Abstract
Background: Growing resistance to clarithromycin is a major concern regarding treating Helicobacter pylori (H. pylori) infection. Resistance rates have a great variation even in different geographic areas within the same country and are associated with point mutations of the microbial 23S rRNA (A2142C, A2142G, and A2143G). Given the absence of available data in Thrace, the objective of this study was to estimate the resistance of H. pylori to clarithromycin and identify specific mutations that contribute to clarithromycin resistance.
Methods: In this prospective study, we enrolled consecutive patients referred for dyspeptic complaints who underwent upper gastrointestinal endoscopy over two years. Gastric biopsies from corpus and antrum were initially tested for the presence of urease by a rapid urease test. Urease positive samples were followed by real-time PCR to confirm the presence of H. pylori and to detect point mutations.
Results: A total of one hundred and thirty patients were included in the study (72 women and 58 men). Resistance to clarithromycin was detected at 23.2 %. Neither gender nor age was independently correlated with resistance rate in our patient group. The most common mutations were A2142G and A2143G.
Conclusions: A high rate of H. pylori resistance to clarithromycin was observed in our region, implicating that it should be addressed in accordance with the recommendations provided by national and international guidelines. Molecular testing should be considered an integral tool for effective monitoring in case of suspected antibiotic resistance. HIPPOKRATIA 2021, 25 (2):51-55.
Keywords: Helicobacter pylori, clarithromycin, resistance, mutation, 23S rRNA, Thrace
Introduction
Isolation and culture of Helicobacter pylori (H. pylori), a gram-negative bacterium that colonizes the stomach, was first described by Warren and Marshall in the 1980s. Today, approximately 50 % of the world’s population is infected. Prevalence is highly variable among regions due to existing socioeconomic differences1-5.
H. pylori has a pivotal role in the pathogenesis of multiple gastrointestinal illnesses like chronic and atrophic gastritis, duodenal and gastric ulcer disease, and gastric adenocarcinoma. Additionally, there is ongoing research regarding extra-gastric gastroduodenal diseases linked to H. pylori. These manifestations include an extensive spectrum of metabolic, hematologic, neurologic, and dermatologic aliments6-9.
The main component of modern H. pylori treatment regimens is clarithromycin. Clarithromycin is a macrolide that inhibits protein synthesis by binding and slowing down bacterial ribosomal unit activity10,11. In a meta-analysis including patients who received clarithromycin-based therapy, the success of eradication rates for the H. pylori sensitive and resistant strains accordingly were as high as 90 and 22 percent, respectively12. Additionally recent data show that resistance to macrolides increases due to its extended use for different indications13. As a result, the success rate of triple therapies containing clarithromycin is declining to unacceptable levels.
H. pylori clarithromycin resistance is predominantly caused by point mutations in the peptidyl transferase region encoded in domain V of the 23S rRNA gene. Common mutations are A2143G, A2142G, and A2142C. These are responsible for most cases of primary resistance to clarithromycin in the western world12-16.
In the present study, we aimed to i) estimate the resistance to clarithromycin in Thrace, Greece, ii) describe the responsible common mutations, and iii) briefly review the most recent available data to assist clinical decision making in choosing optimal treatment for patients affected by H. pylori infection.
Materials and Methods
Patients
This prospective cohort study enrolled all consecutive patients referred to the Endoscopy Department of the University General Hospital of Alexandroupolis from January 2017 to December 2019. We specifically included only patients naïve to H. pylori treatment (Table 1). Patients were excluded if under 18 years of age or had received antibiotics or proton pump inhibitors (PPI) in the previous three months.
Table 1. The demographic and clinical characteristics of the study’s 130 patients referred for dyspeptic complaints and underwent an upper gastrointestinal endoscopy.
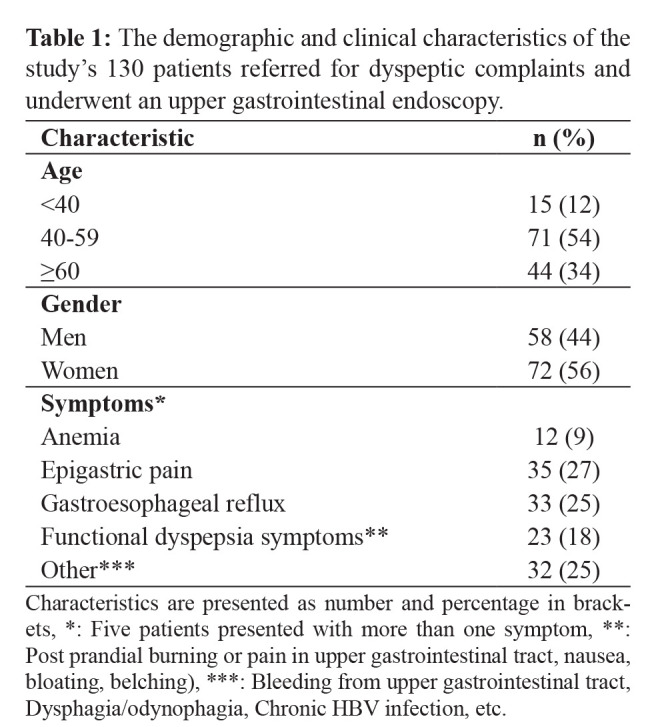
Characteristics are presented as number and percentage in brackets, *: Five patients presented with more than one symptom, **: Post prandial burning or pain in upper gastrointestinal tract, nausea, bloating, belching), ***: Bleeding from upper gastrointestinal tract, Dysphagia/odynophagia, Chronic HBV infection, etc.
A written and signed informed consent was obtained from all participants. The protocol was approved by the Ethics Committee of University General Hospital of Alexandroupolis (decision No 35, date: 3/6/2015).
Biopsies collection and rapid urease test
All patients underwent an upper gastrointestinal endoscopy performed by an Olympus Exera Video Gastrointestinal Endoscope (Olympus, Tokyo, Japan). We obtained two sets of biopsies from the gastric antrum and the corpus. Both biopsies (from antrum and corpus) were used to increase diagnostic accuracy. Samples were initially tested for the presence of urease with the use of a rapid urease test (Pronto Dry, Gastrex, Gilly Lès Cîteaux, France). Due to rapid urease tests’ high sensitivity and specificity, only urease positive samples were further processed for DNA extraction17-21.
DNA extraction
Biopsies were placed in 1.5 ml Eppendorf tubes (Eppendorf AG, Hamburg, Germany) with saline solution and transferred to the Microbiology Department. DNA was extracted using the NucleoSpin Tissue Genomic DNA Purification kit (Macherey-Nagel, Duren, Germany) according to the manufacturer’s instructions (briefly described below). Initially, biopsies were cut into small pieces, placed in 1.5 ml sterilized tubes, and suspended in 180 μL of T1 buffer and 25 μL proteinase K. The mixture was incubated at 56 °C for 1-3 hours (pre-lyse). After that, 200 μL of B3 buffer was added, and samples were incubated at 70 °C for ten minutes (Lyse). In the next step, we added 210 μL of 96-100 % cold ethanol (adjust DNA binding conditions). The supernatant was collected after centrifugation at 11,000 ×g for one minute (Bind DNA). The DNA pellet was washed two times (first wash with 500 μL BW buffer and second wash 600 μL B5 buffer) and centrifuged at 11,000 × g for one minute (wash silica membrane). Next, the silica membrane was dried by centrifugation at 11,000 × g for one minute (Dry silica membrane). After that, 100 μL BE buffer was added, incubated at 70 °C for one minute, and centrifuged at 11,000 × g (for one minute). DNA concentration was checked with the NanoDrop 2000UV-Vis Spectrophotometer (Thermo Scientific, Wilmington, Delaware, USA) and stored at -20 oC until used.
Real-time PCR
DNA was amplified for the 23SrRNA gene by a method primarily described by Oleastro et al. It is a real-time polymerase chain reaction (PCR) used to detect H. pylori and associated gene mutations of clarithromycin resistance (A2142C, A2142G, and A2143G), at the same time. This assay included amplifying a 267 bp fragment of the 23S rRNA gene by probe hybridization and thermal analysis by FRET (fluorescence resonance energy transfer) technology using the Roche LightCycler (Roche, Basel, Switzerland)22,23. The LightCycler was tuned according to the following protocol: First Denaturation at 95 οC for 10 min, followed by Proliferation (45 cycles: 95 οC for 0 sec, 60 οC for 10 sec, 72 οC for 17 sec), then Melting curve (95 °C for 0 sec and 45 °C for 30 sec at temperature transition rate of 20 °C/s; 85 °C at a rate of 0.1 °C/s), and finally Cooling (40 °C for 30 sec). Four different melting curves with melting temperatures (Tm) of approximately 54.11 °C for mutations A2142G and A2143G, 56.29 °C for A2142C, and 61.6 °C for the wild type of strain, were produced by the melting curve analysis of DNA from the positive control strains.
Statistical Analysis
A generalized linear model was used to assess the potential independent correlation of gender and age ≥60 (dependent variables/predictors) with H. pylori resistance (independent variable) in the presence of various symptoms as gastroesophageal reflux disease (GERD), dyspepsia, epigastric pain, anemia, and others (covariates). Medians are accompanied by their interquartile range (IQR), percentages are provided with their 95 % confidence intervals, and all numerical values are given with at least two decimals. The level of statistical significance was set at 0.05. The IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The MedCalc® Statistical Software version 19.8 (MedCalc Software Ltd, Ostend, Belgium) was utilized to construct the forest plot.
Results
The flow chart of this study is presented in Figure 1. In total, one hundred and thirty patients with upper gastrointestinal tract complaints were enrolled. There were 72 women (56 %) and 58 men (44 %) with an average of 53 years of age. Fifteen patients were younger than 40 years old (12 %), 71 were between 40-59 years old (54 %), and 44 were 60 years old or older (34 %). Their main symptoms were epigastric pain (27 %) and gastroesophageal reflux (25 %). Five patients had more than one symptom (Table 1). Neither of them had received therapy for H. pylori nor antibiotics and PPI three months before the endoscopy.
Figure 1. Flow chart of this prospective cohort study that enrolled consecutive patients referred for dyspeptic complaints and underwent upper gastrointestinal endoscopy.
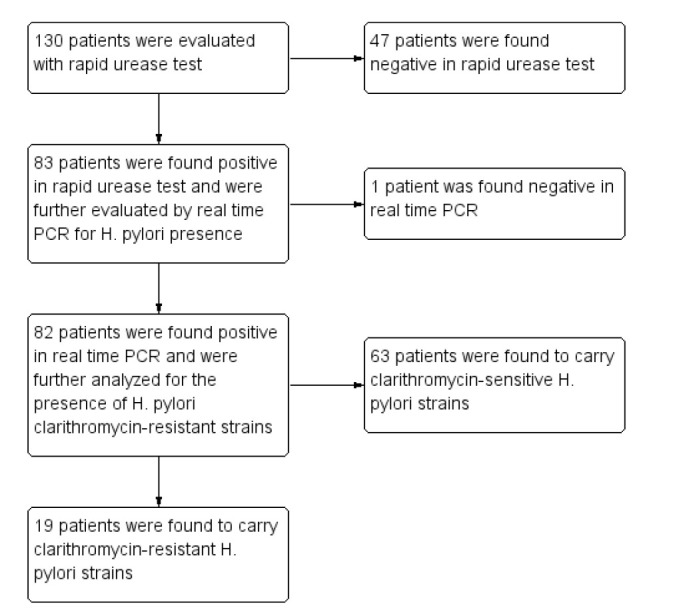
The rapid urease test was positive in 83 out of 130 biopsy samples (63.8 %). H. pylori DNA was confirmed by real-time PCR in 82 of 83. The concordance between the two methods was 98.8 %. Real-time PCR detected clarithromycin resistance in 19 out of 82 (23.2 %) biopsies samples. Thirteen (68 %) had a single mutation at position A2142G or A2143G (H. pylori clarithromycin resistant strains). Six had both susceptible and resistant subpopulations in the same biopsy; Four samples contained a wild type (H. pylori clarithromycin susceptible strain) and a point mutation at A2142G or A2143G, and two samples contained a wild type and a point mutation at A2142C (H. pylori clarithromycin resistant strain) (Table 2).
Table 2. Prevalence of clarithromycin resistance of Helicobacter pylori.
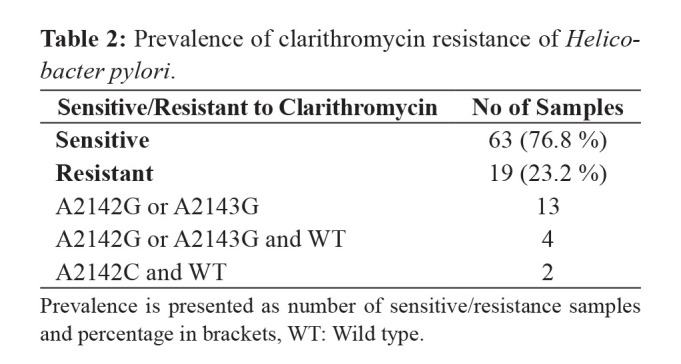
Prevalence is presented as number of sensitive/resistance samples and percentage in brackets, WT: Wild type.
Applying a generalized linear model incorporating H. pylori resistance as the independent variable, gender, and age ≥60 as independent variables (predictors), and symptoms (GERD, dyspepsia, epigastric pain, anemia, and others) as covariates, H. pylori resistance was documented to be independent of both sex (p =0.504) and age ≥60 (p =0.792).
Discussion
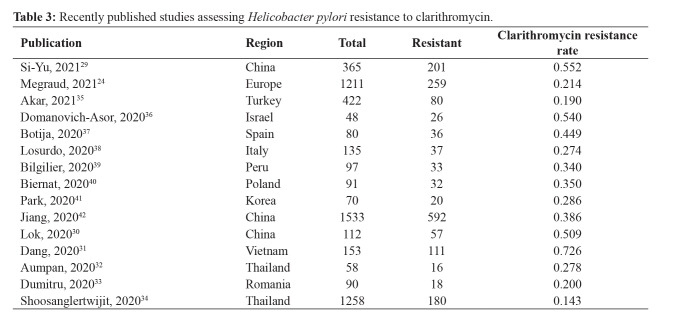
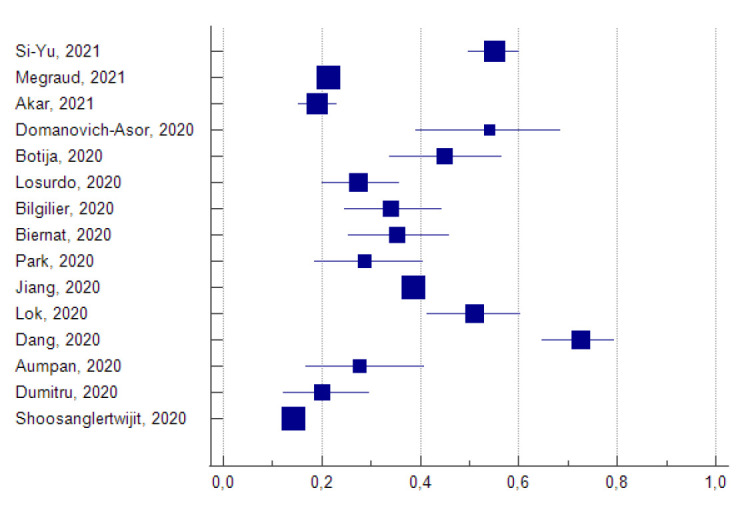
In the current prospective study, the first conducted in Thrace, Greece, we demonstrated that the antimicrobial resistance rate of H. pylori to clarithromycin is as high as 23.2 %. In addition, common mutations such as A2142C, A2142G, and A2143G were also observed. Other studies from Greek researchers report a resistance up to 27.7 %, while in the latest published study by Megraud et al24, using data from European countries, primary clarithromycin resistance in Greece was estimated to be 30 %. Studies derived from different European countries found similar resistant rates, ranging from 20.9 % (France) and 22.6 % (Bulgaria) to 27.4 % (Italy)25-28. These data are in accordance with the results of our study. A summary of all studies assessing H. pylori resistance rates to clarithromycin published from January 2020 until April 2021 (Table 3, Figure 2) demonstrate that high clarithromycin resistance rates are recognized as a current worldwide public health issue, mostly affecting Asian countries17,29-42.
Table 3. Recently published studies assessing Helicobacter pylori resistance to clarithromycin.
Figure 2. Forest plot depicting Helicobacter pylori resistance to clarithromycin as assessed in studies of Table 2. The square area and horizontal lines represent the study weight and the 95 % confidence interval of each rate as derived from the data of Table 2 studies.
Initial triple therapies for H. pylori included a combination of amoxicillin, clarithromycin, and PPI. Recently, the recommendations of Maastricht V/Florence consensus prohibit empirical triple therapies if clarithromycin resistance is above the threshold of 15-20 %43 unless a prior negative susceptibility test for clarithromycin resistance is available. However, in the clinical setting, eradication therapies under these rules remain difficult due to cost and technical requirements.
The use of real-time PCR made susceptibility testing more convenient and rapid to perform, allowing us to detect H. pylori and associated gene mutations responsible for clarithromycin resistance at the same time. Compared to standard methods used (culture and histopathologic examination), real-time PCR is faster and more accurate as it can also detect gene subpopulations. Our study found six patients harboring both wild type and mutant genes. This finding might be a reason for treatment eradication failure.
The most frequently reported genes responsible for resistance to clarithromycin are A2142C, A2142G, and A2143G in the 23S rRNA gene, although additional point mutations have also been described44,45. In our study, clarithromycin resistance was attributed to A2142G or A2143G in 17 out of 19 cases. Neither sex nor age was independently correlated with these clarithromycin resistance genes.
Our study is subject to some limitations. First, we did not perform a sample size calculation, but instead, we have included an equal number of patients as previous studies did. A larger number of patients enriched with demographic data might help us present more comprehensive results. Moreover, additional investigation utilizing DNA sequencing in our sample could be of assistance to further differentiate the responsible mutations. Finally, as there are no previous data from our region, we could not perform any analysis of variability in the local resistance rate.
In conclusion, our results show a high H. pylori resistance to clarithromycin in the Thrace region. These findings have important therapeutic implications and should guide local clinicians to treat H. pylori infection effectively. Moreover, as there is an increased tendency of clarithromycin resistance over the years21,42, surveillance is mandatory, and our results may form the basis for future studies.
Conflict of interest
Authors declare no conflicts of interest. This study received no financial support.
References
- 1.Hu Y, Zhang M, Lu B, Dai J. Helicobacter pylori and Antibiotic Resistance, A Continuing and Intractable Problem. Helicobacter. 2016;21:349–363. doi: 10.1111/hel.12299. [DOI] [PubMed] [Google Scholar]
- 2.Lauener FN, Imkamp F, Lehours P, Buissonnière A, Benejat L, Zbinden R, et al. Genetic Determinants and Prediction of Antibiotic Resistance Phenotypes in Helicobacter pylori. J Clin Med. 2019;8:53. doi: 10.3390/jcm8010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsumoto H, Shiotani A, Graham DY. Current and Future Treatment of Helicobacter pylori Infections. Adv Exp Med Biol. 2019;1149:211–225. doi: 10.1007/5584_2019_367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allahverdiyev AM, Bagirova M, Caliskan R, Tokman HB, Aliyeva H, Unal G, et al. Isolation and diagnosis of Helicobacter pylori by a new method: Microcapillary culture. World J Gastroenterol. 2015;21:2622–2628. doi: 10.3748/wjg.v21.i9.2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu Y, Zhu Y, Lu NH. Recent progress in Helicobacter pylori treatment. Chin Med J (Engl) 2020;133:335–343. doi: 10.1097/CM9.0000000000000618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Güven B, Gülerman F, Kaçmaz B. Helicobacter pylori resistance to clarithromycin and fluoroquinolones in a pediatric population in Turkey: A cross‐sectional study. Helicobacter. 2019;24:e12581. doi: 10.1111/hel.12581. [DOI] [PubMed] [Google Scholar]
- 7.Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon ATR, Bazzoli F, et al. Management of Helicobacter pylori infection--The Maastricht IV/ Florence Consensus Report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084. [DOI] [PubMed] [Google Scholar]
- 8.Wong F, Rayner-Hartley E, Byrne MF. Extraintestinal manifestations of Helicobacter pylori: a concise review. World J Gastroenterol. 2014;20:11950–11961. doi: 10.3748/wjg.v20.i34.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsigalou C, Konstantinidis TG, Cassimos D, Karvelas A, Grapsa A, Tsalkidis A, et al. Inverse association between Helicobacter pylori infection and childhood asthma in Greece: a case-control study. Germs. 2019;9:182–187. doi: 10.18683/germs.2019.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hao H, Yuan Z, Shen Z, Han J, Sahin O, Liu P, et al. Mutational and transcriptomic changes involved in the development of macrolide resistance in Campylobacter jejuni. Antimicrob Agents Chemother. 2013;57:1369–1378. doi: 10.1128/AAC.01927-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghotaslou R, Leylabadlo HE, Asl YM. Prevalence of antibiotic resistance in Helicobacter pylori: A recent literature review. World J Methodol. 2015;5:164–174. doi: 10.5662/wjm.v5.i3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alba C, Blanco A, Alarcón T. Antibiotic resistance in Helicobacter pylori. Curr Opin Infect Dis. 2017;30:489–497. doi: 10.1097/QCO.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 13.Bińkowska A, Biernat MM, Łaczmański Ł, Gościniak G. Molecular Patterns of Resistance Among Helicobacter pylori Strains in South-Western Poland. Front Microbiol. 2018;9:3154. doi: 10.3389/fmicb.2018.03154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hwang TJ, Kim N, Kim HB, Lee BH, Nam RH, Park JH, et al. Change in antibiotic resistance of Helicobacter pylori strains and the effect of A2143G point mutation of 23S rRNA on the eradication of H. pylori in a single center of Korea. J Clin Gastroenterol. 2010;44:536–543. doi: 10.1097/MCG.0b013e3181d04592. [DOI] [PubMed] [Google Scholar]
- 15.Khan R, Nahar S, Sultana J, Ahmad MM, Rahman M. T2182C mutation in 23S rRNA is associated with clarithromycin resistance in Helicobacter pylori isolates obtained in Bangladesh. Antimicrob Agents Chemother. 2004;48:3567–3569. doi: 10.1128/AAC.48.9.3567-3569.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mezmale L, Coelho LG, Bordin D, Leja M. Review: Epidemiology of Helicobacter pylori. Helicobacter. 2020;25 Suppl 1:e12734. doi: 10.1111/hel.12734. [DOI] [PubMed] [Google Scholar]
- 17.Uotani T, Graham DY. Diagnosis of Helicobacter pylori using the rapid urease test. Ann Transl Med. 2015;3:9. doi: 10.3978/j.issn.2305-5839.2014.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang YK, Kuo FC, Liu CJ, Wu MC, Shih HY, Wang SS, et al. Diagnosis of Helicobacter pylori infection: Current options and developments. World J Gastroenterol. 2015;21:11221–11235. doi: 10.3748/wjg.v21.i40.11221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bolor-Erdene M, Namdag B, Yamaoka Y, Jav S. Antibiotic resistance of Helicobacter pylori in Mongolia. J Infect Dev Ctries. 2017;11:887–894. doi: 10.3855/jidc.8619. [DOI] [PubMed] [Google Scholar]
- 20.Pohl D, Keller PM, Bordier V, Wagner K. Review of current diagnostic methods and advances in Helicobacter pylori diagnostics in the era of next generation sequencing. World J Gastroenterol. 2019;25:4629–4660. doi: 10.3748/wjg.v25.i32.4629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tonkic A, Vukovic J, Vrebalov Cindro P, Pesutic Pisac V, Tonkic M. Diagnosis of Helicobacter pylori infection : A short review. Wien Klin Wochenschr. 2018;130:530–534. doi: 10.1007/s00508-018-1356-6. [DOI] [PubMed] [Google Scholar]
- 22.Oleastro M, Ménard A, Santos A, Lamouliatte H, Monteiro L, Barthélémy P, et al. Real-time PCR assay for rapid and accurate detection of point mutations conferring resistance to clarithromycin in Helicobacter pylori. J Clin Microbiol. 2003;41:397–402. doi: 10.1128/JCM.41.1.397-402.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmitt BH, Regner M, Mangold KA, Thomson RB Jr, Kaul KL. PCR detection of clarithromycin-susceptible and -resistant Helicobacter pylori from formalin-fixed, paraffin-embedded gastric biopsies. Mod Pathol. 2013;26:1222–1227. doi: 10.1038/modpathol.2013.48. [DOI] [PubMed] [Google Scholar]
- 24.Megraud F, Bruyndonckx R, Coenen S, Wittkop L, Huang T-D, Hoebeke M, et al. Helicobacter pylori resistance to antibiotics in Europe in 2018 and its relationship to antibiotic consumption in the community . Gut. 2021;70:1815–1822. doi: 10.1136/gutjnl-2021-324032. [DOI] [PubMed] [Google Scholar]
- 25.Boyanova L, Gergova G, Markovska R, Kandilarov N, Davidkov L, Spassova Z, et al. Primary Helicobacter pylori resistance in elderly patients over 20 years: A Bulgarian study. Diagn Microbiol Infect Dis. 2017;88:264–267. doi: 10.1016/j.diagmicrobio.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Mégraud F, Alix C, Charron P, Bénéjat L, Ducournau A, Bessède E, et al. Survey of the antimicrobial resistance of Helicobacter pylori in France in 2018 and evolution during the previous 5 years. Helicobacter. 2021;26:e12767. doi: 10.1111/hel.12767. [DOI] [PubMed] [Google Scholar]
- 27.Losurdo G, Giorgio F, Pricci M, Girardi B, Russo F, Riezzo G, et al. Helicobacter pylori Primary and Secondary Genotypic Resistance to Clarithromycin and Levofloxacin Detection in Stools: A 4-Year Scenario in Southern Italy. Antibiotics. 2020;9:723. doi: 10.3390/antibiotics9100723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Georgopoulos S, Papastergiou V. An update on current and advancing pharmacotherapy options for the treatment H. pylori infection. Expert Opin Pharmacother. 2021;22:729–741. doi: 10.1080/14656566.2020.1845649. [DOI] [PubMed] [Google Scholar]
- 29.Li SY, Li J, Dong XH, Teng GG, Zhang W, Cheng H, et al. The effect of previous eradication failure on antibiotic resistance of Helicobacter pylori: A retrospective study over 8 years in Beijing. Helicobacter. 2021;26:e12804. doi: 10.1111/hel.12804. [DOI] [PubMed] [Google Scholar]
- 30.Lok CH, Zhu D, Wang J, Ren YT, Jiang X, Li SJ, et al. Phenotype and Molecular Detection of Clarithromycin and Levofloxacin Resistance in Helicobacter pylori Clinical Isolates in Beijing. Infect Drug Resist. 2020;13:2145–2153. doi: 10.2147/IDR.S249370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dang NQH, Ha TMT, Nguyen ST, Le NDK, Nguyen TMT, Nguyen TH, et al. High rates of clarithromycin and levofloxacin resistance of Helicobacter pylori in patients with chronic gastritis in the south east area of Vietnam. J Glob Antimicrob Resist. 2020;22:620–624. doi: 10.1016/j.jgar.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Aumpan N, Vilaichone RK, Gumnarai P, Sanglutong L, Ratanachu-Ek T, Mahachai V, et al. Prevalence and Antibiotic Resistance Patterns of Helicobacter pylori Infection in Koh Kong, Cambodia. Asian Pac J Cancer Prev. 2020;21:1409–1413. doi: 10.31557/APJCP.2020.21.5.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dumitru E, Alexandrescu L, Hanu AC, Tocia C, Cozaru GC, Mitroi AF, et al. Genetic Antibiotic Resistance of Helicobacter pylori in South-Eastern Romania. J Gastrointest Liver Dis. 2020;29:19–25. doi: 10.15403/jgld-758. [DOI] [PubMed] [Google Scholar]
- 34.Shoosanglertwijit R, Kamrat N, Werawatganon D, Chatsuwan T, Chaithongrat S, Rerknimitr R. Real-world data of Helicobacter pylori prevalence, eradication regimens, and antibiotic resistance in Thailand, 2013-2018. JGH Open. 2019;4:49–53. doi: 10.1002/jgh3.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Akar M, Aydin F, Kayman T, Abay S, Karakaya E. Detection of Helicobacter pylori by invasive tests in adult dyspeptic patients and antibacterial resistance to six antibiotics, including rifampicin in Turkey. Is clarithromycin resistance rate decreasing? Turk J Med Sci. 2021;51:1445–1464. doi: 10.3906/sag-2101-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Domanovich-Asor T, Motro Y, Khalfin B, Craddock HA, Peretz A, Moran-Gilad J. Genomic Analysis of Antimicrobial Resistance Genotype-to-Phenotype Agreement in Helicobacter pylori. Microorganisms. 2020;9:2. doi: 10.3390/microorganisms9010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Botija G, García Rodríguez C, Recio Linares A, Campelo Gutiérrez C, Pérez-Fernández E, Barrio Merino A. Resistencias antibióticas y tasas de erradicación en infección por Helicobacter pylori [Antibiotic resistances and eradication rates in Helicobacter pylori infection] An Pediatr (Engl Ed) 2020 doi: 10.1016/j.anpedi.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 38.Losurdo G, Giorgio F, Pricci M, Girardi B, Russo F, Riezzo G, et al. Helicobacter pylori rimary and Secondary Genotypic Resistance to Clarithromycin and Levofloxacin Detection in Stools: A 4-Year Scenario in Southern Italy. Antibiotics (Basel) 2020;9:723. doi: 10.3390/antibiotics9100723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bilgilier C, Thannesberger J, Ojeda Cisneros M, Boehnke K, Wu J, Xi C, et al. Antimicrobial Resistance of Helicobacter pylori in Gastric Biopsy Samples from Lima/Peru. Microb Drug Resist. 2021;27:951–955. doi: 10.1089/mdr.2020.0241. [DOI] [PubMed] [Google Scholar]
- 40.Biernat MM, Bińkowska A, Łaczmański Ł, Biernat P, Krzyżek P, Gościniak G. Phenotypic and Genotypic Analysis of Resistant Helicobacter pylori Strains Isolated from Children with Gastrointestinal Diseases. Diagnostics (Basel) 2020;10:759. doi: 10.3390/diagnostics10100759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park JY, Shin TS, Kim JH, Yoon HJ, Kim BJ, Kim JG. The Prevalence of Multidrug Resistance of Helicobacter pylori and Its Impact on Eradication in Korea from 2017 to 2019: A Single-Center Study. Antibiotics (Basel) 2020;9:646. doi: 10.3390/antibiotics9100646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang ZD, He BS, Zhang ZY, Wang SK, Ran D, Wang ZB. Analysis of the primary and post-treatment antibiotic resistance of Helicobacter pylori in Nanjing area. Curr Pharm Biotechnol. 2021;22:682–685. doi: 10.2174/1389201021666200722162613. [DOI] [PubMed] [Google Scholar]
- 43.Malfertheiner P, Megraud F, O’Morain C, Gisbert JP, Kuipers EJ, Axon AT, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66:6–30. doi: 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 44.Ng HK, Goh KL, Chuah KH, Thalha AM, Kee BP, Por LY, et al. Sequencing-based detection of 23S rRNA domain V mutations in treatment-naïve Helicobacter pylori patients from Malaysia. J Glob Antimicrob Resist. 2020;23:345–348. doi: 10.1016/j.jgar.2020.10.012. [DOI] [PubMed] [Google Scholar]
- 45.Abdollahi H, Savari M, Zahedi MJ, Moghadam SD, Hayatbakhsh Abasi M. Detection of A2142C, A2142G, and A2143G Mutations in 23s rRNA Gene Conferring Resistance to Clarithromycin among Helicobacter pylori isolates in Kerman, Iran. Iran J Med Sci. 2011;36:104–110. [PMC free article] [PubMed] [Google Scholar]