Abstract
Background:
Studies of thunderstorm asthma to understand risk factors using high-resolution climate data and asthma outcomes on a large scale are scarce. Moreover, thunderstorm asthma is not well studied in the United States.
Objectives:
We examined whether climate parameters involved in thunderstorms are associated with emergency department (ED) visits for acute asthma attacks in the United States.
Methods:
We analyzed 63,789 asthma-related, daily ED visits for all age groups, and thunderstorm-associated climate data in Louisiana during 2010 through 2012. We performed time-series analyses using quasi-Poisson regression models with natural cubic splines of date, parish, holiday, day of week, season, daily maximum concentrations of ozone () and fine particulate matter [PM in aerodynamic diameter ()], and daily mean pressure, precipitation, and temperature. Because of a significant interaction effect between temperature and lightning days on asthma-related visits, we performed stratified analyses by days with/without lightning or thunderstorm (defined by any lightning and precipitation).
Results:
On thunderstorm days, higher asthma-related ED visits were associated with higher daily mean precipitation [ (95% CI: 1.009, 1.300)] and lower daily mean temperature [ per 1°C change (1.000–1.021)] without carry-over effect to the next non-thunderstorm day. These higher risks were found mainly among children and adults of age. We observed similar results on lightning days. However, we did not find similar associations for non-thunderstorm or non-lightning days. Daily maximum and levels were not significantly associated with asthma ED visits on thunderstorm days.
Discussion:
Higher precipitation and lower temperature on thunderstorm days appear to contribute to asthma attacks among people with asthma, suggesting they should consider taking precautions during thunderstorms. EDs should consider preparing for a potential increase of asthma-related visits and ensuring sufficient stock of emergency medication and supplies for forecasted severe thunderstorm days. https://doi.org/10.1289/EHP10440
Introduction
In the United States, thunderstorm asthma (asthma attacks associated with thunderstorms) is not a well-studied phenomenon, whereas it is better understood in Europe and Australia.1–3 Thunderstorm asthma was first recognized in early 1980s in the United Kingdom.4–6 The most recent severe outbreak was in 2016 in Melbourne, Australia, resulting in patients with severe asthma attacks, 35 patients admitted to intensive care, and 10 deaths.3,7 After the severe thunderstorm event, those who had asthma and hay fever also reported respiratory distress.6 However, thunderstorm asthma is not thought to lead to development of new asthma cases; rather, it is an exacerbation of existing asthma and in some cases, patients with seasonal rhinitis can have asthma attacks.7
Some evidence indicates the frequency of severe thunderstorms is likely to increase in the future with global climate change.3,7,8 All thunderstorms have lightning, and most in North America are short-lived (within a couple of hours from development to dissipation), sometimes producing heavy precipitation and strong wind gusts.9,10 Surface temperature can drop suddenly with falling precipitation and cold downdrafts during the formation of thunderstorms.9 Increases in respirable bioaerosols (cytoplasmic granules of pollens or fungal spores), along with sudden changes in climate conditions, including electrical fields during or after thunderstorms, are considered a potential mechanism for thunderstorm-related asthma outbreaks.2,4,5,11–13
Studies investigating outbreaks of thunderstorm asthma over the past few decades have had limitations, including small sample sizes of thunderstorm days and low spatial resolution of climate data (i.e., applying same climate data to the large area).2 To overcome these, we analyzed daily emergency department (ED) visits for asthma along with high-resolution climate data in all 64 parishes (small geographical units similar to a county) in Louisiana 2010 through 2012. Located along the Gulf Coast, Louisiana has one of the highest frequencies of thunderstorms and the highest prevalence of asthma in nonmetropolitan statistical areas in the United States.14,15 The objective of our study was to examine whether parish-level daily ED visits for acute asthma attacks in Louisiana were associated with meteorological conditions linked to thunderstorm events.
Methods
Data Sources
ED discharge data for Louisiana during 2010 through 2012 were available at the beginning of the study in 2016 and were collected by SharCor LLC, a partner of the Louisiana Hospital Association. Of 123 licensed acute and critical care hospitals in Louisiana, contributed to the data. These did not include any federal facilities, such as Veterans Affairs hospitals. We selected asthma-related ED visits based on primary discharge diagnosis, namely, International Classification of Diseases, Ninth Revision, Clinical Modification16 (ICD-9-CM) code 493. We also identified ED visits from the inpatient discharge database if the point of origin code indicated ED, or if revenue codes 0450–0459 or 0762 were associated with the record. Of records with a valid ICD-9-CM code that were queried, 65,285 records had an ICD-9-CM code consistent with asthma (ICD-9-CM 493). Approximately 13% of these were extracted from the inpatient discharge database based on the point of origin or revenue code. Records were then processed according to the Standards for Nationally Consistent Data and Measures (NCDM) within the Centers for Disease Control and Prevention’s (CDC) National Environmental Public Health Tracking Network,17 removing any observation that did not have a valid Louisiana ZIP Code or city (; 2% of asthma records). Observations with no parish information were assigned one by cross-referencing with the ZIP Code or city data (; 10%). Finally, 42 duplicate records and 3 records of admissions occurring for the same primary ICD-9-CM code within were removed in accordance with the NCDM guidance. The final data set () was then de-identified and aggregated to three age groups [children and adolescents (described as “children” hereafter): , adults: , and older adults: years of age] at the parish level to protect patient confidentiality. Because these de-identified data were collected as part of public health surveillance, the data were considered institutional review board (IRB)–exempt according to the CDC’s IRB determination policy.
A climate database was constructed by extracting climate variables from the National Centers for Environmental Prediction (NCEP) North American Regional Reanalysis (NARR),18 downloaded from the National Oceanic and Atmospheric Administration (NOAA) website.19 NARR contains climate variables in which spatial and temporal resolutions are high and consistent over time (in a grid every 3 h). It incorporates millions of observations from various sources over North America into a data assimilation system. Among the hundreds of climate variables in NARR, we extracted variables associated with the physical and dynamic processes of thunderstorms. To match with daily asthma-related ED visit data, the daily means of NARR climate variables during 2010 through 2012 were extracted from grid cells containing centroid points of each parish in Louisiana, and parish data were organized using Federal Information Processing Standards (FIPS) codes. The climate variables used in the final modeling included daily mean air temperature (in degrees Celsius), daily mean sea level pressure (in kilopascals), daily precipitation rate (in grams of water per square meter per second), and horizontal daily mean wind speed (in meters per second).
Lightning is an electrostatic discharge formed during temporary equalization of opposite charges between the storm cloud and the ground. The radio waves emitted from cloud-to-ground lightning strikes have been recorded by the National Lightning Detection Network (NLDN) each day since 1986,20 and grids of 0.10 degrees were created to show only positive polarity flashes. The lightning data stored at the National Centers for Environmental Information were aggregated to the parish level for each day to match with health outcome data for the study.21 Daily maximum ambient air concentrations of fine particulate matter [PM in aerodynamic diameter ()], in micrograms per cubic meter, and ozone (), in parts per billion, were predicted using the U.S. Environmental Protection Agency’s monitoring data from their Air Quality System sites and using the Bayesian space–time downscaling fusion modeling approach at census-tract centroids for the contiguous United States.22,23 From these predicted data, daily and population-weighted parish-level and concentrations were estimated for the study.
Data Analysis
We performed time-series analyses using log-linear quasi-Poisson regression models that accounted for overdispersion to examine associations of daily asthma-related ED visits with daily climate variables described earlier. Time-series analysis does not require adjustment for other common confounding variables such as age, gender, sex, race, and smoking status because their distributions do not change from day to day at the population level.24 In addition, race/ethnicity data were missing or unreliable for most of the records and, thus, were not collected by the CDC for analysis. We defined thunderstorm days as ones with both lightning and precipitation (with greater than 0 grams water per meter squared per second). To show spatial distribution of the number of daily asthma-related ED visits, lightning strikes, and thunderstorm days over all parishes in Louisiana, they were joined to cartographic files using five-digit parish-level FIPS codes using QGIS (version 3.6.0; QGIS Development Team). The Jenks natural breaks classification scheme was used to determine critical intervals for spatial display of maps.25 We observed that the association of temperature with asthma-related ED visits depended on days with/without lightning in our initial interaction model (). This interaction effect made it difficult to interpret the separate effect of temperature or lightning days (and thunderstorm days because it comprises lightning by definition) on asthma-related ED visits. Therefore, we performed stratified analyses using separate models by status of lightning or thunderstorm.
The full model was constructed with known risk factors for asthma, factors associated with ED visits for asthma, and important meteorological factors involved in formating thunderstorms.9,10,23 The full model included a natural cubic spline of date, parish, Louisiana holiday, day of week, season [dichotomized into non-summer (October–April) vs. summer (May−September) owing to the low frequency of thunderstorm days in spring, fall, or winter], daily maximum and concentrations, and daily mean precipitation rate, temperature, and sea level pressure. Natural cubic spline function was fitted with 12 degrees of freedom per year to adjust for long-term trends in patterns of asthma-related ED visits.23,24 The analyses with the full model were also performed by age group because asthma-related ED visits could differ by age. We also constructed reduced models by excluding and from the full model because they were not significant, and their exclusion little changed ( in RR) associations between temperature or precipitation and asthma-related ED visits on thunderstorm days (Table 1). Horizontal daily mean wind speed was excluded from all models because it was neither a significant predictor nor a confounder of associations of interest ( changes in coefficients). We assumed log-linear relationships between asthma-related ED visits and precipitation rate or temperature because partial regression plots with generalized additive models using a cubic penalized regression spline of precipitation and temperature suggested log-linear relationships (Figures S1 and S2). We evaluated 1-d time–lag effects of temperature and precipitation on asthma-related ED visits during the non-thunderstorm day that followed a thunderstorm day because previous studies indicated that more asthma-related ED visits occurred within several hours after the thunderstorm, as discussed in detail in the “Discussion” section.11,26 Pearson correlation coefficients were estimated among the climate variables. Tukey honest significant differences tests were used for multiple comparisons for the number of parish-days with thunderstorm or lightning strikes among seasons or parish.27 Pearson’s chi-square test was used to examine the difference in lightning days between rainy and dry days. Analysis of variance was used to test difference in climate and air pollutant variables between thunderstorm and non-thunderstorm days. All statistical analyses were performed using R (version.4.0.3; R Development Core Team). Statistical significance for inference was considered at
Table 1.
Associations of precipitation, temperature, pressure, and pollutants with asthma-related ED visits () for days with () or without thunderstorms () in Louisiana, 2010–2012.
| Daily climate and pollutant variables (unit) | Full model RR (95% CI): thunderstorm | Reduced model RR (95% CI): thunderstorm | Full model RR (95% CI): non-thunderstorm | Reduced models RR (95% CI): non-thunderstorm | ||
|---|---|---|---|---|---|---|
| Same day visits () | Next day visits () | Same day visits () | Next day visits () | Same day visits () | ||
| Precipitation rate () | 1.128 (0.992, 1.284) | 0.938 (0.779, 1.130) | 1.145 (1.009, 1.300) | 0.996 (0.831, 1.193) | 1.044 (0.921, 1.184) | 1.022 (0.903, 0.158) |
| Temperature drop (1 °C) | 1.010 (1.000, 1.021) | 1.007 (0.994, 1.019) | 1.011 (1.000, 1.021) | 1.008 (0.996, 1.020) | 1.001 (0.998, 1.004) | 1.001 (0.998, 1.004) |
| Pressure (1 kPa) | 1.010 (0.946, 1.078) | 1.004 (0.930, 1.084) | 1.010 (0.946, 1.078) | 1.012 (0.938, 1.093) | 0.995 (0.971, 1.019) | 0.997 (0.973, 1.020) |
| (1 ppb) | 1.001 (0.998, 1.003) | 1.001 (0.997, 1.004) | — | — | 1.002 (1.001, 1.003) | — |
| () | 0.995 (0.990, 1.003) | 0.986 (0.977, 0.996) | — | — | 0.99 (0.996, 1.002) | — |
Note: Time-series quasi-Poisson regression models were adjusted for long-term trend with natural cubic spline (), parish, Louisiana holidays, day of week, and season (summer vs. non-summer); next day ED visit models analyzed to evaluate associations of precipitation or temperature of the thunderstorm day with the next non-thunderstorm day’s asthma-related ED visits; 1,351 ED visits were deleted from the regression analyses owing to missingness in lightning data. —, variables not included in the reduced models; CI, confidence interval; ED, emergency department; , ozone; , particulate matter in aerodynamic diameter (fine particulate matter); RR, relative risk.
Results
Characterization of Asthma-Related ED Visits and Climate Data
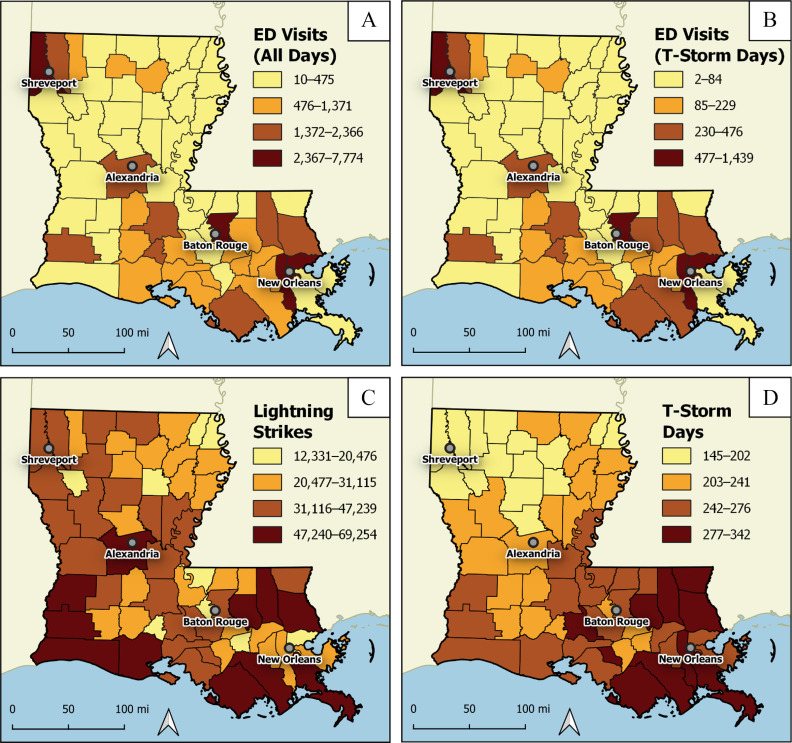
A total of 63,789 asthma-related ED visits were reported in Louisiana during 2010 through 2012 (19,417 in 2010; 20,902 in 2011; and 23,470 in 2012). Parishes in northwestern (Shreveport) and southeastern (New Orleans) Louisiana had a higher number of asthma-related ED visits () than others (Figure 1; Table S1); this pattern was also apparent in the rate of ED visits for asthma per 10,000 population (Figure S3; Table S2).17 The number of asthma-related ED visits differed by age group, with the highest for children (48%), followed by adults (44%), and older adults (8%) (Figure S4).
Figure 1.
Spatial distribution of the number of daily asthma-related ED visits, lightning strikes, and thunderstorm days in Louisiana, 2010–2012 (numerical data in Table S1). The graph presents total number of asthma-related ED visits (A) in all days and (B) on thunderstorm days, (C) total number of cloud-to-ground lightning strikes, and (D) number of thunderstorm days for each Louisiana parish, 2010–2012. Map created using the Free and Open Source QGIS (version 3.16.11; QGIS Development Team). Background map sourced from U.S. Census Bureau (https://www.census.gov/programs-surveys/geography/technical-documentation/naming-convention/cartographic-boundary-file.html). Note: ED, emergency department.
We had a total of 70,144 parish-days, but 1.9% (1,344) of those were missing lightning data; thus, we analyzed a total of 68,800 parish-days, of which 24.7% (16,992) had lightning (Table S3). Of these parish-days with lightning, 10.7% (1,813 parish-days) had lightning with no precipitation, resulting in 15,179 parish-days with thunderstorms (22.1% of the total parish-days with lightning) (Tables S3 and S4). There were more than 2-fold rainy than dry days [48,230 vs. 21,914 parish-days (68.8% vs. 31.2%)], and 32% of 15,179 rainy days had at least one lightning strike. Rainy days were more likely to have lightning () (Table S3). The number of lightning strikes and thunderstorm days were not statistically different by parish (Figure 1; Table S1) but was highest during summer (Figure 2).
Figure 2.
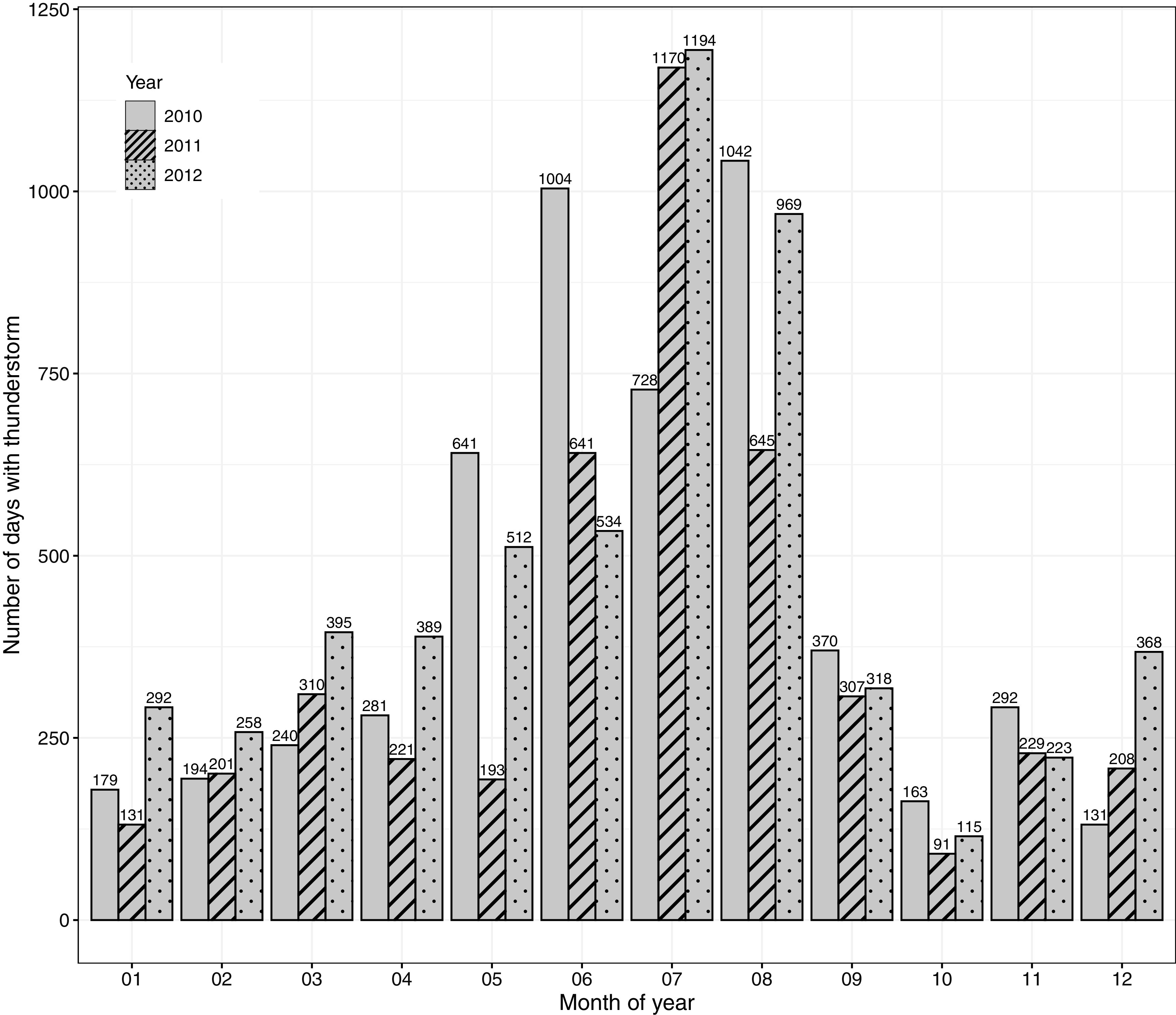
Total number of parish-days with thunderstorms () in Louisiana by month and year, 2010–2012.
Daily mean pressure was lower on thunderstorm days than non-thunderstorm days (101.50 vs. 101.77 kPa; ), but mean temperature was higher (24.7 vs. 18.8°C; ) (Table S5). On average, precipitation rate was -fold higher on thunderstorm days than non-thunderstorm days (0.097 vs. ; ). There were 67 parish-days that had a precipitation rate equal to or exceeding : 24 from thunderstorm days and 43 from non-thunderstorm days (Figure S5). Among the thunderstorm days, precipitation rate was negatively and significantly correlated with mean temperature (correlation coefficient, ), whereas the correlation was positive on non-thunderstorm days () (Figure 3A). Daily mean pressure was negatively correlated () with temperature on thunderstorm days and was weaker than the correlation on non-thunderstorm days () (Figure 3B). Daily mean pressure was also negatively correlated with precipitation rate on both thunderstorm and non-thunderstorm days (Figure 3C). Both daily maximum and levels were negatively correlated with precipitation but positively correlated with temperature () on thunderstorm or non-thunderstorm days (data not shown). The number of lightning strikes on thunderstorm days was significantly () and positively but very weakly correlated with () and ().
Figure 3.
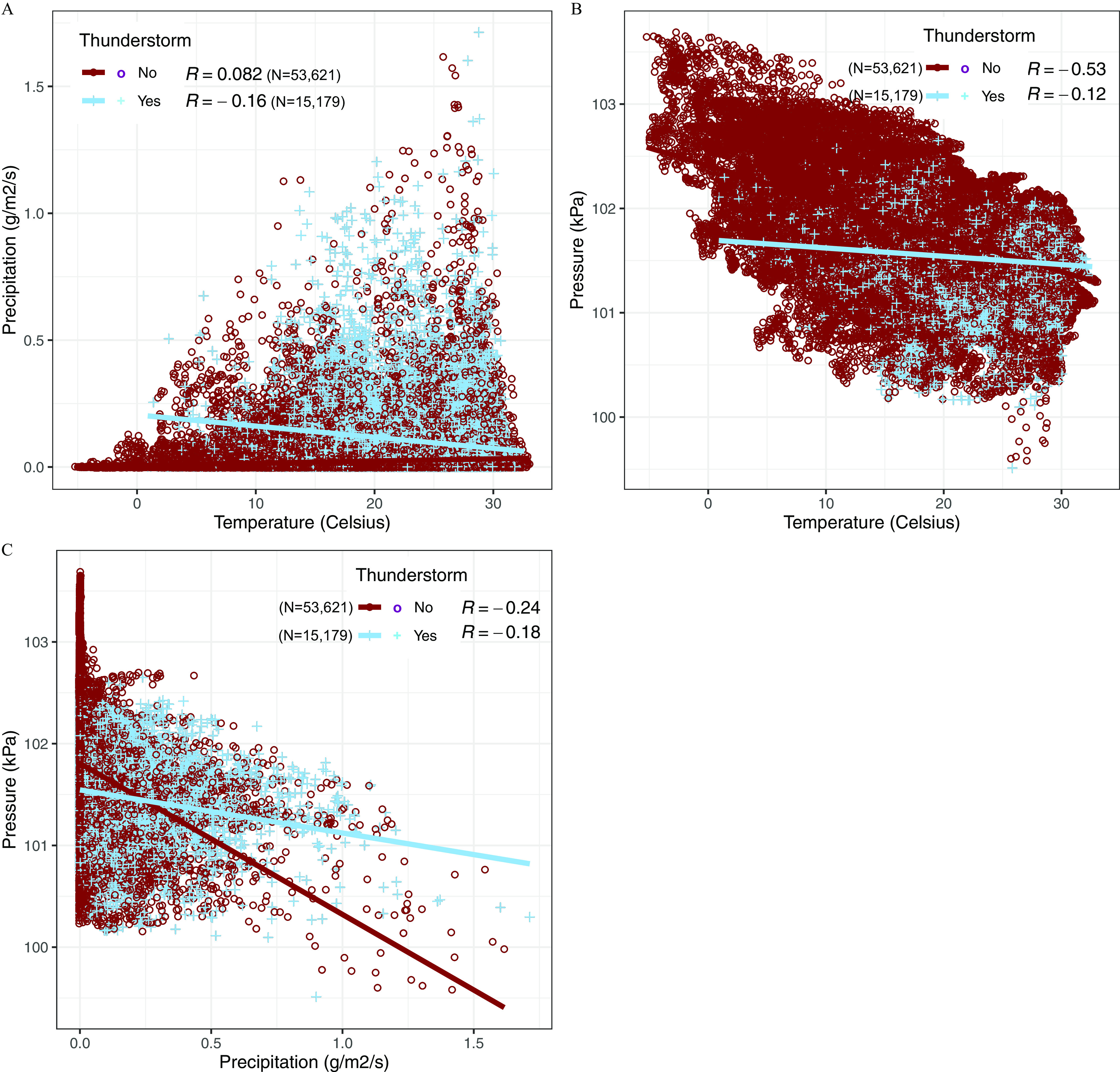
Scatter plots and correlation coefficients among three climate variables by occurrence of thunderstorms in Louisiana, 2010–2012 (). (A) Correlation between temperature and precipitation; (B) correlation between temperature and pressure; and (C) correlation between precipitation and pressure. R represents Pearson correlation coefficients by occurrence of thunderstorms; lines on the scatter plots represent linear regression lines. All correlation coefficients were statistically significant (all ).
Associations of Asthma-Related ED Visits with Meteorological Conditions
On thunderstorm days, the final reduced model indicated that for each () higher daily mean precipitation rate, the risk of asthma-related ED visits was 14.5% higher [; 95% CI: 1.009, 1.300] (Table 1; Figure S5). During the study period, this higher risk was equivalent to 1.6% more asthma-related ED visits as precipitation changed from the 25th to the 75th percentile (interquartile range: ) or 25.4% more visits when the precipitation changed from the median () to the maximum (). The full models yielded a similar magnitude of risk of asthma-related ED visits, as shown in Table 1. The positive association of precipitation with asthma-related ED visits on thunderstorm days was mainly found among children (; 95% CI: 1.056, 1.527) (Table 2). On non-thunderstorm days, no precipitation effects were observed for any age group (Tables 1 and 2). The reduced model also indicated that for each 1°C lower daily mean temperature, the risk of asthma-related ED visits was significantly higher by 1.1% (; 95% CI: 1.000, 1.021) on thunderstorm days, which was found mainly among adults (; 95% CI: 0.998, 1.029). However, on non-thunderstorm days, the association with temperature drop depended on age group, with a positive association (0.4%; ; 95% CI: 1.000, 1.009) for children and a negative association (; ; 95% CI: 0.992, 1.001) for adults (Table 2). Older adults did not contribute to the higher risk of asthma-related ED visits associated with precipitation or temperature during thunderstorm or non-thunderstorm days.
Table 2.
Associations of precipitation, temperature, pressure, and pollutants with asthma-related ED visits () for days with () or without thunderstorms () stratified by age group using full models in Louisiana, 2010–2012.
| Daily climate and pollutant variables (unit) | Children: of age [RR (95% CI)] | Adults: of age [RR (95% CI)] | Older adults: of age [RR (95% CI)] | |||
|---|---|---|---|---|---|---|
| Thunderstorm () | Non-thunderstorm () | Thunderstorm () | Non-thunderstorm () | Thunderstorm () | Non-thunderstorm () | |
| Precipitation () | 1.270 (1.056, 1.527) | 1.044 (0.876, 1.244) | 1.061 (0.880, 1.279) | 1.020 (0.843, 1.236) | 0.887 (0.572, 1.375) | 1.273 (0.830, 1.951) |
| Temperature drop (1°C) | 1.011 (0.996, 1.026) | 1.004 (1.000, 1.009) | 1.014 (0.998, 1.029) | 0.996 (0.992, 1.001) | 0.977 (0.942, 1.011) | 1.005 (0.994, 1.015) |
| Pressure (1 kPa) | 1.042 (0.949, 1.144) | 0.983 (0.950, 1.017) | 0.968 (0.879, 1.067) | 1.010 (0.974, 1.048) | 1.061 (0.857, 1.314) | 0.990 (0.911, 1.076) |
| (1 ppb) | 1.001 (0.997, 1.004) | 1.001 (0.999, 1.002) | 1.001 (0.998, 1.005) | 1.002 (1.001, 1.004) | 1.000 (0.992, 1.008) | 1.002 (0.998, 1.006) |
| () | 0.997 (0.987, 1.007) | 1.004 (1.000, 1.008) | 0.995 (0.985, 1.005) | 0.995 (0.991, 1.000) | 0.985 (0.963, 1.007) | 0.991 (0.981, 1.001) |
Note: Time-series quasi-Poisson regression models were adjusted for long-term trend with natural cubic spline (), parish, Louisiana holidays, day of week, and season (summer vs. non-summer); 1,351 ED visits were deleted from the regression analyses owing to missingness in lightning data. CI, confidence interval; ED, emergency department; , ozone; , particulate matter in aerodynamic diameter (fine particulate matter); RR, relative risk.
Daily maximum level was significantly associated with higher risk (0.2% per change; ; 95% CI: 1.001, 1.003) of asthma-related ED visits on non-thunderstorm days for adults, but this association was not observed for thunderstorm days. Daily maximum level was positively associated with risk of asthma-related ED visits for children but negatively with risk for adults and older adults only on non-thunderstorm days (Table 2). The regression models indicated that risk of asthma-related ED visits was significantly higher in non-summer seasons than summer (data not shown). Precipitation or temperature on the thunderstorm days did not influence asthma-related ED visits on the next day without thunderstorm (Table 1). The RRs from the full and reduced models using different strata categorized by only lightning or no-lightning days (i.e., excluding precipitation from the definition for a thunderstorm day) were similar to those of thunderstorm day models (Table S6). Daily mean pressure and horizontal wind speed did not have significant effects and did not alter the associations of precipitation or temperature with asthma-related ED visits (Tables S7 and S8).
Discussion
On thunderstorm days, a higher daily precipitation rate was associated with a 27.0% higher risk of asthma-related ED visits for children ( of age) but not for other age groups in Louisiana; however, there was no such association for any age group on non-thunderstorm days. Our finding of the positive association of precipitation with asthma-related ED visits during only thunderstorm days appears supported by the proposed mechanism of thunderstorm asthma. The mechanism suggests that at the initial stage of thunderstorm development, whole pollen grains on the ground level can be carried to the cloud base by ascending air parcels. The pollen grains then frequently rupture upon contacting moisture in the cloud, releasing respirable pollen fragments with allergens in much higher concentration than the concentration of pollen grains themselves.28–30 These bioaerosols could be positively charged by lightning activity and carried back down to ground level by precipitation and descending cool air during a thunderstorm.2,11,13,29 Precipitation itself can also influence atmospheric concentrations of pollens and mold spores.2 Grass pollen concentration was positively associated with asthma-related ED visits after a thunderstorm in London in June 1994.11,13 Grundstein et al. reported a positive association of rain on days with thunderstorms with asthma-related ED visits in the Atlanta area, Georgia.31 Positively charged respirable airborne allergens can be more readily deposited in the lungs than uncharged particles13,26 and thus potentially enhance immune responses.32 We observed that precipitation rates were higher on thunderstorm days than non-thunderstorm days, and the more severe a thunderstorm is, the more likely it is to produce heavier precipitation.9 Therefore, more precipitation accompanied by stronger downdrafts during severe thunderstorms might result in higher concentrations of charged respirable bioaerosols at ground level.
We also found that a lower mean temperature was associated, independent of precipitation, with a higher risk of asthma-related ED visits on thunderstorm days. Our finding may be partly explained by an inverse relationship between ambient temperature and asthma hospitalization or ED visits previously reported.33–35 In a retrospective electronic chart review of adults with asthma-related ED visits, May et al. found that acute asthma exacerbations were negatively correlated with monthly mean temperature in the Washington, DC, area during June 2005–May 2006.33 Lam et al. reported from a study of age-specific effects of meteorological factors on asthma hospitalization that adults were most sensitive to temperature and that young children ( of age) were least sensitive.36 The higher asthma-related ED visits on days with lower temperature might be the result of general temperature effects on airway injury.37,38
However, our finding of much stronger negative association of temperature with asthma ED visits on thunderstorm days than non-thunderstorm days suggests that the association might be better explained by the potential association of asthma exacerbation with the thunderstorm-associated rapid temperature drop.5,39 This sudden temperature drop results from a cooler downdraft during thunderstorms and evaporative cooling after precipitation.9 A case study in 1994 reported that increased asthma-related ED visits 6 h after a thunderstorm in London, England, was associated with the sudden temperature drop [ ()].11 Emergency calls in Melbourne, Australia, in 2016, spiked at seven times the regular rate, 5 h after the sudden temperature drop [ ()] during a thunderstorm.26 Sudden temperature drops in the airways can trigger asthma symptoms.40 A recent review found that the effect of sudden temperature drops on an increased risk of asthma attacks is stronger in lower latitude regions with higher baseline temperature,35 which might be the case in Louisiana. From our data, we observed a negative correlation between precipitation rate and daily mean temperature on thunderstorm days. The larger sudden temperature drop during more severe thunderstorms might have contributed to further lowering the daily mean temperature.41
Our finding that similarly strong associations of temperature or precipitation with asthma ED visits were not observed for non-thunderstorm days may indicate that the excessive asthma-related ED visits associated with precipitation and temperature are likely a piece of the thunderstorm asthma phenomenon. Crude attributable fractions estimated from the RRs based upon other research42 indicated that more asthma ED visits could be attributable to a () higher precipitation rate. Further, more asthma ED visits could be attributable, independent of precipitation effect, to a 1°C lower daily average temperature on the thunderstorm days during the study period. Although we were unable to clearly tease out individual mechanisms of thunderstorm asthma hypothesized by other researchers, those hypothetical mechanisms discussed earlier agreed with the findings from our population study in that a) the increase in asthma-related ED visits may be the result of exposure to increased concentrations of aeroallergens by precipitation and lightning, or b) the meteorological condition itself, such as temperature, may be also involved in the mechanisms. These higher risks were observed mainly among children ( of age) and adults ( of age), but not by older adults ( of age). One possible explanation for this finding could be different characteristics of asthma in older adult populations than children or younger adult populations (e.g., nonatopic or neutrophilic asthma is more common in older adults).43 The Melbourne event was also associated with an increase in ED visits among those 20–59 years of age. The Australian researchers noted that this finding deviated from their typical U-shaped curve that is composed mainly of children and older adults.44 Another speculation is that older adults might have learned to stay inside to prevent symptoms on thunderstorm days, whereas children and younger adults might have been caught off-guard and not near rescue inhalers, which could have prevented their ED visits. Regardless of the reason, overwhelming the health care system during severe weather with patients that do not routinely seek ED care for their asthma could disproportionately affect some vulnerable populations. In the United States, neighborhood poverty is associated with higher ED visits and hospitalizations among children with asthma.45
The associations of precipitation and temperature with asthma exacerbation on thunderstorm days were not carried over to the following non-thunderstorm day. This finding is consistent with the report that seven times more emergency ambulance calls than normally expected occurred during a late afternoon thunderstorm in Melbourne, Australia, in 2016.26 It is also consistent with the 15% higher rate of asthma-related ED visits in children on thunderstorm days compared with non-thunderstorm days in the Ottawa region, Canada, from 1993 through 1997.12,26 Thunderstorms in the southern United States around the Gulf of Mexico frequently occur in the afternoon.14 Further, a study of thunderstorm-related asthma in London found a 3- to 6-h–lag effect on increased asthma-related ED visits after a thunderstorm.11 Considering that a thunderstorm is usually a short-term phenomenon frequently occurring in the afternoon, and that it may have several-hour–lag effect, the same-day effects of thunderstorm-associated precipitation and temperature on asthma-related ED visits in our study seem to be justified.
We found a significant positive association of with asthma-related ED visits only on days without thunderstorms. We also found a negative association between concentrations of thunderstorm days and asthma-related ED visits of the next non-thunderstorm days. This might be associated with precipitation decreasing ambient PM during thunderstorms.39 A study reported decreased fine PM of on a thunderstorm day.41 However, may increase lightning activity46 and dust particles may modify the amount of precipitation through changing atmospheric temperatures and concentrations of potential condensation nuclei during thunderstorm formation.47
Our study used 68,800 parish-days in Louisiana, using high-resolution NARR climate data for 3 y, allowing us to overcome the limitations of previously published case or small-scale studies. Although analyses of data with time-stamped thunderstorm events, temperature drops, and precipitation, along with time-stamped asthma-related ED visits, may provide stronger evidence of the effects of thunderstorms on asthma exacerbation, such data would be extremely difficult to obtain. Analysis of multiple state data sets in different climate zones could help confirm similar effects of thunderstorm-associated climate factors on asthma attacks in other climate zones. Adding more years of health and climate data could have increased the reliability of the study findings; however, adding additional years would be an extremely time-intensive process. In addition, the sample size (68,800 parish-days and 63,789 asthma-related ED visits) used in our study provided enough power to demonstrate the associations of meteorological conditions with asthma-related ED visits by days with and without thunderstorms. We could not obtain pollen or mold concentration data in Louisiana for the study period because there were no such data available for all parishes at the beginning of the study. In addition, we acknowledge that there could be other man-made or natural events (e.g., the well-known examples of soybean loading in the New Orleans harbor in the 1950s and 1960s) that can lead to spikes in ED visits.48 Another limitation might be that we adjusted the models for parish but did not consider actual geographic clustering of meteorological factors that may differ by parish. We also note that patients might be exposed to environmental triggers in multiple locations, but geographic information in our data set was limited to residence, an inherent limitation of our ED visits data source; discrepancies between asthma trigger and residence location could have resulted in misclassification. However, these misclassifications in exposure were likely to be random, which might have attenuated the effect size, implying the actual effects might have been stronger without these misclassifications. However, even with this potential attenuation, we identified significant associations between temperature or precipitation and asthma-related ED visits. Last, over the study period, tropical storms have affected parishes in Louisiana during the summer months (May–September; Figure 2), including Tropical Storm Bonnie and Tropical Depression 5 in 2010, Tropical Storm Lee in 2011, and Tropical Storm Debby and Hurricane Isaac in 2012.49 These tropical storms could have affected movement patterns of state residents in the affected area as a result of voluntary or mandatory evacuation, which might have changed the routine seasonal patterns of exposures and asthma ED visits.
In conclusion, we found that a higher daily mean precipitation rate and lower temperature on thunderstorm days were significantly associated with the higher risks of asthma-related ED visits in children and in adults, respectively, while we did not observe the same strong associations during non-thunderstorm days. Asthma exacerbations experienced by children and adults appeared to occur the same day of the thunderstorm. This real-time phenomenon poses a particular challenge to public health practitioners in being able to disseminate messaging related to thunderstorm asthma. However, using meteorological (weather forecast) data to predict high-risk days for thunderstorm asthma may be useful for establishing early warning systems for people with asthma. Such systems will help people with asthma be aware of the risks, take precautions (such as staying indoors), and keep their rescue inhaler medication handy. It will also help EDs, especially in hospitals in metropolitan areas with large populations, be prepared for potential spikes in asthma attacks on forecasted thunderstorm days with heavy precipitation, lightning, and a large, sudden temperature drop. During severe thunderstorm days, prudent measures—such as sufficiently stocking emergency medication and supplies for treating asthma—should be considered. In addition, based on our results, we propose that established asthma surveillance systems regularly collect meteorological and environmental information, in addition to health information, to further the research into the individual risk factors for thunderstorm asthma.
Supplementary Material
Acknowledgments
We are grateful for the National Oceanic and Atmospheric Administration’s National Centers for Environmental Information for providing access to lightning data. We thank M. Shin and D. Blackley for their technical review of the manuscript and C. Hamilton for her editing and proofreading.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Dabrera G, Murray V, Emberlin J, Ayres JG, Collier C, Clewlow Y, et al. 2013. Thunderstorm asthma: an overview of the evidence base and implications for public health advice. QJM 106(3):207–217, PMID: , 10.1093/qjmed/hcs234. [DOI] [PubMed] [Google Scholar]
- 2.Grundstein A, Sarnat SE. 2009. Meteorological mechanisms explaining thunderstorm‐related asthma. Geogr Compass 3(1):45–63, 10.1111/j.1749-8198.2008.00195.x. [DOI] [Google Scholar]
- 3.Kevat A. 2020. Thunderstorm asthma: looking back and looking forward. J Asthma Allergy 13:293–299, PMID: , 10.2147/JAA.S265697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Packe GE, Archer PStJ, Ayres JG. 1983. Asthma and the weather. Lancet 322(8344):281, 10.1016/S0140-6736(83)90260-X. [DOI] [PubMed] [Google Scholar]
- 5.Packe GE, Ayres JG. 1985. Asthma outbreak during a thunderstorm. Lancet 2(8448):199–204, PMID: , 10.1016/S0140-6736(85)91510-7. [DOI] [PubMed] [Google Scholar]
- 6.Alderman PM, Sloan JP, Basran GS. 1986. Asthma and thunderstorms. Arch Emerg Med 3(4):260–262, PMID: , 10.1136/emj.3.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Amato G, Annesi Maesano I, Molino A, Vitale C, D’Amato M. 2017. Thunderstorm-related asthma attacks. J Allergy Clin Immunol 139(6):1786–1787, PMID: , 10.1016/j.jaci.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 8.D’Amato G, Holgate ST, Pawankar R, Ledford DK, Cecchi L, Al-Ahmad M, et al. 2015. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organ J 8(1):25, PMID: , 10.1186/s40413-015-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahrens CD, Samson P. 2011. Thunderstorms. In: Extreme Weather & Climate. Ahrens CD, Samson P, eds. Belmont, CA: Brooks/Cole, 268–297. [Google Scholar]
- 10.Anderson BT, Strahler A. 2008. Thunderstorms and tornadoes. In: Visualizing Weather and Climate. Hoboken, NJ: John Wiley & Sons, 270–275. [Google Scholar]
- 11.Celenza A, Fothergill J, Kupek E, Shaw RJ. 1996. Thunderstorm associated asthma: a detailed analysis of environmental factors. BMJ 312(7031):604–607, PMID: , 10.1136/bmj.312.7031.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dales RE, Cakmak S, Judek S, Dann T, Coates F, Brook JR, et al. 2003. The role of fungal spores in thunderstorm asthma. Chest 123(3):745–750, PMID: , 10.1378/chest.123.3.745. [DOI] [PubMed] [Google Scholar]
- 13.O’Leary M, Koolpiruck D, Balachandran W, Emberlin J, Lewis R. 2005. The role of electrostatic charge accumulated by respirable sized allergens with regard to thunderstorm asthma. In: Proceedings of the Conference Record of the 2005 Industry Applications Conference, 2005. Vol. 2. 2–6 October 2005. Kowloon, Hong Kong: IEEE Industry Applications Society, 778–783. [Google Scholar]
- 14.NOAA National Severe Storms Laboratory. n.d. Severe weather 101—thunderstorms. https://www.nssl.noaa.gov/education/svrwx101/thunderstorms/ [accessed 8 February 2021].
- 15.Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. 2021. Asthma surveillance—United States, 2006–2018. MMWR Surveill Summ 70(5):1–32, PMID: , 10.15585/mmwr.ss7005a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC (Centers for Disease Control and Prevention). 2013. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). http://www.cdc.gov/nchs/icd/icd9cm.htm [accessed 1 March 2014].
- 17.CDC. n.d. National Environmental Public Health Tracking Network. https://www.cdc.gov/ephtracking [accessed 18 April 2018].
- 18.Mesinger F, DiMego G, Kalnay E, Mitchell K, Shafran PC, Ebisuzaki W, et al. 2006. North American regional reanalysis. Bull Amer Meteor Soc 87(3):343–360, 10.1175/BAMS-87-3-343. [DOI] [Google Scholar]
- 19.NOAA Physical Sciences Laboratory. n.d. Gridded Climate Dataset. NCEP North American Regional Reanalysis. https://psl.noaa.gov/data/gridded/help.html#cite [accessed 18 April 2017].
- 20.Global Hydrometeorology Research Center. n.d. National Lightning Detection Network (NLDN). https://ghrc.nsstc.nasa.gov/home/lightning/index/data_nldn [accessed 18 June 2017].
- 21.NOAA National Centers for Environmental Information. n.d. Climate Data Online. https://www.ncdc.noaa.gov/cdo-web/ [accessed 15 August 2018].
- 22.Berrocal VJ, Gelfand AE, Holland DM. 2012. Space–time data fusion under error in computer model output: an application to modeling air quality. Biometrics 68(3):837–848, PMID: , 10.1111/j.1541-0420.2011.01725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strosnider HM, Chang HH, Darrow LA, Liu Y, Vaidyanathan A, Strickland MJ. 2019. Age-specific associations of ozone and fine particulate matter with respiratory emergency department visits in the United States. Am J Respir Crit Care Med 199(7):882–890, PMID: , 10.1164/rccm.201806-1147OC. [DOI] [PubMed] [Google Scholar]
- 24.Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. 2013. Time series regression studies in environmental epidemiology. Int J Epidemiol 42(4):1187–1195, PMID: , 10.1093/ije/dyt092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Smith MJ, Goodchild MF, Longley PA. 2018. Geospatial Analysis: A Comprehensive Guide to Principles Techniques and Software Tools. Winchelsea, England: Winchelsea Press. [Google Scholar]
- 26.Redmayne M. 2018. A proposed explanation for thunderstorm asthma and leukemia risk near high-voltage power lines: a supported hypothesis. Electromagn Biol Med 37(2):57–65, PMID: , 10.1080/15368378.2018.1466309. [DOI] [PubMed] [Google Scholar]
- 27.Tukey JW. 1949. Comparing individual means in the analysis of variance. Biometrics 5(2):99–114, PMID: , 10.2307/3001913. [DOI] [PubMed] [Google Scholar]
- 28.Abou Chakra O, Rogerieux F, Poncet P, Sutra JP, Peltre G, Sénéchal H, et al. 2011. Ability of pollen cytoplasmic granules to induce biased allergic responses in a rat model. Int Arch Allergy Immunol 154(2):128–136, PMID: , 10.1159/000320227. [DOI] [PubMed] [Google Scholar]
- 29.D’Amato G, Vitale C, D’Amato M, Cecchi L, Liccardi G, Molino A, et al. 2016. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy 46(3):390–396, PMID: , 10.1111/cea.12709. [DOI] [PubMed] [Google Scholar]
- 30.Taylor PE, Flagan RC, Valenta R, Glovsky MM. 2002. Release of allergens as respirable aerosols: a link between grass pollen and asthma. J Allergy Clin Immunol 109(1):51–56, PMID: , 10.1067/mai.2002.120759. [DOI] [PubMed] [Google Scholar]
- 31.Grundstein A, Sarnat SE, Klein M, Shepherd M, Naeher L, Mote T. 2008. Thunderstorm associated asthma in Atlanta, Georgia. Thorax 63(7):659–660, PMID: , 10.1136/thx.2007.092882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Willoughby DA, Baily G. 1994. Asthma increase, summer, 1994. Lancet 344(8919):413, PMID: , 10.1016/S0140-6736(94)91442-7. [DOI] [PubMed] [Google Scholar]
- 33.May L, Carim M, Yadav K. 2011. Adult asthma exacerbations and environmental triggers: a retrospective review of ED visits using an electronic medical record. Am J Emerg Med 29(9):1074–1082, PMID: , 10.1016/j.ajem.2010.06.034. [DOI] [PubMed] [Google Scholar]
- 34.Zhang Y, Peng L, Kan H, Xu J, Chen R, Liu Y, et al. 2014. Effects of meteorological factors on daily hospital admissions for asthma in adults: a time-series analysis. PLoS One 9(7):e102475, PMID: , 10.1371/journal.pone.0102475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cong X, Xu X, Zhang Y, Wang Q, Xu L, Huo X. 2017. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res Int 24(28):22535–22546, PMID: , 10.1007/s11356-017-9914-4. [DOI] [PubMed] [Google Scholar]
- 36.Lam HCY, Li AM, Chan EYY, Goggins WB III.. 2016. The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: a time–series study. Thorax 71(12):1097–1109, PMID: , 10.1136/thoraxjnl-2015-208054. [DOI] [PubMed] [Google Scholar]
- 37.Anderson SD, Kippelen P. 2012. Assessment and prevention of exercise-induced bronchoconstriction. Br J Sports Med 46(6):391–396, PMID: , 10.1136/bjsports-2011-090810. [DOI] [PubMed] [Google Scholar]
- 38.Kippelen P, Fitch KD, Anderson SD, Bougault V, Boulet LP, Rundell KW, et al. 2012. Respiratory health of elite athletes—preventing airway injury: a critical review. Br J Sports Med 46(7):471–476, PMID: , 10.1136/bjsports-2012-091056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weber RW. 2003. Meteorologic variables in aerobiology. Immunol Allergy Clin North Am 23(3):411–422, PMID: , 10.1016/S0889-8561(03)00062-6. [DOI] [PubMed] [Google Scholar]
- 40.Koskela HO. 2007. Cold air-provoked respiratory symptoms: the mechanisms and management. Int J Circumpolar Health 66(2):91–100, PMID: , 10.3402/ijch.v66i2.18237. [DOI] [PubMed] [Google Scholar]
- 41.Zou E, Worsham C, Miller NH, Molitor D, Reif J, Jena AB. 2020. Emergency visits for thunderstorm-related respiratory illnesses among older adults. JAMA Intern Med 180(9):1248–1250, PMID: , 10.1001/jamainternmed.2020.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gasparrini A, Leone M. 2014. Attributable risk from distributed lag models. BMC Med Res Methodol 14:55, PMID: , 10.1186/1471-2288-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Crisford H, Sapey E, Rogers GB, Taylor S, Nagakumar P, Lokwani R, et al. 2021. Neutrophils in asthma: the good, the bad and the bacteria. Thorax 76(8):835–844, PMID: , 10.1136/thoraxjnl-2020-215986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thien F, Beggs PJ, Csutoros D, Darvall J, Hew M, Davies JM, et al. 2018. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health 2(6):e255–e263, PMID: , 10.1016/S2542-5196(18)30120-7. [DOI] [PubMed] [Google Scholar]
- 45.Keet CA, Matsui EC, McCormack MC, Peng RD. 2017. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol 140(3):822–827, PMID: , 10.1016/j.jaci.2017.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chowdhuri I, Pal SC, Saha A, Chakrabortty R, Ghosh M, Roy P. 2020. Significant decrease of lightning activities during COVID-19 lockdown period over Kolkata megacity in India. Sci Total Environ 747:141321, PMID: , 10.1016/j.scitotenv.2020.141321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goudie AS, Middleton NJ. 2001. Saharan dust storms: nature and consequences. Earth Sci Rev 56(1–4):179–204, 10.1016/S0012-8252(01)00067-8. [DOI] [Google Scholar]
- 48.White MC, Etzel RA, Olson DR, Goldstein IF. 1997. Reexamination of epidemic asthma in New Orleans, Louisiana, in relation to the presence of soy at the harbor. Am J Epidemiol 145(5):432–438, PMID: , 10.1093/oxfordjournals.aje.a009125. [DOI] [PubMed] [Google Scholar]
- 49.National Hurricane Center. Tropical Cyclone Reports. n.d. https://www.nhc.noaa.gov/data/tcr/index.php?season=2010&basin=atl [accessed 11 January 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.