Abstract
The syndrome of Leser‐Trélat (LT) is a rare paraneoplastic syndrome. However, patients presenting with the sign of Leser‐Trélat should be considered to harbor an occult malignancy or a progressive tumor disease until “proven” otherwise. Herein, we present two cases of non‐small‐cell lung carcinoma associated with LT syndrome.
Keywords: diagnosis, lung cancer, progressive disease, syndrome of Leser‐Trélat
The Leser‐Trélat syndrome is a rare paraneoplastic syndrome. However, patients presenting with the sign of LT should be considered to harbor an occult malignancy or a progressive tumor disease until “proven” otherwise, which can lead to an early diagnosis.

1. INTRODUCTION
The Leser‐Trélat syndrome (LTS) is a rare paraneoplastic syndrome. It may be defined as the sudden eruption of multiple seborrheic keratoses caused by malignancy. 1 The description of this syndrome has been credited separately to Edmund Leser (1853–1916) and Ulysse Trélat (1827–1890). But, in 1990, Hollander was the first to emphasize the association of internal cancer with seborrheic keratoses. 2 This paraneoplastic syndrome is most frequently associated with the gastrointestinal tract tumors (72%) and adenocarcinomas (76%). 3 However, in rare cases, other primary tumors could be seen associated with LTS as breast, ovary, uterus, lymphoma, melanoma, and lung cancer. 2 In fact, patients presenting with the sign of LT should be considered to harbor an occult malignancy until “proven” otherwise. 4 Herein, we present two cases of non‐small‐cell lung carcinomas associated with LTS that highlight the possibility of an early diagnosis of intern malignancy or progressive tumor disease thanks to LT sign.
2. CASE REPORTS
2.1. Case 1
A 78‐year‐old smoker man, presented with 3‐month history of dysphonia, dyspnea, and chest pain. On presentation, he had 97% on pulse oximetry on room air, crackles on auscultation of the right lung and a normal neurological, cardiovascular, and abdominal exam. However, he had innumerable non‐eruptive seborrheic keratoses on his back (Figure 1). Those lesions appeared suddenly one year ago but the patient did not pay any importance to them. High‐resolution computed tomography (CT) scan of the chest demonstrated a large mass of the left apical lung (80 × 50 mm) with mediastinum's invasion which explained the paralysis of the recurrent laryngeal nerve (Figure 2). CT‐guided needle biopsy of the lung was performed and histological analysis showed an adenocarcinoma of the lung. Immunohistochemistry revealed positive reaction in tumor cells for CD56(+), CD117(+), CK7(+), P40(+), TTF1(+) without any ALK or EGFR mutation. The tumor was classified T3N2M1c with renal metastases. Therefore, the appearance of multiple seborrheic keratoses and the presence of lung cancer defined the LTS. In this case, the LTS had appeared 1 year before the lung cancer's symptoms.
FIGURE 1.

Clinical presentation of innumerable seborrheic keratoses on the back (case n°1)
FIGURE 2.
CT scan of case n°1: large mass of the left apical lung (80×50 mm) with mediastinum's invasion
2.2. Case 2
The second patient is a 76‐year‐old smoker man with a history of coronary disease treated by a coronary artery bypass surgery. He had an adenosquamous carcinoma of the lung in first stage (T1N0M0) (Figure 3). Surgery was not possible in front of his hurt disease. He was treated with exclusive radiotherapy. Six months later, the patient presented dry cough, dyspnea, asthenia, and urinary incontinence. He also noticed a sudden appearance of multiple eruptive seborrheic keratoses on his back (Figure 4). Full body CT scan demonstrated large left upper lobar mass which engulfs the left pulmonary artery, invades the hilum, left stem branch up to the carina with multiple hilar and mediastinal lymph nodes (Figure 5) and the appearance of lever, pulmonary, and sacrum metastases. Overall, the findings were compatible with the diagnosis of progressive tumor disease. The appearance of LTS coincides in this case with the tumor progression.
FIGURE 3.

CT scan of case n°2: solid nodular lesion in the upper left lung
FIGURE 4.

Multiple seborrheic keratoses on the back of case n°2
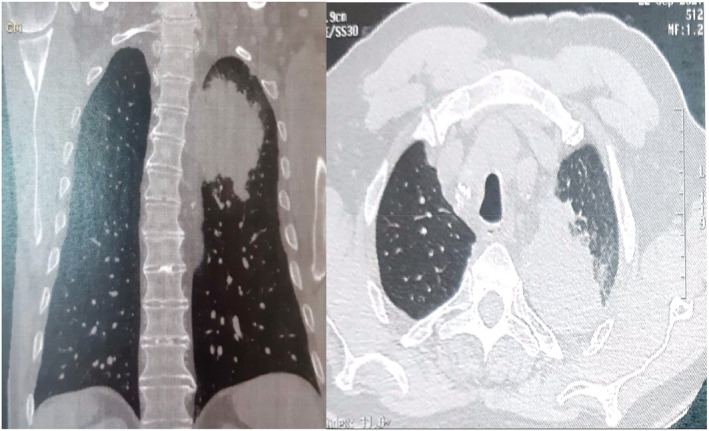
FIGURE 5.

CT scan of the chest demonstrated large left upper lobar mass which engulfs the left pulmonary artery, invades the hilum, left stem branch up to the carina with multiple hilar and mediastinal lymph nodes
3. DISCUSSION
The LTS is a paraneoplastic syndrome characterized by the sudden appearance of multiple seborrheic keratoses in association with internal occult malignancy. 1 We present two non‐small‐cell lung carcinomas associated with LTS that highlight the possibility of an early diagnosis of intern malignancy or progressive disease. In our first case, the appearance of multiple seborrheic keratoses was ignored and the lung cancer was diagnosed 1 year later due to respiratory symptoms. In fact, although seborrheic keratoses are common findings, the early appearance of these keratoses and their eruptive nature are uncommon. However, LTS is probably underestimated because of the lack of importance assigned to multiple seborrheic keratoses in personal clinical surveys. 5 In the literature, rare cases of LT sign associated with lung cancer were reported. 4 , 6 , 7 Heaphy et al 4 were the first to report the sign of LT in association of adenocarcinoma of the lung in 2000. To prove the association with malignant disease, Swartz et al 2 did a retrospective review of 1752 patients with seborrheic keratoses and they found that within 1 year, 62 patients was diagnosed with visceral malignancy. This association was due to the high level of epidermal growth factor receptors (EGFR) protein expressed by the tumor postulated many writers. High levels of EGFR might play a role for the development of seborrheic keratoses. 1 , 2 , 4 , 6 In a review of literature included 121 cases with a mean patient age of 61.8 years, the authors found that this syndrome was observed before (68.3%), after (22.1%), and at the time of (9.6%) malignancy diagnosis. 8 Thus, patients presenting with the sign of LT should be considered to harbor an occult malignancy until proven otherwise. 4 However, the sign of LT as a paraneoplastic dermatoses disappears when the primary tumor is removed and reappear in case of recurrence or metastases of the cancer. 5 The case reported by Heaphy et al 4 showed that one year after treatment, the patient noticed many new seborrheic keratoses. A CT scan confirmed that the tumor had grown significantly such was the case of our second patient. In fact, Hussain and et al found that treatment resulted in clinical improvement (45%), no change (30%), exacerbation (15%), or initial improvement followed by the exacerbation of seborrheic keratoses. 8 And patient outcomes included disease stability/improvement (48.4%), recurrence (9.7%), exacerbation/metastasis/new malignancy (4.8%), and death (37.1%). 8
4. CONCLUSION
LTS is a rare paraneoplastic phenomenon that doctors should pay attention to it to make an early diagnosis of intern malignancy or progressive disease. In fact, patients with LT must be screened to rule out the presence of occult cancer.
AUTHOR CONTRIBUTIONS
Rim Khemakhem and Rahma Jarraya took the lead in writing the manuscript and did the literature review. Nesrine Kallel conceived of the presented idea. All authors provided critical feedback and helped shape the manuscript.
CONSENT
The written consent of patients has been obtained.
ACKNOWLEDGMENTS
None.
Khemakhem R, Kallel N, Jarraya R, Yangui I, Kammoun S. Leser‐Trélat syndrome secondary to non‐small‐cell lung carcinoma. Clin Case Rep. 2022;10:e06069. doi: 10.1002/ccr3.6069
DATA AVAILABILITY STATEMENT
None
REFERENCES
- 1. Jepsen RK, Skov AG, Skov BG. Leser‐Trelat syndrome in malignant mesothelioma and pulmonary adenocarcinoma: is the EGFR pathway part of the syndrome? Virchows Archiv. 2014;464(1):117‐120. [DOI] [PubMed] [Google Scholar]
- 2. Schwartz RA. Sign of Leser‐Trelat. J Am Acad Dermatol. 1996;35(1):88‐95. [DOI] [PubMed] [Google Scholar]
- 3. Wagner RF, Wagner KD. Malignant neoplasms and the Leser‐Trelat sign. Arch Dermatol. 1981;117(9):598‐599. [PubMed] [Google Scholar]
- 4. Heaphy MR Jr, Millns JL, Schroeter AL. The sign of Leser‐Trelat in a case of adenocarcinoma of the lung. J Am Acad Dermatol. 2000;43(2 Pt 2):386‐390. [DOI] [PubMed] [Google Scholar]
- 5. Ponti G, Luppi G, Losi L, Giannetti A, Seidenari S. Leser‐Trelat syndrome in patients affected by six multiple metachronous primitive cancers. J Hematol Oncol. 2010;3:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hattori A, Umegae Y, Kataki S, Nakajima T. Small cell carcinoma of the lung with Leser‐Trelat sign. Arch Dermatol. 1982;118(12):1017‐1018. [PubMed] [Google Scholar]
- 7. Horiuchi Y, Katsuoka K, Yoshimura H, Kanzaki T, Nishiyama S. Acanthosis nigricans and Leser‐Trelat sign associated with squamous cell carcinoma and adenocarcinoma of the lung. Int J Dermatol. 1986;25(7):459‐460. [DOI] [PubMed] [Google Scholar]
- 8. Husain Z, Ho JK, Hantash BM. Sign and pseudo‐sign of Leser‐Trelat: case reports and a review of the literature. J Drugs Dermatol. 2013;12(5):e79‐e87. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None


