Abstract
Recent studies have highlighted high levels of emotional eating during the coronavirus (COVID‐19) pandemic, but have not satisfactorily explained these changing eating patterns. Here, we tested one potential explanatory model broadly based on a biosocial model of emotional eating. Specifically, we examined the extent to which negative emotional reactivity was associated with emotional eating, as well as the mediating role of fear of COVID‐19. A total of 474 women from Romania were asked to complete measures of emotional eating, negative emotional reactivity, and fear of COVID‐19. Mediation analysis showed that higher negative emotional reactivity was significantly and directly associated with greater emotional eating. This direct relationship was also mediated by fear of COVID‐19. These results highlight one possible route through which the ongoing COVID‐19 pandemic may have resulted in elevated rates of emotional eating, though further research is needed.
Keywords: Emotional eating, COVID‐19, emotional reactivity, eating behavior, anxiety
INTRODUCTION
Beyond the threat to physical health, the novel coronavirus (COVID‐19) pandemic has had a profound impact on lifestyles and daily routines in populations worldwide (Haleem, Javaid & Vaishya, 2020). For instance, many countries have introduced travel restrictions, mandatory self‐quarantine, periods of lockdown or social distancing, and the closure of non‐essential services (e.g., bars, gyms, and salons). Such measures have the potential to stop or limit the spread of COVID‐19 (Barnett‐Howell, Watson & Mobarak, 2021; Tian, Liu, Li et al., 2020), but have also triggered profound challenges in finances, educational opportunities, employment, and lifestyles resulting in high levels of stress and anxiety (Shevlin, McBride, Murphy et al., 2020; Tull, Edmonds, Scamaldo, Richmond, Rose & Gratz, 2020) particularly in at‐risk population segments, such as pregnant women (Biviá‐Roig, La Rosa, Gómez‐Tébar et al., 2020). In addition, emerging research has shown that the stress and anxiety triggered by the COVID‐19 pandemic – and attendant changes to daily routines, such as increased screen‐time and decreased physical activity (Cooper, Reilly, Siegel et al., 2020; Rodgers, Lombardo, Cerolini et al., 2020) – has also had adverse effects on other aspects of psychological well‐being, including negative body image (Swami, Horne & Furnham, 2020; Swami, Todd, Robinson & Furnham, 2021) and unhealthy eating patterns (Ashby, 2020; Flaudias, Iceta, Zerhouni et al., 2020; Phillipou, Meyer, Neill et al., 2020; Pujia, Ferro, Maurotti et al., 2021; Robertson, Duffy, Newman, Bravo, Ates & Sharpe, 2020).
In particular, it has been suggested that the negative affect caused by the COVID‐19 pandemic may impede coping mechanisms and amplify maladaptive coping strategies (Rettie & Daniels, 2021). One such maladaptive coping strategy involves emotional eating, defined as food consumption in response to negative emotions (Kaplan & Kaplan, 1957). More specifically, emotional eating represents a failure to discriminate internal hunger cues from the desire to use eating – particularly consumption of energy‐dense, high‐sugar foods – as a strategy for regulating and reducing negative emotions (Bruch, 1973; Evers, Marijn Stok & de Ridder, 2010). Indeed, recent studies have documented a shift toward unhealthy eating patterns (Ammar, Brach, Trabelsi et al., 2020; Sidor & Rzymski, 2020) and high rates of emotional eating in adults from a range of national contexts during the COVID‐19 pandemic (Bemanian, Mæland, Blomhoff et al., 2021; Cecchetto, Aiello, Gentili, Ionta & Osimo, 2021; Giacalone, Frøst & Rodríguez‐Pérez, 2020; Mason, Barrington‐Trimis & Leventhal, 2021; Papandreou, Arija, Aretouli, Tsilidis & Bulló, 2020). For instance, one survey of Saudi women reported that more than half of respondents reported moderate or high levels of emotional eating (Al‐Musharaf, 2020), whereas more than half of Italian adults surveyed reported that they had increased their food intake to manage their anxiety (Di Renzo, Gualtieri, Cinelli et al., 2020).
These findings are concerning because emotional eating is reliably associated with weight gain and long‐term weight retention (van Strien, Konttinen, Homberg, Engels & Winkens, 2016), a finding that has been supported during the ongoing pandemic (Mason et al., 2021). To date, however, most studies on the impact of the COVID‐19 pandemic have been concerned with estimating rates of emotional eating in different social identity groups (e.g., Al‐Musharaf, 2020; Mason et al., 2021; Papandreou et al., 2020) with women in particular identified as being at higher risk for emotional eating (Di Renzo et al., 2020; Giacalone et al., 2020). In contrast, relatively little work has sought to identify potential mechanistic pathways that may explain higher rates of emotional eating during the COVID‐19 pandemic. Of note, it has been suggested that stricter lockdown measures may be related to higher rates of emotional eating (Papandreou et al., 2020), which implies a central role for COVID‐19‐related negative affect (see also Cecchetto et al., 2021; McAtamney, Mantzios, Egan & Wallis, 2021). Consistent with this proposition, one recent study found that perceived stress during the pandemic was significantly associated with greater emotional eating among adults in the United States (Shen, Long, Shih & Ludy, 2020).
However, more work could be done to better understand the pathways that lead to emotional eating during the COVID‐19 pandemic. Emotional reactivity is one factor that may be particularly important in this regard. Emotional reactivity refers to an emotional response to a stimulus, which varies across individuals and also by ease of activation, intensity, and duration (Davidson, 1998; Rothbart & Derrberry, 1981). According to the biosocial model (Linehan, 1993), negative emotional reactivity – or the tendency to demonstrate maladaptive responses to emotional events – results from an interaction between biologically‐based propensities toward high emotional reactivity and childhood invalidation. This biosocial model has historically been applied to models of disordered eating (Wisniewski & Kelly, 2003), but has recently been extended to understandings of emotional eating (Braden, Anderson, Redondo, Watford, Emley & Ferrell, 2021). Thus, it has been shown that individuals who have greater negative emotional reactivity were more likely to engage in emotional eating (Barnhart, Braden & Jordan, 2020; Braden et al., 2021). In explanation, it has been suggested that emotional eating may be a strategy to cope with and manage emotional discomfort (Braden et al., 2021).
While a direct link between negative emotional reactivity and emotional eating appears likely, this relationship may also be mediated by specific emotional responses to the COVID‐19 pandemic. For instance, initial cross‐sectional work has shown that fear of COVID‐19 is particularly high in adults and that greater levels of COVID‐19 fear are associated with higher levels of anxiety and symptoms of depression (Ahorsu, Lin, Imani, Saffari, Griffiths & Pakpour, 2020; Fitzpatrick, Harris & Drawve, 2020). Additionally, greater fear of COVID‐19 has been associated with higher levels of emotional eating during the pandemic (Pak, Süsen, Denizci Nazlıgül & Griffiths, 2021). This is consistent with earlier studies showing that catastrophising and anxiety are associated with greater emotional eating (Janke, Jones, Hopkins, Ruggieri & Hruska, 2016; Zysberg, 2018) and that, in the context of the current pandemic specifically, fear of COVID‐19 is associated with more negative health behaviors (Nguyen, Do, Pham et al., 2020). Likewise, individuals higher in negative emotional reactivity may also be more likely to express greater fear of COVID‐19, although this has not been specifically investigated.
In the present study, therefore, we sought to advance understandings of emotional eating during the COVID‐19 pandemic by testing a novel explanatory model in Romanian women. Specifically, we expected that greater negative emotional reactivity would be significantly and directly associated with greater emotional eating, which is consistent with previous work (Braden et al., 2021). Additionally, we hypothesised that fear of COVID‐19 would mediate the relationship between negative emotional reactivity and emotional eating, which would be consistent with – and extend – the findings of Pak et al. (2021). A graphical depiction of our hypothesised model is provided in Fig. 1. Should our hypotheses be supported, it would point to one possible mechanistic pathway that explains elevated rates of emotional eating during the ongoing COVID‐19 pandemic.
Fig. 1.
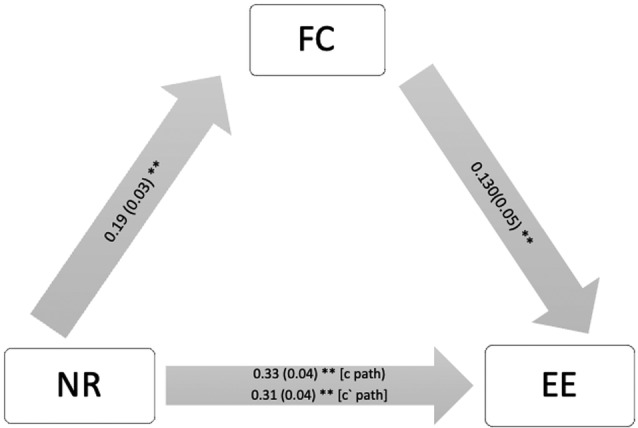
Mediation model of the relationship between negative emotional reactivity (NR) and emotional eating (EE) via fear of COVID‐19 (FC).
METHOD
Participants
The initial pool of participants included 614 women, but we excluded individuals who self‐reported an eating disorder diagnosis (n = 28) and who failed attention check items (n = 112). The final pool of participants, therefore, included 474 women ranging in age from 18 to 40 years (M = 22.91, SD = 4.36) and in self‐reported body mass index (BMI) from 14.34 to 43.28 kg/m2 (M = 22.21, SD = 4.92). All participants were citizens and residents of Romania, and the majority (67.9%) indicated that they were residing in an urban area. In terms of educational qualifications, 50.4% had completed secondary schooling, 2.3% had a post‐secondary qualification, 36.3% had an undergraduate degree, and the remainder had a postgraduate degree.
Measures
Emotional reactivity
To measure negative emotional reactivity, we used the General Negative Reactivity (GNR) subscale of the Perth Emotional Reactivity Scale (PERS; Becerra, Preece, Campitelli & Scott‐Pillow, 2019). This subscale consists of 15 items measuring the activation, intensity, and duration (five items each) of one's negative emotions. All items were rated on a five‐point scale ranging from 1 (very unlike me) to 5 (very like me). Although the GNR can be scored as three subscales (Becerra et al., 2019), an exploratory factor analysis (EFA) with data from the present study indicated that a single, composite factor consisting of all 15 items should be extracted (see Data S1). Therefore, we computed an overall score as the mean of all 15 GNR items, with higher scores reflecting more negative emotional reactivity. Internal consistency, as measured using McDonald's ω, was 0.92 (95% CI = 0.91, 0.93).
Emotional eating
Emotional eating was assessed using the Emotional Eating Scale–Revised (Koball, Meers, Storfer‐Isser, Domoff & Musher‐Eizenman, 2012), a 31‐item instrument measuring the desire to eat in response to anxiety or anger, depression, and boredom. All items were rated on a five‐point scale ranging from 1 (no desire to eat) to 5 (an overwhelming desire to eat). Scores on the English version of the scale have been found to reduce to three dimensions (Koball et al., 2012), but score dimensionality has not been previously assessed on a Romanian translation of the scale. Therefore, we subjected scores from the present study to EFA. The results of parallel analysis indicated that a single factor, consisting of 19 items, should be retained (see Data S1). Thus, we computed an overall score as the mean of the 19 relevant items, with higher scores reflecting a greater desire to eat emotionally. McDonald's ω for this overall score was 0.95 (95% CI = 0.94, 0.95).
Fear of COVID‐19
To measure fear of COVID‐19, participants were asked to complete the Fear of COVID‐19 scale (FC‐19S; Ahorsu et al., 2020). This is a seven‐item scale that measures the intensity of fear one has toward COVID‐19. All items were rated on a five‐point scale ranging from 1 (strongly disagree) to 5 (strongly agree). An EFA of the FC‐19S scores from the present indicated that a single factor with all seven items should be extracted (see Data S1). Therefore, we computed an overall score as the mean of all seven items, with higher scores indicating greater fear of COVID‐19. Internal consistency, as measured using McDonald's ω, was 0.84 (95% CI = 0.81, 0.86).
Demographics
Participants were asked to self‐report their age, area of residence (urban or rural), highest educational qualification, self‐reported diagnosis of an eating disorder, height, and weight. Height and weight data were used to compute self‐reported BMI as kg/m2.
Procedures
Ethics approval for this project was obtained from the institutional research committee of the Faculty of Psychology and Education Sciences and all research was conducted in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Because Romanian translations of all survey instruments were not available at the time of study, we prepared novel translations using the back‐translation method (Brislin, 1970). Between September and October 2020, the study was advertised to potential participants via social media. Inclusion criteria included being a Romanian citizen and resident of adult age, and we excluded participants who had a self‐reported diagnosis of an eating disorder. Eligible participants were asked to provide digital informed consent before being asked to complete an online survey, designed and implemented in accordance with best‐practice recommendations for online surveys (Eysenbach, 2004). The survey was hosted on Google Forms and consisted of the measures described above, presented in a counter‐balanced order for each participant. IP addresses were examined to ensure that no participant took the survey more than once. The anonymous survey also included three attention check items inserted part‐way through. Participation was voluntary and, in exchange for completing the survey, participants were eligible for entry into a prize raffle worth 50 RON. All participants received debriefing information upon completion of the survey.
RESULTS
Preliminary analyses
There were no missing data in the retained dataset. Descriptive statistics and inter‐scale correlations between all study variables are reported in Table 1. As can be seen, scores on all variables were significantly and positively correlated, with small‐to‐medium effect sizes. Regression analyses indicated that negative emotional reactivity significantly predicted fear of COVID‐19, F(1, 473) = 26.39, p < 0.001, Adj. R 2 = 0.05, β = 0.23, and emotional eating, F(1, 473) = 58.90, p < 0.001, Adj. R 2 = 0.11, β = 0.33, whereas fear of COVID‐19 significantly predicted emotional eating, F(1,473) = 17.91, p < 0.001, Adj. R 2 = 0.04, β = 0.19.
Table 1.
Means, standard deviations, and correlations between all study variables
| M | SD | (1) | (2) | (3) | |
|---|---|---|---|---|---|
| (1) Negative emotional reactivity | 3.36 | 0.86 | 0.23* | 0.31* | |
| (2) Fear of COVID‐19 | 1.99 | 0.74 | 0.17* | ||
| (3) Emotional eating | 1.11 | 0.93 |
Note: N = 474.
p < 0.001.
Mediation analysis
We used the bootstrap approach (Hayes, 2017) to conduct mediation analyses (Model 4) based on the hypothesised model depicted in Fig. 1. The bootstrap method does not require normal sampling distribution and has a better balance of Type I error and statistical power than alternative methods (MacKinnon, Lockwood & Williams, 2004; Shrout & Bolger, 2002). As recommended by Preacher and Hayes (2008), 5,000 bootstrap samples were drawn from the dataset to calculate indirect and direct effects, as well as bias‐corrected 95% CIs. Effects were considered to be significant if a respective CI did not overlap zero (MacKinnon et al., 2004). As shown in Fig. 1, there were significant direct effects for all pathways in the model. There was also a significant indirect pathway from negative emotional reactivity to emotional eating via fear of COVID‐19, (indirect effect = 0.02, SE = 0.01, 95% CI = 0.01, 0.51, 7.7% of total effect). These results remained unchanged when BMI was entered as a covariate in the mediation model.
DISCUSSION
A growing body of recent work has highlighted high rates of emotional eating in adults from a wide range of national contexts during the ongoing COVID‐19 pandemic (e.g., Al‐Musharaf, 2020; Bemanian et al., 2021; Cecchetto et al., 2021; Di Renzo et al., 2020; Giacalone et al., 2020; Mason et al., 2021; Papandreou et al., 2020). With few exceptions (e.g., Cecchetto et al., 2021; McAtamney et al., 2021; Papandreou et al., 2020; Shen et al., 2020), the extant research has not attempted to explicate mechanistic and explanatory pathways that may account for high rates of emotional eating during the pandemic. Here, we tested one potential explanatory model: specifically, we examined whether negative emotional reactivity would be associated with emotional eating both directly and indirectly via fear of COVID‐19. Consistent with our hypothesising, we found that more negative emotional reactivity was significantly associated with greater emotional eating. In addition, we also found that fear of COVID‐19 mediated the relationship between negative emotional reactivity and emotional eating.
Consistent with recent work (Barnhart et al., 2020; Braden et al., 2021), we found that greater negative emotional reactivity was significantly and directly associated with greater emotional eating. This finding is consistent with Linehan's (1993) biosocial model, which suggests that emotional regulation difficulties are associated with behavioral outcomes. More specifically, both our findings and those of other researchers (Barnhart et al., 2020; Braden et al., 2021) suggest that individuals who experience easily activated, intense, and more persistent negative emotions are more likely to experience stronger patterns of emotional eating. It may be that individuals high in negative emotional reactivity have few effective emotion regulation strategies (Messerli‐Bürgy, Stülb, Kakebeeke et al., 2018; Steinsbekk, Barker, Llewellyn, Fildes & Wichstrøm, 2018). Faced with persistent negative affect, these individuals may adopt maladaptive behavioral strategies, such as emotional eating, to manage their emotional states. In this sense, emotional eating may provide individuals high in negative emotional reactivity with a means of reasserting a degree of control over their emotions through eating.
Beyond this direct pathway, however, we also found that higher negative emotional reactivity was significantly associated with greater fear of COVID‐19, which in turn was significantly associated with greater emotional eating. In broad outline, this finding is consistent with the suggestion that fear of COVID‐19 is significantly associated with greater emotional eating (Pak et al., 2021), as well as with earlier findings. In terms of the latter, perceived stress, financial strain, and loneliness – all factors that are likely related to fear of COVID‐19 (Ahorsu et al., 2020; Fitzpatrick et al., 2020) – are related to higher emotional eating (Mason, 2020; Mason, Heron, Braitman & Lewis, 2016; Mason & Lewis, 2014; Spinosa, Christiansen, Dickson, Lorenzetti & Hardman, 2019). It is possible, therefore, that individuals who are high in negative emotional reactivity are more likely to develop intense fear toward COVID‐19. In turn, these feelings of fear serve as a further trigger for emotional eating, possibly as a means of regulating or alleviating those feelings of fear. That is, we suggest that, for some individuals, emotional eating may be a maladaptive coping strategy for dealing with the intense feelings of fear triggered by COVID‐19.
Our findings are important, first, because they suggest one possible route through which the COVID‐19 pandemic leads to high rates of emotional eating. Of course, we do not suggest it is the only such route (Cecchetto et al., 2021; McAtamney et al., 2021; Shen et al., 2020); indeed, it may not even be the primary route. However, in the absence of further research, our findings point to potentially important roles played by negative emotional reactivity and fear of COVID‐19 in emotional eating. This is notable because it highlights the impact that the ongoing pandemic may be having on overeating and unhealthy food intake, which could in turn lead to incidental weight gain and negative body image (Swami et al., 2020, 2021). That is, many individuals may be engaging in emotional eating to cope with the fear and anxiety caused by the COVID‐19 pandemic, which in turn could bring downstream negative outcomes that exacerbate and perpetuate poorer psychological outcomes, including symptoms of disordered eating. For instance, psychosocial stressors during the pandemic could increase disordered eating symptomatology by elevating psychological distress (Ramalho et al., 2021) or by promoting unhealthy weight control behaviors, including mindless eating and snacking, increased food consumption, and eating to cope with distress (Simone et al., 2021). In a similar vein, the psychosocial impact of the COVID‐19 pandemic may also include an uptick in addictive behaviors (e.g., more frequent alcohol consumption), which in turn may affect eating patterns either directly or via increased psychological distress (see La Rosa, Gori, Faraci, Vicario & Craparo, 2021).
Our study is not without its limitations. First, because of the dearth of appropriate, psychometrically‐validated tools for use with Romanian‐speaking samples – an issue recognised by scholars (e.g., Swami, Tudorel, Goian, Barron & Vintila, 2017; Vintilă, Todd, Goian, Tudorel, Barbat & Swami, 2020), we relied on EFAs to assess the factorial validity of the instruments included in the present study. In the case of the PERS‐GNR and FC19‐S, our results broadly supported score dimensionality observed with English‐speaking samples. In the case of the EES‐R, however, the results of our EFA suggested that emotional eating in our sample should be conceptualised as a unidimensional construct. Although this is consistent with other recent work suggesting that eating‐related instruments developed for use in English‐speaking samples may not transfer well to Romanian contexts (Vintilă et al., 2020), it nevertheless limits opportunities to examine the extent to which our results are robust across eating in response to different forms of negative emotions, such as anger and boredom. Further, although EFA is a robust method for assessing factorial validity (Swami & Barron, 2019), it would be useful for future work to establish further evidence of factorial validity (e.g., through confirmatory factor analysis) and other psychometric properties. Additionally, although our analytic plans did not change from the point of designing our study through to its execution, it should be noted that our study plan and hypotheses were not preregistered.
Second, due to our recruitment method, caution should be exercised when attempting to generalise our findings to the broader Romanian population. Indeed, Romania is notable for large inter and intra‐regional differences in factors such as socioeconomic status, educational outcomes, urban–rural residence, exercise and eating habits, and the prevalence of overweight and obesity (Vintilă et al., 2020). As such, it would be useful for future work to recruit a representative sample of Romanian adults and to request further demographic information that would enable more in‐depth examinations of subgroups that may be at heightened risk for emotional eating. In a similar vein, given that our study was limited to Romanian adults, it may not be possible to generalise our findings to other national contexts. Indeed, given differences in the transmission of COVID‐19 and in national responses to the threat posed by the coronavirus, it will be important to replicate our findings in other national contexts.
There are additional ways in which the present work could be extended. For instance, it may be useful to examine the impact of positive emotional reactivity on emotional eating (Barnhart et al., 2020), as well as the mediating role of COVID‐19‐related stress and anxiety (Swami et al., 2020), as separate constructs to fear of COVID‐19. Finally, given the cross‐sectional nature of our study, causal inferences should be applied with caution and future work should approach this topic using experimental and longitudinal designs. The above limitations and directions for future research notwithstanding, our findings suggest a possible explanatory model that accounts for high rates of emotional eating during the COVID‐19 pandemic. From a practical point‐of‐view, helping individuals to develop adaptive emotion regulation skills and to enhance strategies to manage COVID‐19‐related fear may be beneficial to reduce emotional eating.
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee of Alexandru Ioan Cuza University and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Supporting information
Data S1. Supplementary Materials
Section Editor: Mia O'Toole
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Ahorsu, D.K. , Lin, C.Y. , Imani, V. , Saffari, M. , Griffiths, M.D. & Pakpour, A.H. (2020). The fear of COVID‐19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 1–9. 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Musharaf, S. (2020). Prevalence and predictors of emotional eating among healthy young Saudi women during the COVID‐19 pandemic. Nutrients, 12, 2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammar, A. , Brach, M. , Trabelsi, K. , Chtourou, H. , Boukhris, O. , Masmoudi, L. et al. (2020). Effects of COVID‐19 home confinement on eating behavior and physical activity: Results of the ECLB‐COVID‐19 international online survey. Nutrients, 12, 1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashby, N.J. (2020). Impact of the COVID‐19 pandemic on unhealthy eating in populations with obesity. Obesity (Silver Spring, Md), 28, 1802–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett‐Howell, Z. , Watson, O.J. & Mobarak, A.M. (2021). The benefits and costs of social distancing in high‐ and low‐income countries. Transactions of the Royal Society of Tropical Medicine and Hygiene, 115, 807–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnhart, W.R. , Braden, A.L. & Jordan, A.K. (2020). Negative and positive emotional eating uniquely interact with ease of activation, intensity, and duration of emotional reactivity to predict increased binge eating. Appetite, 151, 104688. [DOI] [PubMed] [Google Scholar]
- Becerra, R. , Preece, D. , Campitelli, G. & Scott‐Pillow, G. (2019). The assessment of emotional reactivity across negative and positive emotions: Development and validation of the Perth Emotional Reactivity Scale (PERS). Assessment, 26, 867–879. 10.1177/1073191117694455 [DOI] [PubMed] [Google Scholar]
- Bemanian, M. , Mæland, S. , Blomhoff, R. , Rabben, Å.K. , Arnesen, E.K. , Skogen, J.C. et al. (2021). Emotional eating in relation to worries and psychological distress amid the COVID‐19 pandemic: A population‐based survey on adults in Norway. International Journal of Environmental Research and Public Health, 18, 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biviá‐Roig, G. , La Rosa, V.L. , Gómez‐Tébar, M. , Serrano‐Raya, L. , Amer‐Cuenca, J.J. , Caruso, S. et al. (2020). Analysis of the impact of the confinement resulting from COVID‐19 on the lifestyle and psychological wellbeing of Spanish pregnant women: An internet‐based cross‐sectional survey. International Journal of Environmental Research and Public Health, 17, 5933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braden, A. , Anderson, L. , Redondo, R. , Watford, T. , Emley, E. & Ferrell, E. (2021). Emotion regulation mediates relationships between perceived childhood invalidation, emotional reactivity, and emotional eating. Journal of Health Psychology, 26, 2937–2949. [DOI] [PubMed] [Google Scholar]
- Brislin, R.W. (1970). Back‐translation for cross‐cultural research. Journal of Cross‐Cultural Psychology, 1, 185–216. [Google Scholar]
- Bruch, H. (1973). Eating disorders: Obesity, anorexia nervosa, and the person within. New York: Basic Books. [Google Scholar]
- Cecchetto, C. , Aiello, M. , Gentili, C. , Ionta, S. & Osimo, S.A. (2021). Increased emotional eating during COVID‐19 associated with lockdown, psychological and social distress. Appetite, 160, 105122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, M. , Reilly, E.E. , Siegel, J.A. , Coniglio, K. , Sadeh‐Sharvit, S. , Pisetsky, E. et al. (2020). Eating disorders during the COVID‐19 pandemic: An overview of risks and recommendations for treatment and early intervention. Eating Disorders, 30, 54–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, R.J. (1998). Affective style and affective disorders: Perspectives from affective neuroscience. Cognition & Emotion, 12, 307–330. [Google Scholar]
- Di Renzo, L. , Gualtieri, P. , Cinelli, G. , Bigioni, G. , Soldati, L. , Attinà, A. et al. (2020). Psychological aspects and eating habits during COVID‐19 home confinement: Results of EHLC‐COVID‐19 Italian online survey. Nutrients, 12, 2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers, C. , Marijn Stok, F. & de Ridder, D.T. (2010). Feeding your feelings: Emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin, 36, 792–804. [DOI] [PubMed] [Google Scholar]
- Eysenbach, G. (2004). Improving the quality of web surveys: The checklist for reporting results of internet E‐surveys (CHERRIES). Journal of Medical Internet Research, 6, e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick, K.M. , Harris, C. & Drawve, G. (2020). Fear of COVID‐19 and the mental health consequences in America. Psychological Trauma, 12(S1), S17–S21. [DOI] [PubMed] [Google Scholar]
- Flaudias, V. , Iceta, S. , Zerhouni, O. , Rodgers, R.F. , Billieux, J. , Llorca, P.M. et al. (2020). COVID‐19 pandemic lockdown and problematic eating behaviors in a student population. Journal of Behavioral Addictions, 9, 826–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giacalone, D. , Frøst, M.B. & Rodríguez‐Pérez, C. (2020). Reported changes in dietary habits during the COVID‐19 lockdown in the Danish population: The Danish COVIDiet study. Frontiers in Nutrition, 7, 592112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haleem, A. , Javaid, M. & Vaishya, R. (2020). Effects of COVID‐19 pandemic in daily life. Current Medicine Reasesrch and Practice, 10, 78–79. 10.1016/j.cmrp.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A.F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. New York, Guilford Press. [Google Scholar]
- Janke, E.A. , Jones, E. , Hopkins, C.M. , Ruggieri, M. & Hruska, A. (2016). Catastrophizing and anxiety sensitivity mediate the relationship between persistent pain and emotional eating. Appetite, 103, 64–71. [DOI] [PubMed] [Google Scholar]
- Kaplan, H.I. & Kaplan, H.S. (1957). The psychosomatic concept of obesity. Journal of Nervous and Mental Disease, 125, 181–201. [DOI] [PubMed] [Google Scholar]
- Koball, A.M. , Meers, M.R. , Storfer‐Isser, A. , Domoff, S.E. & Musher‐Eizenman, D.R. (2012). Eating when bored: Revision of the Emotional Eating Scale with a focus on boredom. Health Psychology, 31, 521–524. [DOI] [PubMed] [Google Scholar]
- La Rosa, V.L. , Gori, A. , Faraci, P. , Vicario, C.M. & Craparo, G. (2021). Traumatic distress, alexithymia, dissociation, and risk of addiction during the first wave of COVID‐19 in Italy: Results from a cross‐sectional online survey on a non‐clinical adult sample. International Journal of Mental Health and Addiction, 1–17. Advance online publication. 10.1007/s11469-021-00569-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan, M.M. (1993). Skills training manual for treating borderline personality disorder. New York: Guilford Press. [Google Scholar]
- MacKinnon, D.P. , Lockwood, C.M. & Williams, J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, T.B. (2020). Loneliness, eating, and body mass index in parent–adolescent dyads from the family life, activity, sun, health, and eating study. Personal Relationships, 27, 420–432. [Google Scholar]
- Mason, T.B. , Barrington‐Trimis, J. & Leventhal, A.M. (2021). Eating to cope with the COVID‐19 pandemic and body weight change in young adults. Journal of Adolescent Health, 68, 277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, T.B. , Heron, K.E. , Braitman, A.L. & Lewis, R.J. (2016). A daily diary study of perceived social isolation, dietary restraint, and negative affect in binge eating. Appetite, 97, 94–100. [DOI] [PubMed] [Google Scholar]
- Mason, T.B. & Lewis, J.R. (2014). Profiles of binge eating: The interaction of depressive symptoms, eating styles, and body mass index. Eating Disorders, 22, 450–460. [DOI] [PubMed] [Google Scholar]
- McAtamney, K. , Mantzios, M. , Egan, H. & Wallis, D.J. (2021). Emotional eating during COVID‐19 in the United Kingdom: Exploring the roles of alexithymia and emotional dysregulation. Appetite, 161, 105120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messerli‐Bürgy, N. , Stülb, K. , Kakebeeke, T.H. , Arhab, A. , Zysset, A.E. , Leeger‐Aschmann, C.S. et al. (2018). Emotional eating is related with temperament but not with stress biomarkers in preschool children. Appetite, 120, 256–264. [DOI] [PubMed] [Google Scholar]
- Nguyen, H.T. , Do, B.N. , Pham, K.M. , Kim, G.B. , Dam, H.T. , Nguyen, T.T. et al. (2020). Fear of COVID‐19 scale: Associations of its scores with health literacy and health‐related behaviors among medical students. International Journal of Environmental Research and Public Health, 17, 4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pak, H. , Süsen, Y. , Denizci Nazlıgül, M. & Griffiths, M. (2021). The mediating effects of fear of COVID‐19 and depression on the association between intolerance of uncertainty and emotional eating during the COVID‐19 pandemic in Turkey. International Journal of Mental Health and Addiction, 1–15. Advance online publication. 10.1007/s11469-021-00489-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papandreou, C. , Arija, V. , Aretouli, E. , Tsilidis, K.K. & Bulló, M. (2020). Comparing eating behaviors, and symptoms of depression and anxiety between Spain and Greece during the COVID‐19 outbreak: Cross‐sectional analysis of two different confinement strategies. European Eating Disorders Review, 28, 836–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipou, A. , Meyer, D. , Neill, E. , Tan, E.J. , Toh, W.L. , Van Rheenen, T.E. et al. (2020). Eating and exercise behaviors in eating disorders and the general population during the COVID‐19 pandemic in Australia: Initial results from the COLLATE project. International Journal of Eating Disorders, 53, 1158–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K.J. & Hayes, A.F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Pujia, R. , Ferro, Y. , Maurotti, S. , Khoory, J. , Gazzaruso, C. , Pujia, A. et al. (2021). The effects of COVID‐19 on the eating habits of children and adolescents in Italy: A pilot survey study. Nutrients, 13, 2641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramalho, S.M. , Trovisqueira, A. , de Lourdes, M. , Gonçalves, S. , Ribeiro, I. , Vaz, A.R. et al. (2021). The impact of COVID‐19 lockdown on disordered eating behaviors: The mediation role of psychological distress. Eating and Weight Disorders: EWD, 27, 179–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rettie, H. & Daniels, J. (2021). Coping and tolerance of uncertainty: Predictors and mediators of mental health during the COVID‐19 pandemic. American Psychologist, 76, 427–437. [DOI] [PubMed] [Google Scholar]
- Robertson, M. , Duffy, F. , Newman, E. , Bravo, C.P. , Ates, H.H. & Sharpe, H. (2020). Exploring changes in body image, eating and exercise during the COVID‐19 lockdown: A UKsurvey. Appetite, 159, 105062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R.F. , Lombardo, C. , Cerolini, S. , Franko, D.L. , Omori, M. , Fuller‐Tyszkiewicz, M. et al. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53, 1166–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart, M.K. & Derrberry, D. (1981). Development of individual differences in temperament. In Lamb M.E. & Brown A.L. (Eds.), Advances in developmental psychology (pp. 37–86). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Shen, W. , Long, L.M. , Shih, C.H. & Ludy, M.J. (2020). A humanities‐based explanation for the effects of emotional eating and perceived stress on food choice motives during the COVID‐19 pandemic. Nutrients, 12, 2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, M. , McBride, O. , Murphy, J. , Miller, J.G. , Hartman, T.K. , Levita, L. et al. (2020). Anxiety, depression, traumatic stress and COVID‐19 related anxiety in the UK general population during the COVID‐19 pandemic. BJPsych Open, 6, e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout, P.E. & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7, 422–445. [PubMed] [Google Scholar]
- Sidor, A. & Rzymski, P. (2020). Dietary choices and habits during COVID‐19 lockdown: Experience from Poland. Nutrients, 12, 1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simone, M. , Emery, R.L. , Hazzard, V.M. , Eisenberg, M.E. , Larson, N. & Neumark‐Sztainer, D. (2021). Disordered eating in a population‐based sample of young adults during the COVID‐19 outbreak. International Journal of Eating Disorders, 54, 1189–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinosa, J. , Christiansen, P. , Dickson, J.M. , Lorenzetti, V. & Hardman, C.A. (2019). From socioeconomic disadvantage to obesity: The mediating role of psychological distress and emotional eating. Obesity (Silver Spring, MD), 27, 559–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinsbekk, S. , Barker, E.D. , Llewellyn, C. , Fildes, A. & Wichstrøm, L. (2018). Emotional feeding and emotional eating: Reciprocal processes and the influence of negative affectivity. Child Development, 89, 1234–1246. [DOI] [PubMed] [Google Scholar]
- Swami, V. & Barron, D. (2019). Translation and validation of body image instruments: Challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image, 31, 204–220. [DOI] [PubMed] [Google Scholar]
- Swami, V. , Horne, G. & Furnham, A. (2020). COVID‐19‐related stress and anxiety are associated with negative body image in adults from the United Kingdom. Personality and Individual Differences, 170, 110426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swami, V. , Todd, J. , Robinson, C. & Furnham, A. (2021). Self‐compassion mediates the relationship between COVID‐19‐related stress and body image disturbance: Evidence from the United Kingdom under lockdown. Personality and Individual Differences, 183, 11130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swami, V. , Tudorel, O. , Goian, C. , Barron, D. & Vintila, M. (2017). Factor structure and psychometric properties of a Romanian translation of the Body Appreciation Scale‐2. Body Image, 23, 61–68. [DOI] [PubMed] [Google Scholar]
- Tian, H. , Liu, Y. , Li, Y. , Wu, C.H. , Chen, B. , Kraemer, M.U. et al. (2020). An investigation of transmission control measures during the first 50 days of the COVID‐19 epidemic in China. Science, 368, 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull, M.T. , Edmonds, K.A. , Scamaldo, K. , Richmond, J.R. , Rose, J.P. & Gratz, K.L. (2020). Psychological outcomes associated with stay‐at‐home orders and the perceived impact of COVID‐19 on daily life. Psychiatry Research, 289, 113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien, T. , Konttinen, H. , Homberg, J.R. , Engels, R.C. & Winkens, L.H. (2016). Emotional eating as a mediator between depression and weight gain. Appetite, 100, 216–224. [DOI] [PubMed] [Google Scholar]
- Vintilă, M. , Todd, J. , Goian, C. , Tudorel, O. , Barbat, C.A. & Swami, V. (2020). The Romanian version of the Intuitive Eating Scale‐2: Assessment of its psychometric properties and gender invariance in Romanian adults. Body Image, 35, 225–236. [DOI] [PubMed] [Google Scholar]
- Wisniewski, L. & Kelly, E. (2003). The application of dialectical behavior therapy to the treatment of eating disorders. Cognitive and Behavioral Practice, 10, 131–138. [Google Scholar]
- Zysberg, L. (2018). Emotional intelligence, anxiety, and emotional eating: A deeper insight into a recently reported association? Eating Behaviors, 29, 128–131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


