ABSTRACT
Aims/Introduction
The purpose of this retrospective observational cohort study was to compare outpatient diabetes care and glycated hemoglobin (HbA1c) level during the coronavirus disease 2019 pandemic in 2020 with 2019, and to compare the glucose‐lowering effect of telemedicine and clinic visits during the state of emergency in Japan declared from 7 April to 25 May (inter‐period) 2020.
Materials and Methods
A total of 13 weeks before and after the inter‐period were designated as the pre‐period and post‐period, respectively. The number of study participants who had clinic visits during the pre‐period and the post‐period were 3,333 in 2020 and 3,608 in 2019. Propensity score matching was carried out to compare the effect of telemedicine and clinic visits on diabetes control in 2020 among diabetes patients with insufficient glucose control (HbA1c ≥7%). The primary outcome was post‐period HbA1c.
Results
The major difference between 2020 and 2019 was the use of telemedicine in 2020. After adjustment for age, sex, diabetes type, pre‐period HbA1c and pre‐period body mass index, glycemic control evaluated by HbA1c was significantly worse in the post‐period of 2020 than 2019. In the propensity score‐matched 618 pairs, the clinic visit group had significantly better post‐period HbA1c than the telemedicine group (7.5% vs 7.4%, P = 0.023).
Conclusions
Glycemic control was slightly, but significantly, worse in 2020 than 2019. Although telemedicine significantly improved glycemic control during the coronavirus disease 2019 pandemic in 2020, clinic visits improved HbA1c significantly more. The substitution of telemedicine for clinic visits appears to be a viable option under emergency conditions, but clinic visits might be a better option when possible.
Keywords: COVID‐19 pandemic, Diabetes, Telemedicine
Glycemic control was slightly worse in 2020 than 2019. Although telemedicine significantly improved glycemic control during the COVID‐19 pandemic in 2020, clinic visit improved HbA1c significantly more. Whether this difference is clinically significant is uncertain and although clinic visit may be a better option when possible, substitution of telemedicine for clinic visit appears to be a viable option.

INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic changed diabetes outpatient care, especially during lockdowns. A state of emergency was declared in Tokyo by the Japanese government on 7 April to 25 May 2020. During this emergency period, lifestyles changed and affected glucose control among diabetes patients 1 , 2 , 3 , 4 , 5 , 6 . Clinic visits decreased during the state of emergency, especially in prefectures affected more by the pandemic 7 , but telemedicine was utilized to substitute for clinic visits 8 , 9 , 10 , 11 .
We have previously reported that both clinic visits and telemedicine during the first state of emergency of the COVID‐19 pandemic were independently effective in improving glycemic control 10 . As we had no guideline for outpatient diabetes care during a pandemic, we quickly analyzed and reported our findings to be prepared for the next state of emergency. However, we did not evaluate whether our outpatient care in 2020 was able to control diabetes similar to a year without a pandemic, nor did we directly compare the effect of telemedicine versus clinic visits.
There are reports comparing diabetes care during the COVID‐19 pandemic in 2020 with 2019 from other countries 12 , 13 , 14 , 15 , 16 , 17 and from Japan 1 , 6 , 18 . Some report that diabetes control was unchanged 13 , 15 , 16 , 18 , whereas others report diabetes control deteriorated 1 , 6 , 12 , 14 or improved 17 . However, the effect of the COVID‐19 pandemic on diabetes control might be different depending on the local pandemic state and medical systems of each country. There were no reports about diabetes care before and after the first wave of the pandemic in Tokyo, which had the most COVID‐19 patients at that time in Japan, compared with 2019. Furthermore, none of the reports compared the effect of telemedicine with that of clinic visits. Accordingly, we did not know whether choosing telemedicine was inferior or superior to clinic visit for controlling diabetes in emergency conditions.
The purpose of the present study was to compare outpatient diabetes care and glycated heoglobin (HbA1c) levels during the COVID‐19 pandemic in 2020 with 2019, and to compare the effect of telemedicine with clinic visits at our clinic, The Institute of Medical Science, Asahi Life Foundation, in Tokyo, Japan.
MATERIALS AND METHODS
Study design
This was a retrospective observational cohort study at the Institute of Medical Science, Asahi Life Foundation.
Observation periods
The emergency period (7 April to 25 May 2020) encompasses the dates of the first declaration of a state of emergency by the Japanese government, and we designated this as the ‘inter‐period’. The 13 weeks before the inter‐period (7 January to 6 April 2020) were designated as the ‘pre‐period’, and the 13 weeks after the inter‐period (26 May to 24 August 2020) were designated the ‘post‐period’. In our previous report, we defined the pre‐ and post‐emergency period as 8 weeks in duration before and after the emergency period to facilitate a quicker analysis of the data after the lifting of the state of emergency 10 . In the current analysis, we defined the pre‐period and post‐period as 13 weeks long to accommodate the longest duration (90 days) for which drugs can be prescribed in Japan, which means that those who have been prescribed medication will need a prescription refill no longer than every 13 weeks. We chose 13 weeks (91 days) instead of 90 days to eliminate the effect of day of the week. The last visit during the pre‐period and the first visit during the post‐period were designated as pre‐visit and post‐visit, respectively. For the analysis of 2019, the pre‐period was designated from 6 January to 6 April 2019. As 2020 was a leap year, the date of the start of the pre‐period is different between 2019 and 2020. The inter‐period and post‐period for 2019 were designated as 7 April to 25 May and 26 May to 24 August, respectively.
Clinic settings
Our clinic is located in central Tokyo. Approximately half of our outpatients live in the central 23 wards of Tokyo, and the other half come from outside of central Tokyo. Those who live in the central 23 wards of Tokyo can come to the hospital within approximately 40–50 min by public transportation. For those who live outside of the 23 wards of Tokyo, travel to the clinic takes >1 h. Most patients come by public transportation.
There are nine full‐time and 11 part‐time doctors working in our diabetes clinic. Before the COVID‐19 pandemic, most of the patients visited our clinic every 1–2 months according to their health status and the doctor's decision. When the diabetes patients visited our clinic, HbA1c, blood glucose and bodyweight were measured as the standard procedure. HbA1c was not checked more than once a month because of health insurance coverage limitation. Self‐monitoring blood glucose was covered by health insurance for those who were on injection therapy, such as insulin and glucagon‐like pepetide‐1 receptor agonist, but not for those who were taking oral medications only. At our clinic, approximately 30% of the diabetes patients were self‐monitoring their glucose, and most of them were receiving insulin therapy. Therefore, when patients were not receiving insulin treatment, they had to visit the clinic to have HbA1c and/or glucose checked. At their clinic visit, patients consult their attending doctors, and prescriptions were renewed or changed depending on their blood tests and health status. Patients returned to the same doctor unless there were exceptional reasons, such as unscheduled visits. The period between clinic visits depended on each doctor.
When the pandemic started in Japan, most COVID‐19 cases were reported from central Tokyo. Many of our outpatients feared becoming infected during travel to the clinic, so they canceled or postponed their clinic appointments. Before the declaration of the state of emergency, however, on 1 March the government approved sending prescriptions to patients by fax or postage mail, thereby making a clinic visit unnecessary for obtaining a prescription renewal.
Our clinic procedures changed with the spread of the COVID‐19 pandemic. Doctors were encouraged to substitute telemedicine for clinic visit, but because there were no standard guidelines as to which patient should visit the clinic, the decision to substitute telemedicine depended on each attending doctor. The doctors tended to substitute telemedicine for clinic visits more often when pre‐HbA1c was lower. Doctors called the patients several days before their clinic visit appointment to inform them that telemedicine was an option available during the pandemic. Depending on the patients' health status, where they lived and the doctors' decision, clinic visit appointments were substituted by telemedicine appointments by telephone. Doctors advised patients to check their bodyweight at home, not to overeat, to exercise and not gain weight while they stayed home. They were also given advice about preventing COVID‐19 infection. When patients were receiving insulin treatment, the self‐monitored glucose level was reported and insulin dosages were changed according to the attending doctor's decision. After such telemedicine consultations, prescriptions were mailed to the patients who went to their neighborhood pharmacies to get the prescribed drugs.
When patients could not be contacted before their scheduled clinic visit, they came to the clinic as usual. There were some patients who requested a medical certificate to be referred to a clinic in their neighborhood. In such cases, the attending doctor sent the certificate with the patient's medical information, after which the patient did not visit our clinic. Some had neither clinic visits nor telemedicine consultation during the emergency period.
Telemedicine was continued until the state of emergency was lifted on 25 May, following which we encouraged patients to visit the clinic to have their HbA1c and status checked. However, some patients, fearing COVID‐19, especially those who lived far from our clinic, did not visit the clinic, even after the lifting of the emergency period.
Study population
Those who visited our diabetes clinic, and had both HbA1c and body mass index (BMI) checked during both the pre‐period and the post‐period in 2019 and/or 2020 were selected. There were 3,713 patients who visited our clinic during the pre‐period of 2020. Among them, 195 were not followed thereafter, and 185 were seen during the inter‐period, but not during the post‐period. The remaining 3,333 patients comprised the analytic cohort of the year 2020 (Figure 1a). In 2019, 3,943 patients visited during the pre‐period. Among them, 227 were not followed thereafter, and 108 were seen during the inter‐period, but not during the post‐period. The remaining 3,608 patients comprised the analytic cohort of the year 2019 (Figure 1b).
Figure 1.
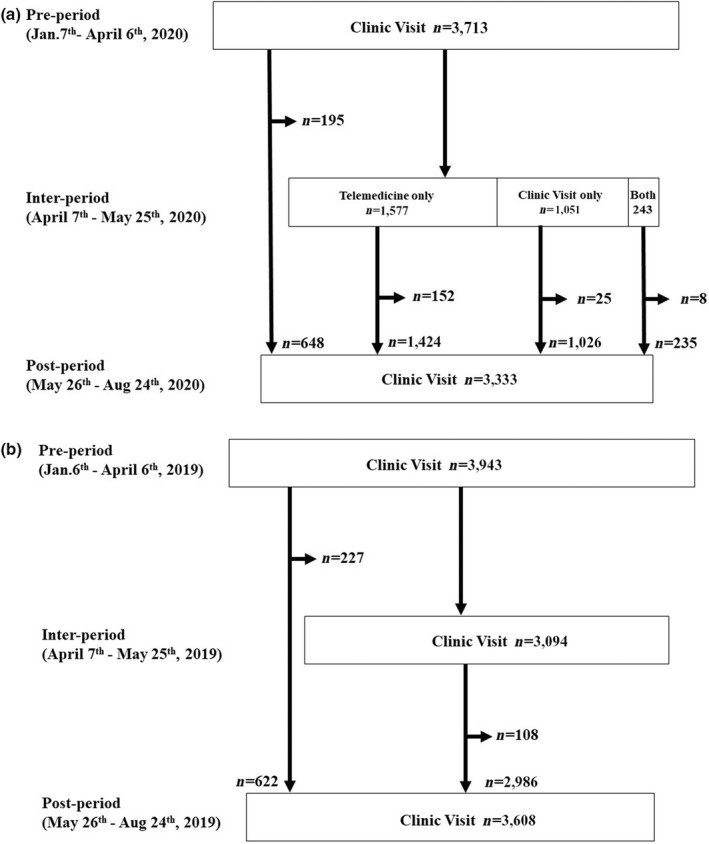
(a) Clinic follow‐up status of diabetes patients 13 weeks before the coronavirus disease 2019 pandemic state of emergency (pre‐period; 7 January to 6 April 2020), during the state of emergency period (inter‐period; 7 April to 25 May 2020) and 13 weeks after the state of emergency period (post‐period; 26 May to 24August 2020). There were 3,713 patients who visited our clinic during the pre‐period. Among them, 843 did not visit during the inter‐period, but 648 visited during the post‐period, whereas 195 did not. Among the initial 3,713 patients, 1,577 utilized only telemedicine after their pre‐visit, and 1,424 visited during the post‐period, whereas 152 did not. Among the initial 3,713 patients, 1,051 had only clinic visits during the inter‐period, and 1,026 visited during the post‐period, whereas 25 did not. Finally, among the initial 3,713 patients, 243 had both clinic visits and telemedicine, and 235 visited during the post‐period, whereas eight did not. Those 3,333 patients who visited both during the pre‐ and post‐periods comprised the analytic cohort of the year 2020. (b) Clinic follow‐up status of diabetes patients during the pre‐period of 2019 (6 January to 6 April 2019), inter‐period (7 April to 25 May 2019) and post‐period (26 May to 24 August 2019). There were 3,943 patients who visited our clinic during the pre‐period. Among them, 849 did not visit during the inter‐period, but 622 visited during the post‐period, whereas 227 did not. Of the initial 3,943 patients, 3094 visited the clinic during the inter‐period, and 2,986 visited during the post‐period, whereas 108 did not. Those 3,608 patients who visited both during the pre and post‐periods comprised the analytic cohort of year 2019.
This research was approved by the Human Subjects Review Committee at the Institute for Medical Science (approval number12205). Informed consent was obtained by opt out online.
Measurements
We defined HbA1c and BMI at the pre‐/post‐visit as the pre‐/post‐HbA1c and pre‐/post‐BMI, respectively, and the change of HbA1c and BMI from pre‐visit to post‐visit as ΔHbA1c and ΔBMI. A phone consultation between the pre‐visit and the post‐visit was considered a telemedicine event.
Statistical analysis
Characteristics of the population are presented as the mean (standard deviation) for continuous variables with normal distribution, and the median (interquartile range) for continuous variables that did not have normal distribution or the number (proportion) for categorical data. The significance of the difference of variables was tested by t‐test for continuous variables with normal distribution, by the Mann–Whitney U‐test or the Kruskal–Wallis test and Dunn's test with Bonferroni adjustment for continuous variables that did not have normal distribution, and χ2‐tests for the proportions of categorical variables. Multiple linear regression analysis was used to evaluate the factors associated with post‐HbA1c value, adjusted for age, sex, pre‐HbA1c, pre‐BMI and diabetes type.
To account for differences in baseline characteristics between those who had telemedicine and clinic visits in 2020, we carried out a one‐to‐one propensity score matching analysis. Logistic regression analysis was used to calculate propensity scores for patients who had clinic visits or telemedicine, using age, sex, pre‐HbA1c, pre‐BMI and diabetes type. Each patient who had clinic visits in 2020 was matched with a patient who had telemedicine in 2020, with the closest estimated propensity score on the logit scale with no‐replacement. The width of the caliper was set at 20% of the standard deviation of the propensity scores on the logit scale. Balances in baseline variables using standardized differences were estimated. Absolute values <10% were considered balanced 19 .
After the propensity score matching, we compared post‐HbA1c and ΔHbA1c by t‐test or Wilcoxon rank‐sum test. The threshold of statistical significance was P (two‐tailed) <0.05. Statistical analyses were carried out using Stata MP, version 16.0 (StataCorp, College Station, TX, USA).
RESULTS
Follow‐up status
Among the 3,333 patients in the year 2020 study cohort, 648 did not have a clinic visit or receive telemedicine consultation during the inter‐period, whereas 1,424 had only telemedicine, 1,026 had only a clinic visit, and 235 had both clinic visit and telemedicine during the inter‐period (Figure 1a). In 2019, the study population was 3,608, and 622 did not have a clinic visit, whereas 2,986 had clinic visits during the inter‐period (Figure 1b).
Characteristics of the study participants of 2020 and 2019
The characteristics of the 3,333 study participants of the year 2020 and 3,608 of the year 2019 are shown in Table 1. The major difference between 2020 and 2019 was that many clinic visits were substituted by telemedicine in 2020 during the inter‐period. The average number of days between clinic visits during the inter‐period was significantly longer in 2020 compared with 2019 (84 vs 45.5 days). The average number of days between clinic visits and/or telemedicine during the inter‐period in 2020 was also significantly greater than the average number of days between clinic visits during the inter‐period in 2019 (56 vs 45.5 days). There were significantly more patients who did not have any contact during the inter‐period by either clinic visit or telemedicine in 2020 compared with 2019 (19.4% vs 17.2%). There were statistically significant differences in pre‐HbA1c, ΔBMI and ΔHbA1c between 2020 and 2019. Although there was no statistically significant difference in crude post‐HbA1c between 2020 and 2019, when we carried out multiple regression analysis to assess the effect of the emergency period in 2020 on post‐HbA1c, the year 2020 was significantly associated with higher post‐HbA1c adjusted for age, sex, type of diabetes, pre‐HbA1c and pre‐BMI (Table 2).
Table 1.
Characteristics of study participants of 2020 and 2019
| Characteristics | 2020 (n = 3,333) | 2019 (n = 3,608) | P‐value |
|---|---|---|---|
| Pre‐period | |||
| Age (years) | 68.7 (59.0, 75.5) | 68.5 (59.0, 75.3) | 0.53 |
| Male sex | 2,609 (78.3) | 2,786 (77.2) | 0.29 |
| Type 2 diabetes | 3,141 (94.2) | 3,393 (94.0) | 0.73 |
| Pre‐BMI (kg/m2) | 24.5 (4.0) | 24.5 (4.0) | 0.94 |
| Pre‐HbA1c | 7.3 (1.0) | 7.4 (1.0) | 0.002 |
| Visiting state during inter‐period | |||
| No visit nor telemedicine | 648 (19.4) | 622 (17.2) | 0.018 |
| Only clinic visit | 1,026 (30.8) | 2,986 (82.8) | <0.001 |
| Only telemedicine | 1,424 (42.7) | NA | |
| Both clinic visit and telemedicine | 235 (7.1) | NA | |
| Average no. days between clinic visits | 84 (58, 112) | 45.5 (32.4, 63) | <0.001 |
| Average no. days between clinic visits and/or telemedicine | 56 (40, 65) | 45.5 (32.4, 63) | <0.001 |
| Post‐period and change from pre‐period | |||
| Post‐BMI | 24.6 (4.0) | 24.5 (4.0) | 0.31 |
| Post‐HbA1c | 7.2 (1.0) | 7.2 (0.9) | 0.43 |
| ΔBMI (kg/m2) | 0.01 (0.6) | −0.08 (0.5) | <0.001 |
| ΔHbA1c | −0.1 (0.6) | −0.2 (0.6) | <0.001 |
Data are median (quartile 1, quartile 3), mean (standard deviation) or number (%).
BMI, body mass index; HbA1c, glycated hemoglobin.
Table 2.
Multiple linear regression analysis of glycated hemoglobin at post‐period in 2020 and 2019
| Independent variables in the model | β | β’ | P | Model R 2 |
|---|---|---|---|---|
| (n = 6,941) | ||||
| Year 2020 | 0.039 | 0.020 | 0.003 | |
| Pre‐HbA1c | 0.776 | 0.808 | <0.001 | 0.667 |
| Pre‐BMI | 0.011 | 0.047 | <0.001 | |
Model adjusted for age, gender, and type of diabetes. β, regression coefficient; β’, standardized regression coefficient. BMI, body mass index; HbA1c, glycated hemoglobin.
Association of telemedicine, clinic visit and HbA1c
To assess the effect of telemedicine and/or clinic visits on post‐HbA1c, we examined pre‐HbA1c, post‐HbA1c and ΔHbA1c stratified by pre‐HbA1c and clinic visit/telemedicine status in 2020 and 2019 (Tables S1 and S2). Among patients with pre‐HbA1c <7%, the median post‐HbA1c were all 6.5% or 6.4%, which means the glucose control remained good. Therefore, we focused on patients with pre‐HbA1c ≥7%.
Among those with pre‐HbA1c ≥7%, we assessed the association between clinic visits and/or telemedicine and post‐HbA1c measured in the post‐period adjusted for age, sex, diabetes type, pre‐HbA1c, and pre‐BMI by multiple regression analysis in both 2020 and 2019 (Table 3). Clinic visits, pre‐HbA1c and pre‐BMI were significantly associated with post‐HbA1c in both years, but age and sex were associated with post‐HbA1c only in 2020. ‘Telemedicine only’ and ‘telemedicine and clinic visit’ in 2020 were also independent significant factors. The coefficient of clinic visit was −0.221, and the lowering effect was greater than that of telemedicine, −0.139. These results were consistent with our previous findings covering a shorter period 10 .
Table 3.
Multiple linear regression analysis of glycated hemoglobin at post period in 2020 and 2019
| Independent variables in the model | β | β’ | P | Model R 2 | β | β’ | P | Model R 2 |
|---|---|---|---|---|---|---|---|---|
| Participants with pre‐HbA1c ≥7.0% | Year 2020 (n = 2,095) | Year 2019 (n = 2,344) | ||||||
| No clinic visit nor telemedicine | ||||||||
| Telemedicine only | −0.136 | −0.074 | 0.001 | N/A | N/A | N/A | ||
| Clinic visit only | −0.221 | −0.115 | <0.001 | −0.129 | −0.050 | 0.001 | ||
| Telemedicine and clinic visit | −0.223 | −0.066 | <0.001 | N/A | N/A | N/A | ||
| Pre‐HbA1c | 0.759 | 0.697 | <0.001 | 0.509 | 0.700 | 0.707 | <0.001 | 0.520 |
| Pre‐BMI | 0.021 | 0.095 | <0.001 | 0.011 | 0.047 | 0.003 | ||
| Age | 0.003 | 0.043 | 0.012 | 0.002 | 0.024 | 0.130 | ||
| Male sex | −0.080 | −0.038 | 0.017 | −0.048 | −0.023 | 0.118 | ||
| Type 2 diabetes | −0.045 | −0.013 | 0.423 | −0.100 | −0.029 | 0.052 | ||
β, regression coefficient; β’, standardized regression coefficient.
BMI, body mass index; HbA1c, glycated hemoglobin; N/A, not available.
Comparison of the effect of telemedicine and clinic visit on post‐HbA1c
To further investigate whether clinic visits lowered post‐HbA1c more than telemedicine, we carried out propensity score matching. Among the analytic cohort patients with preHbA1c ≥7%, there were 876 who had only telemedicine and 697 who had only clinic visit during the emergency period. After one‐to‐one propensity score matching, we selected 618 pairs (Figure 2). The C‐statistic was 0.64. Table 4 shows the baseline characteristics of the unmatched and propensity score‐matched groups. Before propensity score matching, the telemedicine group was older and had more women, fewer type 2 diabetes patients, lower pre‐BMI, and lower pre‐HbA1c compared with the clinic visit group. After propensity score matching, patients' characteristics were well balanced between the two groups (Table 4). Before matching, crude post‐HbA1c and ΔHbA1c were 7.4 and −0.15% for the telemedicine group, and 7.5 and −0.31% for the clinic visit group, respectively (Table 5). In the propensity score‐matched comparison, post‐HbA1c was slightly, but statistically significantly, better in the clinic visit group than the telemedicine group (7.4 vs 7.5%, P = 0.023), and the improvement of HbA1c evaluated by ΔHbA1c was also slightly, but statistically significantly, better in the clinic visit group (−0.23 vs −0.15%, P = 0.019; Table 5).
Figure 2.
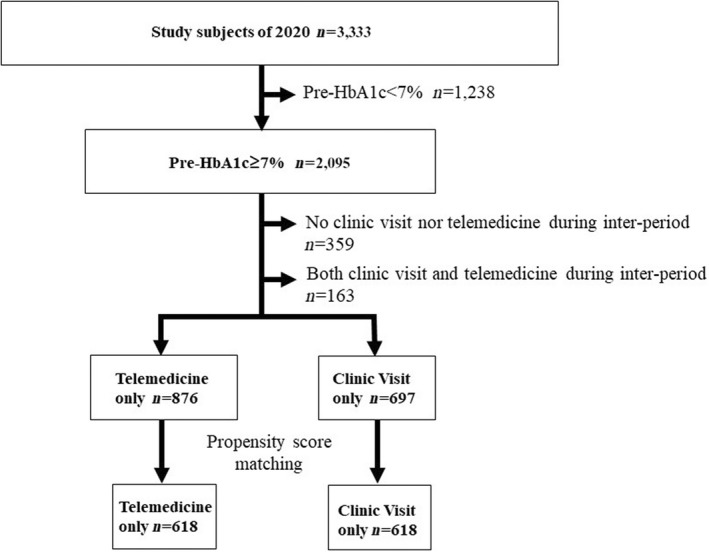
Patient selection flow for propensity score matching.
Table 4.
Baseline patient characteristics before and after propensity score matching (pre‐glycated hemoglobin ≥7.0%)
| Variables | Before matching | After matching | ||||
|---|---|---|---|---|---|---|
| Visit type | Telemedicine (n = 876) | Clinic visit (n = 697) | Standardized difference (%) | Telemedicine (n = 618) | Clinic visit (n = 618) | Standardized difference (%) |
| Age (years) | 70.7 (61.0,76.6) | 66.4 (57.4,73.4) | 28.7 | 68.2 (57.8, 75.3) | 67.9 (59.2,74.0) | 0.2 |
| Sex (female) | 240 (27.4) | 126 (18.1) | 22.4 | 121 (19.6) | 119 (19.3) | 0.8 |
| Type 2 | 804 (91.8) | 646 (92.7) | 32.3 | 573 (92.7) | 572 (92.6) | 7.5 |
| Pre‐BMI | 24.4 (3.8) | 25.0 (4.0) | 14.5 | 24.9 (3.9) | 24.8 (3.8) | 2.6 |
| Pre‐HbA1c | 7.5 (7.2, 7.9) | 7.7 (7.3, 8.2) | 32.3 | 7.6 (7.3, 8.1) | 7.6 (7.3, 8.0) | 7.5 |
Data are median (Q1,Q3), mean (SD), or number (%).
BMI, body mass index; HbA1c, glycated hemoglobin.
Table 5.
Outcomes in the unmatched and propensity score‐matched groups (pre‐glycated hemoglobin ≥7.0%)
| Variables | Before matching | After matching | ||||
|---|---|---|---|---|---|---|
| Visit type | Telemedicine (n = 876) | Clinic visit (n = 697) | P‐value | Telemedicine (n = 618) | Clinic visit (n = 618) | P‐value |
|
Post‐HbA1c |
7.4 (7.0, 7.9) | 7.5 (7.1, 8.0) | 0.008 | 7.5 (7.1, 8.0) | 7.4 (7.1, 7.9) | 0.023 |
| ΔHbA1c | −0.15 (0.59) | −0.31 (0.70) | <0.001 | −0.15 (0.64) | −0.23 (0.56) | 0.019 |
Data are median (Q1, Q3) or mean (SD), HbA1c, glycated hemoglobin.
DISCUSSION
The present retrospective cohort study showed that during the state of emergency due to the COVID‐19 pandemic in 2020, clinic visits were replaced by telemedicine consultation for many diabetes patients. Glucose control measured by adjusted HbA1c in 2020 after the state of emergency was statistically significantly worse compared with the HbA1c measured in a similar timeframe of 2019. Additionally, we were able to show that telemedicine and clinic visits were both effective in terms of improving glucose control, but clinic visits were significantly more effective than telemedicine.
Telemedicine was technically available, but not common, until there was a rapid increase of its use during the COVID‐19 pandemic. There are several international survey results reporting the use of telemedicine for diabetes care at the early stage of the COVID‐19 pandemic 8 , 11 , 15 . However in these studies, HbA1c was not measured 8 , 11 , or the glucose‐lowering effect of telemedicine was not compared with clinic visits 15 . We have previously explored in a short report that telemedicine was effective in improving glucose control during the COVID‐19 pandemic 10 , but did not directly compare it with clinic visits. With a longer follow‐up period and larger study population, the present report shows that clinic visits improved glucose control significantly better than with telemedicine.
There are some retrospective cohort studies that reported glucose control during the COVID‐19 pandemic in 2020, and comparing that with a similar timeframe of 2019, but their results were inconclusive 1 , 6 , 12 , 13 , 14 , 15 , 17 , 18 . Some studies reported that glucose control was better during the pandemic in 2020 17 , whereas other studies reported that it deteriorated 1 , 6 , 12 , 14 or did not change 13 , 15 , 16 , 18 compared with 2019. Most of these did not adjust for essential confounding factors 1 , 12 , 13 , 15 , 17 , 18 or lacked adjustment for BMI 6 , 14 . Some explored only type 1 1 or type 2 diabetes 6 , 12 , 13 , 14 , 15 , 18 , or did not specify the diabetes type 16 . Furthermore, most of the study populations were relatively small compared with the present study population 1 , 6 , 13 , 16 , 17 , 18 . A large retrospective study with a cohort exceeding 6,000 type 2 diabetes patients from Korea reported that social distancing associated with COVID‐19 deteriorated glucose control levels, evaluated by adjusted change of HbA1c before and after the pandemic, compared with 2019. However, there was no evaluation of telemedicine in that study 14 . From Japan, there were three reports among hospitalized type 11, or hospitalized 18 or outpatient 6 type 2 diabetes patients, comparing glucose control levels in 2020 and 2019. A study of type 2 diabetes patients in the Tohoku area of Japan reported that glycemic control deteriorated in 2020 after the state of emergency by mixed linear model 6 . In their study, however, only 1.7% utilized telemedicine, whereas 49.8% of the present study participants did, showing the difference in the use of telemedicine among areas within Japan. As clinic style differed depending on the local pandemic status, even within the same country, diabetes care and glucose control status during the state of emergency, and its difference from 2019, might also have varied depending on location. In the present study, because of the relatively large study population with both type 1 and type 2 diabetes patients, we were able to compare by multivariate analysis glucose control status in 2020 during the COVID‐19 pandemic with that in 2019. Glucose control was slightly, but significantly, worse in 2020, and this was consistent with the finding that telemedicine was also slightly, but significantly, worse than clinic visits.
Telemedicine was effective in lowering post‐HbA1c during the pandemic when pre‐HbA1c was ≥7.0%. As telemedicine was carried out by attending physicians who already knew the patients' lifestyle, it was possible to give the patients appropriate advice depending on their situations by phone. There are several cross‐sectional studies reporting that lifestyle changes were associated with glucose control during the pandemic 1 , 2 , 3 , 4 , 5 , which suggest that asking about each patient's lifestyle during the state of emergency and giving lifestyle improvement advice by telemedicine would be likely to improve HbA1c. There are some reports showing that lifestyle counseling and a higher frequency of clinic visits are effective in achieving HbA1c goals 20 , 21 . Although these reports were about clinic visit counseling when there was no pandemic, they are probably applicable to telephone lifestyle counseling during the pandemic.
A clinical implication of the present study is that clinic visits improved HbA1c statistically significantly more than telemedicine during the state of emergency, but from a clinical perspective, this difference might be considered small. We should be cautious with interpreting the present findings, however, because the first announcement of a state of emergency was for just 7 weeks, so we do not know how long we can substitute telemedicine for clinic visits. We also do not know whether a clinic visit might be necessary even for those with fairly good glucose control if the state of emergency lasted longer than 7 weeks.
There were several limitations to the present study. First, this was a single‐site study, which means that the result of this study might not be applicable to other locations in Japan and/or worldwide. Second, this was a retrospective observational study, where the type of contact during the emergency period was decided by patients and/or doctors. Thus, there might be confounders, such as comorbidities, distance between patient's home and our clinic, and other unknown confounders behind the decision. However, the ethics of carrying out a prospective randomized trial balancing confounders by assigning some patients to telemedicine or a clinic visit despite the risk of possible COVID‐19 infection is problematic. Third, we could not evaluate the risk of COVID‐19 infection associated with clinic visits during the emergency period. However, we were unable to find any patient who was infected because of visiting the clinic. Fourth, we do not have any information about the duration of diabetes, comorbidities, distance between our clinic and the patients' home, the medication and its prescription changes that might have been made by the attending doctors. Finally, the COVID‐19 state of emergency in Tokyo that we focused on in the present study lasted for 7 weeks. We do not know the effect on diabetes control of a longer duration of telemedicine. Future study is required to evaluate these limitations.
In conclusion, the present retrospective longitudinal study of the substitution of telemedicine for clinic visits during the COVID‐19 pandemic in 2020 showed that diabetes control during the COVID‐19 pandemic in 2020 was slightly, but statistically significantly, worse than in 2019. Additionally, the present study showed that telemedicine significantly improved glycemic control during the COVID‐19 pandemic in 2020, but clinic visits improved HbA1c significantly more. The results should be interpreted with caution, but this suggests that under emergency conditions, telemedicine might be a reasonable substitution for clinic visits, but clinic visits might result in slightly better glycemic control.
DISCLOSURE
The authors declare no conflict of interest.
Approval of research protocol: This research was approved by the Human Subjects Review Committee at the Institute for Medical Science (approval number12205).
Informed consent: Informed consent was obtained by opt out online.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Supporting information
Table S1 | Comparison patients having clinic visits and/or telemedicine in 2020 according to pre‐glycated hemoglobin.
Table S2 | Comparison patients having clinic visits in 2019 according to pre‐glycated hemoglobin.
ACKNOWLEDGMENTS
We greatly appreciate the contribution of Wilfred Y Fujimoto for reviewing our study as a scientific advisor, Nobuhiro Tachibana for data management and staff members for their skilled assistance in collecting clinical data.
REFERENCES
- 1. Hosomi Y, Munekawa C, Hashimoto Y, et al. The effect of COVID‐19 pandemic on the lifestyle and glycemic control in patients with type 1 diabetes: a retrospective cohort study. Diabetol Int 2021; 13: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kishimoto M, Ishikawa T, Odawara M. Behavioral changes in patients with diabetes during the COVID‐19 pandemic. Diabetol Int 2020; 12: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Munekawa C, Hosomi Y, Hashimoto Y, et al. Effect of coronavirus disease 2019 pandemic on the lifestyle and glycemic control in patients with type 2 diabetes: a cross‐section and retrospective cohort study. Endocr J 2020; 68: 201–210. [DOI] [PubMed] [Google Scholar]
- 4. Takahara M, Watanabe H, Shiraiwa T, et al. Lifestyle changes and their impact on glycemic control and weight control in patients with diabetes during the coronavirus disease 2019 pandemic in Japan. J Diabetes Investig 2021; 13: 375–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tanaka N, Hamamoto Y, Kurotobi Y, et al. Lifestyle changes as a result of COVID‐19 containment measures: bodyweight and glycemic control in patients with diabetes in the Japanese declaration of a state of emergency. J Diabetes Investig 2021; 12: 1718–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tanji Y, Sawada S, Watanabe T, et al. Impact of COVID‐19 pandemic on glycemic control among outpatients with type 2 diabetes in Japan: a hospital‐based survey from a country without lockdown. Diabetes Res Clin Pract 2021; 176: 108840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Osawa I, Goto T, Asami Y, et al. Physician visits and medication prescriptions for major chronic diseases during the COVID‐19 pandemic in Japan: retrospective cohort study. BMJ Open 2021; 11: e050938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fisher L, Polonsky W, Asuni A, et al. The early impact of the COVID‐19 pandemic on adults with type 1 or type 2 diabetes: a national cohort study. J Diabetes Complications 2020; 34: 107748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Luzi L, Carruba M, Crialesi R, et al. Telemedicine and urban diabetes during COVID‐19 pandemic in Milano, Italy during lock‐down: epidemiological and sociodemographic picture. Acta Diabetol 2021; 58: 919–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Onishi Y, Yoshida Y, Takao T, et al. Diabetes management by either telemedicine or clinic visit improved glycemic control during the coronavirus disease 2019 pandemic state of emergency in Japan. J Diabetes Investig 2021; 13: 386–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scott SN, Fontana FY, Zuger T, et al. Use and perception of telemedicine in people with type 1 diabetes during the COVID‐19 pandemic‐results of a global survey. Endocrinol Diabetes Metab 2021; 4: e00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Coma E, Miro Q, Medina M, et al. Association between the reduction of face‐to‐face appointments and the control of patients with type 2 diabetes mellitus during the Covid‐19 pandemic in Catalonia. Diabetes Res Clin Pract 2021; 182: 109127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. D'Onofrio L, Pieralice S, Maddaloni E, et al. Effects of the COVID‐19 lockdown on glycaemic control in subjects with type 2 diabetes: the glycalock study. Diabetes Obes Metab 2021; 23: 1624–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park SD, Kim SW, Moon JS, et al. Impact of social distancing due to coronavirus disease 2019 on the changes in glycosylated hemoglobin level in people with type 2 diabetes mellitus. Diabetes Metab J 2021; 45: 109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Patel SY, McCoy RG, Barnett ML, et al. Diabetes care and glycemic control during the COVID‐19 pandemic in the United States. JAMA Intern Med 2021; 181: 1412–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thomas AM, Baker JW, Hoffmann TJ, et al. Clinical pharmacy specialists providing consistent comprehensive medication management with increased efficiency through telemedicine during the COVID19 pandemic. J Am Coll Clin Pharm 2021; 4: 934–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wong VW, Wang A, Manoharan M. Utilization of telehealth for outpatient diabetes management during COVID‐19 pandemic: how did the patients fare? Intern Med J 2021; 51: 2021–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Watanabe T, Temma Y, Okada J, et al. Influence of the stage of emergency declaration due to the coronavirus disease 2019 outbreak on plasma glucose control of patients with diabetes mellitus in the Saku region of Japan. J Rural Med 2021; 16: 98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity‐score matched samples. Stat Med 2009; 28: 3083–3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morrison F, Shubina M, Turchin A. Encounter frequency and serum glucose level, blood pressure, and cholesterol level control in patients with diabetes mellitus. Arch Intern Med 2011; 171: 1542–1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Morrison F, Shubina M, Turchin A. Lifestyle counseling in routine care and long‐term glucose, blood pressure, and cholesterol control in patients with diabetes. Diabetes Care 2012; 35: 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 | Comparison patients having clinic visits and/or telemedicine in 2020 according to pre‐glycated hemoglobin.
Table S2 | Comparison patients having clinic visits in 2019 according to pre‐glycated hemoglobin.


