Abstract
The COVID-19 pandemic has wracked even the most modern healthcare systems worldwide and has influenced India’s healthcare sector and vastly affected the government’s and corporate stakeholders’ healthcare reform plans; hence, this chapter is intended to unfold the paradigm shift in India’s primary healthcare industry due to the pandemic in the last one and half years. This chapter described India’s experience with the coronavirus during the first and second waves and tried examining the public health difficulties in the COVID era. It provides a timeline of significant events of the pandemic’s growth in India and worldwide and how India responded to the situations through their economic and healthcare policies. We also go through some of the pandemic’s impacts and India’s recovery approach and strategies for its revival. All possibly available secondary data like Scopus, Web of Science, Medline/PubMed, and Google Scholar search engines, newspapers, government websites, etc., were excavated to meet this purpose; secondary sources were used to analyze the data. This chapter also examined the effect of COVID-19 on healthcare workers in India. This chapter critically examined the primary healthcare’s role during this pandemic and the government’s policies and processes to deal with COVID-19 and any other unforeseen situations which the country may encounter in the future.
Keywords: COVID-19, Primary healthcare, Government policies, Public health, Healthcare workers
1. Introduction
When the very first patient was reported with pneumonia-like symptoms in China, nobody on this earth had the slightest idea of how things would change after this. This, invisible with naked eyes, opponent, has taken the entire world under its shock waves. On January 30, 2020, the World Health Organization classified the global COVID-19 outbreak as an immediate public health emergency for the whole world to be concerned about. On March 11, 2020, it was declared a pandemic. On a worldwide scale, as of May 29, 2021, there have been 169,118,995 confirmed cases and 3,519,175 fatalities (Covid19.who.int, 2021). Since then, every individual present on this earth has been putting all their efforts into staying safe and survive this crisis. The healthcare industry has emerged as a critical player in this war against the novel coronavirus.
The healthcare industry or medical industry is much bigger than usual, one knows. This sector provides all possible products and services to help patients cure, prevention, rehabilitation, or palliative care. There are many subdivisions in the modern healthcare sector. To meet the health requirements of individuals and the whole population, this sector is dependent on interdisciplinary teams of paraprofessionals and trained professionals. This industry holds the key to provide good quality and healthy life to the people in any country. The significant players or participants in this entire process of delivering healthcare to the communities and individuals have been depicted in Fig. 1 as follows.
Fig. 1.

Healthcare industry structure (TechnoFunc, 2021).
Before going ahead on the road of understanding this novel virus and its impact on the healthcare industry and its workers, the history of pandemics has to be understood. This is not the first time that humanity is facing something like this. With the evolution of civilizations, these epidemics and pandemics have always been a part of our lives. Table 1 enlists the top 10 worst hitting pandemics in world history in the recent past.
Table 1.
Most fatal pandemics in the world history.
| Pandemic | Duration | Death toll | Causes |
|---|---|---|---|
| HIV/AIDS pandemic | 2005–12 | 36,000,000 | HIV/AIDS |
| Flu pandemic | 1968 | 1,000,000 | Influenza |
| Asian flu | 1956–58 | 2,000,000 | Influenza |
| Flu pandemic | 1918–20 | 20–50,000,000 | Influenza |
| Sixth cholera pandemic | 1910–11 | More than 800,000 | Cholera |
| Russian flu pandemic | 1889–90 | 1,000,000 | Influenza |
| Third cholera pandemic | 1852–60 | 1,000,000 | Cholera |
| The Black Death | 1346–53 | 75–200,000,000 | Bubonic plague |
| Plague of Justinian | 541–542 AD | 25,000,000 | Bubonic plague |
| Antonine Plague | 165 AD | 5,000,000 | Unknown |
Source: Earth5R, 2021. Covid 19 (Coronavirus) and 10 Worst Pandemics in History. [Online] https://earth5r.org/covid-19-coronavirus-and-other-pandemics/ (Accessed 20 May 2021).
India, too, has its share of such epidemics. Table 2 lists the most recent Indian pandemics/epidemics that have brought humanity to its knees. During the 19th century, India mostly had close encounters with epidemics like Cholera and Plague. The primary reasons behind these infections were caused by poor hygiene factors and practices, poor living conditions, illiteracy, overcrowded slums, heavy rainfall, and floods.
Table 2.
Major epidemics in the 20th century in India.
| Pandemic/epidemic | Duration |
|---|---|
| Nipah outbreak | 2018 |
| Indian swine flu outbreak | 2015 |
| Odisha jaundice epidemic | 2014 |
| H1N1 flu pandemic | 2009 |
| Gujarat jaundice epidemic | 2009 |
| Dengue outbreak | 2006 |
| Chikungunya outbreak | 2006 |
| Meningococcal meningitis epidemic | 2005 |
| SARS epidemic | 2003 |
| Dengue epidemic | 2003 |
| Plague of Northern India | 2002 |
| Surat plague epidemic | 1994 |
| Small pox epidemic | 1974 |
| Polio epidemic | 1970–90 |
| Influenza pandemic | 1918 |
Source: Swetha, G., Eashwar, V., Gopalakrishnan, S., 2019. Epidemics and pandemics in India throughout history: a review article. Indian J. Public Health Res. Devel. 10(8), 1570.
1.1. COVID-19 and the world
Wuhan Municipal Health Commission, Wuhan, Hubei Province, China, reported some patients with symptoms like pneumonia on December 31, 2019. Eventually, a novel coronavirus was identified. Soon, in January 2021, the first corona patient was detected outside China in Thailand. This was just the beginning. In the same month, the United States of America (USA), Nepal, Vietnam, France, Malaysia, Russia, Italy, United Kingdom, India, Philippines, UAE reported their first case of the novel coronavirus. In response to this speedy spread of the virus, many countries closed their borders to foreign tourists. All the flights to China originating from many countries were canceled for an indefinite time duration. In the meanwhile, the number of cases in China was exploding. This novel coronavirus got its name COVID-19 by WHO on February 11, 2020. Most countries adopted emergency lockdown as an immediate measure to control the spread of this disease in their country, including India, in March 2020. In the next 9 months, the world saw the spread of this virus, and the count rose to 82 million, and the death count was more than 1.8 million (News, 2021). The United Kingdom started administrating a thoroughly trialed and tested COVID-19 vaccine on its people and became the first nation in the world to do so on December 8, 2020 (Kantis et al., 2021) (Graph 1 ).
Graph 1.

Statistical reference to the total number of cases of coronavirus in the most affected countries in the world.
(Source: Worldometers.info, 2021. COVID Live Update: 171,010,903 Cases and 3,556,329 Deaths From the Coronavirus – Worldometer. [Online] https://www.worldometers.info/coronavirus/#countries (Accessed 19 May 2021).)
Mahajan and Kaushal (2020) mentioned in their article that as of March 11, 2020, COVID-19 had spread to 114 countries, with 118,326 active cases and 4292 deaths, and was declared a pandemic by the World Health Organization (WHO). This viral outbreak had an impact on India as well. The situation worsened within a week of the pandemic’s announcement. After China, Italy had become the second most affected country. While the virus spread like wildfire, scientists put in all their efforts, and they started understanding more about it. In this process, using a mask, social distancing, and washing hands were discovered as the essential means of reducing the chances of getting infected with this virus. The governments declared emergencies and immediately completed lockdown to break the chain of infection. This did help in controlling the spread of this disease even though it affected the world economy very adversely. Once the spread of infection got under control and the countries decided to lift the restrictions and let the economy open to revival, this virus came back with much more threatening effects. This is usually called the second wave of COVID-19. Since last year, sooner or later, almost all the countries on the world map have been or are presently facing this second wave of coronavirus. Countries like Kyrgyzstan, Australia, South Korea, Israel, New Zealand, United States, Southeast Asia, India, Nepal, Laos, Thailand, United Kingdom, Germany, Japan, and Spain have either suffered or are suffering or are on the verge of suffering the second wave of coronavirus (WION, 2021; Standard, 2021).
The second wave of coronavirus marked its re-entry in India in mid-March 2021, almost a year after it appeared for the first time here. Moreover, this time, it has been much faster in infecting people. This time, new mutations have been observed in the virus by scientists. India’s top virologists had confirmed that when in September 2020, the UK-variant was first found in India, it should have been considered an alarm for India (Priyamvatha, 2021). Because of these mutants of coronavirus, India has registered 2,720,716 active cases and 303,720 deaths, as reported by the Ministry of Health and Family Welfare on May 24, 2021 (MoHFW, 2021a, MoHFW, 2021b). This rising number of infected individuals has been putting extreme pressure on the Indian healthcare system. The demand and supply equation of major medical facilities like hospital beds, emergency medicines, oxygen supplies, ICU beds, ventilators, etc., is in jeopardy. All this has further led to add to the severity of the situation and worsen the whole scenario. India began its vaccination phase in January 2021 (Correspondent, S, 2021). Vaccination has been considered a solid intervention to take control of this crippling situation. However, the shortage of vaccination supplies has further just added to the trouble. Getting the entire Indian population vaccinated anywhere nearby to stop this pandemic seems a mammoth task for the Indian Government. Some of the significant trends of this second wave that has been a point of concern for India (Varma, 2021) are as follows:
-
(a)
As per the Union Health Ministry, what was initially confined to 3–5 states in India has spread to 10 states. Furthermore, these 10 states of India account for 73% of the new cases registered (The Economic Times, 2021). Andhra Pradesh, Delhi, Haryana, Uttar Pradesh, Tamil Nadu, Karnataka, Kerala, West Bengal, Rajasthan, and Maharashtra flag bearers.
-
(b)
Indian railway enjoys the reputation of employing one of the most significant numbers of employees in the world. During the pandemic, it has continued serving as an essential service. Indian railway has played an important role and the transportation of essentials of COVID-19 like drugs, equipment, and oxygen. However, all this has put the Indian railway employees in a vulnerable situation. As per the senior officials of Indian railways, 1000 employees are getting infected daily (Press Trust of India, 2021).
-
(c)
To control the second wave COVID-19 situation, many Indian states and union territories have announced night curfews with Section 144, stringent restrictions on weekends, or partial lockdown. This restriction poses extreme challenges for the lower-income and daily wage workers whose livelihood is in great danger.
-
(d)
Unlike the first wave of COVID-19, rural India reports a 1.39 times higher number of cases than urban India (Jha, 2021). This is a great matter of concern for the governing bodies. This is being considered as an upcoming terror. When urban India faces such a hike in the COVID-19 massacre despite the availability of good healthcare facilities, the upcoming picture of rural India seems unimaginable. There are limitations of these facilities in the rural parts of India.
-
(e)
Trouble for India does not seem to be ending here. A new health problem called Mucormycosis, the Black fungus has emerged as an epidemic (Ray, 2021). This disease is being associated with coronavirus. Various clinical reasons are being discussed behind the cause of this trouble.
-
(f)
Recently, IIT Kanpur, in their study, the third wave of COVID-19 has been predicted. No time frame has been disclosed as such, but it is being said that this third wave would probably put the children and newborns in a threatening position.
This COVID-19 pandemic has brought a revolutionary shift in the healthcare industry. In India, the change in the pre- and postscenario is remarkable. Because of this, pandemic is visible through the overall outlook of the country’s seriousness and investment toward human health. In the financial year of 2017, the healthcare industry of India was approximately 160 billion USD. Moreover, it was worth over 140 billion US dollars as of 2016. This has been estimated to go up to 370 billion USD by 4 (Bajaj, 2021). The public health expenditure value for the financial year 2018 for India was recorded at approximately ₹1.58 trillion (Statista Research Department, 2021). This accounted for 1.28% of the GDP of India. The per capita health expenditure in India was calculated around ₹1600. However, there was not an equal distribution of this amount in all the parts of India. The Indian Government introduced the “Ayushman Bharat National Health Protection Mission” in August 2018 (National Portal of India, n.d.). This plan covers secondary and tertiary care hospitalization for a family of five for $5000 per year (on a family floater basis).
Other schemes like “Mission Indradhanush” aimed at achieving 90% immunization in India (Rastogi, 2019).
Business in the healthcare sector is considered giants of the industry had taken over several established multispecialty healthcare groups and hospitals. This sector has appeared attractive for inviting FDI and huge investments from other countries (ETHealthWorld, 2021).
The tide of digitalization has pushed telemedicine in the Indian healthcare industry. This technology is viewed as a beautiful opportunity to reach out to the most unreachable in the country. Various leading industries of India have also started pouring in liquidity in the upcoming field of telemedicine. The Indian Government had also been too active to make the best of these opportunities. As a result, according to the NITI Aayog report (2018), the Indian Government plans to increase public healthcare spending from 1.1% to 2.5% of GDP over the next 4 years. This was further planned to go up to 5% in 5 years (Mishra, 2019).
The trend of single-specialty hospitals and specialty clinics has been like hot selling cake in India. This trend has helped in penetrating the untapped market. There has been a new success mantra called the “Bouquet hospital” model.
All this has made humankind put on their thinking hats. All the nations are all set with their arms and ammunition to counter any war conditions. Still, nobody was ready to handle a world crisis where the opponent is so minute that it is not even visible by the naked eyes. This was something nobody was prepared to take. As soon as COVID-19 struck the world, it compelled all the countries to introspect themselves rather than pointing fingers at others. This pandemic has highlighted the weak links of all the countries, whether developed or developing nations. For example, it has been too complicated for countries like the United States and United Kingdom to control the mortality rate in 2020. Similarly, the situation is getting horrible in India in 2021.
COVID-19 has brought the healthcare industry into the limelight in India because earlier, this was not enjoying much attention by the nation. On one end, India’s healthcare industry has done a commendable job of treating and curing COVID-19 patients, which is a humongous task because of the population. However, on the other end, it has to face many hardships similar to many other sectors. The most critical pillars in combating the COVID-19 pandemic are frontline healthcare staff. Also, the best logistics would be insufficient if our frontline staff are not safe and well supported. Given the magnitude of the epidemic, it is critical to protect the health of these individuals as a public health measure. To this end, determining the prevalence of psychological manifestations in healthcare personnel is vital. Evidence-based assessments and mental health interventions for this group, on the other hand, are rare globally and nearly nonexistent in India. There are some data from India on mental health manifestations among frontline healthcare providers (Chew et al., 2020).
The virus causes debility, morbidity, and death, but it also causes massive physical and psychological fatigue to a large degree. As a result of this breakdown, health departments and ministries are contacting retired medical personnel and others who spend more time researching to encourage them to return to clinical practice to alleviate the mounting stresses on the health system. Indeed, many healthcare workers accept that a vaccine is necessary to stop the virus’s spread, particularly in light of recent mutations that are thought to make it more contagious.
In the pre-COVID-19 era, India was planning to stretch its expenditure on public healthcare, but during the COVID-19, India has spent much higher than what it would have ever targeted. Because of this pandemic, other health-related issues of India, like the crisis of malnutrition, infant healthcare, etc., have been amplified. The 15th Finance Commission has raised a projection of ₹5.38 lakh crores for the Ministry of Health between 2020 and 2025 for primary healthcare and conducting immunization, testing, screening, and treating COVID-19. This amount would grow much higher when the non-COVID-19 conditions are accounted for (Kurian, 2021).
To achieve Universal Health Coverage, India needs to improve its healthcare services from the bottom to rural India. This COVID-19 pandemic exposed the structural weaknesses of the Indian healthcare industry right from inadequate equipment, supplies, medicines, insufficient and overloaded healthcare workers, unethical practices, black marketing of lifesaving drugs, ambiguity in immunization drive, etc. Proper and accurate government intervention would only be able to ensure an improvement in these areas. The Indian Government has already started attending to these issues one by one.
The Indian pharmaceutical industry is the largest provider of generic medicines in the world. It stands at third rank in the world by volume and 14th place by pharmaceutical production value. It accounts for 20% of the medical supplies (India Brand Equity Foundation, 2021). By 2030, this industry is expected to go up to $130 billion. India successfully developed its COVID-19 vaccination called Covaxin by the pharmaceutical company named Bharat Biotech. Post-COVID-19, India can be more focused on getting health insurance, as this has gained momentum. The proof is the growth of 17.16% Y-O-Y to ₹51,637.84 crores (US$ 7.39 billion) in the gross direct premium income that was underwritten in FY20 (India Brand Equity Foundation, 2021).
1.2. India’s measures to fight COVID-19
-
•
Steps for precaution: To control the viral infection spread, the Indian Government has strict screenings and compulsory quarantine rules for all incoming travelers from international destinations. It has also canceled all the international flights. Even traveling within the country has been restricted and under strict scrutiny. Along with all this, the Indian Government made all possible arrangements for the emergency evacuation of its expatriates from various parts of the world. Further, restrictions like complete lockdown have been implemented. Under this rule, other than few essential services, all the rest of the movements were suspended. Special passes and permissions are issued for special urgent situations.
-
•
Steps related to medical facilities: The government has designated 1264 government laboratories and 1326 private laboratory centers to diagnose COVID-19 (Indian Council for Medical Research, 2021). The government is putting in many efforts to meet the rising demand for beds, ICU beds, ventilators, oxygen, etc. Meanwhile, the government is all dedicated to the mission vaccination for India. Covaxin is all developed and made in India vaccination. From no production to the second-largest manufacturer of PPE kits, the Indian Government is putting all efforts into fighting back coronavirus.
-
•Steps related to financial assistance: Looking at the turbulent times, the Indian Government has already announced various relief packages, funds, and plans for low-income groups, daily wage earners, laborers, farmers, hawkers, etc. They are also being supported by direct benefits transferred from the government. Various healthcare-related insurance schemes have been announced. Moreover, many more relief plans and support functions are being rendered by the Indian Government. The investment in public healthcare has been expanded in the Union Budget 2021 to 137% YoY. This brings the total healthcare allocation for the financial year 4 to ₹223,846 crores (US$ 30.70 billion). The Government of India announced ₹64,180 crores (US$ 8.80 billion) for strengthening the National Health Mission in the union budget 2021–22 (The Hindu, 2021). This amount would be used to develop primary, secondary, and tertiary care. The healthcare institutions and infrastructure are aimed to be improved and upgraded to international standards and capacities to detect and cure new & emerging diseases. Other initiatives take in India to strengthen the healthcare industry during recent times:
-
–More than 5.84 crores doses of COVID-19 vaccines have been exported to 70 countries, including Morocco, South Africa, Brazil (Mukherjee, 2021).
-
–The National Backward Classes Finance and Development Corporation (NBCFDC) and Apollo Medskills Pvt. Ltd. have signed a Memorandum of Understanding Ltd. will co-fund COVID-19 vaccination administration training workshops for NBCFDC target community nurses, medical & nursing students, and pharmacists (Press Information Bureau, 2021).
-
–The procurement of Varian Medical Systems, Inc. by Siemens Healthineers Holding I Gmb (SHS GmbH) has been agreed upon by the Competition Commission of India (CCI) (Orissadiary.com, 2021).
-
–Under the vaccination drive of India, on May 27, 2021, as per the Ministry of Health and Welfare dashboard, 20,26,95,874 Indian citizens have been vaccinated successfully (MoHFW, 2021a, MoHFW, 2021b).
-
–Under the scheme of Pradhan Mantri Garib Kalyan Yojana, the Union Minister of Finance & Corporate Affairs Nirmala Sitharaman, under Pradhan Mantri Garib Kalyan Yojana, announced Rs 1.70 lakh crore relief package for people with poverty to combating coronavirus (Pib.gov.in, 2021).
-
–In Pradhan Mantri Kisan Samman Nidhi (PMKSN) that the Indian Government entirely funds, all farmer households receive annual income support of Rs. 6000/- in three equal installments of Rs. 2000/- every 4 months under the scheme.
-
–Since lockdown was imposed, the MNREGA, an essential aspect of the Central Government’s response to the COVID-19 issue, has been seen with cautious optimism. MNREGA provides a rural home with 100 days of pay employment per year if all adult members are prepared to conduct unskilled manual labor at the minimum wage (Megsres.nic.in, 2021).
-
–
India has taken the initial steps to cross-learning between various states and administrated the best practices in the healthcare industry. A lot is still to be done. This COVID-19 pandemic has brought an economic crisis in the country, which would, in turn, push millions of people below the poverty line. To ensure the health and well-being of this new and larger group of the poor, all local governments, state governments, the Central Government, and citizens must work together.
During this time, India’s broad coverage of over 25,000 primary healthcare centers (PHCs), which are the first and lowest health tiers and delivers critical preventative, and remedial health services such as vaccinations and immunizations, has proven to be a lifesaver. Essential medications, maternity and child health, and health education are difficult to manage in rural, suburban, and underprivileged areas.
Be it in rural or urban areas, the entire system is linked to primary healthcare centers. As a result, PHCs’ ability to provide safe, patient-centered care to meet the population’s current health demands, as well as strengthening and including PHCs in this pandemic response, could play a critical role in breaking the virus’s chain of transmission through early detection, service variations, management of mild-to-moderate types of cases at the periphery and could help in assisting the vast population. This could prove to be a cost-effective technique of reducing the number of lives lost and suffering in the short and long term.
1.3. India fights COVID-19 with computer science and software engineering
Like the many other countries around the world, India, too, has turned all the stones to fight against the unknown enemy called the novel coronavirus. Computer science and software engineering has been some of the most effective weapons in this war. Indian Government, both at the central and state level, nonprofit organizations, private players, hospitals, etc., have taken help from IT and ITES companies to develop various software and smartphone-based applications (World, 2020).
Some of the major software and apps developed in India during COVID-19 to manage and control the pandemic and help people handle their health are as follows:
-
(a)
Aarogya Setu: This is the primary contact tracing application widely used by India. The National Informatics Centre under the Ministry of Electronics & Information Technology has developed this smartphone-based application. This application keeps track of contact with other people who are using the app. This app uses the phone’s GPS capabilities and Bluetooth features and alerts users to contact a COVID-19 positive person (The Hindu, 2020).
-
(b)
COVID-19 Feedback: The Indian Ministry of Electronics and Information Technology has developed this survey as a tool by gathering information from the users regarding their recent COVID-19 tests/treatments (Budd et al., 2020). This app has proved to be very helpful to the government to identify the coronavirus effect in various areas and improve the medical facilities in those areas.
-
(c)
MyGov: This is a Government of India app that is a platform for the engagement of Indians where they share their opinions, creative ideas, comments, and suggestions directly to the Government of India.
-
(d)
SAHYOG: This app compliments Aarogya Setu in the process of contact tracing and creating public awareness and deliveries of essential items to the needy (Dst.gov.in, 2021).
-
(e)
Lyfas COVID score: Developed by Acculi Labs of Bangalore, an application-based score shows one’s propensity to COVID-19 infection. This plays a significant role in the early detection of disease and the assessment of the infection. Lyfas is a “proper medical screening test” that depends on test results (Sahay, 2020).
-
(f)
COVID Severity Score: Recently, the software has been developed which uses an algorithm to calculate a COVID Severity Score, eventually identifying the COVID-19 patients who require ventilation. The Foundation has developed this software for Innovation in Health, Kolkata, with biotechnology and IIT Guwahati (Ghosh, 2021a, Ghosh, 2021b).
-
(g)
The Central Bed Allotment system software: This software has been developed to manage the shortage of hospital beds for COVID-19 patients in Karnataka by the Bruhat Bengaluru Mahanagara Palike, the Bangaluru’s civic body (Poovanna, 2020).
-
(h)
The Delhi Corona app: This mobile phone-based application helps update people about vacant hospital beds for COVID-19 patients in Delhi (Chaturvedi, 2020).
-
(i)
NCDIR e-Mortality Software (NCDIR e-Mor): To meet the requirement of reporting COVID-19 deaths more appropriately, the National Centre for Disease Informatics and Research under the Indian Council of Medical Research has developed this software (Kaul, 2020).
-
(j)
The Vee + Svasa mobile app: With the support from Johns Hopkins University, United States, software developers have developed a smartphone-based mobile app, which guides COVID-19 patients isolating at home. This app provides vital information on reaching out to local medical facilities and various informative and educational videos (IANS, 2021).
-
(k)
CoWIN: COVID Vaccine Intelligence Network (CoWIN) system has emerged as the backbone of the biggest vaccination drive in this world against coronavirus. This system benefits everyone involved in the process, including government employees in India. It is a cloud-based IT solution for planning, administering, monitoring, and assessing COVID-19 vaccination (Ghosh, 2021a, Ghosh, 2021b).
2. Methodology
The approach for performing a review and synthesis of the literature addresses the contentious and complex research question to address how there has been a remarkable change in India’s healthcare industry due to the pandemic in the last one and a half years and the role of primary healthcare. There are several methods for performing a literature review of research studies and reports; however, a desk research methodology was chosen as the best tool for interpreting and critiquing existential studies on the role of primary healthcare during the pandemic. In this research, various literature published between 2020 and 2021 were reviewed. The period selected is justifiable since there is an onset of coronavirus during specific in addition. The body of literature for review depends on relevant studies that address the subject of interest. All possibly available secondary data from reputed databases like Scopus, WOS, and Google Scholar search engines, newspapers, government websites, etc., have been being excavated to meet this purpose; secondary sources have been used to analyze the data (Prisma Diagram below). This chapter also examines how COVID-19 has impacted Indian health workers. This chapter aims to critically explore the role of PHC’s and the government’s policies and processes to deal with COVID-19 and any other unforeseen situations that the country may encounter in the future.
The Prisma diagram of systematic review is mentioned below

3. Journey of PHC from conceptualization to the reality
In the Indian context, the concept of primary healthcare (PHC) is not new. Its evolution dates to 1946; the Bhore Committee proposed a primary healthcare center (PHC). As per this committee, PHC would be responsible for combining preventive and curative healthcare as the most basic health unit in rural India. The first few primary healthcare centers (PHCs) in India were set up under the Community Development (Ranga Rao, 1993) Program in 1952. This set the base to create a three-tier healthcare system (M/o Statistics & Programme Implementation, GOI – MOSPI, 2016). For the first four decades, successive government bodies continued to build the network of PHCs, with one to three PHCs being constructed per decade, with the help of various committees (Table 3 ).
Table 3.
Timeline of evolution of Primary Health Centre in India.
| Timeline | Recommendations |
|---|---|
| 1946—Bhore Committee | All administrative levels’ preventative and curative services will be integrated, and the Primary Health Centre is developed in two stages: short term and long term |
| 1952—Mudaliar Committee | Strengthen of PHC before opening new ones, and All India Health service should replace Indian Medical service |
| 1967—Jungalwalla | Integration of health organizations at all levels in the country by taking few steps like special pay for particular work, equal pay for equal work, common seniority, improvement in service conditions |
| 1973—Kartar Singh Committee | A single cadre of versatile workers should be formed by combining many groupings of peripheral workers. A single Primary Health Centre must serve a 50,000-people community PHC established three cadres of health workers between community-level workers and doctors, notably multipurpose health workers and health assistants |
| 1975—Shrivastava Committee | For planning, a “Referral Services Complex” and a Medical and Health Education Commission were established |
| 1977—Rural Health Scheme | It was constructed on the principles of “placing people’s health in people’s hands” |
| 1977—Village Health Guide Scheme | Village Health Guides (VHGs) assist rural communities with preventative, promotive, and primary curative care |
| 1978—Alma-Ata Conference (PHC) | As a result of the declaration, primary healthcare (PHC) became the official health policy of all member countries |
Governments worldwide were looking to improve their healthcare systems’ efficiency, efficacy, and responsiveness. The importance of primary healthcare in accomplishing these goals cannot be overstated. India’s National Health Policy (NHP) 2017 advocated for boosting primary healthcare systems and allocating two-thirds or more of government health spending to primary care, and increasing the overall government health budget to 2.5% of GDP by 2025, up from 1.18% in 2015–16 (Ministry of Health and Welfare, Government of India, 2017). According to the Government’s Rural Health Statistics Report (2018–10), the government has continually endeavored, as shown in the Table 4 .
Table 4.
Number of PHC, CHC, and subcenter in India.
| The average number of villages covered in a rural area | 2005 (Rural) | 2019 (Urban + rural) | Increase in the number | |
|---|---|---|---|---|
| Subcenter | 4 | 146,026 | 160,713 (3302 + 157,411) | 11,385 |
| Primary Health Centre (PHC) | 26 | 23,236 | 30,045 (5190 + 24,855) | 1619 |
| Community Health Centre (CHC) | 120 | 3346 | 5685 (350 + 5335) | 1989 |
Source: Government of India Ministry of Health and Family Welfare Statistics Division, 2019. Rural Health Statistics. Government of India.
3.1. Challenges faced by PHC during COVID-19
Rural India has a strong subcenter, Primary Health Centre (PHC), and Community Health Center (CHC). While a robust plan was being made to strengthen the PHC, that’s when the pandemic has hit hard and also impacted the primary healthcare survival in emerging economies, and so in India too; currently, there is a vast population of rural India which are deprived of primary healthcare due to shortfall of these centers, the number is quite alarming like 18% shortfall at the subcenter level, 22% at the primary healthcare center, and 30% at the community level. Though India has been trying hard to increase the number of facilities, the workers working in this area of healthcare have been substantially low as recommended by WHO. Looking at the statistics, rural India has only 3.2 government hospitals bed per 10,000. First, India imposed a lockdown on March 23, 2020, which shut down all public transportation. Then, as things began to recover, India was hit by a second wave of the virus, making healthcare services even more inaccessible.
Medical personnel, particularly doctors and nurses, were diverted to take COVID-19 patients. At the same time, many frontline workers and social activists were involved in contact tracing, which caused absenteeism of community deployment of women healthcare workers and caregivers to continue the immunization program (Ministry of Health & Family Welfare, 2021).
Social distancing norms suggested by WHO further put a question mark on the feasibility of separating waiting rooms for immunization, and curative services became a challenge.
One of the other challenges faced was that the primary healthcare workers were at an increased risk of contracting the virus while handling the patient and had to go into isolation when they felt they had been exposed to this virus.
The acute shortage of PPE kits in the first wave was severe (Kumar, 2020), because of which the production of PPE kits all over the world was increased to tackle the second wave, which hit hard in India. PHC requires support and boost to strengthen themselves at many ends. This pandemic has necessitated us to do much restructuring so that they are well prepared to handle this pandemic and its variations of the second and third wave, small measures like separate space to treat COVID-19 patients while ensuring social distancing and proper usage of the mask. Despite various initiatives by the government, like the National Health Mission, adequate and reasonable healthcare is still an illusion. Rural Indians face an acute shortage of medical representatives which will have a long-lasting negative impact on the healthcare system in rural India, especially regarding the quality of care available to them. Many states were not prepared to handle COVID-19 and their transmission due to the issues mentioned above (Rekha, 2020). The rural Indian health system is divided into three tiers: primary, secondary, and tertiary care. The subcenter is the primary point of contact between the primary healthcare system and the community (Rai et al., 2021). In rural India, a substantial network of subcenters, Primary Health Centres (PHCs), and Community Health Centers were built (CHC). Due to preexisting vulnerability caused by a lack of health infrastructure in rural areas and a diversion of essential medical resources for providing care, many secondary and tertiary care clinics in low and lower-middle-income countries face significant challenges in managing the COVID-19 pandemic. Several secondary and tertiary care clinics that previously handled outpatient cases have been repurposed to provide medical care and supervision for COVID-19 clients (Garg et al., 2020).
3.2. Role of PHC to mitigate the crisis
PHC in India has a complex structure of government services and private sectors pharmacies and small clinics. In contrast, this system has always been backfired with criticisms for leading to fragmentation and poor quality of care due to dependence on each other. At this moment of the pandemic, the variety of primary care offered cannot be overlooked. They can play a good role in mitigating this crisis in several ways.
-
•
Testing centers: Using the PHC, pharmacies, and health and wellness centers as testing locations. This will help make the testing quicker, reduce the waiting time, and reduce the patient volume at the critical health centers.
-
•
Telehealth: The transition from hospital-based services to telemedicine and virtual treatment and increased demand for portable point-of-care solutions are two of the most critical impacts on the healthcare industry. Demand for digital health and drive-through clinics has also increased. Although there is no denying the importance of human contact in emergency treatment and that it cannot be entirely replaced by technology, long term, a strategic transition toward automation and digital transformation is on the horizon. In the short term, this involves tasks including contact tracing and AI-based solutions for detecting early infections and controlling and suppressing the spread. As a result of the crisis, major healthcare companies collaborate on open-source ventilator prototypes, vaccine testing, drug development, and essential equipment manufacturing. It is inspiring to see first-of-their-kind humanitarian collaborations that go beyond and beyond the call of duty (Sachan, 2021).
In India, the telemedicine market has enormous potential in the eHealth segment. According to a recent Inc42 Plus report titled India’s eHealth Market Opportunity Report, 2021, it is expected to expand at a 31% compound annual growth rate to $5.4 billion by 2025 (CAGR) 2021 (Dayalani et al., 2021).
The Indian Government has already released telemedicine practice guidelines, but adoption has been restricted or reserved for more extensive facilities. Telehealth can be used by primary care providers for remote triaging, ensuring critical health services, and monitoring tools to find possible COVID-19 hotspots (Graph 2 ).
-
•
Safe care: Improving facility operations necessitates new ideas, such as deciding the order of treatment of the incoming patients before arriving at a clinic and providing staff with adequate personal protective equipment (PPE). Guidelines for proper PPE use and establishing a safe environment for infection protection and control are available from India’s Ministry of Health and Family Welfare. At the PHC stage, supply chain shortages for PPE can be partially resolved by encouraging at-home treatment and telehealth when necessary.
-
•
Deployment of community health workers (CHWs): CHWs can provide community-based care and address COVID-19 infection in hard-to-reach and remote areas when adequately resourced and compensated. Other countries’ CHWs have been able to provide uninterrupted treatment through the pandemic’s most challenging moments. The present crisis is a brilliant opportunity to increase the capacity of Accredited Social Health Activists (ASHAs) to provide preventative and effective curative care during the pandemic and beyond by educating and equipping them with appropriate PPE and payment (Abdel-All et al., 2019). To quickly build up the expertise and skills of physicians, nurses, and other health professionals, a mix of various approaches—written protocols, web sessions, on-the-job training and support, and telephonic one-on-one conversations—works well. This awareness is essential for them to feel empowered and confident when they deal with the situation. A balanced combination of accountability and power has to be introduced and executed at the grass-root level. A regular audit and the community’s feedback would help ensure transparency in the entire flow of action.
-
•
Home care: We may prevent unnecessary visits to health facilities by arming patients and their families with more knowledge of maintaining their home health. Enabling self-management at home would be beneficial both in terms of infection prevention and in terms of operations. Especially in light of how overburdened healthcare facilities are at the moment. This online platform, for example, can be used to provide COVID-19 risk information to a patient and is available in various languages. These widely disseminated infographics can aid patients in determining when hospitalization is required versus when at-home treatment is appropriate.
-
•
Clear Health Messages: A clear and compelling risk communication stream must be established to avoid mixed signals at the local and national levels. Consistent messaging through private and public primary care clinics can help reach a large audience across several contact points with the health system. ASHAs may rely on links with local communities in more remote areas to provide consistent information (Saprii et al., 2015).
-
•
Safe community practices: Most rural inhabitants live far from tertiary hospitals, and the same strategy used in large hospitals is likely to be unsuccessful in the long run. The relevance of individual and group behavior in pandemic control becomes vital in these circumstances. Putting boundaries in place would not be enough to encourage good behavior.
Graph 2.
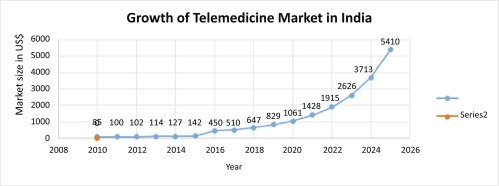
Telemedicine market in India.
(Source: Dayalani, V., Dayalani, V., Staff, I., 2021. Telemedicine: A Post-COVID Reality in India. [Online] Inc42 Media. Available from: https://inc42.com/datalab/telemedicine-a-post-covid-reality-in-india.)
There is fear that coronavirus care will hinder care for persons with other conditions in public health circles, resulting in higher mortality. This anxiety is not illogical. People with life-threatening illnesses have less access to medicines, treatments, and diagnostics. Tuberculosis (T.B.), which kills over 1200 people every day in India, has been demonstrated in prior epidemics to increase fatalities from these underlying illnesses (Mohan Nachiket Mor, 2020).
3.3. Vaccination drive and PHC’s role
Having a widespread urban and rural India’s Vaccination Program universal immunization program (UIP), it is one of the world’s most well-known kinds, targeting over 2.67 crore babies and 2.9 crore pregnant women each year. India lacks adequate resources and preparation for the present COVID-19 outbreak, including vaccine supply, shipping, manufacturing, and availability. The Department of Biotechnology (DBT), according to the government, has backed 10 vaccine proposals, 7 of which are in clinical trials. To streamline COVID-19 vaccine logistics, India built the Electronic Vaccine Intelligence Network (eVIN). It automates vaccine stock management, cold chain monitoring, and logistics at all levels of vaccine storage across the country.
The massive immunization campaign in India started on January 16, 2021. The health ministry planned to vaccinate four target categories: healthcare employees, people over 50, public workers, and people under 50 with comorbidities, with the first two groups receiving vaccinations first in a 30-million-person launch, but COVID-19’s second wave was a cause for worry, and the government opened the immunization for above 18 years to combat the virus. The status of immunization program is stated below (Graph 3 ).
Graph 3.

Top 10 most populated beneficiaries vaccinated with a first and second dose of coronavirus.
(Source: https://www.mohfw.gov.in/pdf/CumulativeCovidVaccinationCovergeReport as of May 28, 2021.)
In their recent announcement dated June 7, 2021, the Central Government has rolled out a new policy of vaccinating the country free of cost, wherein private hospitals can procure 25% vaccine from the manufacturer directly and the rest the Central Government will use 75% to vaccinate the people of India. This is indeed a landmark announcement during these crucial times.
State governments and hospitals will now buy vaccinations directly from manufacturers under the Central Government’s revised vaccination program.
Because India is the world’s largest vaccine producer, it appears that vaccines are in short supply. Experts estimate that vaccinating India’s entire population would take years at this pace (BBC News, 2021).
The ability to operate cold chains that keep vaccines is dependent on the availability of electricity. Nearly 5% of rural PHCs in India, which serve over 2.8 million people, do not have access to electricity. As the government prepares for the COVID-19 immunization campaign, there is an opportunity to improve the energy efficiency of rural hospitals by designing better structures and investing in renewable energy sources such as solar. To accelerate a vaccination drive, the government has plans to seek associated healthcare professionals such as pharmacists and public health officials as pharmacists know cold chain storage that might help maintain the doses of the vaccine safe (Kumar et al., 2021).
3.4. How the present crisis can be an opportunity for change in the healthcare industry
Recent memory’s most significant health crises have revealed our healthcare system’s many flaws and imbalances and the importance of investing in “well-being” personally and systemic. It has brought in a new era of digital and technological advancements that will assist communities in meeting their requirements much more promptly. The question is what can be done in the future with the knowledge gained from this situation. Here are a few things that can be made to prevent similar crises in the future.
-
•
Potential for job creation in the healthcare sector: India’s healthcare sector has experienced a rapid and sustained expansion in recent years, resulting in many job openings. According to research conducted by KPMG and the FICCI, the healthcare business grew to become the fifth-largest employer in 2015; according to the National Sustainable Development Commission, the health sector will directly employ over 7.5 million people by 4, with around 2.7 million new employments created between 2017 and 4—an average of over 500,000 new positions per year. The health industry can employ many women employees. According to the WHO study, economic growth is boosted by USD 0.77 due to indirect and induced impacts for every dollar spent in the health sector.
-
•
National Digital Health Mission (NDHM): Our honorable Prime Minister Narendra Modi announced the launch of the NDHM in his address to the nation on India’s 74th Independence Day. The mission’s goals include creating databases of public and private hospitals, health service providers, laboratories, and pharmacies, improving clinical decision-making, and delivering Telemedicine services (Sarwal et al., 2021).
-
•
Medical manufacturing adoption: Nontraditional businesses like the auto and defense industries are experimenting with producing ventilators and lifesaving equipment. N95 masks, for example, are made by Honeywell, while ventilators are made by Tesla and Mahindra Auto. However, their long-term ability to work in the medical device industry is unknown. Still, such companies may think of diversifying in these areas as they have massive potential in the future.
-
•
Greater Focus on Digital Technology: Digital interfaces for remote patient monitoring and teleconsultations for nonemergency or elective physician consultations will become more common in the sector. Digital tools are already in use for contact tracing and some of the most notable technological advancements.
4. Discussion
When the first case of COVID-19 was reported in India on January 27, 2020, nobody knew that this monster would engulf 37,04,099 Indians (Ministry of Health and Family Welfare, 2021) within 15 months. Telemedicine services are gaining popularity, and the government has introduced new regulations to make it a lawful business in India. The Ministry of Health and Family Welfare (MoH&FW) has announced new rules in collaboration with NITI Aayog to allow medical practitioners to work from home. In addition, the government has launched the NDHM to address the country’s health issues (National Digital Health Mission). Health I.D.s, Telemedicine, health records, e-pharmacy, and Digi-doctor services are all part of this goal.
PHC is critical for ensuring global health security and accelerating progress toward universal health coverage. Strengthening PHC now will protect communities from future COVID-19 variants and other disease threats, aid in the recovery of social and economic activities by ensuring people’s health, and contribute to long-term global health goals.
More money should be put into primary healthcare, particularly in low- and middle-income nations, so that individuals may obtain inexpensive, accessible, and high-quality treatment regardless of where they reside or their circumstances.
-
•
More and better data should be produced and used to aid leaders in identifying significant deficiencies in health systems far before the next crisis comes.
-
•
Protect and support PHC workers as the backbone of robust health systems. They provide the tools they need to effectively combat COVID-19, prevent future disease outbreaks, and offer access to critical services.
-
•
As part of the Ayushman Bharat National Health Protection Scheme, the Indian Government wants to refurbish and build 150,000 primary care centers (Gopichandran and Subramaniam, 2020).
-
•
Nonetheless, to strengthen PHC in India and drastically boost their capacity and functions during a pandemic, a significant focus on infrastructural upgrades like ordering more ventilators, etc.
-
•
Governments must make the most of these expenditures by stressing primary healthcare as the foundation for a healthier, more equitable future (Ministry of Health and Family Welfare 2021a). The key to this achievement is the availability of quality and competitive medical facilities and skilled doctors at reasonable pricing and supportive immigration and insurance coverage, further investments in innovation, and growth by the Indian Government.
It is a wake-up call for us, and what is most important thing right now is to take the lessons learned from this pandemic and apply them in various Indian states where healthcare systems can be improved. We need to invest in and prepare healthcare workers for this epidemic; launch a massive public-education campaign, and establish a robust surveillance system to help reduce the spread and fatalities.
5. Conclusion
Coronavirus took the world by storm, and we have not recovered from it yet. To fight this monstrous virus, the government raised its budget allocation from 52,800 crores for health in 2018–19 (Business Today on May 13, 2021) to over ₹2.2 lakh crores in 2021–22. More than 15 types of health insurance schemes and policies are available for Indian citizens by the Government of India. The Indian pharmaceutical industry, which stands as the third-largest producer globally, has been growing exponentially. All this and many more are happening in the Indian healthcare industry. The healthcare sector was also significantly impacted and underwent various changes. This pandemic has affected almost one-sixth population as India being the second-most populous country globally, with a population of 1.35 billion. Both the business and public sectors were involved in the overall response to the pandemic. Private Indian healthcare organizations stepped up and provided the government with all of the resources needed, including testing COVID cases, quarantine facilities, medical professionals, and requisite equipment at government COVID-19 hospitals and home care. India’s healthcare market is predicted to grow to USD 372 billion by 4, thanks to improved healthcare knowledge, increased income, and easier access to insurance. The Indian Government wants healthcare spending to reach 2.5% of GDP (gross domestic product) by 2025 (Sarwal et al., 2021).
Therefore, a study of its trends and forecasts is essential to formulate effective strategies.
India, specifically, has a long way to go in this race. India has to take essential measures to increase the number of investments and resources in this sector. The quality of health services, the access to health facilities for everyone, and the preparedness for handling any such emergencies in the future have to be looked at. Gaining self-dependency in research and development, technology, raw materials, and production cannot be overlooked.
Glossary
- ASHA
Accredited Social Health Activists is a community of health workers governed by the Ministry of Health and Family Welfare in India, in 2005.
- FICCI
Federation of Indian Chambers of Commerce and Industry (FICCI) is an association of Indian business organizations established in 1927 and is dedicated to promoting the growth and global competitiveness of Indian businesses.
- Ministry of AYUSH
The Ministry of Ayurveda, Yoga, Naturopathy, Unani, Siddha, Sowa-Rigpa, and Homeopathy is purposed with developing education, research, and propagation of indigenous alternative medicine systems in India.
- NBCFDC
National Backward Classes Finance and Development Corporation was established in 1992 by the Government of India to improve and develop the economic activities for the members of Backward Classes who live below double the poverty line.
- NDHM
The National Digital Health Mission aims to develop the backbone necessary to support the integrated digital health infrastructure of the country. It will bridge the existing gap among different stakeholders of the Healthcare ecosystem through digital highways.
- NHM
The National Health Mission was launched by the Indian Government in 2013 by combining National Rural Health Mission and National Urban Health Mission, which aims to provide universal access to quality healthcare, affordable and equitable.
- NHP
National Health Policy is the decisions, plans, and actions undertaken by the Indian Government to achieve specific healthcare goals in India.
- NITI Aayog
This is a public policy think tank of the Government of India, established to achieve sustainable development goals with cooperative federalism by fostering the involvement of State Governments of India in the economic policy-making process using a bottom-up approach.
- NSDC
National Skill Development Corporation is a not-for-profit public limited company incorporated on July 31, 2008, under section 25 of the Companies Act, 1956, as a Public-Private Partnership model by the Ministry of Finance in India.
- PHC
Primary Health Centre, sometimes referred to as public health centers, are state-owned rural healthcare facilities in India.
- PM-JAY
Pradhan Mantri Jan Arogya Yojana is the most significant health assurance scheme in the world, which aims at providing a health cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization to over 10.74 crores poor and vulnerable families (approximately 50 crore beneficiaries) that form the bottom 40% of the Indian population.
- Pradhan Mantri Garib Kalyan Anna Yojana
It is a food security welfare scheme announced by the Government of India in March 2020 during the COVID-19 Pandemic in India.
- Primary healthcare
State-owned rural healthcare facilities in India.
- Secondary healthcare
District hospitals and Community Health Caters at the block level.
- Tertiary healthcare
Third level of the health system in which specialized consultative care is provided, usually on primary and secondary healthcare referral.
Abbreviations
- CHCs
Community Health Centers
- CHWs
community health workers
- DBT
Department of Biotechnology
- eVIN
Electronic Vaccine Intelligence Network
- IRDAI
The Insurance Regulatory and Development Authority of India
- MoH&FW
The Ministry of Health and Family Welfare in India
- SHS GmbH
Siemens Healthineers Holding I Gmb
- UIP
universal immunization program
- VHGs
Village Health Guides
References
- Abdel-All M., Abimbola S., Praveen D., Joshi R. What do Accredited Social Health Activists need to provide comprehensive care that incorporates non-communicable diseases? Findings from a qualitative study in Andhra Pradesh, India. Hum. Resour. Health. 2019;17(1):73. doi: 10.1186/s12960-019-0418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj A. Healthcare Industry in India Is Projected to Reach $372 bn by 2022. 2021. https://www.investindia.gov.in/sector/healthcare
- BBC News India Coronavirus: Over-18s Vaccination Drive Hit by Shortages. 2021. https://www.bbc.com/news/world-asia-india-56345591 [Online]
- Budd J., Miller B., Manning E., Lampos V., Zhuang M., Edelstein M., Rees G., Emery V., Stevens M., Keegan N., Short M., Pillay D., Manley E., Cox I., Heymann D., Johnson A., McKendry R. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020;26(8):1183–1192. doi: 10.1038/s41591-020-1011-4. [DOI] [PubMed] [Google Scholar]
- Chaturvedi A. Hindustan Times; 2020. Delhi Launches an App to Help Track Hospital Beds for Covid-19 Patients.https://www.hindustantimes.com/india-news/delhi-launches-app-to-help-track-hospital-beds-for-covid-19-patients/story-hXqAkjGqze28mQIVPcGZTM.html [Online] [Google Scholar]
- Chew N., Lee G., Tan B., Jing M., Goh Y., Ngiam N., Yeo L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A., Komalkumar R., Meenakshi P., Shah K., Patel B., Chan B., Sunny S., Chandra B., Ong J., Paliwal P., Wong L., Sagayanathan R., Chen J., Ying Ng A., Teoh H., Tsivgoulis G., Ho C., Ho R., Sharma V. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correspondent, S . The Hindu; 2021. Coronavirus | World’s Largest Vaccination Programme Begins in India on January 16.https://www.thehindu.com/news/national/coronavirus-worlds-largest-vaccination-programme-begins-in-india-on-january-16/article33582069.ece [Online] [Google Scholar]
- Covid19.who.int WHO Coronavirus (COVID-19) Dashboard. 2021. https://covid19.who.int/ [Online]
- Dayalani V., Dayalani V., Staff I. Inc42 Media; 2021. Telemedicine: A Post-Covid Reality in India.https://inc42.com/datalab/telemedicine-a-post-covid-reality-in-india/ [Online] [Google Scholar]
- Dst.gov.in Integrated Geospatial Platform to Help Area-Specific Strategies & Decisions in COVID-19 Outbreak | Department of Science & Technology. 2021. https://dst.gov.in/integrated-geospatial-platform-help-area-specific-strategies-decisions-covid-19-outbreak> [Online]. Available from:
- ETHealthWorld . ET HealthWorld; 2021. Indian Healthcare Industry in 2018 and Forecast for 2019.https://health.economictimes.indiatimes.com/news/industry/indian-healthcare-industry-in-2018-and-forecast-for-2019/67286959 [Online]. ETHealthworld.com. [Google Scholar]
- Garg S., Basu S., Rustagi R., Borle A. Primary health care facility preparedness for outpatient service provision during the COVID-19 pandemic in India: cross-sectional study. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/19927. https://publichealth.jmir.org/2020/2/e19927 (Accessed 28 May 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh A. The Print; 2021. What Is CoWIN, and What You Need to Register on the App for Covid Vaccine Shot.https://theprint.in/health/what-is-cowin-and-what-you-need-to-register-on-the-app-for-covid-vaccine-shot/579307/ [Online] [Google Scholar]
- Ghosh P. Hindustan Times; 2021. What Is Covid Severity Score? Govt’s New Software for Better Covid-19 Management.https://www.hindustantimes.com/india-news/what-is-covid-severity-score-govt-s-new-software-for-better-covid-19-management-101624103804398.html [Online] [Google Scholar]
- Gopichandran V., Subramaniam S. Response to Covid-19: an ethical imperative to build a resilient health system in India. Indian J. Med. Ethics. 2020;05(02):89–92. doi: 10.20529/ijme.2020.026. [DOI] [PubMed] [Google Scholar]
- IANS . News18; 2021. Johns Hopkins-Supported App to Guide Covid Patients at Home in India.https://www.news18.com/news/india/johns-hopkins-supported-app-to-guide-covid-patients-at-home-in-india-3885473.html [Online] [Google Scholar]
- India Brand Equity Foundation . India Brand Equity Foundation; 2021. Indian Pharmaceuticals Industry Report. [Online] [Google Scholar]
- Indian Council for Medical Research Total Operational (Initiated Independent Testing) Laboratories Reporting to ICMR. 2021. https://www.icmr.gov.in/pdf/covid/labs/archive/COVID_Testing_Labs_30052021.pdf [Online]
- Jha A. Second Wave Spreading Much Faster in Rural India Than First. 2021. https://www.hindustantimes.com/india-news/second-wave-spreading-much-faster-in-rural-India-than-first-101620416984127.html
- Kantis C., Kiernan S., Bardi J. Council on Foreign Relations; 2021. UPDATED: Timeline of the Coronavirus | Think Global Health.https://www.thinkglobalhealth.org/article/updated-timeline-coronavirus [Online] [Google Scholar]
- Kaul R. Hindustan Times; 2020. Covid-19: New Software in Focus for Registry of Deaths.https://www.hindustantimes.com/india-news/new-software-in-focus-for-registry-of-deaths/story-vkI73C8ZLNqUTPlMom20KI.html [Online] [Google Scholar]
- Kumar R. Fever, flu, and family physicians during COVID 19 pandemic 2020 in India. J. Fam. Med. Prim. Care. 2020;9(4):1781. doi: 10.4103/jfmpc.jfmpc_617_20. https://www.jfmpc.com/article.asp?issn=2249-4863;year=2020;volume=9;issue=4;spage=1781;epage=1783;aulast=Kumar [Online] (Accessed 28 May 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V.M., Pandi-Perumal S.R., Trakht I., et al. Strategy for COVID-19 vaccination in India: the country with the second-highest population and number of cases. npj Vaccines. 2021;6:60. doi: 10.1038/s41541-021-00327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurian O.C. Running to Stand Still: Healthcare in India in 2021. 2021. https://www.orfonline.org/expert-speak/running-stand-still-healthcare-india-in-2021/
- M/o Statistics & Programme Implementation, GOI – MOSPI . National Sample Survey Office; 2016. India – Social Consumption - Health Survey: NSS 71st Round, Schedule 25, January–June 2014. [Google Scholar]
- Mahajan P., Kaushal J. Epidemic trend of COVID-19 transmission in India during lockdown-1 phase. J. Community Health. 2020;45(6):1291–1300. doi: 10.1007/s10900-020-00863-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megsres.nic.in Salient Features of MGNREGA | Official Website of State Rural Employment Society, Government of Meghalaya, India. 2021. https://megsres.nic.in/salient-features-mgnrega [Online]. Available from:
- Ministry of Health & Family Welfare . Ministry of Health & Family Welfare; 2021. Containment Plan: Novel Coronavirus Disease 2019 (COVID 19): Version 2.https://www.mohfw.gov.in/pdf/Containmentplan16052020.pdf [Online] [Google Scholar]
- Ministry of Health and Welfare, Government of India . Ministry of Health and Welfare, Government of India; 2017. National Health Policy; p. 28.https://www.nhp.gov.in/nhpfiles/national_health_policy_2017.pdf [Online] [Google Scholar]
- Mishra A. Healthcare Industry 2018 Recap 2019 Forecast. 2019. https://www.medicalmagazine.in/healthcare-industry-2018-recap-2019-forecast/
- Mohan Nachiket Mor P. BusinessLine by Times of India; 2020. Covid-19 Crisis: Shift Focus From Hospitals to Primary Care.https://www.thehindubusinessline.com/opinion/covid-19-crisis-shift-focus-from-hospitals-to-primary-care/article31278485.ece [Online] [Google Scholar]
- MoHFW . Ministry of health and Welfare, Government of India; 2021. Micro Plan for Containing Local Transmission of Coronavirus Disease (COVID-19) pp. 1–26.https://www.mohfw.gov.in/pdf/ModelMicroplanforcontainmentoflocaltransmissionofCOVID19.pdf (eBook) [Google Scholar]
- MoHFW MoHFW. 2021. https://www.mohfw.gov.in/ [Online] Mohfw.gov.in.
- Mukherjee I. India News – Times of India; 2021. Covid Vaccine Export: India Exports over Twice the Number of Doses Used at Home.https://timesofindia.indiatimes.com/india/india-exports-over-twice-the-number-of-doses-used-at-home/articleshow/81540812.cms [Online] The Times of India. [Google Scholar]
- National Portal of India, n.d. https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission. Ayushman Bharat. National Health Protection Mission. National Portal of India.
- News W. WHO – Times of India; 2021. Significant Undercount of Covid-19 Deaths Globally, Real Number About 2 Times Higher Than Official Stats.https://timesofindia.indiatimes.com/world/us/significant-undercount-of-covid-19-deaths-globally-real-number-about-2-times-higher-than-official-stats-who/articleshow/82848634.cms [Online] The Times of India. [Google Scholar]
- Orissadiary.com CCI Approves Acquisition by Siemens Healthineers Holding I Gmb (SHS GmbH) of Varian Medical Systems, Inc. (Varian) 2021. https://orissadiary.com/cci-approves-acquisition-by-siemens-healthineers-holding-i-gmb-shs-gmbh-of-varian-medical-systems-inc-varian/ [Online] orissadiary.com.
- Pib.gov.in Finance Minister Announces Rs 1.70 Lakh Crore Relief Package Under Pradhan Mantri Garib Kalyan Yojana for the Poor to Help Them Fight the Battle Against Corona Virus. 2021. https://pib.gov.in/PressReleasePage.aspx?PRID=1608345 [Online] Available from:
- Poovanna S. Covid-19: Karnataka govt Develops Software to Manage Shortage of Hospital Beds. 2020. https://www.livemint.com/news/india/covid-19-karnataka-govt-develops-software-to-manage-shortage-of-hospital-beds-11593930441365.html [Online] mint.
- Press Information Bureau COVID Vaccination Administration Training Programme for Health Care Workers Belonging to Target Group of NBCFDC. 2021. https://pib.gov.in/Press Release Detail.aspx?PRID=1694468 [Online]
- Press Trust of India Covid Effect: 1,952 Employees Dead, 1,000 Infected Daily, Says Railways. 2021. https://www.business-standard.com/article/indian-railways/covid-effect-1-952-employees-dead-1-000-infected-daily-says-railways-121051000958_1.html
- Priyamvatha P. India Today; 2021. How India’s Second Covid Wave Started, What Went Wrong, and What Can Be Done: top Virologist Answers.https://www.indiatoday.in/coronavirus-outbreak/story/india-second-covid-wave-start-went-wrong-top-virologist-answers-details-1795743-2021-04-28 [Online] [Google Scholar]
- Rai R., Tripathi S., de Lange A.H. In: Integrating the Organization of Health Services, Worker Wellbeing and Quality of Care Towards Healthy Healthcare. Tevik Løvseth L., de Lange A.H., editors. Springer Nature Switzerland AG; 2021. Healthy healthcare systems in India: a prognosis. (Accessed 28 May 2021) [DOI] [Google Scholar]
- Ranga Rao S. Mittal Publications; New Delhi, India: 1993. Administration of Primary Health Centres in India. [Google Scholar]
- Rastogi A. Mission Indradhanush. 2019. https://www.nhp.gov.in/mission-indradhanush1_pg
- Ray S. India Declares ‘Black Fungus’ Epidemic as Infections Rise Among Covid-19 Patients. 2021. https://www.forbes.com/sites/siladityaray/2021/05/20/india-declares-black-fungus-epidemic-as-infections-rise-among-covid-19-patients/?sh=38fe3f7110af
- Rekha M. COVID-19: Health Care System in India. Health Care: Curr. Rev. 2020;(S1):262. [Google Scholar]
- Sachan D. How Will COVID-19 Shape the Future of the Healthcare Industry? 2021. https://www.cyient.com/blog/medical-technology-healthcare/how-will-covid-19-shape-the-future-of-the-healthcare-industry [Online] Cyient.com.
- Sahay, A., 2020. Indian Startup Develops Covid 19 Detecting Mobile App, Takes 5 Minutes. Hindustan Times. https://www.hindustantimes.com/india-news/indian-startup-develops-covid-19-detecting-mobile-app-takes-5-minutes/story-pB69DtRslPDJkx3tF1gOdN.html (Accessed 25 July 2021).
- Saprii L., Richards E., Kokho P., Theobald S. Community health workers in rural India: analysing the opportunities and challenges Accredited Social Health Activists (ASHAs) face in realising their multiple roles. Hum. Resour. Health. 2015;13(1):95. doi: 10.1186/s12960-015-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwal R., Prasad U., Madangopal K., Kalal S., Kaur D., Kumar A., Regy P., Sharma J. NITI Aayog; 2021. Investment Opportunities in India’s Healthcare Sector.https://niti.gov.in/sites/default/files/2021-03/InvestmentOpportunities_HealthcareSector_0.pdf [Online] [Google Scholar]
- Standard B. International News: World News Headlines, World Breaking News, Global News. 2021. https://www.business-standard.com/international?time=1622423456 [Online] Business-standard.com.
- Statista Research Department Estimated Value of Public Health Expenditure in India From Financial Year 2017 to 2020. 2021. https://www.statista.com/statistics/684924/india-public-health-expenditure/#:~:text=In%20fiscal%20year%202018%2C%20the,percent%20of%20the%20country's%20GDP
- TechnoFunc . Technofunc.com; 2021. Sectors of Healthcare Industry.https://www.technofunc.com/index.php/domain-knowledge/healthcare-industry/item/sectors-of-healthcare-industry [Google Scholar]
- The Economic Times Ten States Account for Over 73 Per cent of New COVID-19 Cases in India. 2021. https://economictimes.indiatimes.com//news/india/ten-states-account-for-over-73-per-cent-of-new-covid-19-cases/articleshow/82516130.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst Read more at.
- The Hindu How Does the Aarogya Setu App Work? 2020. https://www.thehindu.com/news/national/how-does-the-aarogya-setu-app-work/article31532073.ece [Online]
- The Hindu Healthcare Industry Welcomes Increased Budget Allocation. 2021. https://www.thehindu.com/business/budget/healthcare-industry-welcomes-increased-budget-allocation-for-health-well-being/article33717111.ece [Online]. Available from:
- Varma A. Second COVID-19 Wave in India: Here Are Some Challenges & Points of Concern. 2021. https://www.republicworld.com/india-news/general-news/second-covid-19-wave-in-india-here-are-some-challenges-and-points-of-concern.html [Online]
- WION Coronavirus Second Wave Hits Countries as Lockdown Ends. 2021. https://www.wionews.com/photos/coronavirus-second-wave-hits-countries-as-lockdown-ends-308495 [Online]
- World, G . Geospatial World; 2020. Top Indian Apps to Fight COVID-19.https://www.geospatialworld.net/blogs/top-indian-apps-to-fight-covid-19/ [Online] [Google Scholar]
Further reading
- Associates, D . India Briefing News; 2021. COVID-19 in India: Updates Till December 31, 2020 – India Briefing News.https://www.india-briefing.com/news/covid-19-india-december-31-2020-20585.html/ [Online] [Google Scholar]
- Chathukulam J., John M.S. Empowerment of women panchayat members: learning from Kerala (India) Asian J. Women’s Stud. 2000;6:66–101. [Google Scholar]
- Declaration of Alma-Ata, n.d. International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978. https://www.who.int/publications/almaata_declaration_en.pdf?ua=1 (Accessed 7 January 2021).
- Government of India Indian Public Health Standards (IPHS) Guidelines for Primary Health Centers. 2021. http://clinicalestablishments.gov.in/WriteReadData/360.pdf Revised 2012. [Online] Clinicalestablishments.gov.in.
- Independence Day 2018 PM Narendra Modi May Announce National Healthcare Policy on August 15; Ayushman Bharat Cover for 10 Crore Poor Families. https://www.india.com/business/indepedence-day-2018-pm-narendra-modi-may-announce-national-healthcare-policy-on-august-15-ayushman-bharat-to-offer-rs-5-lakh-cover-to-10-crore-poor-families-3222173/
- Khazir M., Abdullah S., Tangade P., Jain A., Gupta A. How Primary Health Care was originated in India. TMU J. Dent. 2018;5(3):10–12. http://www.tmujdent.co.in/pdf/vol5issue3/vol%205%20issue%203_04.pdf [Online] (Accessed 28 May 2021) [Google Scholar]
- Mahajan P.B. ROME scheme: from reorientation to research-oriented medical education, a new beginning. Indian J. Med. Res. 2010;132:110. [Medline: 20693602] [PubMed] [Google Scholar]
- Ministry of Health & Family Welfare Containment Plan: Novel Coronavirus Disease 2019 (COVID 19): Version 2. 2020. https://www.mohfw.gov.in/pdf/Containmentplan16052020.pdf
- Ministry of Health & Family Welfare . 2021. Micro plan for containing local transmission of coronavirus disease (COVID-19) [Google Scholar]
- Mohfw.gov.in . Home; 2021. MoHFW.https://www.mohfw.gov.in/ [Online] [Google Scholar]
- Organization, W. and (UNICEF), U Immunization in the Context of COVID-19 Pandemic: Frequently Asked Questions (FAQ) 2021. https://apps.who.int/iris/handle/10665/331818 16 April 2020. [Online] Apps.who.int.
- PM Office Cabinet Approves the Allocation of Additional Food Grain to NFSA Beneficiaries Under Pradhan Mantri Garib Kalyan Anna Yojana (Phase III) for Another Period of Two Months, May and June 2021. 2021. https://www.pmindia.gov.in/en/news_updates/cabinet-approves-allocation-of-additional-foodgrain-to-nfsa-beneficiaries-under-pradhan-mantri-garib-kalyan-anna-yojana-phase-iii-for-another-period-of-two-months-may-and-june-2021/?comment=disable [Online] Pmindia.gov.in.
- Pmkisan.gov.in Home. 2021. https://pmkisan.gov.in/ [Online] Available from: (Accessed 17 September 2021)
- Press Information Bureau Delhi Key Highlights of Union Budget 2021–22. 2021. https://pib.gov.in/PressReleasePage.aspx?PRID=1693907 [Online]
- Royal A., Mali M.A., Kumar V., Wagh I.A., Bhushan S., Mokal A.N., Mehta K., Bhattacharya S. Harnessing the potential of the primary healthcare facilities in India to respond COVID-19 Pandemic: a scoping evidence-based research synthesis. J. Fam. Med. Prim. Care. 2021;10:116–121. doi: 10.4103/jfmpc.jfmpc_1609_20. https://www.jfmpc.com/text.asp?2021/10/1/116/307936 [Online] (Accessed 31 May 2021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Consumption . Health Survey: NSS 71st Round, Schedule 25, January–June 2014, India (pdf) 2014. http://www.icssrdataservice.in/datarepository/index.php/catalog/107,DDI-IND-MOSPI-NSSO-71Rnd-Sch25pt0-Jan-June-2014 [Google Scholar]
- Tatacapitalblog What Are the Steps Taken by the Government to Fight Coronavirus in India? 2020. https://www.tatacapital.com/blog/trends/what-are-the-steps-taken-by-the-government-to-fight-coronavirus-in-India/
- Ved R., Gupta G., Singh S. India’s health and wellness centres: realizing universal health coverage through comprehensive primary health care. WHO South East Asia J. Public Health. 2019;8(1):18–20. doi: 10.4103/2224-3151.255344. Medline: 30950425. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 1978. Primary Health Care: Report of the International Conference on Primary Health Care Alma Ata, USSR, 6–12 September 1978. Geneva, Switzerland. [Google Scholar] [Google Scholar]
- World Health Organization . World Health Organization; 2020. Coronavirus Disease 2019 (COVID-19): Situation Report-51.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrs n=1ba62e57_10 [Google Scholar]
- Worldometers.info . Worldometer; 2021. COVID Live Update: 171,010,903 Cases and 3,556,329 Deaths From the Coronavirus.https://www.worldometers.info/coronavirus/#countries [Online] [Google Scholar]


