene); therefore, Special Health Examinations should be regularly performed. Special Health Examinations were conducted according to a predetermined schedule (from 6 months to 24 months), based on the risks and characteristics of the health effect of each factor [11].
3.2. Work Environment Monitoring
Work Environment Monitoring of hazardous materials for each company is allowed in the GROCS. Under the Occupational Safety and Health Act in Korea, workers' exposure levels of 192 materials must be measured. Therefore, the following elements should be measured if companies use hazardous materials: 114 kinds of organic compounds, 24 kinds of metals, 17 kinds of acid–alkali compounds, 15 kinds of gases, 12 kinds of permitted substances, 1 metalworking fluid, 2 kinds of physical factors, and 7 kinds of dusts [11]. Work Environment Monitoring prevents workplace accidents and injuries (e.g., chemical explosions, asphyxiation disasters in enclosed spaces, etc.) that may result from exposure to physical or chemical hazardous factors and contribute to the improvement of workplace health.
3.3. Occupational Health Service
Occupational Health Service included workplace environment management, health and medical consultation, health education, first aid guidance, and occupational injury or disease management [12]. Workplace environment management was conducted by consulting the results of the Work Environment Monitoring, hazardous environment management, and workplace surveillance. Health and medical consultations assessed the results of Workers' Health Surveillance, chronic disease management, healthy behavioral education, and disease prevention. Occupational injury or disease management included statics of occupational injury or disease and improvement.
4. Discussion
The GROCS is a large-scale longitudinal study of occupational safety and health in Incheon, Korea. Due to its continuous follow-up of workplace environments and workers' health, it can be used to identify the long-term effects of low levels of exposure to hazardous materials. One of the GROCS′ key strengths is that it evaluates Occupational Health Service and workplace management. According to the Occupational Safety and Health Act in Korea, Occupational Health Service and workplace management must be provided, but there is less chance to evaluate them. Since the GROCS contains data from Occupational Health Service, it allows for the evaluation of Occupational Health Service and workplace management.
This study had some limitations. First, each company has the prerogative to choose a specific health institution that can provide Occupational Health Services to the company each quarter or year. Additionally, all workers are also allowed to choose health institutions to undergo Workers' Health Surveillance. If companies or workers choose different institutions, it is possible to lose follow-up studies or have missing data. Second, workplace environments change constantly; hazardous materials used by companies can be replaced by safer ones or workers may no longer be exposed to hazadous materials. In such cases, it may no longer be necessary to conduct Work Environment Monitoring or specialized Workers' Health Examinations, which may lead to a lapse in follow-ups. Third, because this study used large-scale data, some data may be insufficient or missing.
GROCS, a large-scale occupational cohort study of workers in Incheon, expects researchers to utilize its reliable data for academic and political purposes to lead to improved workers' health and working environment.
Ethical considerations
The data used in this study are based on workplace measurements, Workers' Health Surveillance, and Occupational Health Service at GUGMC. However, to avoid ethical issues regarding privacy, these data were collected and operated at an external data management institution. The GROCS data were provided in a retrospective cohort manner after personal identification information was removed from the institution. These derived data were used only for research and analysis and were not stored for any other purpose. In addition, this study was conducted after approval by the Institutional Review Board (IRB) of the GUGMC (IRB No. GFIRB2020-038).
Conflicts of interest
The authors have no conflict of interest to declare.
References
- 1.Park J., Kim Y. The history of occupational health service in Korea. Ind Health. 1998;36:393–401. doi: 10.2486/indhealth.36.393. [DOI] [PubMed] [Google Scholar]
- 2.KIH Association . 1993. Thirty years history of the Korean industrial health association. [Google Scholar]
- 3.Kim S.-T. National disease of South Korea in 1950s∼1970s. Public Health Aff. 2018;2:131–137. [Google Scholar]
- 4.Cho K.S. Tuberculosis control in the Republic of Korea. Epidemiol Health. 2018;40 doi: 10.4178/epih.e2018036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang S.-K., Kim E.A. Occupational diseases in Korea. J Korean Med Sci. 2010;25:S4–S12. doi: 10.3346/jkms.2010.25.S.S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park J., Kim Y. The present and the future of occupational health in Korea. J Occup Health. 1999;41:51–56. [Google Scholar]
- 7.Park J., Kim Y. The history of occupational health in South Korea. Arch Environ Occup Health. 2019;74:50–57. doi: 10.1080/19338244.2018.1541859. [DOI] [PubMed] [Google Scholar]
- 8.Kang S.K., Jee Y.K., Ahn Y.S., Kim H.O., Ha M.N., Kwon H.J., et al. The present status and perspective of nationwide occupational diseases surveillance system. Korean J Occup Environ Med. 2001;13:116–126. [Google Scholar]
- 9.Kim Y., Park J., Moon Y. Special medical examination program reform proposal in Korea. Ind Health. 1999;37:109–115. doi: 10.2486/indhealth.37.109. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Employment and Labor . 2019. Occupational safety and health act. Act No.17326. [Google Scholar]
- 11.Ministry of Employment and Labor . 2021. Enforcement rules of the occupational safety and health act. Ordinance of the Ministry of Employment and Labor No.308. [Google Scholar]
- 12.Enforcement decree of the occupational safety and health act. 2018. Presidential Decree No. 31576. [Google Scholar]