Abstract
Objectives
To compare the performance of four N95 respirator types with respect to quantitative fit test pass rate and health care worker‐rated usability and comfort.
Design, setting, participants
Health care workers who participated in the respiratory protection program at the Royal Melbourne Hospital, 1 October 2020 – 31 May 2021. Participants underwent quantitative N95 respirator fit testing (at least three of four types: semi‐rigid cup, flat‐fold cup, duckbill, and three‐panel flat‐fold types), and were invited to complete an online usability and comfort assessment for respirators for which their fit test results were passes.
Main outcome measures
Fit test pass rate, and user‐rated overall comfort and assessment ratings (five‐point Likert scales), by N95 respirator type.
Results
A total of 2161 health care workers underwent quantitative fit testing (women, 1586 [73.4%]; nurses, 1271 [58.8%]). The overall fit test pass rates were 65.0% for the semi‐rigid cup respirators (1029/1583 tests), 32.4% for the flat‐fold respirator (660/2035 tests), 59.2% for the duckbill respirators (2005/3387 tests), and 96.4% for the three‐panel flat‐fold respirator (1876/1946 tests). 378 health care workers completed the comfort and usability survey. Overall comfort and assessment ratings each differed by respirator group (P < 0.001); the median overall comfort (4; IQR, 3–4) and overall assessment values (4; IQR, 3–5) were highest for the three‐panel flat‐fold respirator and lowest for the semi‐rigid cup respirators (comfort: 2 [IQR, 1–3]; assessment: 2 [IQR, 2–3]).
Conclusions
The three‐panel flat‐fold N95 respirator outperformed the three alternative types with regard to fit test pass rate and user‐rated comfort and usability. To maximise respiratory protection for health care workers, these factors should be considered when making respirator procurement decisions.
Keywords: Prevention and control, Protective devices, Public health, Public policy, Respiratory tract infections, Infection control
The known: Assessing the fit test pass rate, usability, and comfort of N95 filtering facepiece respirators is not required for their certification, but can affect respirator fit, user compliance, and procurement decisions.
The new: The fit test pass rate was very high for three‐panel flat‐fold type N95 respirator (96%), and health care workers rated their comfort and overall usability higher than those of semi‐rigid cup, flat‐fold cup, and duckbill type N95 respirators.
The implications: Fit test results and performance evaluation by health care workers should be incorporated into respirator procurement decision making to ensure optimal respiratory protection.
Minimising the risk of exposure of health care workers to respiratory hazards is an essential infection control measure. 1 This is particularly important during the coronavirus disease 2019 (COVID‐19) pandemic given the high aerosol transmissibility of some severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) variants of concern, including the Delta and Omicron variants. 2 The Australian Infection Control Expert Group has published guidance on the use of personal protective equipment, 3 and some states have respiratory protection programs that include compulsory quantitative fit testing, with the aim of ensuring that health care workers wear properly fitted N95 filtering facepiece respirators. 4 , 5 However, health care workers often do not comply with recommendations for using respirators, particularly N95 respirators. 6 , 7 Explanations for non‐compliance include the lack of standardisation of donning and doffing techniques, and design features of respirators that reduce comfort and usability. 7 , 8 , 9 , 10
Respirators used in health care settings, as medical devices under the Commonwealth Therapeutic Goods Act 1989, must be included in the Australian Register of Therapeutic Goods. 11 Several types of N95 respirator have been registered, but assessing fit test pass rates, usability, and comfort is not required by the certification process. 8 , 12 , 13 A 2015 review of respirator literature 14 found only limited information on these characteristics, and only a few small studies have assessed comfort and usability. 10 , 15 , 16 , 17 , 18 Most found no significant differences in outcomes; in one study (27 volunteer participants), the duckbill type and respirators with exhalation valves were better tolerated than cup style respirators or respirators without exhalation valves. 18
As it is vital for effective protection that health care workers comply with recommendations for using respirators, the comfort and usability of N95 respirators are as important as their filtering efficiency and respirator fit. We therefore compared the performance of four common N95 respirator types in three domains: quantitative fit test pass rates, and usability and comfort as evaluated by health care workers participating in the respiratory protection program at the Royal Melbourne Hospital. Our aim was to provide performance data that can guide respirator model selection and procurement decisions.
Methods
We undertook our study within the respiratory protection program at the Royal Melbourne Hospital, a major Victorian tertiary hospital, during 1 October 2020 – 31 May 2021. The program, initiated by the Victorian government, was established in October 2020 in accordance with relevant Australian standards and guidelines. 4 , 19
Health care workers participating in the program completed a baseline survey (demographic data, professional information, preferred type of N95 respirator) and underwent online education in the safe use of four types of N95 respirator:
-
•
semi‐rigid cup type: cupped particulate respirator and surgical mask 1860 or 1860S (3M);
-
•
flat‐fold cup type: particulate respirator DE2322 (BYD Care);
-
•
duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard); and
-
•
three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M) (Supporting Information, part 1).
Participants were required to undergo quantitative fit testing with at least three N95 respirator types, as recommended by the Victorian Department of Health and Human Services guideline. 19 The order of respirator testing was determined by the director of the respiratory program, guided by health department advice regarding current and prospective supply.
Quantitative fit testing was performed by qualified testers using a PortaCount Pro+ 8048 fit tester (TSI) and according to United States Occupational Safety and Health Administration protocols, with four conventional exercises. 20 All male participants were clean‐shaven. The fit tester provided constructive feedback to each participant prior to the fit test to ensure the best seal, including position adjustment of the mask and guidance on moulding the nosepiece, and repeated the test if necessary. Fit factor is calculated by the PortaCount machine by dividing the concentration of particles in ambient air outside the respirator by that inside the respirator; 21 an overall fit factor exceeding 100 was deemed a pass. At the completion of fit testing, participants were given a result sheet that listed the fit test results (pass or fail) for each tested N95 respirator. The results and participants’ demographic and professional details were electronically stored in the hospital REDCap 10.5.2 system.
Four to six weeks after fit testing, participants were invited by email to complete an online REDCap survey on the usability and comfort of N95 respirators for which their fit test results were passes (development and validation: Supporting Information, part 2). The survey included three questions regarding usability (seal of mask, ease of donning and doffing, pass fit check success) and comfort (firmness of fit, breathability, eye irritation, skin irritation limiting use, anxiety limiting use, anatomic pressure areas). Participants were asked to provide overall comfort and overall assessment grades on a five‐point Likert scale (1, poor; 2, adequate; 3, good; 4, very good; 5, excellent) (Supporting Information, part 3). Participants were advised to undertake fit testing annually.
Statistical analysis
The statistical significance of group differences in demographic characteristics and fit test results was assessed in t (continuous data) or χ2 tests (categorical data). Group differences in usability and comfort assessment by N95 respirator type were assessed in χ2 tests. Overall comfort and assessment ratings of respirator types were each assessed in Friedman tests; P < 0.05 was deemed statistically significant. Each of the six possible pairs of N95 respirator types were then compared in post hoc Wilcoxon rank‐sum tests, with Bonferroni‐adjusted P < 0.01 deemed statistically significant. Analyses were conducted in Stata 13.
Free text comments in the online survey were categorised as positive (eg, good seal, comfortable), negative (eg, discomfort, skin reaction), or neutral (eg, unable to answer due to infrequent use), or as logistic problems (eg, availability).
Ethics approval
The study was approved by the Melbourne Health Human Research Ethics Committee (QA2020174).
Results
Quantitative fit test pass rate
Data for 2161 consecutive health care workers who underwent quantitative fit testing were collected over the eight‐month study period, including 1586 women (73.4%) and 1271 nurses (58.8%) (Box 1). The overall fit test pass rates were 65.0% for semi‐rigid cup respirators (1029 of 1583 tests), 32.4% for the flat‐fold cup respirator (660 of 2035 tests performed), 59.2% for duckbill respirators (2005 of 3387 tests), and 96.4% for the three‐panel flat‐fold respirator (1876 of 1946 tests). Pass rates were similar for men and women (data not shown), except for the semi‐rigid cup respirator (men, 281 of 376, 74.7%; women, 729 of 1179, 61.8%; P < 0.001).
Box 1. Baseline characteristics of the 2161 participants who underwent N95 respirator quantitative fit testing.
| Characteristic | All participants | Survey respondents* |
|---|---|---|
| Number of participants | 2161 | 378 |
| Age (years), mean (SD) | 39.0 (11.5) | 38.5 (10.8) |
| Sex | ||
| Men | 532 | 95 |
| Women | 1586 | 277 |
| Other | 6 | 1 |
| Missing data | 37 | 5 |
| Body mass index (kg/m2), mean (SD) | 24.5 (6.7) | 25.4 (7.0) |
| Ethnic background | ||
| European | 279 | 98 |
| Non‐European | 214 | 65 |
| Missing data | 1668 | 215 |
| Professional group | ||
| Medical practitioner | 305 (14.1%) | 64 (17%) |
| Nursing | 1271 (58.8%) | 228 (60.3%) |
| Allied health | 262 (12.1%) | 37 (9.8%) |
| Medical imaging | 29 (1.3%) | 7 (2%) |
| Other health care worker | 159 (7.4%) | 24 (6.3%) |
| Non‐clinical employee | 116 (5.4%) | 13 (3.4%) |
| Pharmacist | 14 (0.7%) | 0 |
| Dental professional | 1 (0.1%) | 1 (0.3%) |
| Missing data | 4 (0.2%) | 4 (1%) |
| Health care experience (years) | ||
| Median (IQR) | 10 (5–19) | 10 (6–20) |
| Range | 0.2–55 | 1–51 |
| Preferred N95 respirator type before participation in the program | ||
| Semi‐rigid cup | 151 (7.0%) | 21 (5.6%) |
| Flat‐fold cup | 171 (7.9%) | 37 (9.8%) |
| Duckbill | 1293 (59.8%) | 249 (65.6%) |
| Three‐panel flat‐fold | 173 (8.0%) | 36 (9.5%) |
| Other | 118 (5.5%) | 18 (4.8%) |
| Missing data | 255 (11.8%) | 17 (4.5%) |
IQR = interquartile range; SD = standard deviation.
Completed the usability and comfort assessment survey.
Usability and comfort survey
We assessed 714 respirator‐specific survey responses from 378 health care workers regarding comfort and usability (17.5% response rate), including 277 women (73.2%) and 228 nurses (60.3%). The only statistically significant difference in baseline characteristics was in mean body mass index (respondents, 25.4 kg/m2; standard deviation [SD], 7.0 kg/m2; non‐respondents, 24.3 kg/m2; SD, 6.6 kg/m2; P = 0.015) (Box 1).
Of the 714 responses, 192 referred to the semi‐rigid cup respirators (survey response rate, 19%), 66 the flat‐fold cup respirator (10%), 262 the duckbill respirators (13%), and 194 the three‐panel flat‐fold respirator (10%). Ninety‐four of 454 respondents who tested semi‐rigid cup or duckbill respirators (21%) required small rather than regular size versions. Most respondents (623 of 714, 87%) wore the evaluated N95 respirator fewer than five times a week during the study period; 250 (35%) wore it for two to four hours each time, and ten (1.4%) for more than four hours.
Usability was similar for the four respirator types, most respondents reporting that donning and doffing the respirator was easy (531, 74.4%) or somewhat difficult (164, 23.0%). Most respondents (645, 90.3%) reported they could pass the fit check every time or most of the time, with no differences by respirator type. Ten of 66 respondents (15%) reported poor seal with the semi‐rigid type, four of 66 (6%) with the flat‐fold type, one of 262 (0.5%) with the duckbill type, and one of 294 (0.3%) with the three‐panel flat‐fold type (Box 2).
Box 2. Ratings of usability and comfort of N95 respirators by 378 participants who completed the usability and comfort survey.
| N95 respirator type* | |||||
|---|---|---|---|---|---|
| Characteristic | Semi‐rigid cup | Flat‐fold cup | Duckbill |
Three‐panel flat‐fold |
P |
| Number of respondents | 192 | 66 | 262 | 194 | |
| Usability | |||||
| Ease of donning and doffing | 0.31 | ||||
| Easy | 134 (70%) | 48 (73%) | 201 (77%) | 148 (76%) | |
| Somewhat difficult | 51 (27%) | 18 (27%) | 53 (20%) | 42 (22%) | |
| Difficult | 6 (3%) | 0 | 5 (2%) | 2 (1%) | |
| Missing data | 1 (< 1%) | 0 | 3 (1%) | 2 (1%) | |
| Pass fit check | 0.02 | ||||
| Every time | 55 (29%) | 16 (24%) | 96 (37%) | 89 (46%) | |
| Most of the time | 111 (58%) | 45 (68%) | 140 (53%) | 93 (48%) | |
| Sometimes | 18 (9%) | 4 (6%) | 18 (7%) | 7 (4%) | |
| Rarely | 4 (2%) | 1 (2%) | 2 (< 1%) | 2 (1%) | |
| Never | 1 (< 1%) | 0 | 0 | 0 | |
| Missing data | 3 (2%) | 0 | 6 (2%) | 3 (2%) | |
| Seal | < 0.001 | ||||
| Excellent | 28 (15%) | 7 (11%) | 51 (20%) | 54 (28%) | |
| Very good | 57 (30%) | 23 (35%) | 86 (33%) | 76 (39%) | |
| Good | 54 (28%) | 16 (24%) | 78 (30%) | 52 (27%) | |
| Adequate | 42 (22%) | 16 (24%) | 43 (16%) | 10 (5%) | |
| Poor | 10 (5%) | 4 (6%) | 1 (< 1%) | 1 (< 1%) | |
| Missing data | 1 (< 1%) | 0 | 3 (1%) | 1 (< 1%) | |
| Comfort | |||||
| Firmness of fit | < 0.001 | ||||
| Too tight | 99 (52%) | 13 (20%) | 30 (12%) | 7 (4%) | |
| About right | 90 (47%) | 50 (76%) | 224 (86%) | 183 (94%) | |
| Too loose | 3 (2%) | 3 (4%) | 7 (3%) | 2 (1%) | |
| Missing data | 0 | 0 | 1 (< 1%) | 2 (1%) | |
| Breathability | < 0.001 | ||||
| Good | 35 (18%) | 25 (38%) | 138 (53%) | 133 (69%) | |
| Average | 111 (58%) | 39 (59%) | 113 (43%) | 57 (29%) | |
| Poor | 45 (23%) | 2 (3%) | 9 (3%) | 3 (2%) | |
| Missing data | 1 (< 1%) | 0 | 2 (< 1%) | 1 (< 1%) | |
Semi‐rigid cup type respirator: cupped particulate respirator and surgical mask 1860 or 1860S (3M); flat‐fold cup type: particulate respirator DE2322 (BYD Care); duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard); three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M).
Reported firmness of fit and breathability differed by respirator type; 99 of 192 respondents (52%) found the semi‐rigid cup respirators too tight and 45 (23%) rated their breathability as poor, while for 183 of 194 respondents (94%) the three‐panel flat‐fold respirators provided appropriate firmness of fit and 190 (98%) rated their breathability as average or good (Box 2).
The proportions of participants reporting effects that limit respirator use (eye irritation, skin irritation, anxiety) (Box 3) and of those who experienced pressure on their nose or cheeks (Box 4) were larger for the semi‐rigid and flat‐hold cup N95 types than for the other two types.
Box 3. Proportions of respondents who reported eye irritation, skin irritation, or and anxiety limiting respirator use, by N95 respirator type*.
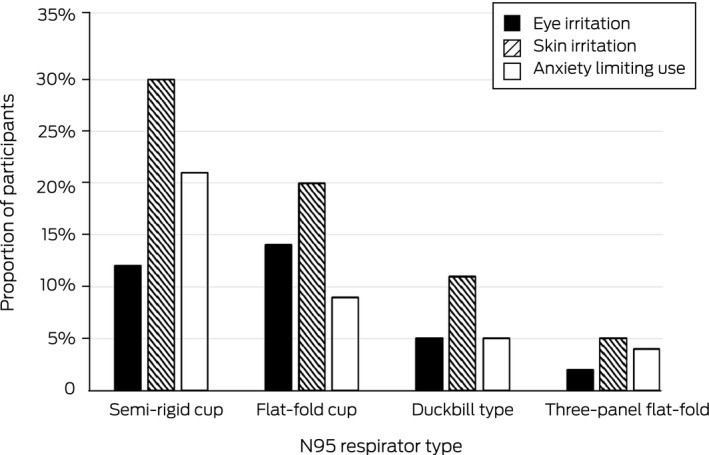
* Semi‐rigid cup type respirator: cupped particulate respirator and surgical mask 1860 or 1860S (3M) (192 respondents); flat‐fold cup type: particulate respirator DE2322 (BYD Care) (66 respondents); duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard) (262 respondents); three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M) (194 respondents).
Box 4. Proportions of respondents who reported pressure areas that limited duration of use of N95 respirators, by respirator type*.
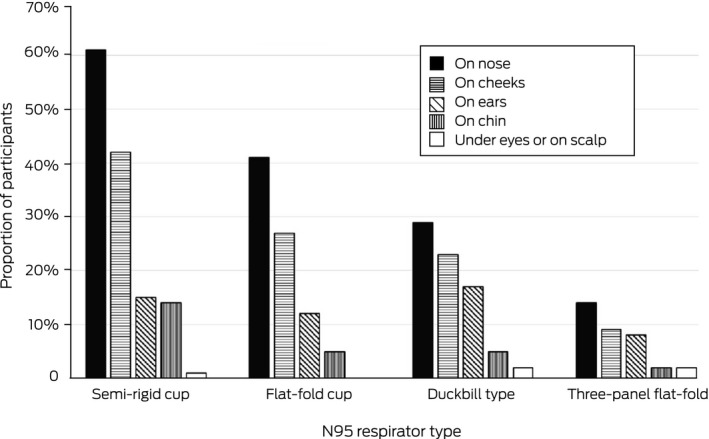
* Semi‐rigid cup type respirator: cupped particulate respirator and surgical mask 1860 or 1860S (3M) (192 respondents); flat‐fold cup type: particulate respirator DE2322 (BYD Care) (66 respondents); duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard) (262 respondents); three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M) (194 respondents).
Overall comfort and assessment ratings
The median overall comfort rating was 4 (interquartile range [IQR], 3–4) for the three‐panel flat‐fold style, 3 (IQR 2–4) for the duckbill style, 3 (IQR 2–3) for the flat‐fold cup style, and 2 (IQR, 1–3) for the semi‐rigid cup style (Box 5). Comfort rating scores for men and women were similar for all respirator types (data not shown).
Box 5. Overall comfort rating by respondents: violin plot, by N95 respirator type*.
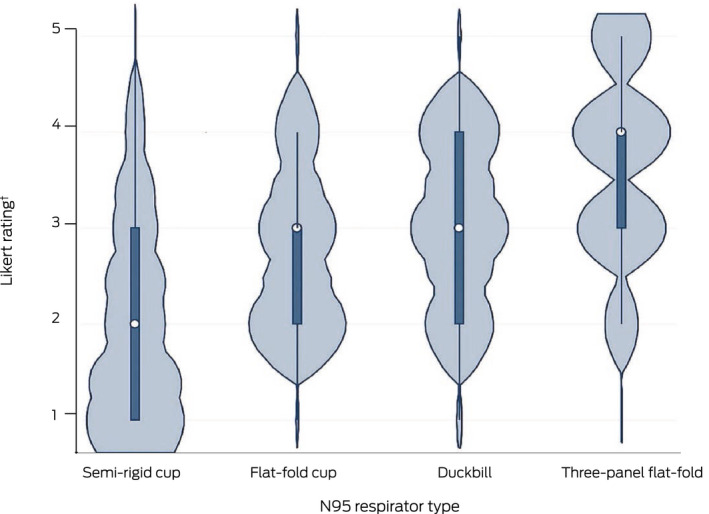
* Semi‐rigid cup type respirator: cupped particulate respirator and surgical mask 1860 or 1860S (3M) (192 respondents); flat‐fold cup type: particulate respirator DE2322 (BYD Care) (66 respondents); duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard) (262 respondents); three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M) (194 respondents).
† 1 = poor; 2 = adequate; 3 = good; 4 = very good; 5 = excellent.
The median overall assessment rating was 4 (IQR, 3–5) for the three‐panel flat‐fold style, 3 (IQR, 3–4) for the flat‐fold cup style, 3 (IQR, 3–4) for the duckbill style, and 2 (IQR, 2–3) for the semi‐rigid cup style (Box 6).
Box 6. Overall respirator assessment rating by respondents: violin plot, by N95 respirator type*.
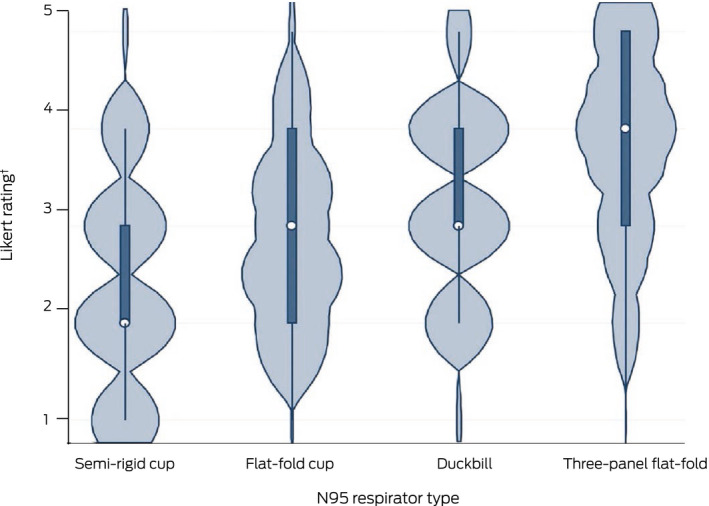
* Semi‐rigid cup type respirator: cupped particulate respirator and surgical mask 1860 or 1860S (3M) (192 respondents); flat‐fold cup type: particulate respirator DE2322 (BYD Care) (66 respondents); duckbill type: ProShield (BSN Medical) or Fluidshield surgical masks (Halyard) (262 respondents); three‐panel flat‐fold type: Aura 9320A+ particulate respirator (3M) (194 respondents).
† 1 = poor; 2 = adequate; 3 = good; 4 = very good; 5 = excellent.
The median values for overall comfort and assessment ratings differed by respirator type (each: P < 0.001). In post hoc tests, the three‐panel flat fold respirator was rated higher, and the semi‐rigid cup type respirators lower, than each of the other three types on both ratings.
Free text comments
We received a total of 89 free text comments in the 714 survey responses. The only respirator to receive more positive than negative comments was the three‐panel flat‐fold type. Twenty of the 28 respondents who commented on the semi‐rigid cup respirator provided negative comments (pain, discomfort, lack of breathability, skin reaction). Eleven participants noted that certain respirators were not always available, particularly small size and three‐panel flat‐fold respirators (Supporting Information, part 4).
Discussion
Our evaluation of four typical N95 respirator types was relatively large compared with similar studies. 14 We found that quantitative fit test pass rates differed by type, ranging from 32% for the flat‐fold cup type to 96% for the three‐panel flat‐fold respirator. The overall comfort and assessment ratings were lowest for the semi‐rigid cup style respirators and highest for the three‐panel flat‐fold respirator. Our findings are important for institutional respirator model selection and procurement, as both good respirator fit and compliance with recommended use are essential for maximising respiratory protection for health care workers.
Several studies have found that the ability to achieve a satisfactory seal is greater with three‐panel flat‐fold N95 respirators than with other styles. 14 , 22 , 23 In our study, the fit test pass rate was similarly highest for the three‐panel flat‐fold respirator, and overall comfort and overall assessment ratings by health care workers were higher than for the other types, although only 8% had preferred this mask type prior to the study. Taken together, these findings suggest that procurement of this N95 respirator type should be preferred.
Although the fit test pass rate for the semi‐rigid cup respirator was reasonable (65%), it received the lowest overall comfort and overall assessment ratings. The rigidity of the respirator cup, together with tightness of the strap, contribute to a satisfactory seal, but probably also to the discomfort experienced by many health care workers. 8 , 18 Half of the 192 respondents who commented on this feature found the respirator too tight, and almost one‐quarter that it made breathing difficult; 60% reported uncomfortable pressure on the nose and 40% on the cheek. Protective measures, such as a thin hydrocolloid dressing on the bridge of the nose across each cheekbone, might reduce skin injury and improve tolerability, but quantitative fit testing should then be undertaken with this dressing in place. 24
Project BREATHE was initiated by the United States Veterans Health Administration Office of Public Health and Environmental Hazards to improve compliance with recommendations for respiratory protective device use in health care. 8 , 25 Two of the four key themes to emerge were that respirators should perform their intended function safely and effectively, and that they should be comfortable and tolerable for the duration of wear. Most of the recommendations by Project BREATHE to improve compliance with appropriate use are still not considered by the respirator certification process. 8
Limitations
The assessment of usability and comfort in our study was subjective, as no validated objective tools or standardised criteria for this type of assessment are available. Unmeasured factors, such as perception of intelligible speech while wearing a respirator, may have influenced preferences. Second, we were unable to ask each participant to rate all four N95 respirator types. Third, the sample size for the usability and comfort assessment was relatively small for the flat‐fold cup type, the result of its lower fit check pass rate. Finally, we undertook our study during a period of relatively low N95 mask use, most participants wearing masks fewer than five times a week.
Conclusion
We found that the quantitative fit test pass rate for the three‐panel flat‐fold N95 respirator was very high (greater than 90%, as recommended by Project BREATHE), 8 , 25 and its overall comfort and overall assessment ratings by health care workers were higher than for than the semi‐rigid cup, flat‐fold cup, and duckbill types. The three‐panel flat‐fold N95 respirator type should therefore be preferred for health care workers. Further investigations based on large respiratory protection programs and the development of a standardised performance evaluation tool would be useful. To achieve maximum respiratory protection for our health care workers, respiratory protection program administrators and state and federal health departments should select and stockpile the most effective respirator models by incorporating clinical data into their decisions.
Open access
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
Competing interests
No relevant disclosures.
Data sharing
The de‐identified data underlying this report will be available from the corresponding author for five years from the publication date, as will the study protocol and statistical analysis.
Supporting information
Supplementary methods and results
Acknowledgements
We thank all the Royal Melbourne Hospital Respiratory Protection Program staff for their assistance with this study.
References
- 1. Centers for Disease Control and Prevention (USA) . The National Institute for Occupational Safety and Health (NIOSH). Hierarchy of controls. Updated Jan 2015. https://www.cdc.gov/niosh/topics/hierarchy (viewed Feb 2022).
- 2. World Health Organization . Infection prevention and control during health care when coronavirus disease (COVID‐19) is suspected or confirmed. Interim guidance. 12 July 2021. https://www.who.int/publications/i/item/WHO‐2019‐nCoV‐IPC‐2021.1 (viewed Feb 2022).
- 3. Australian Government Infection Control Expert Group . Guidance on the use of personal protective equipment (PPE) for health care workers in the context of COVID‐19. June 2021. https://www.health.gov.au/sites/default/files/documents/2021/06/guidance‐on‐the‐use‐of‐personal‐protective‐equipment‐ppe‐for‐health‐care‐workers‐in‐the‐context‐of‐covid‐19.pdf (viewed Feb 2022).
- 4. Department of Health and Human Services (Victoria) . COVID‐19 Victorian Respiratory Protection program guidelines; version 1.1. 25 Sept 2020. https://www.health.vic.gov.au/victorian‐respiratory‐protection‐program‐COVID‐19‐pdf (viewed Feb 2022).
- 5. Clinical Excellence Commission (New South Wales) . Respiratory protection program manual, version 1.0. Dec 2021. https://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0004/696712/Respiratory‐Protection‐Program‐Manual.pdf (viewed Feb 2022).
- 6. Honda H, Iwata K. Personal protective equipment and improving compliance among healthcare workers in high‐risk settings. Curr Opin Infect Dis 2016; 29: 400‐406. [DOI] [PubMed] [Google Scholar]
- 7. Fukakusa J, Rosenblat J, Jang B, et al. Factors influencing respirator use at work in respiratory patients. Occup Med (Lond) 2011; 61: 576‐582. [DOI] [PubMed] [Google Scholar]
- 8. Gosch ME, Shaffer ER, Eagan AE, et al. B95: a new respirator for health care personnel. Am J Infection Control 2013; 41: 1224‐1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baig AS, Knapp C, Eagan AE, Radonovich LJ. Health care workers’ views about respirator use and features that should be included in the next generation of respirators. Am J Infect Control 2010; 38: 18‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bryce E, Forrester L, Scharf S, Eshghpour M. What do healthcare workers think? A survey of facial protection equipment user preferences. J Hosp Infect 2008; 68: 241‐247. [DOI] [PubMed] [Google Scholar]
- 11. Australian Government . Therapeutic Goods Act 1989 (Act No. 21 of 1990). Federal Register of Legislation. Updated 27 Sept 2021. https://www.legislation.gov.au/Series/C2004A03952 (viewed Feb 2022). [Google Scholar]
- 12. Code of Federal Regulations . Approval of respiratory protective devices (42 CFR part 84). Updated 16 May 2022. https://www.ecfr.gov/current/title‐42/part‐84 (viewed May 2022).
- 13. Standards Australia . AS/NZS 1716‐2012: Respiratory protective devices. 2012. https://www.standards.org.au/standards‐catalogue/sa‐snz/publicsafety/sf‐010/as‐slash‐nzs‐‐1716‐2012 (viewed Feb 2022).
- 14. Shaffer RE, Janssen LL. Selecting models for a respiratory protection program: what can we learn from the scientific literature? Am J Infect Control 2015; 43: 127‐132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee K, Slavcev A, Nicas M. Respiratory protection against mycobacterium tuberculosis: quantitative fit test outcomes for five type N95 filtering‐facepiece respirators. J Occup Environ Hyg 2004; 1: 22‐28. [DOI] [PubMed] [Google Scholar]
- 16. Viscusi DJ, Bergman MS, Novak DA, et al. Impact of three biological decontamination methods on filtering facepiece respirator fit, odor, comfort, and donning ease. J Occup Environ Hyg 2011; 8: 426‐436. [DOI] [PubMed] [Google Scholar]
- 17. Shenal BV, Radonovich LJ, Cheng J, et al. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg 2012; 9: 59‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Radonovich LJ, Cheng J, Shenal BV, et al. Respirator tolerance in health care workers. JAMA 2009; 301: 36‐38. [DOI] [PubMed] [Google Scholar]
- 19. Department of Health and Human Services (Victoria) . COVID‐19 Respiratory Protection Program guidelines, version 1.1. Updated 25 Sept 2020. https://www.health.vic.gov.au/victorian‐respiratory‐protection‐program‐COVID‐19‐pdf (viewed Feb 2022).
- 20. Occupational Safety and Health Administration (United States Department of Labor) . Additional ambient aerosol CNC quantitative fit testing protocols: respiratory protection standard. Federal register 84: 50739‐50756. 26 Sept 2019. https://www.osha.gov/laws‐regs/federalregister/2019‐09‐26 (viewed Feb 2022).
- 21. TSI . PortaCount respirator fit tester models 8040 and 8048: operation/user manual (P/N 6010633, revision F). May 2021. https://tsi.com/getmedia/7d511812‐408e‐498f‐a611‐6f2561e3507b/PortaCount_8040_8048_Op_User_Mnl_6010633_US‐web?ext=.pdf (viewed May 2022).
- 22. Shin H, Oh J, Lim TH, et al. Comparing the protective performances of 3 types of N95 filtering facepiece respirators during chest compressions. Medicine (Baltimore) 2017; 96: e8308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lam SC, Lui AKF, Lee LYK, et al. Evaluation of the user seal check on gross leakage detection of 3 different designs of N95 filtering facepiece respirators. Am J Infect Control 2016; 44: 579‐586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ng I, Kave B, Begg F, et al. Impact on quantitative fit test results after application of prophylactic hydrocolloid dressing under N95 respirators. Infect Control Hosp Epidemiol 2021; 10.1017/ice.2021.293 [online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Office of Public Health and Environmental Hazards (US Veterans Health Administration) . Better respiratory equipment using advanced technologies for healthcare employees (Project BREATHE). A report of an interagency working group of the US Federal Government. 2009. https://www.cdc.gov/niosh/npptl/hospresptoolkit/pdfs/ProjectBREATHE‐final‐report‐508.pdf (viewed Feb 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary methods and results


