Abstract
Background
During the COVID‐19 pandemic, health care provider well‐being was affected by various challenges in the work environment. The purpose of this study was to evaluate the relationship between the perceived work environment and mental well‐being of a sample of emergency physicians (EPs), emergency medicine (EM) nurses, and emergency medical services (EMS) providers during the pandemic.
Methods
We surveyed attending EPs, resident EPs, EM nurses, and EMS providers from 10 academic sites across the United States. We used latent class analysis (LCA) to estimate the effect of the perceived work environment on screening positive for depression/anxiety and burnout controlling for respondent characteristics. We tested possible predictors in the multivariate regression models and included the predictors that were significant in the final model.
Results
Our final sample included 701 emergency health care workers. Almost 23% of respondents screened positive for depression/anxiety and 39.7% for burnout. Nurses were significantly more likely to screen positive for depression/anxiety (adjusted odds ratio [aOR] 2.04, 95% confidence interval [CI] 1.11–3.86) and burnout (aOR 2.05, 95% CI 1.22–3.49) compared to attendings. The LCA analysis identified four subgroups of our respondents that differed in their responses to the work environment questions. These groups were identified as Work Environment Risk Group 1, an overall good work environment; Risk Group 2, inadequate resources; Risk Group 3, lack of perceived organizational support; and Risk Group 4, an overall poor work environment. Participants in the two groups who perceived their work conditions as most adverse were significantly more likely to screen positive for depression/anxiety (aOR 1.89, 95% CI 1.05–3.42; and aOR 2.04, 95% CI 1.14–3.66) compared to participants working in environments perceived as less adverse.
Conclusions
We found a strong association between a perceived adverse working environment and poor mental health, particularly when organizational support was deemed inadequate. Targeted strategies to promote better perceptions of the workplace are needed.
INTRODUCTION
As health care organizations went into crisis mode during the COVID‐19 pandemic, employee health and safety were jeopardized. Health care workers (HCWs) faced limited availability of personal protective equipment (PPE), inadequate infection control practices, and staffing shortages. 1 , 2 , 3 They worked in environments that were unsafe for themselves and their patients. 1 , 2 , 3 In addition to the physical threat of exposure to COVID‐19, there was the emotional toll of worrying about transmitting the illness to loved ones. 4 Emergency HCWs faced unprecedented rates of anxiety, depression, and burnout. 5 , 6 , 7 , 8
While lack of available resources may have contributed to these adverse mental health outcomes, the relationship between perceived working conditions and mental health is likely more complex. Workers who perceive a more positive working environment can potentially mitigate the role of low resources on stress, while perceptions of a less supportive working environment may exacerbate this association. Prior studies acknowledge the role of these factors individually in contributing to HCW stress during the pandemic, but do not attempt to evaluate the relationship or direction of effects of these factors in concert. 6 , 9 , 10 , 11 , 12
The purpose of this study was to evaluate the relationship between the perceived work environment and mental well‐being of a sample of emergency physicians (EPs), emergency medicine (EM) nurses, and emergency medical services (EMS) providers during the COVID‐19 pandemic. Our study is unique because we used latent class analysis (LCA) to examine the association between the perceived working environment on workplace stress as a mediator causing depression, anxiety, and burnout. We explored both positive and negative factors that affect mental health outcomes. We hypothesized that perceived adverse working conditions would be associated with a high proportion of emergency HCWs screening positive for depression, anxiety, and burnout and this would largely be attributable to job stress, but that a positive organizational culture would help offset this relationship. We also hypothesized that EM nurses would report the poorest mental health due to extended patient contact.
METHODS
Study design
We conducted a cross‐sectional survey at 10 academic emergency departments (EDs) across the United States to evaluate the impact of perceived workplace conditions on the mental health of emergency HCWs during the COVID‐19 pandemic. The study was part of a larger mixed‐methods study. From November 19, 2020, to December 31, 2020, we surveyed EPs, EM nurses, and EMS providers across the 10 sites using a questionnaire that measured perceived workplace conditions and psychological distress as well as factors that influence the relationship. The institutional review board (IRB) of the principal investigator (PI) in Washington, DC, approved the study and acted as the IRB of record for all 10 sites.
Study setting and sample
The 10 academic sites varied in terms of geographic location, hospital size, and confirmed COVID‐19 cases in their county/city at the time of selection in June 2020 (range 388 cases/100,000–2690 cases/100,000). 13 The sites were Birmingham (Alabama); Dallas (Texas); Detroit (Michigan); Fulton County (Georgia); Los Angeles (California); New Orleans (Louisiana); New York City (New York); Omaha (Nebraska); Providence (Rhode Island); and Washington, DC. We aimed to survey 15 attending EPs, 15 resident EPs, 20 EM nurses, and 15 EMS providers at each site for a total of 650 participants, given our budget and with as little selection bias as possible. To do this, the principal collaborator at each site sent the PI an email list with the contact information of all EPs, residents, and nurses working at the site. The statistician for the project randomly selected 20 full‐time EM attendings, 20 EM residents, and 27 full‐time nurses from each site's master list; we assumed a 75% response rate.
The PI sent an email via Redcap to all those randomly selected, inviting them to participate. The email included a hyperlink to a Redcap survey and written consent that was implied by the completion of the survey. The survey took approximately 10 min to complete and all respondents who completed the survey received a $10 Amazon gift card. The survey was anonymous; however, it was designed to track the participation rate by site and provider type. This made it possible to resend the survey link to non‐responders without being able to specifically identify them. We resent the survey to nonresponders a maximum of five times before we randomly selected a second batch of participants according to the provider response rate at each site until we reached the target sample size.
Survey
Guided by the conceptual framework we developed to evaluate the influence of perceived working conditions during the COVID‐19 pandemic on the health of emergency HCWs (see Figure S1), we designed the survey to measure the following: (1) worker demographic and job characteristics; (2) workplace conditions and organizational factors; (3) mental health and well‐being; (4) job stress; and (5) perceived handling of the pandemic by the public, government, and news/social media. We reviewed the survey with our entire investigative team and piloted it on five HCWs who were not included in the final sample to test for comprehension and usability.
A copy of the survey is included in Figure S2. In addition, a summary of the scales and questions we included in the survey and how we categorized them for analysis can be found in Table S1. A brief summary of the survey components follows and Table S1 details how we measured each construct (i.e., validated scale or self‐designed question), the number of items, and how we treated them in the analysis.
The first section of the survey measured background information of the respondent, their family, and their job. For example, we asked each participant about their marital status, how many people they lived with, whether they had primary childcare responsibilities, and whether they or a family member were at risk of COVID‐19 complications. We also asked respondents how long they had been working in their current profession, whether they worked a fixed or rotating schedule, and how many hours they worked per shift.
The second section of the survey measured perceived workplace conditions and organizational factors that influence the work environment using scales developed by the National Institute of Occupational Safety and Health 14 or by Maunder and colleagues 15 during the SARS epidemic. Respondents rated the adequacy of infection control training and PPE. 15 We used an organizational support scale that asked about employer appreciation, with employee well‐being taken into account, availability of emotional support services at work, and supportive workplace as well as other scales that measured whether specific types of people at work were supportive (i.e., organizational leadership, supervisor, and colleagues). 14 , 15 We also asked participants whether they had experienced any reductions in pay, benefits, or staffing.
The third section of the survey measured mental health outcomes including our primary outcomes: depression and anxiety. We used the four‐item Patient Health Questionnaire for Anxiety and Depression (PHQ‐4) and categorized respondents as positive for depression/anxiety if their score was ≥6 (moderate to severe). 16 We assessed our secondary outcome, burnout, with a single item measure. 17 We defined burnout as a score of 4 or greater which indicates that the participant reported feeling burnout at least once per week. We also asked respondents about specific sources of anxiety, including ability to pay their bills, perceived effects of the public health response to COVID‐19, of the community not adhering to public health guidelines, and of misinformation by the news or social media so that we could control for these sources of anxiety when evaluating the influence of working conditions on depression/anxiety and burnout. 18
Finally, the survey also included scales and questions that we hypothesized may act as possible mediators or moderators of the relationship between working conditions and mental health. More specifically, we included a 5‐item job stress scale so that we could evaluate whether job stress acts as a mediator between working conditions and mental health. 19
To control for the possibility that survey responses may be influenced by COVID‐19 transmission rates in their community at the time of survey administration, we created two variables that reflected whether the community was in a COVID‐19 surge during the period of survey administration as well as how many days had lapsed between the community's first major COVID‐19 peak and survey administration. 13
Statistical analysis
The analysis was conducted in five phases. First, we examined the relationship among the items that measured perceived working conditions and the organizational factors that influence them. The majority of the conditions were measured using a single item with a dichotomous response option (i.e., yes or no) and the few that were not were dichotomized as above or below the sample mean (see Table S1). For each condition, a value of 1 represents a more adverse state. Among the 16 working conditions, missing data were minimal (i.e., <2%). We used multiple imputation by chained equations (MICE) and assumed missing at random to impute the missing dichotomous values for each item. For each pair of working conditions, we computed a log odds ratio (OR; and the corresponding OR) to measure the strength of the association. All bivariate analyses were corrected for the multiple comparisons we made using the Bonferroni correction method. 20
Second, because of the moderate to strong association among many of the workplace conditions, we used LCA to identify distinct work environment risk groups. Rather than examine each workplace condition in isolation, we used LCA to identify a finite number of subgroups of our cohort with similar response profiles to the workplace condition questions. We estimated LCA models with C = 3–6 classes. We estimated the Akaike information criterion (AIC) and Bayesian information criteria (BIC) for each C to evaluate the different class model solutions. We also examined the model diagnostics, including class size, entropy, and average latent class posterior probability. After we identified the work environment risk groups, we evaluated the relationship between each perceived workplace condition and perceived work environment risk group using a chi‐square test of homogeneity.
Third, we examined the percent distribution of respondent characteristics, perceived work environment risk group, and community COVID‐19 status at time of survey on depression/anxiety and burnout using a chi‐square test of homogeneity for categorical variables and ANOVA for continuous variables.
Fourth, we separately estimated the effect of the perceived work environment on screening positive for depression/anxiety and burnout controlling for respondent characteristics, community COVID‐19 status, and site. We tested all possible predictors in the multivariate logistic regression models and included the predictors that were significant in the final models (p ≤ 0.05).
Finally, we evaluated the extent to which job stress acted as an atemporal mediator between the perceived work environment and the two mental health outcomes. In other words, could the relationship between the perceived work environment and depression/anxiety and burnout be explained by job stress? To do this, we estimated the mediating effect of job stress by subtracting the difference in the regression coefficients of the perceived work environment risk groups of the model that did (direct effect) from the model that did not include job stress (total effect) and dividing the difference by the total perceived work environment risk group effect. We used the bootstrap method to estimate the 95% confidence intervals (CIs) for the mediation effect estimates.
RESULTS
For all EMS providers at the 10 sites and EM nurses at two sites, the site principal collaborators distributed flyers to recruit respondents because a master email list was not available. Of the 802 surveys completed, 701 were eligible after excluding duplicates or surveys with missing job title information. The average response rates for EM attendings, residents, and nurses were 73%, 80%, and 75%, respectively (the nurse response rate excludes the two sites where we used recruitment flyers). The average response rate across the 10 sites was 77% with a range of 51%–91% (excluding EMS providers at all sites and the nurses at the two sites that used flyers).
The mean (±SD) age of the 701 emergency HCWs in our sample was 35 (±10) years old (see Table 1). The sample was almost equally represented by sex (52% male) and one‐third of respondents were Black, Hispanic, Asian, or other race. On average, the participants reported working in their current profession for 8 years (SD ±8) and 21% reported they had been infected by COVID‐19. Attending EM physicians were the least likely to report being infected by COVID‐19 (13%) compared to the other emergency HCWs (21%–24%). Job stress was highest among the nurses (mean 3.7) and EMS providers (mean 3.5) compared to the attendings (mean 3.2) and residents (mean 3.1).
TABLE 1.
Percent distribution of selected respondent characteristics and work environment risk class by type of emergency HCW
| Characteristic | Overall, N = 701 | Emergency HCW | |||
|---|---|---|---|---|---|
| Attending, n = 159 | Resident, n = 169 | Nurse, n = 221 | EMS, n = 152 | ||
| Respondent characteristics | |||||
| Age (years)* | 35.3 (±9.7) | 42.2 (±9.3) | 29.7 (±4.3) | 34.9 (±10.1) | 34.8 (±9.7) |
| Male gender* | 364 (52) | 99 (62) | 105 (62) | 50 (23) | 110 (72) |
| Race* | |||||
| Non‐Hispanic White | 470 (67) | 121 (76) | 113 (67) | 142 (64) | 94 (62) |
| Non‐Hispanic Black | 65 (9) | 12 (8) | 16 (9) | 18 (8) | 19 (13) |
| Hispanic | 46 (7) | 4 (3) | 2 (1) | 19 (9) | 21 (14) |
| Asian | 71 (10) | 17 (11) | 23 (14) | 25 (11) | 6 (4) |
| Other | 48 (7) | 5 (3) | 15 (9) | 17 (8) | 11 (7%) |
| Years in profession* | 8.3 (±8.2) | 12.7 (±8.4) | 2.6 (±3.1) | 8.2 (±8.3) | 10.2 (±8.3) |
| Lives alone | 149 (21) | 23 (14) | 50 (30) | 46 (21) | 30 (20) |
| Infected by COVID‐19 | 144 (21) | 20 (13) | 41 (24) | 46 (21) | 37 (24) |
| Perceived work environment | |||||
| Work environment risk class* | |||||
| Class 1 (overall good work environment) | 283 (40) | 82 (52) | 88 (52) | 56 (25) | 57 (38) |
| Class 2 (inadequate resources) | 159 (23) | 36 (23) | 37 (22) | 48 (22) | 38 (25) |
| Class 3 (lack of organizational support) | 124 (18) | 24 (15) | 25 (15) | 51 (23) | 24 (16) |
| Class 4 (poor work environment) | 135 (19) | 17 (11) | 19 (11) | 66 (30) | 33 (22) |
| Job stress* | 3.4 (±0.8) | 3.2 (±0.8) | 3.1 (±0.7) | 3.7 (±0.7) | 3.5 (±0.8) |
Note: Data are reported as mean (±SD) or n (%).
Abbreviation: HCW, health care worker.
p < 0.00625 after Bonferroni correction for all the comparisons.
Many of the perceived workplace conditions were strongly associated with one another (see Figure S3). For example, there was a strong association between an unsupportive workplace and no mental health resources offered by the employer (OR 8.2, 95% CI 5.3–12.8). The employer not taking employee well‐being into account was strongly correlated with work life not made easier by administration (OR 6.8, 95% CI 4.6–10.2), supervisor (OR 7.9, 95% CI 5.2–12.2), and colleagues (OR 8.5, 95% CI 5.7–12.8). There was also a strong relationship between the perception of inadequate infection control training and the perception of no protective equipment available (OR 9.3, 95% CI 5.8–15.1). Decrease in pay and decrease in benefits were significantly related to one another (OR 10.0, 95% CI 5.9–17.1) but not to the majority of the other workplace condition variables.
The LCA identified subgroups of our respondents that differed in their responses to the perceived work environment questions (see Table S2). The BIC identified a four‐class model, the AIC suggested a six‐class model but the smallest class size was too small (4%). Because the four‐class model also had good model fit and the four groups differentiated themselves well, we selected the four‐class model solution. The prevalence of perceived adverse working conditions differed significantly across the four perceived work environment risk groups (see Table S3).
Figure 1 displays the four perceived work environment risk groups identified by the LCA using a radar chart. Work Environment Risk Group 1, an overall good work environment, includes 40% of our sample (depicted in light green). Less than 10% of participants in this group reported a poor physical environment, inadequate training, or insufficient protective equipment. They reported satisfaction with all aspects of organizational support (i.e., appreciated by employers, mental health resources available) and with the social support of their colleagues and supervisor. The single major complaint in this group was 64% reported that their work life was not made easier by their administration. While this is high in Risk Group 1, it is meaningfully lower than the other risk groups (range 91%–96%).
FIGURE 1.
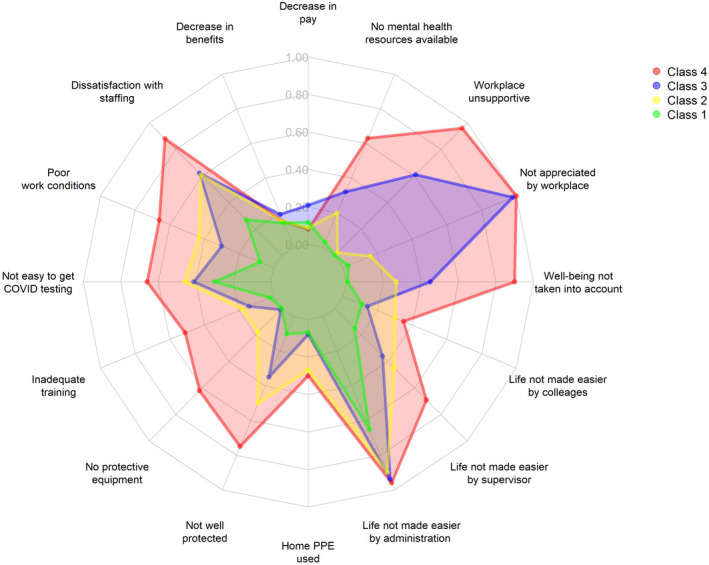
Radar chart displaying the four perceived work environment risk groups by each perceived workplace condition. The four perceived work environment risk groups identified by LCA display different typologies across the 16 perceived workplace conditions. LCA, latent class analysis; PPE, personal protective equipment.
Risk Group 2, inadequate resources (depicted in yellow), includes 23% of the sample. Participants in this work environment risk group were more likely to report a poor physical environment (48%), not having easy access to COVID‐19 testing at work (48%), and not feeling adequately protected from COVID‐19 exposure at work (56%) compared to participants in Risk Group 1. The majority of respondents were satisfied with organizational and social support in their work environment. Almost three‐quarters (70%) reported that their employer took their well‐being into account when making decisions and more than half were satisfied with the support they received from their supervisor (53%) and colleagues (66%).
Risk Group 3 is characterized by a lack of organizational support (shown in purple) and represents 18% of the sample. A higher percentage of respondents in this class reported an adequate physical environment (70%), satisfactory training (87%), and protective equipment (99%) compared to participants in Risk Group 2. However, 99% of respondents in this work environment risk group reported that they did not feel appreciated by their employer, 56% stated that the workplace was not supportive, and 40% reported that their employer did not take their well‐being into account when making decisions. Risk Group 3 participants were also more likely to report a decrease in pay (23%) and benefits (19%) compared to respondents in the other risk classes.
Risk Group 4 is the poorest work environment (shown in red) and consists of 19% of the sample. Participants in this group were the most likely to report a poor physical environment (67%), inadequate training (52%), and inadequate protective equipment (61%). Three‐quarters felt inadequately protected from COVID‐19 exposure at work. All respondents in this group felt unappreciated by their employer, they described their workplace as unsupportive (97%) and they did not feel that the administration (96%) or their supervisor (70%) made their work life easier. Almost two‐thirds (64%) of participants in Risk Class 4 also stated that their organization did not have emotional support resources available. Notably, nurses and EMS providers were significantly more likely to cluster in Risk Groups 3 and 4 (53% and 38%, respectively) compared to attending and resident physicians (26%; see Table 1).
Table 2 displays the relationship between different types of risk factors and screening positive for our mental health outcomes. Almost 23% of respondents screened positive for depression/anxiety and 39.7% for burnout. Nurses were significantly more likely to screen positive for depression/anxiety (42%) and burnout (43%) compared to the other emergency HCWs. Participants who reported that they or one of their household members were at increased risk of COVID‐19 complications were significantly more likely to screen positive for both outcomes. Depression/anxiety and burnout were also significantly associated with other types of stressors such as concern about paying bills, misinformation about COVID‐19 in the news/media, the public health response to COVID‐19, and their community not adhering to public health guidelines.
TABLE 2.
Percent distribution of respondent, work environment, and community characteristics by mental health outcomes
| Characteristic | Positive for depression/anxiety | Positive for burnout | ||
|---|---|---|---|---|
| No, n = 532 | Yes, n = 156 | No, n = 415 | Yes, n = 273 | |
| Respondent | ||||
| Age (years)* | 35.8 (±9.6) | 33.0 (±9.5) | 35.9 (±9.7) | 34.2 (±9.7) |
| Male gender** | 297 (56) | 59 (38) | 243 (59) | 113 (41) |
| Race | ||||
| Non‐Hispanic White | 356 (67) | 104 (67) | 280 (67) | 181 (66) |
| Non‐Hispanic Black | 49 (9) | 16 (10) | 41 (10) | 24 (9) |
| Hispanic | 32 (6) | 14 (9) | 28 (7) | 18 (7) |
| Asian | 62 (12) | 9 (6) | 44 (11) | 27 (10) |
| Other | 32 (6) | 13 (8) | 21 (5) | 23 (8) |
| Present job title** | ||||
| Attending EP | 135 (25) | 22 (14) | 115 (28) | 42 (15) |
| Resident EP | 135 (25) | 31 (20) | 114 (27) | 52 (19) |
| EM nurse | 152 (29) | 66 (42) | 102 (25) | 117 (43) |
| EMS provider | 110 (21) | 37 (24) | 84 (20) | 62 (23) |
| Years in profession | 8.6 (±8.4) | 7.0 (±7.0) | 8.3 (±8.4) | 8.2 (±8.1) |
| Lives alone | 112 (21) | 34 (22) | 86 (21) | 61 (22) |
| Has primary childcare responsibilities | 149 (28) | 42 (27) | 122 (29) | 69 (25) |
| Self or household member at risk of COVID‐19 complications** | 172 (32) | 72 (46) | 128 (31) | 116 (42) |
| Infected by COVID‐19 | 107 (20) | 37 (24) | 86 (21) | 57 (21) |
| Not easy to talk with spouse, relative, or friends** | 50 (9) | 33 (21) | 35 (8) | 49 (18) |
| Life not made easier by spouse, relative, and friends | 74 (14) | 34 (22) | 63 (15) | 46 (17) |
| Extremely anxious about paying bills during COVID‐19** | 53 (10) | 40 (26) | 31 (7) | 61 (22) |
| Extremely anxious about misinformation in news/media** | 241 (45) | 105 (67) | 166 (40) | 181 (66) |
| Extremely anxious about government/public health response to COVID‐19** | 184 (35) | 81 (52) | 128 (31) | 137 (50) |
| Extremely anxious about people in my community not adhering to public health guidelines** | 164 (31) | 92 (59) | 125 (30) | 131 (48) |
| Used mental health resources during pandemic* | 95 (18) | 50 (32) | 75 (18) | 70 (26) |
| Perceived work environment | ||||
| Work environment risk class** | ||||
| Class 1 (overall good work environment) | 236 (44) | 39 (25) | 223 (54) | 52 (19) |
| Class 2 (inadequate resources) | 126 (24) | 33 (21) | 95 (23) | 64 (23) |
| Class 3 (lack of organizational support) | 86 (16) | 36 (23) | 61 (15) | 60 (22) |
| Class 4 (poor work environment) | 84 (16) | 48 (31) | 36 (9) | 97 (36) |
| Job stress score** | 3.3 (±0.8) | 3.8 (±0.7) | 3.1 (±0.7) | 3.8 (±0.7) |
| Community perceptions and risk of COVID‐10 | ||||
| Surge during survey period | 482 (91) | 140 (90) | 375 (90) | 247 (90) |
| Days since first peak | 93 (±138) | 124 (±137) | 89 (±138) | 118 (±136) |
Note: Data are reported as mean (±SD) or n (%).
p < 0.0025 for depression/anxiety only
p < 0.0025 for both depression/anxiety and burnout after Bonferroni correction for all the comparisons.
Participants who perceived that they worked in more adverse working environments (Risk Classes 3 and 4) were significantly more likely to screen positive for depression/anxiety and burnout compared to those who did not (i.e., Classes 1 and 2). The mean job stress score was also significantly higher among participants who were positive for depression/anxiety (mean 3.8) and burnout (mean 3.8) compared to those who were not (mean 3.3 and mean 3.1, respectively; p < 0.05).
There was no significant difference in the percentage of respondents who screened positive for the mental health outcomes by whether the survey was administered during a local surge in COVID‐19 cases (see Table 2). However, the average days since the first COVID‐19 peak in the community was significantly higher among participants who screened positive for depression/anxiety (mean 124) and burnout (mean 118) compared to those that did not (mean 93 and mean 89, respectively; p < 0.05).
Table 3 shows the results of the multivariate logistic regression models of the significant predictors of both mental health outcomes with and without job stress. Nurses were significantly more likely to screen positive for depression/anxiety (adjusted OR [aOR] 2.04, 95% CI 1.11–3.86) and burnout (aOR 2.05, 95% CI 1.22–3.49) compared to attendings, adjusted for other factors. Participants who reported that it was not easy to talk with their spouse/significant other, relative, or friends were significantly more likely to screen positive for both mental health outcomes compared to those who did have a confidant. Participants who reported being extremely anxious about paying their bills or about their community's response to COVID‐19 were also significantly more likely to screen positive for depression/anxiety and burnout compared to those who reported somewhat to no anxiety over these issues.
TABLE 3.
Adjusted OR (95% CI) of screening positive for depression/anxiety and burnout by significant respondent, perceived work environment, and community characteristics
| Characteristic a | Depression/anxiety b | Burnout b | ||
|---|---|---|---|---|
| Without job stress | With job stress | Without job stress | With job stress | |
| Job title (attending) | ||||
| Resident | 1.53 (0.81–2.95) | 1.77 (0.92–3.48) | 1.27 (0.74–2.20) | 1.47 (0.83–2.60) |
| Nurse | 2.26 (1.26–4.18) | 1.91 (1.04–3.6) | 2.25 (1.35–3.8) | 1.78 (1.03–3.07) |
| EMS provider | 1.84 (0.95–3.64) | 1.53 (0.76–3.10) | 1.63 (0.91–2.93) | 1.35 (0.73–2.49) |
| Not easy to talk with spouse, relative, or friends | 2.29 (1.3–4.02) | 2.16 (1.21–3.86) | 1.93 (1.09–3.44) | 1.83 (1.01–3.32) |
| Extremely anxious about paying bills | 2.11 (1.26–3.50) | 1.93 (1.13–3.27) | 2.24 (1.31–3.88) | 2.06 (1.17–3.66) |
| Extremely anxious about community response | 1.52 (1.28–1.8) | 1.39 (1.17–1.67) | 1.52 (1.3–1.79) | 1.39 (1.18–1.65) |
| Perceived work environment Risk Class 1 (good work environment) | ||||
| Risk Class 2 (inadequate resources) | 1.2 (0.68–2.11) | 0.96 (0.53–1.72) | 2.48 (1.53–4.04) | 2.01 (1.22–3.34) |
| Risk Class 3 (lack of organizational support) | 2.08 (1.17–3.69) | 1.83 (1.01–3.29) | 3.61 (2.15–6.12) | 3.29 (1.92–5.69) |
| Risk Class 4 (poor work environment) | 2.27 (1.28–4.04) | 1.46 (0.79–2.69) | 9.56 (5.5–16.98) | 6.74 (3.75–12.32) |
| Job stress (continuous) | Not applicable | 2.32 (1.67–3.27) | Not applicable | 2.69 (2.00–3.68) |
Reference group in parentheses.
Models include a fixed effect for site (not shown).
The perceived work environment was also significantly associated with both mental health outcomes (see Table 3). Participants in Work Environment Risk Groups 3 and 4 were significantly more likely to screen positive for depression/anxiety (aOR 1.89, 95% CI 1.05–3.42; and aOR 2.04, 95% CI 1.14–3.66, respectively) compared to participants in Risk Group 1. The relationship between the perceived work environment and burnout was similar but participants in Work Group 2 also had a significantly higher odds of screening positive for burnout (aOR 2.07, 95% CI 1.27–3.40) compared to those in Work Group 1. When we added job stress to the model, not only was it a significant predictor of depression/anxiety but it also fully mediated (100%) the relationship between the perceived work environment risk group and depression/anxiety. Job stress was also a significant predictor of burnout but its mediation effect was partial (i.e., 5%–20%).
DISCUSSION
A high rate of respondents in our sample screened positive for depression/anxiety, and burnout. Notably, individuals who worked in an environment with few resources and little perceived organizational support had the highest rates of depression/anxiety and burnout. Respondents who worried about a loved one at risk for contracting COVID‐19 or who had the added stress of worrying about paying bills, being exposed to public misinformation, and concern about the public's response to the pandemic were more likely to report negative mental health sequelae.
Our rates of positive screens for depression/anxiety among emergency HCWs were within the range of that shown in previous studies during this period (anxiety [13%–44%], 6 , 9 , 10 , 12 , 21 depression [20%–50%], 5 , 6 burnout [30%–49%]). 6 , 10 , 22 , 23 Although limited and mainly measured in smaller populations, prepandemic studies have demonstrated high overall rates of burnout 24 and depression 25 among EPs, particularly among residents. Nurses also have high baseline rates of depression and burnout especially when hospital based. 26 Less work has focused on the EMS population, although reported burnout rates are high. 27 , 28 It is important to note that many prior studies focused on limited samples and none have examined these outcomes among a combined sample of EPs, nurses, and EMS providers.
Many approaches to HCW health and wellness during the pandemic have focused on addressing mental health outcomes during times of crisis, such as through hospital‐based peer support programs and stress management techniques. 29 , 30 While mental health support and interventions targeting individual‐level stress relief and resilience building are important, it is crucial to emphasize that organizational factors must also be addressed as a root cause of burnout, depression, and anxiety. Failure to recognize the role of these organizational factors can result in unfair blaming of symptomatic individuals for their failure to show resilience. Approaches to address burnout and mental health must be multifactorial. This includes fostering healthier workplace environments, improving organizational culture, and ultimately implementing broader policy‐level changes.
We found a strong association between an adverse working environment and poor mental health particularly when organizational support was deemed inadequate. Providers in Work Environment Risk Groups 3 and 4, which had the most challenging working conditions, were most likely to report symptoms of depression/anxiety and burnout. For example, Group 4 HCWs comprised the largest percentage of those who screened positive for depression/ anxiety and for burnout. They reported poor workplace conditions across all domains, including a poor physical work environment, inadequate training, limited equipment, poor employer support, and lack of appreciation by leadership.
The perception of a poor organizational structure among a significant proportion of emergency HCWs is not a new finding. Rather, the COVID‐19 pandemic has further exposed an already flawed work environment. 31 , 32 , 33 The National Academy of Medicine has developed a framework to address provider well‐being at multiple points including at the site of care delivery, at the organizational level, and at the industry level. 34 The Institute for Healthcare Improvement suggests that health care leaders gather input directly from employees about their perceptions of ideal working conditions, address barriers to achieving these ideals, and then follow metrics to assess the impact of changes. 35 Organizations are starting to recognize the importance of addressing HCW well‐being. 36 It is important that providers feel comfortable using mental health resources at the workplace without stigma or fear of negative repercussions on work or licensure. 7 Strategies to address burnout include investment in technology to support provider work tasks, reducing administrative burdens, and providing a positive and supportive work and learning environment. Small‐scale approaches that shorten working hours and streamline HCW workload and that engage frontline providers in identifying potential interventions that improve well‐being may be effective. 37 , 38 , 39 , 40 , 41 , 42 However, most of these interventions are oriented to the physician rather than to other HCWs such as nurses or EMS providers. In addition, few are specifically targeted to emergency HCWs, who have unique workplace challenges. 43 , 44
In the recognition the importance of addressing burnout and stress, the U.S. Department of Health and Human Services recently budgeted over 100 million dollars to address issues to promote mental health well‐being among HCWs. 45 As part of this initiative, 45 health care organizations have received grants to address this issue over the next 3 years. 46
While more work needs to be done to evaluate the most effective approaches to reducing job stress for emergency HCWs, what is certain is that the consequences of burnout, depression, and anxiety can be detrimental, both to HCWs and to patients. Poor HCW mental well‐being is associated with lower productivity and decreased job satisfaction. 47 It is also associated with an increased risk of workplace errors that can undermine patient safety. 48 , 49 Burnout additionally can lead to problems at the organizational level, lowering staff retention rate and affecting overall output, resulting in loss of health care revenue and further staffing shortages. 47 At extremes, it can lead to HCW substance use and suicide. 50 , 51 , 52
LIMITATIONS
Our study has a number of limitations. First, all data are self‐reported. Second, the cross‐sectional nature of the data limited us to an atemporal mediation analysis. We cannot establish causality between our mental health outcomes and the risk factors due to the lack of a temporal sequence of events. In addition, because do not have a baseline assessment of our mental health outcomes, we cannot rule out the possibility of their existence prior to the pandemic. Third, the generalizability of our results may be limited because the sample is based on emergency HCWs employed at 10 academic sites and not all types of participants were randomly selected Fourth, although we focused on job stress, we understand that in many cases there may have been overlap with home stress. Finally, although we relied largely on validated scales, we did include some self‐designed items tailored to the pandemic that were pilot tested in a sample prior to administration of the survey to our study sample. To increase the interpretability of the LCA, we dichotomized some of the workplace conditions based on an arbitrary cutoff point rather than previously validated threshold levels.
CONCLUSIONS
In conclusion, the COVID‐19 pandemic undeniably presents extraordinary hardship on the mental health and well‐being of emergency health care workers. Our study demonstrated a strong association between a perceived adverse working environment and poor mental health. This was particularly present when the perceived organization work environment was not favorable, demonstrating potential opportunities for intervention. Ultimately, a culture change that prioritizes health care worker well‐being is crucial as we look toward the future.
CONFLICT OF INTEREST
The authors have no conflicts of interests to disclose.
AUTHOR CONTRIBUTIONS
Janice Blanchard and Melissa McCarthy were involved in all stages of the study including securing of funding, conception of the study, data collection, analysis, and composition of the manuscript. Yixuan Li was involved in the data collection, analysis, and composition of the manuscript. Anne M. Messman, Suzanne K. Bentley, Michelle D. Lall, Yiju Teresa Liu, Rory Merritt‐Recchia, Randy Sorge, Christopher Greene, Jordan M. Warchol, and Deborah B. Diercks were involved in survey development, recruitment, and composition of the manuscript. James Griffith and Rita A. Manfredi contributed to survey development and composition of the manuscript.
Supporting information
Figure S1
Figure S2
Figure S3
Tables S1‐S2
Table S3
Blanchard J, Li Y, Bentley SK, et al. The perceived work environment and well‐being: A survey of emergency health care workers during the COVID‐19 pandemic. Acad Emerg Med. 2022;29:851‐861. doi: 10.1111/acem.14519
Supervising Editor: Steven Bird, MD
REFERENCES
- 1. Mhango M, Dzobo M, Chitungo I, Dzinamarira T. COVID‐19 risk factors among health workers: a rapid review. Saf Health Work. 2020;11:262‐265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mehta S, Machado F, Kwizera A, et al. COVID‐19: a heavy toll on health‐care workers. Lancet Respir Med. 2021;9:226‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Calò F, Russo A, Camaioni C, De Pascalis S, Coppola N. Burden, risk assessment, surveillance and management of SARS‐CoV‐2 infection in health workers: a scoping review. Infect Dis Poverty. 2020;9:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dean W, Jacobs B, Manfredi RA. Moral injury: the invisible epidemic in COVID health care workers. Ann Emerg Med. 2020;76:385‐386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wright HM, Griffin BJ, Shoji K, et al. Pandemic‐related mental health risk among front line personnel. J Psychiatr Res. 2020;137:673‐680. [DOI] [PubMed] [Google Scholar]
- 6. Rodriguez RM, Montoy JCC, Hoth KF, et al. Symptoms of anxiety, burnout, and PTSD and the mitigation effect of serologic testing in emergency department personnel during the COVID‐19 pandemic. Ann Emerg Med 2021;78:35‐43.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chor WPD, Ng WM, Cheng L, et al. Burnout amongst emergency healthcare workers during the COVID‐19 pandemic: a multi‐center study. Am J Emerg Med. 2020;46:700‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kelker H, Yoder K, Musey P, et al. Longitudinal prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID‐19 pandemic. Res Sq. Preprint 2020. 10.21203/rs.3.rs-87786/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians' anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID‐19 pandemic. Acad Emerg Med. 2020;27:700‐707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu Q, Luo D, Haase JE, et al. The experiences of health‐care providers during the COVID‐19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8:e790‐e798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Teo I, Chay J, Cheung YB, et al. Healthcare worker stress, anxiety and burnout during the COVID‐19 pandemic in Singapore: a 6‐month multi‐centre prospective study. PLoS One. 2021;16:e0258866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Johns Hopkins University . Johns Hopkins University Coronavirus Resource Center. Vol 2021.
- 14. Centers for Disease Control and Prevention . National Assessment of Occupation Safety in the Workforce. Accessed October 1, 2020. https://www.cdc.gov/niosh/oshworkforce/default.html#questionnaire
- 15. Maunder RG, Lancee WJ, Rourke S, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004;66:938‐942. [DOI] [PubMed] [Google Scholar]
- 16. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra‐brief screening scale for anxiety and depression: the PHQ‐4. Psychosomatics. 2009;50:613‐621. [DOI] [PubMed] [Google Scholar]
- 17. Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med. 2015;30:582‐587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Canady V. APA poll finds nearly half anxious about getting COVID‐19. Mental Health Weekly. 2021;30:5. [Google Scholar]
- 19. Chong M‐Y, Wang W‐C, Hsieh W‐C, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185:127‐133. [DOI] [PubMed] [Google Scholar]
- 20. Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu Y, Long Y, Cheng Y, et al. Psychological impact of the COVID‐19 outbreak on nurses in China: a nationwide survey during the outbreak. Front Psych. 2020;11:598712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baumann BM, Cooper RJ, Medak AJ, et al. Emergency physician stressors, concerns, and behavioral changes during COVID‐19: a longitudinal study. Acad Emerg Med. 2021;28:314‐324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Teo YH, Xu JTK, Ho C, et al. Factors associated with self‐reported burnout level in allied healthcare professionals in a tertiary hospital in Singapore. PLoS One. 2021;16:e0244338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, drop out, suicide: physician loss in emergency medicine, Part I. West J Emerg Med. 2019;20:485–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Williamson K, Lank PM, Olson A, Cheema N, Lovell E. A positive depression screen is associated with emergency medicine resident burnout and is not affected by the implementation of a wellness curriculum. West J Emerg Med. 2021;22:1341‐1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dyrbye LN, West CP, Leep Hunderfund A, et al. Relationship between burnout and professional behaviors and beliefs among US nurses. J Occup Environ Med. 2020;62:959‐964. [DOI] [PubMed] [Google Scholar]
- 27. Boland LL, Kinzy TG, Myers RN, et al. Burnout and exposure to critical incidents in a cohort of emergency medical services workers from Minnesota. West J Emerg Med. 2018;19:987‐995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Crowe RP, Bower JK, Cash RE, Panchal AR, Rodriguez SA, Olivo‐Marston SE. Association of burnout with workforce‐reducing factors among EMS professionals. Prehosp Emerg Care. 2018;22:229‐236. [DOI] [PubMed] [Google Scholar]
- 29. Wu PE, Styra R, Gold WL. Mitigating the psychological effects of COVID‐19 on health care workers. CMAJ. 2020;192:E459‐E460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Horan KA, Marks M, Ruiz J, Bowers C, Cunningham A. Here for my peer: the future of first responder mental health. Int J Environ Res Public Health. 2021;18:11097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Strecker C, Huber A, Höge T, Hausler M, Höfer S. Identifying thriving workplaces in hospitals: work characteristics and the applicability of character strengths at work. Appl Res Qual Life. 2020;15:437‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Karasek R. The stress‐disequilibrium theory: chronic disease development, low social control, and physiological de‐regulation. Med Lav. 2006;97:258‐271. [PubMed] [Google Scholar]
- 33. Soto‐Rubio A, Giménez‐Espert MDC, Prado‐Gascó V. Effect of emotional intelligence and psychosocial risks on burnout, job satisfaction, and nurses' health during the COVID‐19 pandemic. Int J Environ Res Public Health. 2020;17:7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. National Academies of Sciences Engineering and Medicine (U.S.). Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well‐Being . Taking action against clinician burnout: a systems approach to professional well‐being. The National Academies Press; 2019. [PubMed] [Google Scholar]
- 35. Perlo J, Balik B, Swensen S, Kabcenell A, Landsman J, Feeley D. IHI framework for improving joy in work. Institute for Healthcare Improvement; 2017. [Google Scholar]
- 36. Association of American Medical Colleges . The rise of wellness initiatives in health care: using national survey data to support effective well‐being champions and wellness programs. Association of American Medical Colleges; 2021. [Google Scholar]
- 37. Fassiotto M, Simard C, Sandborg C, Valantine H, Raymond J. An integrated career coaching and time‐banking system promoting flexibility, wellness, and success: a pilot program at Stanford University School of Medicine. Acad Med. 2018;93:881‐887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta‐analysis. Lancet. 2016;388:2272‐2281. [DOI] [PubMed] [Google Scholar]
- 39. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516‐529. [DOI] [PubMed] [Google Scholar]
- 40. Shanafelt TD, Wang H, Leonard M, et al. Assessment of the association of leadership behaviors of supervising physicians with personal‐organizational values alignment among staff physicians. JAMA Netw Open. 2021;4:e2035622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Swensen SJ, Shanafelt T. An Organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf. 2017;43:308‐313. [DOI] [PubMed] [Google Scholar]
- 42. Shanafelt T, Trockel M, Rodriguez A, Logan D. Wellness‐centered leadership: equipping health care leaders to cultivate physician well‐being and professional fulfillment. Acad Med. 2021;96:641‐651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lall MD, Gaeta TJ, Chung AS, et al. Assessment of physician well‐being, part one: burnout and other negative states. West J Emerg Med. 2019;20:278‐290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gaeta TJ. Need for a holistic approach to reducing burnout and promoting well‐being. J Am Coll Emerg Physicians Open. 2020;1:1050‐1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Department of Health and Human Services . Biden‐Harris Administration Awards $103 Million in American Rescue Plan Funds to Reduce Burnout and Promote Mental Health and Wellness Among Health Care Workforce. Accessed April 20, 2022. https://www.hhs.gov/about/news/2022/01/20/biden‐harris‐administration‐awards‐103‐million‐american‐rescue‐plan‐funds‐reduce‐burnout‐promote‐mental‐health‐wellness‐among‐health‐care‐workforce.html
- 46. American Medical Association . 3 health organizations get nearly $8 million to fight burnout. Accessed April 20, 2022. https://www.ama‐assn.org/practice‐management/physician‐health/3‐health‐organizations‐get‐nearly‐8‐million‐fight‐burnout
- 47. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well‐being. JAMA Intern Med. 2017;177:1826‐1832. [DOI] [PubMed] [Google Scholar]
- 48. Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta‐analysis. Ann Intern Med. 2019;171:555‐567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mangory KY, Ali LY, Rø KI, Tyssen R. Effect of burnout among physicians on observed adverse patient outcomes: a literature review. BMC Health Serv Res. 2021;21:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Harvey SB, Epstein RM, Glozier N, et al. Mental illness and suicide among physicians. Lancet. 2021;398:920‐930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ye GY, Davidson JE, Kim K, Zisook S. Physician death by suicide in the United States: 2012‐2016. J Psychiatr Res. 2021;134:158‐165. [DOI] [PubMed] [Google Scholar]
- 52. Menon NK, Shanafelt TD, Sinsky CA, et al. Association of physician burnout with suicidal ideation and medical errors. JAMA Netw Open. 2020;3:e2028780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. United States Census. Accessed April 20, 2022. https://www.census.gov
- 54. McCarthy ML, Zheng Z, Wilder ME, Elmi A, Li Y, Zeger SL. The influence of social determinants of health on emergency departments visits in a medicaid sample. Ann Emerg Med. 2021;77:511‐522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. American Psychological Association . Stress in America 2020: a national mental health crisis. Accessed April 20, 2022. https://www.apa.org/news/press/releases/stress/2020/report‐october
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1
Figure S2
Figure S3
Tables S1‐S2
Table S3


