Abstract
Background
Assisted living (AL) is the largest residential long‐term care provider in the United States, including for persons with Alzheimer's disease and related dementias. Despite recognizing the challenge of infection control for persons with dementia, this study of 119 AL communities is the first to describe dementia‐relevant COVID‐19 infection control across different types of AL communities, and to discuss implications for the future.
Methods
From a parent study sampling frame of 244 AL communities across seven states, 119 administrators provided data about COVID‐19 infection control practices and resident behaviors. Data were collected from July 2020 through September 2021. Communities were differentiated based on the presence of beds/units dedicated for persons living with dementia, as being either dementia‐specific, mixed, or integrated. Data obtained from administrators related to feasibility of implementing seven infection control practices, and the extent to which residents themselves practiced infection prevention. Analyses compared practices across the three community types.
Results
Less than half of administrators found it feasible to close indoor common areas, all community types reported a challenge organizing group activities for safe distancing, and more than half of residents with dementia did not wear a face covering or maintain physical distance from other residents when indicated. Dementia‐specific AL communities were generally the most challenged with infection control during COVID‐19.
Conclusion
All AL community types experienced infection control challenges, more so in dementia‐specific communities (which generally provide care to persons with more advanced dementia and have fewer private beds). Results indicate a need to bolster infection prevention capacity when caring for this especially vulnerable population, and have implications for care in nursing homes as well.
Keywords: assisted living, COVID‐19, dementia, infection control
Key points
Assisted living is the primary provider of residential long‐term care for persons living with dementia, but during the COVID‐19 pandemic, assisted living administrators across a range of community types found it challenging to implement infection control practices for residents with dementia.
Less than half of administrators found it feasible to close indoor common areas, all community types reported a challenge organizing group activities for safe distancing, and more than half of residents with dementia did not wear a face covering or maintain physical distance from other residents when indicated.
Dementia‐specific assisted living communities were generally the most challenged with infection control during COVID‐19.
Why does this paper matter?
Even after the wake of COVID‐19, data indicate the need to bolster infection control capabilities when providing care for assisted living residents with dementia.
INTRODUCTION
COVID‐19 had an enormous impact on older adults residing in long‐term care settings. Most concern focused on nursing homes, with less attention paid to assisted living (AL). Although AL communities are not licensed as healthcare settings, they provide care for a population with many of the same underlying conditions as nursing homes. More so, AL is the primary residential long‐term care provider in the United States, including for persons with Alzheimer's disease and related dementias 1 : 42% of residents have a dementia diagnosis, and as many as 38% of the remainder meet diagnostic criteria for probable dementia. 2 Given their COVID‐19 risks, it is not surprising that AL mortality rates in 2020 were 17% higher than in 2019. 3
The ability to implement infection control practices for residents with dementia is critical. It is of special importance in congregate settings due to ongoing contact with others, and is especially challenging when social distancing, mask wearing, and other preventive practices are hindered among those who do not understand the related risk and need. For these reasons, the fact that no research has yet examined COVID‐19 infection control practices for residents with dementia in AL is a critical gap in guiding future policy and practice—especially because many of the recommendations issued during the pandemic were relevant to AL. 4 , 5
An ongoing seven‐state study of dementia, medical, and mental health care in AL provided the backdrop to conduct a supplemental study of COVID‐19. It also allowed examination of infection control practices across the three types of AL communities that provide care for residents with dementia: (a) dementia‐specific communities (10% of communities, which provide care only for persons with dementia); (b) mixed communities (12% of communities, which include a dementia unit and non‐dementia dedicated beds); and (c) integrated communities (78% of communities, in which residents with dementia reside alongside those without dementia). 6 Although only 14% of residents overall are in dementia special care communities/units—meaning the majority of AL residents with dementia do not reside there—they care for 46% of residents with severe cognitive impairment. 7 Therefore, understanding infection control experiences across all three setting types is important.
METHODS
This supplemental COVID‐19 study drew on an initial pool of 250 AL communities randomly sampled proportionate to size that were participating in an ongoing study of dementia care in AL, details of which have been described elsewhere. 8 , 9 , 10 Specifically, a parent study initiated in 2015 recruited a random sample of AL communities across seven states, with the states selected due to regional variability in dementia care practices (AR, LA, NJ, NY, OK, PA, TX). Because the parent study entailed on‐site data collection, two geographic regions were constructed in each state to represent the entire state in regard to demographic variables used in other work: per capita income, percent of population below the poverty level, percent of population non‐White, unemployment rate, percent of population aged 65 and older; number of primary care physicians, and hospital and nursing home beds per person 65 and older. 11 In AR, LA, NJ, and OK, the regions included the entire state. Eligible AL communities provided residential, long‐term care to more than four adults and largely served a population of older adults (N = 1624). With the intent to recruit 35–40 sites per state (total N = 250), communities were randomly sampled proportionate to the size and invited to participate. The supplemental study recruited data from the 244 communities (of the original 250) still in operation in 2019; of those, 119 provided COVID‐19 data. Data were collected July 2020 through September 2021.
Interviews were conducted with the AL administrator regarding community type (dementia‐specific, mixed, integrated), the feasibility of implementing seven infection control practices, and the extent to which residents themselves practiced infection prevention (wearing a face covering, maintaining six‐foot distance). Additional questions related to COVID‐19 outbreaks and descriptive information about the communities. Questions were contextualized as being “specifically about care for residents with dementia.” Additional data used to describe communities were derived from resident‐level chart data obtained during on‐site visits, aggregated to the community (i.e., percent of residents with dementia diagnosis, behavioral symptoms, female, white). The University of North Carolina at Chapel Hill Institutional Review Board approved all procedures for the parent and supplement studies.
Analyses compared COVID‐19 practices across the three community types using Pearson chi‐square tests to evaluate omnibus differences with statistical significance defined as p < 0.05. When the overall test was significant, comparisons of pairs of types (i.e., dementia‐specific vs mixed, dementia‐specific vs integrated, mixed vs integrated) were tested with chi‐square tests using a Bonferonni adjustment whereby p ≤ 0.017 (i.e., 0.05/3) was set as the significance level. Finally, Kruskal–Wallis tests were used to compare reported infection control behaviors across community types (p < 0.05).
RESULTS
The AL administrators who participated in the project averaged 51 years of age; they were largely white (83%) and female (81%), and 4% were Hispanic/Latino. On average, the 119 AL communities had 49 beds (standard deviation [SD] = 27), ranging from 44 to 45 beds in dementia‐specific and integrated communities to 65 beds in mixed communities. Two‐thirds (67%, SD = 34%) were in private rooms; dementia‐specific communities had fewest beds in private rooms (55% vs 68–71%) but a more favorable staffing ratio (9 residents/care aide vs 11–15 in the other community types). Overall, 41% of residents had a dementia diagnosis (SD = 28%), with 99%, 47%, and 26% in dementia‐specific, mixed, and integrated communities, respectively; the proportion who required attention for behaviors followed a similar pattern. Fewer residents were receiving Medicaid (13% in total, ranging from 1% in dementia specific communities to 10% and 17% in mixed and integrated communities, respectively). The mean female case‐mix was 74% (SD = 11%) and 95% (SD = 12%) were white. Administrators reported that the majority (88%) of communities had a COVID‐19 case (69% had a COVID‐19 case among residents, and 87% had a COVID‐19 case among staff) before data collection.
The percentage of AL administrators reporting the implementation of COVID‐19 infection control practices as feasible varied by practice and community type (Table 1). More than half of administrators did not consider it feasible to close all common indoor areas, and in no case did at least 90% of administrators organize group activities for safe distancing, provide additional mental health support, or assure that residents with COVID‐19 were in a private room. Examining differences by community type, serving all residents meals in their rooms and having residents with COVID‐19 self‐isolate was considered least feasible in dementia‐specific communities, and statistically significantly less so than in integrated communities (21% considered this feasible); however, administrators from dementia‐specific communities did more often consider it feasible to cluster residents with COVID‐19 (79% vs 48–68%; pair‐wise comparisons not significant).
TABLE 1.
Administrator reported feasibility of COVID‐19 infection practices for residents with dementia, by community type (N = 119)
| All community types (N = 119) | Dementia‐specific N = 14, N (%) | Mixed with dementia unit a N = 28, N (%) | Integrated b N = 77, N (%) | Omnibus test p‐value (Pearson chi‐square) | |
|---|---|---|---|---|---|
| Serve all residents meals in their rooms | 66 (57%) | 3 (21%) | 12 (43%) | 51 (70%) | 0.001 c |
| Close all indoor common areas | 54 (47%) | 5 (36%) | 15 (54%) | 34 (47%) | 0.55 |
| Organize group activities that allow for safe physical distancing | 88 (77%) | 8 (57%) | 21 (75%) | 59 (82%) | 0.13 |
| Provide additional mental health support for residents | 68 (60%) | 5 (36%) | 19 (68%) | 44 (61%) | 0.14 |
| Assure that residents with COVID‐19 are in a private room | 91 (79%) | 8 (57%) | 24 (86%) | 59 (81%) | 0.10 |
| Cluster residents with COVID‐19 | 65 (57%) | 11 (79%) | 19 (68%) | 35 (48%) | 0.04 |
| Have residents with COVID‐19 self‐isolate | 61 (53%) | 3 (21%) | 15 (54%) | 43 (59%) | 0.04 c |
Note: Due to missing data, the number of respondents for any given item is 114–115.
Assisted living communities that have dementia‐designated beds as well as residents without dementia.
Assisted living communities that do not have dementia‐designated beds; residents with dementia are integrated with residents without dementia. Data are missing for one community related to organizing group activities and providing additional mental health support.
Pairwise comparison of dementia‐specific and integrated communities statistically significant (p ≤ 0.017).
As shown in Table 2 and Figure 1A and B, the behaviors of residents with dementia indicated challenges wearing a face covering and maintaining social distance. In the 14 dementia‐specific communities, only 1 or 2 of all administrators reported that half or more residents did so, which for face covering was statistically significantly fewer than all other community types. In no case did a majority of residents practice either behavior, regardless of community type.
TABLE 2.
Administrator reported infection control behaviors, by residents with dementia and by community type (N = 119)
| Estimated proportion of residents | |||||
|---|---|---|---|---|---|
| None | Less than half | About half | More than half | All | |
| Proportion of residents who wore a face covering at all times when within 6‐feet of someone else* | |||||
| Dementia‐specific (N = 14) | 7 (50%) | 6 (43%) | 1 (7%) | 0 (0%) | 0 (0%) |
| Mixed with dementia unit a (N = 28) | 9 (32%) | 8 (29%) | 3 (11%) | 4 (14%) | 4 (14%) |
| Integrated b (N = 73) | 16 (22%) | 22 (30%) | 10 (14%) | 15 (21%) | 10 (14%) |
| Proportion of residents who maintained a 6‐foot distance from other residents at all times** | |||||
| Dementia‐specific (N = 14) | 6 (43%) | 6 (43%) | 0 (0%) | 1 (7%) | 1 (7%) |
| Mixed with dementia unit a (N = 28) | 9 (32%) | 7 (25%) | 4 (14%) | 4 (14%) | 4 (14%) |
| Integrated b (N = 73) | 18 (25%) | 22 (30%) | 7 (10%) | 14 (19%) | 12 (16%) |
Note: Due to missing data, the number of respondents for any given item is 115.
Note: Kruskal–Wallis tests: *p = 0.013; **p = 0.15.
Assisted living communities that have dementia‐designated beds as well as residents without dementia.
Assisted living communities that do not have dementia‐designated beds; residents with dementia are integrated with residents without dementia.
FIGURE 1.
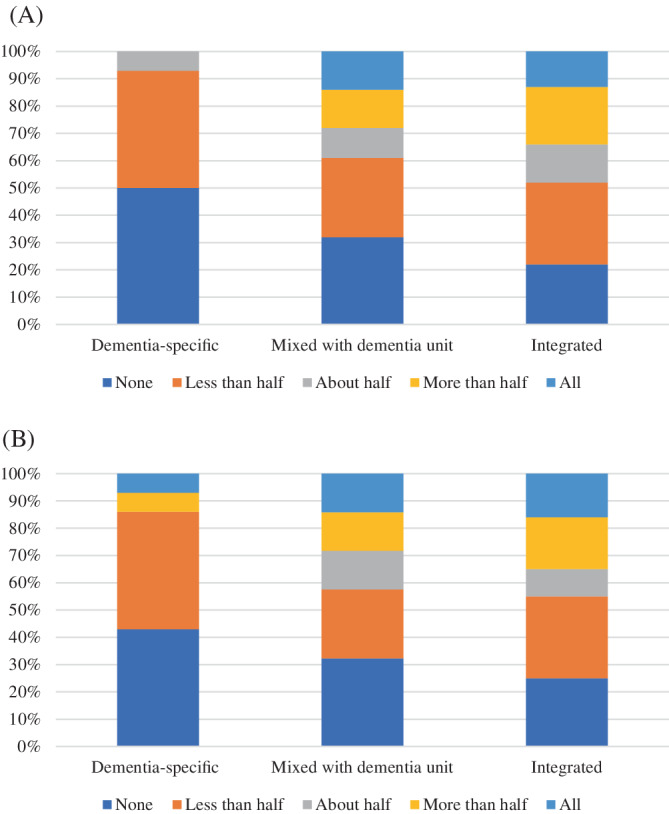
Percent of residents with dementia who practiced infection control, by community type. (A) Wore a face covering. (B) Maintained physical distance.
DISCUSSION
Data regarding COVID‐19 infection control practices for residents with dementia in AL—the largest provider of residential dementia care in the United States—indicate that no communities nor residents implemented every practice. The fact that dementia‐specific communities and their residents were generally the most challenged is consistent with the fact that 99% of their residents had a dementia diagnosis compared with 47% and 26% of residents in mixed and integrated communities, respectively. For that very reason, there is cause to consider the practice‐ and policy‐relevant implications of these findings.
Administrators in dementia‐specific communities found it least feasible to serve all residents meals in their rooms and isolate residents with COVID‐19, which may relate to the fact that these communities had the lowest proportion of beds in private rooms (55% compared with 71% and 68% in mixed and integrated communities, respectively). In the interest of infection control for AL residents who are least able to care for themselves, it is worth reconsidering the physical structure of these communities. Structural modifications could include more private rooms and enlarged shared spaces (i.e., recent findings indicate more space relates to lower COVID‐19 cases and deaths in nursing homes, and that smaller overall models of care—such as the Green House model—may be beneficial to care). 12 , 13 Because dementia‐specific communities have fewer residents on Medicaid (reported above) and because they charge higher rates than other communities (roughly $800–$1000 more in 2010 dollars) 7 it seems feasible that proportionately, they have resources available for restructuring. Additional staffing might also be beneficial, but these communities already have more favorable staffing ratios than other community types, and it may not be feasible to further increase their numbers given workforce challenges.
Overall, the data suggest bolstering infection control capabilities for persons with dementia across AL community types. Less than half of administrators found it feasible to close indoor common areas, and all community types reported a challenge organizing group activities for safe distancing. While the lack of physical distancing is a detriment to infection control, it is likely advantageous in terms of reducing isolation. In addition, administrators reported that masking and physical distancing were not common among residents with dementia. New infection control policies and related technology might be helpful in this regard (e.g., financing for air filtration systems, e‐health visits), given that numerous states lack AL infection policies, and when they do, they vary greatly across and within states. 14
The data in this study were obtained from statewide samples of AL communities across seven states, and while the findings are expected to be generalizable due to the face validity of challenges in infection control for persons with dementia, the specific statistics from this sample of 119 communities are not presumed to indicate national averages (further noted because one large chain of AL communities was not represented in the sample). In addition, larger samples are necessary to conduct analyses by key subgroups such as those specific to race, gender, and socioeconomic status. Finally, because data collection was cross‐sectional and obtained at various times across the 119 communities, experiences may have changed over various waves of COVID‐19; however, data collection did not begin until 5 months into the pandemic, suggesting that all participants grappled with the infection disease practices examined in this study and were well aware of feasibility and resident behaviors. That said, respondent recall may have introduced some error, and the reports were not verified for accuracy.
CONCLUSION
Persons with dementia are at increased risk of COVID‐19 and related hospitalization and mortality. 15 This study documented challenges implementing infection control practices for residents with dementia (e.g., closing indoor areas, maintaining physical distancing, wearing face coverings) reported by 119 AL administrators across a range of community types. All AL community types experienced infection control challenges, with dementia‐specific communities and their residents being generally the most challenged. Results indicate a need to bolster infection prevention capacity in AL when caring for this especially vulnerable population. In addition, the results have implications for nursing homes. Almost half of nursing home residents have dementia (48%), and although fewer than 1% of nursing homes are dementia‐specific, 15% have dementia care units, 16 pointing out the need for similar study.
AUTHOR CONTRIBUTIONS
Sheryl Zimmerman oversaw study concept and design and supervised all work, and along with Kali S. Thomas obtained funding for the study; Johanna Silbersack Hickey coordinated data collection; and Selen P. Gizlice, John S. Preisser, and Christopher J. Wretman conducted data analyses. All authors contributed to and participated in preparation of the manuscript.
CONFLICT OF INTEREST
The authors report no conflicts of interest.
SPONSOR'S ROLE
The sponsor of this research, the National Institute on Aging, had no role in the design, recruitment, data collection, data analysis, preparation, or any other component of this manuscript. The views expressed here are those of the authors alone.
FINANCIAL DISCLOSURE
This research was supported by National Institute on Aging awards R01AG050602 and R01AG057746.
ACKNOWLEDGMENTS
The authors thank the staff who participate in the Collaborative Studies of Long‐Term Care for their dedication to the well‐being of people who reside in assisted living communities and nursing homes; their efforts during COVID are especially recognized and appreciated.
Zimmerman S, Sloane PD, Hickey JS, et al. Dementia and COVID‐19 infection control in assisted living in seven states. J Am Geriatr Soc. 2022;1‐6. doi: 10.1111/jgs.17923
“We certify that this work is novel or confirmatory of recent novel clinical research.”
Funding information National Institute on Aging, Grant/Award Numbers: R01AG050602, R01AG057746
REFERENCES
- 1. Zimmerman S, Carder P, Schwartz L, et al. The imperative to reimagine assisted living. J Am Med Dir Assoc. 2022;23(2):225‐234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zimmerman S, Sloane PD, Williams CS, et al. Residential care/assisted living staff may detect undiagnosed dementia using the minimum data set cognition scale. J Am Geriatr Soc. 2007;55(9):1349‐1355. doi: 10.1111/j.1532-5415.2007.01289.x [DOI] [PubMed] [Google Scholar]
- 3. Thomas KS, Zhang W, Dosa DM, Carder P, Sloane P, Zimmerman S. Estimation of excess mortality rates among us assisted living residents during the COVID‐19 pandemic. JAMA Netw Open. 2021;4(6):e2113411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vipperman A, Zimmerman S, Sloane PD. COVID‐19 recommendations for assisted living: implications for the future. J Am Med Dir Assoc. 2021;22(5):933‐938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zimmerman S, Sloane PD, Katz PR, Kunze M, O'Neil K, Resnick B. The need to include assisted living in responding to the covid‐19 pandemic. J Am Med Dir Assoc. 2020;21(5):572‐575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harris‐Kojetin L, Sengupta M, Park‐Lee E, et al. Long‐term care providers and services users in the United States: data from the National Study of Long‐Term Care Providers, 2013–2014. National Center for Health Statistics. Vital Health Stat. 2016;3(38). [PubMed] [Google Scholar]
- 7. Zimmerman S, Sloane PD, Reed D. Dementia prevalence and care in assisted living. Health Aff (Millwood). 2014;33(4):658‐666. [DOI] [PubMed] [Google Scholar]
- 8. Dobbs D, Zimmerman S, Carder P, Beeber AS, Palmertree SJ. Staff reports of behavioral expressions of persons with dementia in 250 assisted living communities. Gerontologist. 2021;62(2):169‐180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Peketi P, Zimmerman S, Miller S, Wretman C, Preisser J, Sloane P. Melatonin prescribing in assisted living. J Am Med Dir Assoc. 2022;23:1031‐1037. doi: 10.1016/j.jamda.2021.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thomas KS, Wretman CJ, Sloane PD, et al. To what extent do local nursing home prescribing patterns relate to psychotropic prescribing in assisted living? J Am Med Dir Assoc. 2021;22(9):1813‐1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zimmerman S, Sloane PD, Eckert JK, et al. How good is assisted living? Findings and implications from an outcomes study. J Gerontol B Psychol Sci Soc Sci. 2005;60(4):S195‐S204. [DOI] [PubMed] [Google Scholar]
- 12. Zhu X, Lee H, Sang H, et al. Nursing home design and COVID‐19: implications for guidelines and regulation. J Am Med Dir Assoc. 2022;23(2):272‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zimmerman S, Dumond‐Stryker C, Tandan M, et al. Nontraditional small house nursing homes have fewer COVID‐19 cases and deaths. J Am Med Dir Assoc. 2021;22(3):489‐493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bucy T, Smith L, Carder P, Winfree J, Thomas K. Variability in state regulations pertaining to infection control and pandemic response in us assisted living communities. J Am Med Dir Assoc. 2020;21(5):701‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang Q, Davis PB, Gurney ME, Xu R. COVID‐19 and dementia: analyses of risk, disparity, and outcomes from electronic health records in the US. Alzheimers Dement. 2021;17(8):1297‐1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris‐Kojetin L, Sengupta M, Lendon JP, et al. Long‐term care providers and services users in the United States, 2015–2016. National Center for Health Statistics. Vital Health Stat. 2019;3(43). [PubMed] [Google Scholar]


