Abstract
Understanding the pattern and severity of myocarditis caused by the coronavirus disease 2019 (COVID‐19) vaccine is imperative for improving the care of the patients, and cardiac evaluation by MRI plays a key role in this regard. Our systematic review and meta‐analysis aimed to summarize cardiac MRI findings in COVID‐19 vaccine‐related myocarditis. We performed a comprehensive systematic review of literature in PubMed, Scopus, and Google Scholar databases using key terms covering COVID‐19 vaccine, myocarditis, and cardiac MRI. Individual‐level patient data (IPD) and aggregated‐level data (AD) studies were pooled through a two‐stage analysis method. For this purpose, all IPD were first gathered into a single data set and reduced to AD, and then this AD (from IPD studies) was pooled with existing AD (from the AD studies) using fixed/random effect models. I 2 was used to assess the degree of heterogeneity, and the prespecified level of statistical significance (P value for heterogeneity) was <0.1. Based on meta‐analysis of 102 studies (n = 468 patients), 79% (95% confidence interval [CI]: 54%–97%) of patients fulfilled Lake Louise criteria (LLC) for diagnosis of myocarditis. Cardiac MRI abnormalities included elevated T2 in 72% (95% CI: 50%–90%), myocardial late gadolinium enhancement (LGE) in 93% (95% CI: 83%–99%; nearly all with a subepicardial and/or midwall pattern), impaired left ventricular ejection fraction (LVEF) (<50%) in 4% (95% CI: 1.0%–9.0%). Moreover, elevated T1 and extracellular volume fraction (ECV) (>30), reported only by some IPD studies, were detected in 74.5% (76/102) and 32% (16/50) of patients, respectively. In conclusion, our findings may suggest that over two‐thirds of patients with clinically suspected myocarditis following COVID‐19 vaccination meet the LLC. COVID‐19 vaccine‐associated myocarditis may show a similar pattern compared to other acute myocarditis entities. Notably, preserved LVEF is probably a common finding in these patients.
Evidence Level
4
Technical Efficacy
Stage 3
Keywords: COVID‐19 vaccine, cardiac MRI, myocarditis
The coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) continues to be a global health challenge. 1 To end the ongoing pandemic, a growing number of countries adopted the mass vaccination program using newly approved vaccines against the virus; as of February 7, 2022, about half of the population around the world has been fully vaccinated. 2 Despite the undeniable efficacy of vaccines for decreasing the burden of disease in areas with high vaccination rates, some side effects, mainly related to the activation of local and/or systemic inflammation, have been identified for them. 3
Several cases of clinically suspected myocarditis have been reported worldwide shortly after COVID‐19 vaccination, mainly for messenger ribonucleic acid (mRNA)‐based vaccines. 4 Timely diagnosis and management are crucial for improving the prognosis of this complication. 5 An increasing number of studies have utilized cardiac MRI, as the most important noninvasive diagnostic tool, to assess suspected myocarditis associated with COVID‐19 vaccination. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 One narrative review article attempted to address the pattern of myocardial injury following COVID‐19 vaccination based on cardiac MRI findings from 11 case series. 4 Since the last review, a large number of case reports/series have been published. Hence, we conducted the present comprehensive systematic review and meta‐analysis study to include all available case reports and case series evaluating cardiac MRI findings in patients with clinically suspected myocarditis following COVID‐19 vaccination.
Materials and Methods
Our study was undertaken according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines. As a systematic review and meta‐analysis of published studies, it required no ethical approval. We included all eligible studies that reported cardiac MRI findings in patients with COVID‐19 vaccine‐associated myocarditis.
Search
A comprehensive search was performed on three databases, including PubMed, Scopus, and Google Scholar, on January 21, 2022 and updated on April 27, 2022, using a combination of the key terms in three domains: 1) COVID‐19 vaccine, 2) myocarditis, and 3) cardiac MRI. Detailed search strings for each database are presented in the Supplementary Table S1.
In addition, reference lists of the included articles and systematic reviews on similar topics were manually checked to identify any additional eligible studies. Citations from all retrieved articles were imported into EndNote X9 software (version EndNote X9.3.2, Captivate Analytics, California USA), and the duplicates were removed.
Study Inclusion
Two researchers (P.S. and E.J.A.), both with 2 years of experience in medicine independently screened the titles, abstracts, and full texts of retrieved studies to identify the eligible items. Any disagreement resolved by a third researcher (N.S.H., 13 years of experience in medicine or H.R., 11 years of experience in research) based on the topic.
Eligibility Criteria
We included all studies that met all our inclusion criteria as follows:
Inclusion of patients with clinically suspected myocarditis following COVID‐19 vaccination.
Cardiac evaluation by MRI.
Observational study design: cohort studies, case series, and case reports.
Written in English.
Data Extraction
Three out of four mentioned researchers (H.R., P.S., and E.J.A.) extracted the data from the full texts of the included studies into the “Data Extraction Form” produced using Microsoft Excel (version 2016, Microsoft Corp., Redmond, WA, USA). Extracted data were: first author's name, country, study design, sample size, age, sex, study population, time from vaccine to symptoms, time from symptoms to MRI, symptoms type, elevated troponin, electrocardiogram (ECG) changes, echocardiography findings, and main cardiac MRI findings including myocardial and pericardial late gadolinium enhancement (LGE), T1, T2, extracellular volume (ECV), left ventricle (LV) ejection fraction (EF), pericardial effusion (PE), and wall motion abnormality (WMA).
Quality Assessment
Two trained researchers mentioned above (P.S. and E.J.A.) independently assessed the quality of the articles by the Joanna Briggs Institute (JBI) appraisal tool adapted for use in case series. 20 Furthermore, any disagreement was resolved through discussion with a third researcher (H.R. or N.S.H.). JBI's critical appraisal tool contained 10 items, and its total score ranged from 0 to 10. 20
Statistical Analyses
Data sets were classified as individual‐level patient data (IPD) and aggregate‐level data (AD). We collected available IPD from each case report/series of patients with clinically suspected myocarditis following the COVID‐19 vaccine who underwent cardiac MRI. Characteristics of these patients were reported in terms of demographic/clinical data, laboratory results including serum troponin, ECG findings, and imaging findings from echocardiography and cardiac MRI. We calculated percentages for categorical variables based on valid denominators (i.e. the number of patients with data for the characteristic of interest). Continuous data were summarized using median (interquartile range [IQR]) or mean and standard deviation (SD).
Then, summarized cardiac MRI findings from IPD were combined with findings from AD studies using both fixed and random‐effect models, which are standard AD meta‐analysis methods. Based on the size of the observed heterogeneity, the values were derived either from the random or fixed‐effect model. The chi‐square test and I 2 statistic were used to measure the heterogeneity among the studies; if I 2 > 75% and the P value for heterogeneity < 0.1, it was considered that there was significant heterogeneity. Data were processed in SPSS (version 20; IBM Corp., Armonk, NY, USA) and analyzed using RStudio (version 1.4.1103, PBC, Boston, MA, USA).
Results
Our systematic literature search revealed 2543 citations through the initial search databases. After excluding duplications, 1997 publications remained for the title and abstract screening. Overall, 266 publications were retrieved for review of full‐text articles. Finally, 102 publications, including 56 case reports 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 92 , 93 , 94 , 97 , 98 , 101 , 102 , 105 , 106 and 46 case series 5 , 7 , 10 , 23 , 35 , 45 , 51 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 95 , 96 , 100 , 103 , 104 , 107 fulfilled the inclusion criteria. Figure 1 shows the selection process in detail.
FIGURE 1.
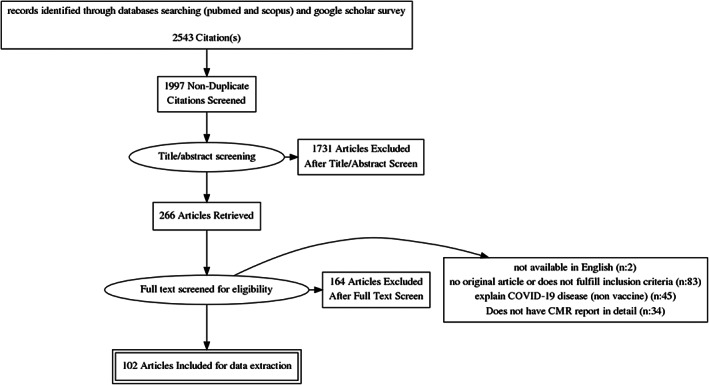
PRISMA flowchart of literature search and selection process
A total of 468 patients with suspected myocarditis and cardiac MRI findings were included in this study (n = 294 from case reports/case series with IPD 5 , 7 , 9 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 68 , 70 , 71 , 72 , 73 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 89 , 91 , 92 , 93 , 94 , 95 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 and n = 174 from five case series 67 , 69 , 74 , 88 , 90 with AD). Based on data provided by 100 out of 102 studies, all included patients met CDC criteria for suspected myocarditis. Supplementary Table 2 shows the quality of the included case series; all studies scored eight or higher.
TABLE 2.
Study Characteristics and Cardiac MRI Findings in Case Series With Aggregated‐Level Data
| ID | Author | N | Male/Female | Age (Years) | Type of Vaccine | First/SeconD dose | Time From Vaccine to Symptom (Days) | Cardiac Symptoms and Biomarkers and ECG | Echocardiography Findings | Time From Vaccine to MRI (Day) | Cardiac MRI Findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Jain et al (2021) | 56 | NR | 12–20 | mRNA (NR) | 0/56 | 0–7 |
Chest pain: 56/56 Elevated troponin: 56/56 |
NR | 4.9 (2.3) a |
Abnormal T2: 50/56 (89%) LGE: 49/56 (88%) Inferolateral or lateral: 49/49 ECV: 32.6 (9) a LLC: 49/56 (88%) LVEF: 58 (6) a Abnormal LVEF: 13/56 (23%) Others: NR |
| 2 | Montogomery et al (2021) | 8 | 8/0 | NR | mRNA (NR) | NR | <4 days |
Elevated troponin: 8/8 Chest pain: 8/8 ECG: NR |
NR | NR |
Abnormal T2: 8/8 (100%) LGE: 8/8 (100%) Subepicardial: 8/8 (100%) LLC: 8/8 (100%) Others: NR |
| 3 | Troung et al (2021) | 97 | NR | Adolescents and young adults | mRNA (Pfizer) | NR | NR | Elevated troponin: 8/8 | NR | 5 (3–17) b |
Abnormal T2: 54/97 (55.4%) LGE: 74/97 (76.3%) LLC: 49/97 (50.5%) LVEF: 60% (55%–62.7%) b Others: NR |
| 4 | Viskin et al (2021) | 7 | 6/1 | 20–34 | mRNA (Pfizer) | 0/7 | 3–7 |
Chest pain: 7/7 Elevated troponin: 7/7 Abnormal ECG: 4/7 Hospitalized: 7/7 |
LVEF < 55%: 2/7 | NR |
Abnormal T2: 1/7 (14%) LGE: 6/7 (86%) Subepicardial: 1/6 (17%) Subepicardial and midwall: 5/6 (83%) LLC: 6/7 (86%) Others: NR |
| 5 | Pfajfer et al (2021) | 3 | 3/0 | 17 [17] a | mRNA (Pfizer) | 2/1 | 1–10 |
Chest pain: 3/3 Elevated troponin: 3/3 Abnormal ECG: 1/3 ST‐Elevation: 0/3 Hospitalized: 3/3 |
LVEF < 55%: 0/3 WMA: 0/3 Pericardial Effusion: 0/3 |
5–10 |
Abnormal T2: 0/3 LGE: 3/3 Subepicardial: 2/3 Midwall: 1/3 LLC: 0/3 Precardial Effusion: 1/3 Abnormal LVEF: 0/3 Others: NR |
| 6 | Lyengar et al (2022) | 3 | NR | 27 | NR | 0/3 | 3 |
Chest pain: 3/3 Elevated troponin: 3/3 Abnormal ECG: 2/3 ST‐Elevation: 2/3 Hospitalized: 3/3 |
LVEF < 55%: 2/3 | 3–5 |
Abnormal T2: 3/3 (100%) LGE: 3/3 (100%) Subepicardial: 2/3 (66%) Subepicardial and Midwall: (33%) LLC:NR Others: NR |
ECV = extracellular volume; ECG = electrocardiography; LGE = late gadolinium enhancement; LLC = Lake Louise criteria; LVEF = left ventricular ejection fraction; mRNA = messenger ribonucleic acid; NR = not reported; WMA = wall motion abnormality.
Mean (standard deviation).
Median (inter quartile range).
Characteristic and Cardiac MRI Findings of Patients in IPD Studies
Detailed characteristics and cardiac MRI findings of each included IPD study are presented in Supplementary Tables S3 and S4, respectively. Table 1 summarizes baseline characteristics and cardiac MRI findings in 294 patients. Overall, 89.8% (264/294) of the included patients were male with a mean age of 27.3 years ([SD]: 14.1 years). The 95.2% (280/294) of evaluated cases with suspected myocarditis had a recent history of an mRNA‐based vaccination, mainly the second dose (78.2%).
TABLE 1.
Characteristics and Cardiac MRI Findings of Patients in Studies With Individual‐Level Patient Data
| Characteristics | Data Availability (n) | Findings | |
|---|---|---|---|
| Age (years), mean (SD) | 274 | 27.3 (14.1) | |
| Male, n (%) | 294 | 264 (89.8%) | |
| Survived, n (%) | 263 | 263 (100%) | |
| Vaccine type, n (%) | Pfizer (BNT162b2) | 294 | 213 (72.4%) |
| Moderna (mRNA‐1273) | 67 (22.8%) | ||
| Janssen (ad26.COV2.S) | 4 (1.4%) | ||
| AstraZeneca (chAdOx1‐SARS‐COV‐2) | 9 (3.1%) | ||
| Covaxin (BBV152) | 1 (0.3%) | ||
| Vaccine dose, n (%) | First dose | 293 | 54 (18.4%) |
| Second dose | 230 (78.2%) | ||
| Third dose | 9 (3.1%) | ||
| Time from vaccine to symptoms (day), median (IQR) | 282 | 3 (2.0 to 4.0) | |
| Symptom type, n (%) | Chest pain | 266 | 254 (95.4%) |
| Dyspnea | 58 (21.8%) | ||
| Abnormal ECG | 259 | 221 (85.3%) | |
| ST segment elevation | 198 | 150 (75.7%) | |
| Diffuse PR depression | 32 (16.1%) | ||
| Nonspecific ST‐T changes | 41 (20.7%) | ||
| Elevated troponin, n (%) | 278 | 276 (99.3%) | |
| Echocardiography findings | |||
| LVEF (%), mean (SD) | 137 | 53.70 (9.4) | |
| LVEF < 50%, n (%) | 137 | 34 (24.8%) | |
| LVEF < 55%, n (%) | 203 | 63 (31%) | |
| Pericardial effusion, n (%) | 95 | 7 (7.3%) | |
| Wall motion abnormality, n (%) | 113 | 49 (43.3%) | |
| Cardiac MRI findings | |||
| Time from vaccine to MRI (day), Median (IQR) | 68 | 6.0 (5 to 8.8) | |
| Lake louise criteria, n (%) | 114 | 99 (86.8%) | |
| Native T1 (msec), Mean (SD) | 73 | 1083.91 (94.3) | |
| Elevated T1, n (%) | 102 | 76 (74.5%) | |
| Native T2 (msec), Mean (SD) | 69 | 55.9 (9.5) | |
| Elevated Native T2, n (%) | 102 | 62 (60.8%) | |
| T2 weighted or T2 STIR or T2 mapping abnormality, n (%) | 160 | 131 (81.9%) | |
| Myocardial LGE, n (%) | |||
| Positive LGE | 285 | 268 (94%) | |
| LGE Pattern | |||
| Subepicardial + & Mid wall −, n (%) | 208 | 137 (65.9%) | |
| Subepicardial − & Mid wall +, n (%) | 23 (11.1%) | ||
| Subepicardial + & Mid wall +, n (%) | 46 (22.1%) | ||
| Subepicardial + | Mid wall +, n (%) | 206 (99.0%) | ||
| Subepicardial − & Mid wall −, n (%) | 2 (0.9%) | ||
| Subepicardial/Mixed LGE | 208 | 183 (88.0) | |
| Mid wall/Mixed LGE | 208 | 69 (33.2%) | |
| Nonischemic pattern of myocarditis, n (%) | 214 | 214 (100%) | |
| Involved segment, n (%) | |||
| Basal or mid inferolateral, n (%) | 202 | 124 (61.4%) | |
| Other segments, n (%) | 202 | 78 (38.6%) | |
| ECV (%), Mean (SD) | 50 | 29.61 (6.04) | |
| ECV > 30%, n (%) | 16 (32%) | ||
| LVEF (%), Mean (SD) | 155 | 56.7 (7.57) | |
| LVEF <55%, n (%) | 177 | 58 (32.8%) | |
| LVEF <50%, n (%) | 174 | 16 (9.2%) | |
| Wall motion abnormality, n (%) | 93 | 29 (31.2%) | |
| Pericardial enhancement, n (%) | 119 | 39 (32.8%) | |
| Pericardial effusion, n (%) | 147 | 40 (27.2%) | |
ECV = extracellular volume; ECG = electrocardiography; IQR = interquartile range; LGE = late gadolinium enhancement; LVEF = left ventricular ejection fraction; mRNA = messenger ribonucleic acid; N = number; SD = standard deviation; STIR = short‐tau inversion recovery.
Survival status was reported for 263 patients; death occurred in none of them and all were discharged in favorable clinical conditions. Overall, 95.4% (254/266) of patients presented with chest pain and 21.8% (58/266) with dyspnea. The median (IQR) time from vaccine to symptoms was 3.0 days (2.0–4.0 days). ECG data were available in 259 cases, and 221 (85.3%) of them had abnormal findings, mainly ST‐segment elevations (75.7% [150/198]). An elevated troponin level was found in 276 of 278 evaluated cases. Echocardiography showed LVEF < 50% in 24.8% (34/137) of patients, PE in 7.3% (7/95), and WMA in 43.3% (49/113).
The median time from vaccine to MRI was 6.0 days (IQR: 5.0–8.8 days). On cardiac MRI, diagnosis of myocarditis was established in 99 (86.6%) of 114 patients using revised/old Lake Louise criteria (LLC).
Myocardial LGE was detected in 94.0% (268/285) of patients, predominantly with a subepicardial and/or mid‐wall pattern (99.0% [206/208]) and localized in the basal or mid inferolateral segment of the LV (61.4% [124/202]). Mean (SD) T2, reported in 69 patients, was 55.9 ms (9.5 msec). Abnormal T2, detected by quantitative or qualitative methods, was found in 81.9% (131/160). Mean (SD) T1 was 1083.91 msec (94.3 msec) (n = 73), and abnormal T1 was observed in 74.5% (76/102). Mean (SD) ECV was 29.61 (6.4), and in 32% (16/50) it was greater than 30%.
On cardiac MRI, regarding pericardial involvement, effusion was observed in 27.2% (40/147) of patients and enhancement in 32.8% (39/119). The mean (SD) LVEF was 56.7% (7.57%), and 16 out of 174 (9.2%) patients had an impaired LVEF (<50%). Overall, WMA was found in 29 out of 93 assessed patients (31.2%).
Characteristic and Cardiac MRI Findings of AD Studies
Six case series reported aggregated characteristic and cardiac MRI findings of 174 patients with suspected myocarditis following mRNA‐based COVID‐19 vaccines (Table 2). Sample sizes varied from 3 to 97 patients. Overall, patients were teenagers and young adults who presented with elevated troponin and chest pain. The reported mean/median time from symptoms to cardiac MRI was less than 7 days.
In summary, cardiac MRI findings in AD studies were as follows: myocarditis based on LLC in 65% (112/171), abnormal T2 in 66.6% (116/174), and LGE in 82.2% (143/174) of patients. The pattern of LGE was reported only in four studies with 21 patients and it was subepicardial and/or mid‐wall in all of them.
Pooled Analyses of Individual and Aggregated‐Level Cardiac MRI Data
Data heterogeneity, described by I 2, was high in all parameters, except for LVEF. Hence, we reported results of the random effects model for these variables (Fig. 2). In our pooled analyses, 79% (95% confidence interval [CI]: 54%–97%; I 2: 91%) of patients with suspected clinical myocarditis met the LLC. Elevated T2 measured by a qualitative or quantitative method was found in 72% (95% CI: 50%–90%; I 2: 89%) and elevated quantitative native T2 in 69% of cases (95% CI: 37%–95%; I 2: 89%). Myocardial LGE was detected in 93% (95% CI: 83%–99%; I 2: 73%) of patients (subepicardial/mid‐wall pattern: 206/208 [99.0%]). In addition, LVEF less than 55% and 50% was observed in 28% (95% CI: 22%–35%; I 2: 38%, P value = 0.20) and 4% (95% CI: 1%–9%; I 2: 0.0%, P value = 0.85) of patients, respectively. Pooled mean LVEF was 58.35% (95% CI: 56.57–60.14%; I 2: 83.0%) (Fig. 2 and Supplementary Fig. S1).
FIGURE 2.
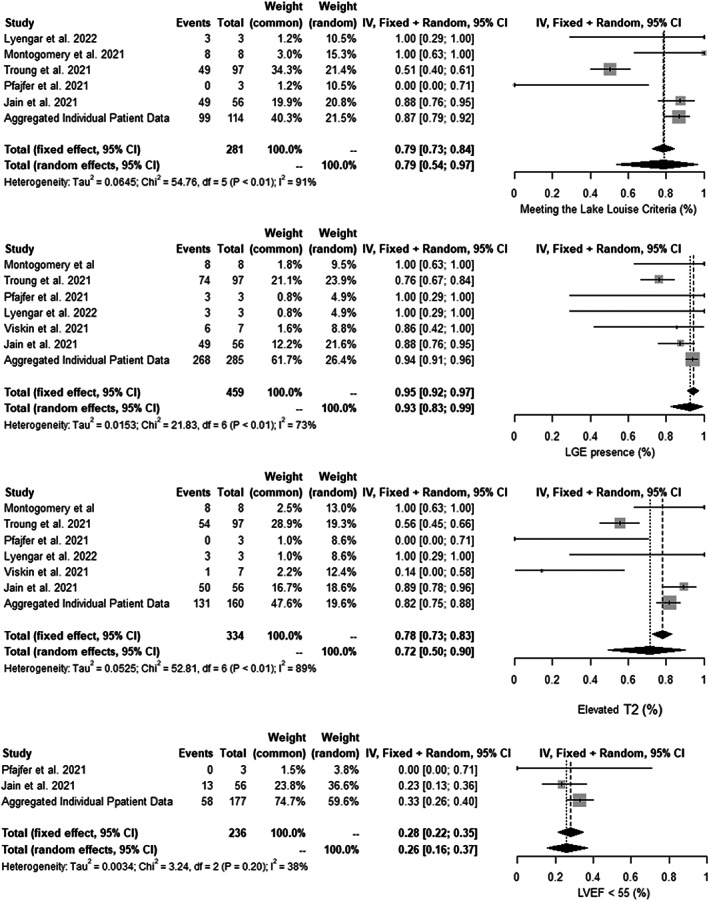
Forest plot showing percentage (95% confidence interval [CI]) of cardiac MRI abnormalities in patients with suspected myocarditis following COVID‐19 vaccination.
Discussion
Based on our systematic review and meta‐analysis approach, cardiac MRI diagnosis of myocarditis was established in three‐quarters of patients presenting with suspected clinical myocarditis following the COVID‐19 vaccine according to the LLC. Elevated T2, assessed by a qualitative or quantitative method, was detected in 72% of patients (50%–90%). Also, 93% (83%–99%) had myocardial LGE, predominantly located in the basal inferolateral wall with a subepicardial and/or mid‐wall pattern. Most patients (96%) had a preserved LVEF (LVEF > 50%). In addition, elevated T1 and ECV > 30% were found in 74.5% (76/91102) and 32% (16/50) of patients, respectively. Less than one‐third of patients had WMA.
Diagnosis of myocarditis is still challenging due to the heterogeneity of clinical presentations, multiple potential underlying etiologies, and variable severity and prognosis. 108 , 109 The abilities of cardiac MRI make it the first choice for the noninvasive assessment of suspected cases. 110
Based on available evidence, the patterns of myocardial injury in COVID‐19 vaccine‐associated myocarditis are similar to findings in acute myocarditis induced by other causes such as viral and idiopathic myocarditis. In a cardiac MRI study of patients meeting both clinical and imaging diagnostic criteria for acute myocarditis, Fronza et al found a similar pattern of cardiac injury in patients with COVID‐19 vaccine‐associated myocarditis compared to those with myocarditis induced by COVID‐19 disease and other causes; the most frequent pattern of LGE in three groups was subepicardial with basal inferolateral wall distribution. 9 However, septal involvement was less frequent in the vaccine‐associated myocarditis group. 9
In 2009, LLC was defined as diagnostic cardiac MRI criteria for patients with suspected myocarditis. 111 In this multiparametric approach, acute myocarditis diagnosis was established with at least two out of three of the following tissue‐based cardiac MRI markers: T2‐weighted ratio, early gadolinium enhancement (EGE), and LGE. 111 To improve the diagnostic performance of the recommended criteria, LLC was revised following the introduction of mapping techniques in 2018. 8 In the revised LLC, the presence of at least one edema‐sensitive cardiac MRI criteria (T2‐weighted images or T2 mapping) combined with at least one additional T1‐based tissue characterization technique (LGE, T1 mapping, or ECV) was considered as a positive case. 8 In patients with clinically suspected myocarditis, the presence of only one T1‐/T2‐based marker may still support the diagnosis of myocardial inflammation. LV systolic dysfunction and presence of pericardial involvement are supportive parameters but not required for the diagnosis of myocarditis based on both the revised and original LLC. 4 Based on our pooled analyses of available cardiac MRI studies, LLC‐based diagnosis of myocarditis was established in over two‐thirds of patients with suspected myocarditis following COVID‐19 vaccination. However, included studies mainly failed to provide information on the version of utilized LLC.
Myocardial involvement seems to be less severe in COVID‐19 vaccine‐associated myocarditis than those induced by other causes. Based on our analyses, most patients with myocarditis following the COVID‐19 vaccination had a preserved LVEF, and WMA was not common in these patients. In the study by Fronza et al, patients with vaccine‐associated myocarditis had markedly less cardiac functional impairment, lower noncontrast T1, and less frequent involvement of the septum compared to patients with myocarditis induced by other causes. 9
Based on our systematic review, all reported cases with abnormal cardiac MRI findings showed a favorable clinical course at the acute phase. Similarly, myocarditis induced by other causes was recognized to be self‐resolving in patients presenting with mild symptoms, even with minimal ventricular dysfunction. However, progression to dilated cardiomyopathy can occur in up to 30% of patients with biopsy‐proven myocarditis. 112 In a follow‐up study by Chalala et al, three out of five patients reported mild intermittent self‐resolving chest pain after discharge, leading to an emergency department visit in one patient. 7 Two patients underwent a second cardiac MRI 3 months after discharge, showing a persistent but diminished LGE with a similar distribution as compared to the initial MRI. 7 In 2019, Aquaro et al evaluated the clinical and prognostic role of 6‐month repetition of cardiac MRI in patients with acute myocarditis and found that LGE persisted at 6 months in about 90% of cases. 6 The presence of LGE without edema at a 6‐month cardiac MRI was the predictor of a worse prognosis, particularly in those with a mid‐wall septal pattern; the presence of edema shows a residual chance of recovery. 6 Cardiac MRI can be useful in the follow‐up examination of patients with myocarditis to detect the disease activity and progression. 113
Limitations
As a review of published reports, one of our major limitations was that a core laboratory did not review the actual images. Our data sets were incomplete for several variables, mainly due to the retrospective design of the included studies. Furthermore, the majority of included studies were conducted in the United States and European countries, and thus caution should be taken in generalizing the findings of this review to other populations. However, we performed a comprehensive search strategy and included all relevant studies to present a synthesis of currently existing evidence.
Conclusion
Diagnosis of myocarditis may be detected in over two‐thirds of patients with suspected myocarditis following COVID‐19 vaccination using the LLC. Myocardial LGE with a nonsischemic pattern and elevated T2 might probably be the most common cardiac MRI findings in these patients.
Supporting information
Supplementary Table 1 Search strategy
Supplementary Table 2: Quality of the included studies
Supplementary Table 3: Characteristics of the included studies
Supplementary Table 4: Cardiac MRI findings
Figure S1: The random and fixed effects model for proportions (95% confidence interval [CI]) of other cardiac MRI abnormalities
Acknowledgment
Researchers appreciated the Clinical Research Development Units of Kamali and Rajaee Hospitals in Alborz University of Medical Sciences.
Parham Samimisedeh and Elmira Jafari Afshar equally contributed as first authors.
Contributor Information
Neda Shafiabadi Hassani, Email: drnsh2005@yahoo.com.
Hadith Rastad, Email: h.rastad91@gmail.com.
References
- 1. Cossarizza A, De Biasi S, Guaraldi G, Girardis M, Mussini C, Group MCW . SARS‐CoV‐2, the virus that causes COVID‐19: Cytometry and the new challenge for global health. Cytometry 2020;97:340‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Flanagan KL, MacIntyre CR, McIntyre PB, Nelson MR. SARS‐CoV‐2 vaccines: Where are we now? J Allergy Clin Immunol Pract 2021;9:3535‐3543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riad A, Hocková B, Kantorová L, et al. Side effects of mRNA‐based COVID‐19 vaccine: Nationwide phase IV study among healthcare workers in Slovakia. Pharmaceuticals 2021;14:873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sanchez Tijmes F, Thavendiranathan P, Udell JA, Seidman MA, Hanneman K. Cardiac MRI assessment of nonischemic myocardial inflammation: State of the art review and update on myocarditis associated with COVID‐19 vaccination. Radiology 2021;3:e210252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID‐19 mRNA vaccines. Circulation 2021;144:471‐484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aquaro GD, Ghebru Habtemicael Y, Camastra G, et al. Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J Am Coll Cardiol 2019;74:2439‐2448. [DOI] [PubMed] [Google Scholar]
- 7. Chelala L, Jeudy J, Hossain R, Rosenthal G, Pietris N, White C. Cardiac MRI findings of myocarditis after COVID‐19 mRNA vaccination in adolescents. Am J Roentgenol 2022;218:651‐657. [DOI] [PubMed] [Google Scholar]
- 8. Ferreira VM, Schulz‐Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: Expert recommendations. J Am Coll Cardiol 2018;72:3158‐3176. [DOI] [PubMed] [Google Scholar]
- 9. Fronza M, Thavendiranathan P, Chan V, et al. Myocardial injury pattern at MRI in COVID‐19 vaccine–associated myocarditis. Radiology 2022; in press. 10.1148/radiol.212559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim HW, Jenista ER, Wendell DC, et al. Patients with acute myocarditis following mRNA COVID‐19 vaccination. JAMA Cardiol 2021;6:1196‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Klugar M, Riad A, Mekhemar M, et al. Side effects of mRNA‐based and viral vector‐based COVID‐19 vaccines among German healthcare workers. Biology 2021;10:752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abbate A, Gavin J, Madanchi N, et al. Fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 mRNA COVID‐19 vaccination in two patients. Int J Cardiol 2021;340:119‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Agdamag ACC, Gonzalez D, Carlson K, et al. Fulminant myocarditis following coronavirus disease 2019 vaccination: A case report. Eur Heart J 2022;6:ytac007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Albert E, Aurigemma G, Saucedo J, Gerson DS. Myocarditis following COVID‐19 vaccination. Radiol Case Rep 2021;16:2142‐2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ammirati E, Cavalotti C, Milazzo A, et al. Temporal relation between second dose BNT162b2 mRNA Covid‐19 vaccine and cardiac involvement in a patient with previous SARS‐COV‐2 infection. Int J Cardiol Heart Vasc 2021; in press. Epub ahead of print. 10.1016/j.ijcha.2021.100778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Azir M, Inman B, Webb J, Tannenbaum L. STEMI mimic: Focal myocarditis in an adolescent patient after mRNA COVID‐19 vaccine. J Emerg Med 2021;61:e129‐e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cereda A, Conca C, Barbieri L, et al. Acute myocarditis after the second dose of SARS‐CoV‐2 vaccine: Serendipity or atypical causal relationship? Anatol J Cardiol 2021;25:522‐523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chai Q, Nygaard U, Schmidt RC, Zaremba T, Møller AM, Thorvig CM. Multisystem inflammatory syndrome in a male adolescent after his second Pfizer‐BioNTech COVID‐19 vaccine. Acta Paediatr 2022;111:125‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cimaglia P, Tolomeo P, Rapezzi C. Acute myocarditis after SARS‐CoV‐2 vaccination in a 24‐year‐old man. Rev Port Cardiol 2022;41:71‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid Synth 2020;18:2127‐2133. [DOI] [PubMed] [Google Scholar]
- 21. Shumkova M, Vassilev D, Karamfiloff K, et al. Acute myocarditis associated with the Pfizer/BioNTech vaccine. Kardiol Pol 2021;79:1282‐1283. [DOI] [PubMed] [Google Scholar]
- 22. D'Angelo T, Cattafi A, Carerj ML, et al. Myocarditis after SARS‐CoV‐2 vaccination: A vaccine‐induced reaction? Can J Cardiol 2021;37:1665‐1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Di Tano G, Moschini L, Calvaruso EV, Danzi GB. Recurrent myocarditis after the first dose of SARS‐CoV‐2 mRNA‐1273 vaccine. MedRxiv 2021;6:2018. [Google Scholar]
- 24. Ehrlich P, Klingel K, Ohlmann‐Knafo S, et al. Biopsy‐proven lymphocytic myocarditis following first mRNA COVID‐19 vaccination in a 40‐year‐old male: Case report. Clin Res Cardiol 2021;110:1855‐1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. García B, Ortega P, Fernández JAB, León AC, Burgos LR, Dorta EC. Acute myocarditis after administration of the BNT162b2 vaccine against COVID‐19. Rev Esp Cardiol 2021;74:812‐814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gautam N, Saluja P, Fudim M, Jambhekar K, Pandey T, Al'Aref S. A late presentation of COVID‐19 vaccine‐induced myocarditis. Cureus 2021;13:e17890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Habedank D, Lagast A, Novoa‐Usme M, Atmowihardjo I. A case of myocarditis in a 60‐year‐old man 48 h after mRNA vaccination against SARS‐CoV2. Clin Res Cardiol 2021;111:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Habib MB, Hamamyh T, Elyas A, Altermanini M, Elhassan M. Acute myocarditis following administration of BNT162b2 vaccine. IDCases 2021;25:e01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hasnie AA, Hasnie UA, Patel N, et al. Perimyocarditis following first dose of the mRNA‐1273 SARS‐CoV‐2 (Moderna) vaccine in a healthy young male: A case report. BMC Cardiovasc Disord 2021;21:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hung Y‐P, Sun K‐S. A case of myopericarditis with pleuritis following AstraZeneca covid‐19 vaccination. QJM 2021;114:879‐881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Isaak A, Feisst A, Luetkens JA. Myocarditis following COVID‐19 vaccination. Radiology 2021;301:E378‐E379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaneta K, Yokoi K, Jojima K, Kotooka N, Node K. Young male with myocarditis following mRNA‐1273 vaccination against coronavirus disease‐2019 (COVID‐19). Circ J 2022;86:721. [DOI] [PubMed] [Google Scholar]
- 33. Kim I‐C, Kim H, Lee HJ, Kim JY, Kim J‐Y. Cardiac imaging of acute myocarditis following COVID‐19 mRNA vaccination. J Korean Med Sci 2021;36:e229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. King WW, Petersen MR, Matar RM, Budweg JB, Pardo LC, Petersen JW. Myocarditis following mRNA vaccination against SARS‐CoV‐2, a case series. Am Heart J Plus 2021;8:100042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Koizumi T, Awaya T, Yoshioka K, et al. Myocarditis after COVID‐19 mRNA vaccines. QJM 2021;114:741‐743. [DOI] [PubMed] [Google Scholar]
- 36. Minocha PK, Better D, Singh RK, Hoque T. Recurrence of acute myocarditis temporally associated with receipt of the mRNA coronavirus disease 2019 (COVID‐19) vaccine in a male adolescent. J Pediatr 2021;238:321‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miqdad MA, Nasser H, Alshehri A, Mourad AR. Acute myocarditis following the administration of the Second BNT162b2 COVID‐19 vaccine dose. Cureus 2021;13:e18880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mohammadi A, Rezaiye M, Goharrizi MASB. Acute myocarditis following the third dose of SARS‐CoV‐2 vaccine: A case report. MedRxiv 2022. 10.21203/rs.3.rs-1220786/v1. [DOI] [Google Scholar]
- 39. Muthukumar A, Narasimhan M, Li Q‐Z, et al. In‐depth evaluation of a case of presumed myocarditis after the second dose of COVID‐19 mRNA vaccine. Circulation 2021;144:487‐498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nguyen TD, Mall G, Westphal JG, Weingärtner O, Möbius‐Winkler S, Schulze PC. Acute myocarditis after COVID‐19 vaccination with mRNA‐1273 in a patient with former SARS‐CoV‐2 infection. ESC Heart Fail 2021;8:4710‐4714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Owuor H, Gikonyo A, Ponoth P, Gikonyo D. Covid vaccine induced myocarditis: A bolt from the blue: A case report. J Cardiovasc Med Surg 2021;7:51‐55. [Google Scholar]
- 42. Chen JH, Ikwuanusi IA, Bommu VJL, et al. COVID‐19 vaccine‐related myocarditis: A descriptive study of 40 case reports. Cureus 2022;14:e21740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Park J, Brekke DR, Bratincsak A. Self‐limited myocarditis presenting with chest pain and ST segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine. Cardiol Young 2022;32:146‐149. [DOI] [PubMed] [Google Scholar]
- 44. Patrignani A, Schicchi N, Calcagnoli F, et al. Acute myocarditis following Comirnaty vaccination in a healthy man with previous SARS‐CoV‐2 infection. Radiol Case Rep 2021;16:3321‐3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schmitt P, Demoulin R, Poyet R, et al. Acute myocarditis after COVID‐19 vaccination: A case report. Rev Med Interne 2021;42:797‐800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Singh B, Kaur P, Cedeno L, et al. COVID‐19 mRNA vaccine and myocarditis. Eur J Case Rep Int Med 2021;8:002681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sivakumaran P, Sunny J, Tsagkridi A, Khanji MY. Myopericarditis following SARS‐CoV‐2 mRNA vaccine: The role of cardiac biomarkers and multimodality imaging. Eur Heart J‐Cardiovasc Imaging 2022;23:e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sokolska JM, Kurcz J, Kosmala W. Every rose has its thorns—Acute myocarditis following COVID‐19 vaccination. Kardiol Pol 2021;79:1153‐1154. [DOI] [PubMed] [Google Scholar]
- 49. Sulemankhil I, Abdelrahman M, Negi SI. Temporal association between the COVID‐19 Ad26. COV2. S vaccine and acute myocarditis: A case report and literature review. Cardiovasc Revasc Med 2022;38:117‐123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Tailor PD, Feighery AM, El‐Sabawi B, Prasad A. Case report: Acute myocarditis following the second dose of mRNA‐1273 SARS‐CoV‐2 vaccine. Eur Heart J 2021;5:ytab319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Marshall M, Ferguson ID, Lewis P, et al. Symptomatic acute myocarditis in 7 adolescents after Pfizer‐BioNTech COVID‐19 vaccination. Pediatrics 2021;148:e2021052478. [DOI] [PubMed] [Google Scholar]
- 52. Tiwari A, Chakrabarti SS, Panda PK, Karna G, Kaur U. Hyper‐eosinophilic syndrome with myocarditis after inactivated SARS‐CoV‐2 vaccination: A case study. MedRxiv 2021. 10.2174/1574886317666220509165317. [DOI] [PubMed] [Google Scholar]
- 53. Umei TC, Kishino Y, Watanabe K, et al. Recurrence of myopericarditis following mRNA COVID‐19 vaccination in a male adolescent. CJC Open 2022;4:350‐352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Van Kerkhove O, Renders F, Leys M. A case of myocarditis following ChAdOx1 nCov‐19 vaccination. Acta Cardiol 2022;77:1‐3. [DOI] [PubMed] [Google Scholar]
- 55. Vollmann D, Eiffert H, Schuster A. Acute perimyocarditis following first dose of mRNA vaccine against COVID‐19. Dtsch Arztebl Int 2021;118:546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Williams CB, Choi J‐i, Hosseini F, Roberts J, Ramanathan K, Ong K. Acute myocarditis following mRNA‐1273 SARS‐CoV‐2 vaccination. CJC Open 2021;3:1410‐1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wilson H, Norris MD, Frosch O, Agarwal PP. Late gadolinium enhancement after COVID‐19 vaccination. Radiology 2021;3:e210199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wong J, Sharma S, Yao JV, Aggarwal A, Grigg L. COVID‐19 mRNA vaccine (Comirnaty)‐induced myocarditis. Med J Aust 2022;216:122‐123. [DOI] [PubMed] [Google Scholar]
- 59. Aviram G, Viskin D, Topilsky Y, et al. Myocarditis associated with COVID‐19 booster vaccination. Circ Cardiovasc Imaging. 2022;15:e013771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bews H, Bryson A, Bortoluzzi T, Tam JW, Jassal DS. COVID‐19 vaccination induced myopericarditis: An imager's perspective. CJC Open 2022; in press. 10.1016/j.cjco.2022.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Chamling B, Vehof V, Drakos S, et al. Occurrence of acute infarct‐like myocarditis following COVID‐19 vaccination: Just an accidental co‐incidence or rather vaccination‐associated autoimmune myocarditis? Clin Res Cardiol 2021;110:1850‐1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Das BB, Kohli U, Ramachandran P, et al. Myopericarditis after messenger RNA coronavirus disease 2019 vaccination in adolescents 12 to 18 years of age. J Pediatr 2021;238:26‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Di Dedda EA, Barison A, Aquaro GD, et al. Cardiac magnetic resonance imaging of myocarditis and pericarditis following COVID‐19 vaccination: A multicenter collection of 27 cases. Eur Radiol 2022; in press. Epub ahead of print. 10.1007/s00330-022-08566-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Dickey JB, Albert E, Badr M, et al. A series of patients with myocarditis following SARS‐CoV‐2 vaccination with mRNA‐1279 and BNT162b2. Cardiovascular Imaging 2021;14:1862‐1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Fleming‐Nouri A, Haimovich AD, Yang D, Schulz WL, Coppi A, Taylor RA. Myopericarditis in young adults presenting to the emergency department after receiving a second COVID‐19 mRNA vaccine. Acad Emerg Med 2021;28:802‐805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Freise NF, Kivel M, Grebe O, et al. Acute cardiac side effects after COVID‐19 mRNA vaccination, a case series. MedRxiv 2021. 10.21203/rs.3.rs-1157175/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jain SS, Steele JM, Fonseca B, et al. COVID‐19 vaccination–associated myocarditis in adolescents. Pediatrics 2021;148:e2021053427. [DOI] [PubMed] [Google Scholar]
- 68. Larson KF, Ammirati E, Adler ED, et al. Myocarditis after BNT162b2 and mRNA‐1273 vaccination. Circulation 2021;144:506‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Łaźniak‐Pfajfer A, Surmacz R, Rajewska‐Tabor J, Pyda M, Lesiak M, Bobkowski W. Myocarditis associated with COVID‐19 vaccination in three teenage males. Pol Arch Intern Med 2022;132:16160. [DOI] [PubMed] [Google Scholar]
- 70. Levin D, Shimon G, Fadlon‐Derai M, et al. Myocarditis following COVID‐19 vaccination–a case series. Vaccine 2021;39:6195‐6200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Manfredi R, Bianco F, Bucciarelli V, et al. Clinical profiles and CMR findings of young adults and pediatrics with acute myocarditis following mRNA COVID‐19 vaccination: A case series. Vaccine 2022;10:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Mansour J, Short RG, Bhalla S, et al. Acute myocarditis after a second dose of the mRNA COVID‐19 vaccine: A report of two cases. Clin Imaging 2021;78:247‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Meyer‐Szary J, Bazgier M, Lubocka P, Dorniak K, Sabiniewicz R. Cardiac magnetic resonance characteristics of acute myocarditis occurring after mRNA‐based COVID‐19 vaccines immunization. Cardiol J 2022;29:160‐162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Montgomery J, Ryan M, Engler R, et al. Myocarditis following immunization with mRNA COVID‐19 vaccines in members of the US military. JAMA Cardiol 2021;6:1202‐1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Mouch SA, Roguin A, Hellou E, et al. Myocarditis following COVID‐19 mRNA vaccination. Vaccine 2021;39:3790‐3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Murakami Y, Shinohara M, Oka Y, et al. Myocarditis following a COVID‐19 messenger RNA vaccination: A Japanese case series. Intern Med 2022;61:8731‐8721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Nunn S, Kersten J, Tadic M, et al. Case report: Myocarditis after COVID‐19 vaccination–case series and literature review. Front Med 2022;9:836620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Onderko L, Starobin B, Riviere AE, et al. Myocarditis in the setting of recent COVID‐19 vaccination. Case reports. Cardiology 2021;2021:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Pareek M, Asnes J, Baldassarre L, et al. Myopericarditis after Covid‐19 vaccination–A case series. 2021. Available at SSRN: 10.2139/ssrn.3874571. [DOI]
- 80. Patel YR, Louis DW, Atalay M, Agarwal S, Shah NR. Cardiovascular magnetic resonance findings in young adult patients with acute myocarditis following mRNA COVID‐19 vaccination: A case series. J Cardiovasc Magn Reson 2021;23:1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Perez Y, Levy ER, Joshi AY, et al. Myocarditis following COVID‐19 mRNA vaccine: A case series and incidence rate determination. Clin Infect Dis 2021. 10.1093/cid/ciab926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Rosner CM, Genovese L, Tehrani BN, et al. Myocarditis temporally associated with COVID‐19 vaccination. Circulation 2021;144:502‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Schauer J, Buddhe S, Colyer J, et al. Myopericarditis after the Pfizer messenger ribonucleic acid coronavirus disease vaccine in adolescents. J Pediatr 2021;238:317‐320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Shaw KE, Cavalcante JL, Han BK, Gössl M. Possible association between COVID‐19 vaccine and myocarditis: Clinical and CMR findings. Cardiovasc Imaging 2021;14:1856‐1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Shiyovich A, Witberg G, Aviv Y, et al. Myocarditis following COVID‐19 vaccination: Magnetic resonance imaging study. Eur Heart J 2021. 10.1093/ehjci/jeab230. [DOI] [PubMed] [Google Scholar]
- 86. Starekova J, Bluemke DA, Bradham WS, Grist TM, Schiebler ML, Reeder SB. Myocarditis associated with mRNA COVID‐19 vaccination. Radiology 2021;301:E409‐E411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Tano E, San Martin S, Girgis S, Martinez‐Fernandez Y, Sanchez VC. Perimyocarditis in adolescents after Pfizer‐BioNTech COVID‐19 vaccine. J Pediatr Infect Dis Soc 2021;10:962‐966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Truong DT, Dionne A, Muniz JC, et al. Clinically suspected myocarditis temporally related to COVID‐19 vaccination in adolescents and young adults. Circulation 2022;145:345‐356. [DOI] [PubMed] [Google Scholar]
- 89. Vidula MK, Ambrose M, Glassberg H, et al. Myocarditis and other cardiovascular complications of the mRNA‐based COVID‐19 vaccines. Cureus 2021;13:e15576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Viskin D, Topilsky Y, Aviram G, et al. Myocarditis associated with COVID‐19 vaccination: Echocardiography, cardiac tomography, and magnetic resonance imaging findings. Circ Cardiovasc Imaging 2021;14:e013236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Bengel CP, Kacapor R. A report of two cases of myocarditis following mRNA coronavirus disease 2019 vaccination. Eur Heart J 2022;6:ytac004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Brage ET, Ruíz JR, Martín JG, et al. Fulminant myocarditis in a patient with a lung adenocarcinoma after the third dose of modern COVID‐19 vaccine. A case report and literature review. Curr Probl Cancer Case Rep 2022;6:100153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Camastra G, Ciolina F, Corsi MP, Gemmiti MP, Arcari L. Monitoring the evolution of myocarditis following COVID‐19 mRNA vaccination with serial cardiac magnetic resonance imaging. Int J Cardiovasc Imaging 2022. 10.1007/s10554-022-02603-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Fosch X, Serra J, Torres PL, Preda L, González R, Mojer F. Acute myocarditis after a third dose of the BNT162b2 COVID‐19 vaccine. Rev Esp Cardiol (Engl Ed). 2022; in press. 10.1016/j.recesp.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Frustaci A, Verardo R, Galea N, et al. Hypersensitivity myocarditis after COVID‐19 mRNA vaccination. J Clin Med 2022;11:1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Iyengar RL, Alam L, Konje S, Otobo E, Pena M, Talebi S. Acute myocarditis after MRNA COVID‐19 vaccination and diagnosis aided with cardiac magnetic resonance findings CASE series in young patients. J Am Coll Cardiol 2022;79:3101. [Google Scholar]
- 97. Kojima N, Tada H, Okada H, et al. Case report: Myocarditis associated with COVID‐19 mRNA vaccination following myocarditis associated with Campylobacter jejuni . Front Cardiovasc Med 2022;9:837759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Mengesha B, Asenov AG, Hirsh‐Raccah B, Amir O, Pappo O, Asleh R. Severe acute myocarditis after the third (booster) dose of mRNA COVID‐19 vaccination. Vaccine 2022;10:575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Rubin EJ, Longo DL. Covid‐19 mRNA vaccines—Six of one, half a dozen of the other. N Engl J Med 2022;386:183‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Moosmann J, Gentles T, Occleshaw C, Mitchelson B. COVID vaccine‐associated myocarditis in adolescent siblings: Does it run in the family? Vaccine 2022;10:611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Ohnishi M, Tanaka Y, Nishida S, Sugimoto T. Case report of acute myocarditis after administration of coronavirus disease 2019 vaccine in Japan. Eur Heart J 2022;6:ytab534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Oka A, Sudo Y, Miyoshi T, et al. Fulminant myocarditis after the second dose of COVID‐19 mRNA vaccination. Clin Case Rep 2022;10:e05378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Patel P, Desai D, Ganta N, et al. Symptomatic myocarditis post COVID‐19 vaccination. Cureus 2022;14:e24052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Puchalski M, Kamińska H, Bartoszek M, Brzewski M, Werner B. COVID‐19‐vaccination‐induced myocarditis in teenagers: Case series with further follow‐up. Int J Environ Res Public Health 2022;19:3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wu B, Mittal N, Adler ED, Hong KN. Acute myocarditis after receiving first dose of BNT162b2 mRNA vaccine. J Cardiol Cases 2022; in press. 10.1016/j.jccase.2021.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Yamamoto S, Arita Y, Ogasawara N. Myocarditis following the second dose of COVID‐19 vaccination in a Japanese adolescent. Cureus 2022;14:e23474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Sciaccaluga C, D'Ascenzi F, Cameli M, et al. Case report: Two case reports of acute myopericarditis after mRNA COVID‐19 vaccine. Front Cardiovasc Med 2022;9:827237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Cooper LT Jr, Fairweather D. We see only what we look for: Imaging cardiac inflammation. Am Heart Assoc 2013;6:165‐166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Razzano D, Fallon JT. Myocarditis: Somethings old and something new. Cardiovasc Pathol 2020;44:107155. [DOI] [PubMed] [Google Scholar]
- 110. Gannon MP, Schaub E, Grines CL, Saba SG. State of the art: Evaluation and prognostication of myocarditis using cardiac MRI. J Magn Reson Imaging 2019;49:e122‐e131. [DOI] [PubMed] [Google Scholar]
- 111. Friedrich MG, Sechtem U, Schulz‐Menger J, et al. Cardiovascular magnetic resonance in myocarditis: A JACC White paper. J Am Coll Cardiol 2009;53:1475‐1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J 2013;34:2636‐2648. [DOI] [PubMed] [Google Scholar]
- 113. Monney P, Locca D, Muzzarelli S, Hullin R, Jeanrenaud X, Schwitter J. Cardiac magnetic resonance in acute myocarditis: A new non‐invasive diagnostic gold standard? Rev Med Suisse 2012;8:1177‐1183. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1 Search strategy
Supplementary Table 2: Quality of the included studies
Supplementary Table 3: Characteristics of the included studies
Supplementary Table 4: Cardiac MRI findings
Figure S1: The random and fixed effects model for proportions (95% confidence interval [CI]) of other cardiac MRI abnormalities


