Abstract
Previous research on coronavirus disease 2019 (COVID‐19) vaccine hesitancy lacks a gender perspective, and it is unclear whether gender intersects with socioeconomic status to co‐produce inequalities in people's intent to take vaccines. The current study draws on intersectionality theory and uses data from the 2021 US Household Pulse Survey (n = 50,359). Both bivariate and multivariate statistical analyses were conducted. The results suggest that American women had a higher vaccine hesitancy rate than men. Gender interacts with socioeconomic status to shape people's vaccine hesitancy in a complex way. Specifically, women living in poverty or currently working were more vaccine‐hesitant, while poverty and employment status did not affect men's vaccine hesitancy. However, not having a college education contributed to both women's and men's COVID‐19 vaccine hesitancy. Moreover, women were more worried about the safety of the vaccine, but men's hesitancy tended to be driven by lower perceptions of COVID‐19 dangers and belief in conspiratorial claims.
Keywords: COVID‐19, gender, socioeconomic status, vaccine hesitancy
INTRODUCTION
The long‐term control of the coronavirus disease 2019 (COVID‐19) pandemic hinges on the development and uptake of preventive vaccines. In March 2021, the Biden administration started a large‐scale vaccine confidence campaign to encourage Americans to get vaccinated against the coronavirus (Diamond, 2021). According to the Centres for Disease Control and Prevention, by the end of May 2021, nearly 50.5% of Americans had received at least one dose of the COVID‐19 vaccine, and more than 40.7% were fully vaccinated (CDC, 2021). However, a sizeable proportion of the population is still hesitant about COVID‐19 vaccines. An NPR poll conducted in April 2021 suggests that one in four Americans said they would refuse a coronavirus vaccine, and another 5% were “undecided” (Brumfiel, 2021). Defined as: “delay in acceptance or refusal of vaccination despite the availability of vaccination services” (MacDonald, 2015), vaccine hesitancy is a complex cognitive and behavioural construct depending on types of vaccines, places, and times (World Health Organization, 2014). Vaccine hesitancy is particularly concerning for the global efforts to control the COVID‐19 pandemic as it prevents nations from reaching herd immunity.
In the literature of vaccine hesitancy, findings on gender have been inconsistent. For example, some researchers found that men were more likely than women to accept influenza vaccination (Nagata et al., 2013), while others argued that gender was not a consistent predictor of influenza vaccine hesitancy (Yeung et al., 2016). A linkage between gender and COVID‐19 vaccine hesitancy has been identified by recent studies. Based on an online survey (n = 672) conducted in May 2020 in the US, Malik et al. (2020) reported that women were less willing to take COVID‐19 vaccines than men. This finding was confirmed by many other studies conducted in the US or other countries (e.g., Callaghan et al., 2021; Fisher et al., 2020; Latkin, Dayton, Yi, Colon, & Kong, 2021; Lazarus et al., 2021; Malik et al., 2020; Sallam, 2021; Troiano & Nardi, 2021). However, a small group of researchers suggested different results. Khubchandani et al. (2021) surveyed a community‐based sample of the American adult population (n = 1878) in June 2020. Their analyses did not indicate gender differences in COVID‐19 vaccine hesitancy. Latkin, Dayton, Yi, Konstantopoulos, et al. (2021) conducted an online survey (n = 592) in July 2020 and found that women had greater intentions to obtain a COVID‐19 vaccine than men. Different sampling strategies, analytical approaches, and sample characteristics may have caused the mixed findings, but more importantly, neither of those studies have a particular focus on gender. In other words, the ongoing dialogue about COVID‐19 vaccine hesitancy lacks a gender perspective.
On the other hand, some evidence suggests that people's vaccine hesitancy is also related to their socioeconomic backgrounds. For instance, people with lower income and less education are less willing to pursue COVID‐19 vaccination (Callaghan et al., 2021; Fisher et al., 2020; Malik et al., 2020). Some researchers found that people who lost a job or were not working were more likely to accept a COVID‐19 vaccine than those who continued to work during the pandemic (Dror et al., 2020). Others argued that employed individuals were more inclined to take COVID‐19 vaccines than people who were unemployed (Malik et al., 2020). However, the intersection of gender and socioeconomic status remains unanswered in the context of COVID‐19 vaccine hesitancy. The intersectionality approach was first introduced by feminist scholars to study gender and race. They argued that gender and race should be examined as intersecting dimensions of oppression but not separate mechanisms of power (Collins, 1990; Crenshaw, 1989, 1991). Later, other axes of significant, such as social class, sexuality, and age, have been added to the framework (Kosnick, 2011; Zarkov, 2011). To the best of our knowledge, the intersectionality approach has never been applied to research to COVID‐19 vaccine hesitancy.
Moreover, there are other sociodemographic factors influencing people's willingness to accept vaccination. Due to interpersonal and systemic racism, less interaction with healthcare professionals, and historical biomedical‐related mistrust, racial/ethnic minorities, especially African Americans, have lower confidence in COVID‐19 vaccines (Callaghan et al., 2021; Hamel et al., 2021; Malik et al., 2020). Age is also an important predictor, as younger adults are less enthusiastic about taking COVID‐19 vaccines (Sallam, 2021). Interestingly, Khubchandani et al. (2021) noticed that in the US, COVID‐19 vaccine hesitancy was greater for people who had children at home. Dror et al. (2020) also observed that having children at home was a negative predictor for accepting COVID‐19 vaccines in Israel. In addition, recent publications suggest that hesitancy or opposition to COVID‐19 vaccination might be caused by the novelty of the disease, the rapid speed of vaccine development, mistrust in science, and the politicization of the vaccine (Funk & Tyson, 2020; Hamel et al., 2020).
In summary, to fill the gaps in the literature and advance the understanding of COVID‐19 vaccine hesitancy in the US, the current study draws on intersectionality theory and offers a novel gender perspective. We applied sophisticated statistical modeling to clarify the intersectional effects of gender and socioeconomic status on vaccine hesitancy while controlling for other sociodemographic factors. We address three key research questions: RQ1) Are there gender differences in COVID‐19 vaccine hesitancy in the US? RQ2) How does gender intersect with socioeconomic status to shape people's hesitancy towards COVID‐19 vaccination? RQ3) Do women and men have different concerns about COVID‐19 vaccines? To answer those questions, we utilize a nationally representative sample from the 2021 Household Pulse Survey (HPS), administered by the US Census Bureau.
METHODS
Data
The US HPS is designed to quickly and efficiently collect data to measure American household experiences during the coronavirus pandemic. In collaboration with other federal agencies, the US Census Bureau developed the HPS questionnaire and selected a large national representative sample by utilising its Master Address File (MAF), which is considered the gold standard frame for US statistics (Fields et al., 2020). Email addresses and mobile telephone numbers were added from the Census Bureau Contact Frame to the MAF (Fields et al., 2020). The HPS questionnaire includes questions on how education, employment, food security, health, housing, household spending, intention to receive a COVID‐19 vaccination, and transportation have been affected by the ongoing crisis.
Data used in this paper were from the Phase three collection of the HPS. Specifically, we used a sample collected between 17 February 2021 and 1 March 2021. The Census Bureau used Qualtrics as the data collection platform. Sampled households were contacted by both email and text messages, and reminders were sent to nonrespondents. In total, 1,039,370 housing units were selected from the sampling frame, and 77,788 people answered the online questionnaire. Our analyses included 50,359 respondents who reported that they had not received a COVID‐19 vaccine. We applied the recommended sampling weight to our analyses, so that the results of this study can be generalized to the national level. The publicly available microdata file was downloaded from the HPS public use file webpage (https://www.census.gov/programs‐surveys/household‐pulse‐survey/datasets.html).
Outcome measures
In Phase three of the HPS, a series of questions about people's attitudes and behaviours related to COVID‐19 vaccines were added to the questionnaire. In particular, the HPS asks: “Once a vaccine to prevent COVID‐19 is available to you, would you…” Responses include “definitely get a vaccine,” “probably get a vaccine,” “probably NOT get a vaccine,” and “definitely NOT get a vaccine.” Our primary outcome variable takes on a value of one if the respondent intended to refuse (“definitely NOT get a vaccine” or “probably NOT get a vaccine”) COVID‐19 vaccination and 0 if the respondent intended to be vaccinated (“definitely get a vaccine” or “probably get a vaccine”). We created a binary variable as the outcome measure because we were interested in what factors were associated with people being vaccine‐hesitant. Among the 50,359 respondents who had not received a COVID‐19 vaccine, 9% reported they would “definitely NOT get a vaccine,” 12% “probably NOT get a vaccine,” 19% “probably get a vaccine,” and 60% “definitely get a vaccine.”
Respondents who answered that they were hesitant to be vaccinated were presented with a follow‐up multi‐answer question asking about their specific concerns regarding COVID‐19 vaccines. Using responses to this question, we constructed four dichotomous indicators for four typical vaccine‐related concerns (see Table 1).
TABLE 1.
Descriptive statistics (n = 50,359)
| Min. | Max. | Mean | Std. Dev. | Yes | No | % Missing | |
|---|---|---|---|---|---|---|---|
| Outcome measures: | |||||||
| The intention on getting COVID‐19 vaccine | |||||||
| Definitely NOT get a vaccine | 0 | 1 | ‐ | ‐ | 4491 | 45,750 | 0.2 |
| Probably NOT get a vaccine | 0 | 1 | ‐ | ‐ | 5765 | 44,476 | 0.2 |
| Probably get a vaccine | 0 | 1 | ‐ | ‐ | 9567 | 40,674 | 0.2 |
| Definitely get a vaccine | 0 | 1 | ‐ | ‐ | 30,418 | 19,823 | 0.2 |
| Concerns related to COVID‐19 vaccines | |||||||
| “I am concerned about possible side effects of a COVID‐19 vaccine.” | 0 | 1 | ‐ | ‐ | 10,016 | 40,343 | 0.0 |
| “I don't believe I need a COVID‐19 vaccine.” | 0 | 1 | ‐ | ‐ | 2967 | 47,392 | 0.0 |
| “I don't trust the government.” | 0 | 1 | ‐ | ‐ | 3742 | 46,617 | 0.0 |
| “I am concerned about the cost of a COVID‐19 vaccine.” | 0 | 1 | ‐ | ‐ | 1094 | 49,265 | 0.0 |
| Explanatory measures: | |||||||
| Demographics | |||||||
| Age | 18 | 88 | 50.7 | 14.8 | ‐ | ‐ | ‐ |
| Sex | |||||||
| Male [ref] | 0 | 1 | ‐ | ‐ | 20,479 | 29,880 | 0.0 |
| Female | 0 | 1 | ‐ | ‐ | 29,880 | 20,479 | 0.0 |
| Race/ethnicity | |||||||
| White [ref] | 0 | 1 | ‐ | ‐ | 36,452 | 13,907 | 0.0 |
| Black | 0 | 1 | ‐ | ‐ | 4186 | 46,173 | 0.0 |
| Asian | 0 | 1 | ‐ | ‐ | 2486 | 47,873 | 0.0 |
| Hispanic | 0 | 1 | ‐ | ‐ | 5397 | 44,962 | 0.0 |
| Other racial/ethnic groups | 0 | 1 | ‐ | ‐ | 1838 | 48,521 | 0.0 |
| Socioeconomic status variables | |||||||
| Household income | |||||||
| Above the poverty threshold [ref] | 0 | 1 | ‐ | ‐ | 30,455 | 19,904 | 0.0 |
| Below the poverty threshold | 0 | 1 | ‐ | ‐ | 19,904 | 30,455 | 0.0 |
| Education level | |||||||
| Bachelor's or graduate degree [ref] | 0 | 1 | ‐ | ‐ | 25,118 | 25,241 | 0.0 |
| Below Bachelor's degree | 0 | 1 | ‐ | ‐ | 25,241 | 25,118 | 0.0 |
| Employment status | |||||||
| Employed | 0 | 1 | ‐ | ‐ | 29,977 | 20,231 | 0.3 |
| Unemployed [ref] | 0 | 1 | ‐ | ‐ | 12,523 | 37,685 | 0.3 |
| Retired | 0 | 1 | ‐ | ‐ | 7708 | 42,500 | 0.3 |
| Household structure | |||||||
| Living with children | |||||||
| No [ref] | 0 | 1 | ‐ | ‐ | 31,530 | 18,829 | 0.0 |
| Yes | 0 | 1 | ‐ | ‐ | 18,829 | 31,530 | 0.0 |
| Marital status | |||||||
| Unmarried [ref] | 0 | 1 | ‐ | ‐ | 21,476 | 28,600 | 0.6 |
| Married | 0 | 1 | ‐ | ‐ | 28,600 | 21,476 | 0.6 |
| Household size | 1 | 10 | 2.9 | 1.5 | ‐ | ‐ | ‐ |
| Building type | |||||||
| House [ref] | 0 | 1 | ‐ | ‐ | 31,572 | 9202 | 19.0 |
| Apartment | 0 | 1 | ‐ | ‐ | 7582 | 33,192 | 19.0 |
| Mobile home | 0 | 1 | ‐ | ‐ | 1412 | 39,362 | 19.0 |
| RV/van/boat | 0 | 1 | ‐ | ‐ | 208 | 40,566 | 19.0 |
| Health‐related variables | |||||||
| Had COVID‐19 | |||||||
| No [ref] | 0 | 1 | ‐ | ‐ | 43,505 | 6724 | 0.3 |
| Yes | 0 | 1 | ‐ | ‐ | 6724 | 43,505 | 0.3 |
| Covered by a health insurance | |||||||
| Yes [ref] | 0 | 0 | ‐ | ‐ | 47,900 | 2459 | 0.0 |
| No | 0 | 0 | ‐ | ‐ | 2459 | 47,900 | 0.0 |
Explanatory measures
Based on insights from previous research, we used four groups of explanatory measures: demographics, socioeconomic status, household structure, and health‐related variables. For demographics, age was calculated based on the respondent's reported date of birth; we used the respondent sex variable from the HPS (1 = female; 0 = male [reference]); race/ethnicity was recoded into five binary variables (White, non‐Hispanic [reference]; Black, non‐Hispanic; Asian, non‐Hispanic; Hispanic; Other racial/ethnic groups, non‐Hispanic). For our sample, the average age was 51 years old; 59% of respondents were female, 72% White, 8% Black, 5% Asian, 11% Hispanic, and 4% were from other racial/ethnic groups.
Socioeconomic status was measured through three dimensions. First, based on respondents' reported highest degree completed, two categories were created to measure their education level (1 = below Bachelor's degree; 0 = Bachelor's or graduate degree [reference]). Second, household income before taxes was provided by the HPS. Based on the federal poverty threshold, household income, household size, and numbers of children, we categorised respondents into two groups: living in households above the federal poverty threshold [reference] and living in households below the federal poverty threshold. Third, we included employment status: during the last 7 days, the respondent was employed [reference], unemployed, or retired. In total, 40% of respondents in our sample were from households below the poverty threshold, 50% did not have a Bachelor's degree, and 25% were unemployed when taking the survey.
In terms of household structure, we included whether the respondent was living with children (1 = yes; 0 = no [reference]), the total number of people (adults and children) living with the respondent in the same household, and the respondent's current marital status (1 = married; 0 = unmarried [reference]). We also controlled for the type of building where the respondent was living, such as a house [reference], an apartment, a mobile home, or an RV/van/boat. The average household size was 3 people, about 37% of respondents were living with children, and 57% were married. Moreover, 63% of respondents were living in a house, 15% were living in an apartment, 3% were living in a mobile house, and 0.4% were living in a recreational vehicle (RV), van, or boat.
Finally, for health‐related variables, the HPS asked whether a doctor or other health care provider ever told the respondent that she/he was infected with the coronavirus (1 = yes; 0 = no [reference]). We constructed a variable to measure if the respondent was currently covered by a health insurance or health coverage plan (1 = yes; 0 = no [reference]). In March 2021%, 13% of respondents in our sample had COVID‐19 before, and 5% did not have any health insurance. Descriptive statistics of all analysis variables are included in Table 1.
Research design and statistical analysis
Figure 1 demonstrates the overall research design of the study. In total, three sets of analyses were conducted to answer the three research questions. For Analysis I, we conducted the Chi‐square test to compare women versus men's intentions to be vaccinated against COVID‐19. Analysis II involves using generalized estimating equations (GEEs) to predict COVID‐19 vaccine hesitancy. Specifically, to examine the intersectionality between gender and socioeconomic status, two GEE models were estimated among women (Model 1) versus men (Model 2). In both models, vaccine hesitancy was used as the dependent variable, socioeconomic status variables were focal independent variables, and demographics, household structure variables, and health‐related variables were used as control variables. Analysis III was conducted among respondents who indicated that they were hesitant to take a COVID‐19 vaccine. Four GEE models (Models 3–6) were estimated to predict the four vaccine‐related concerns, in which gender was used as the focal independent variable, while other variables (i.e., socioeconomic status, demographics, household structure, health) were control variables.
FIGURE 1.
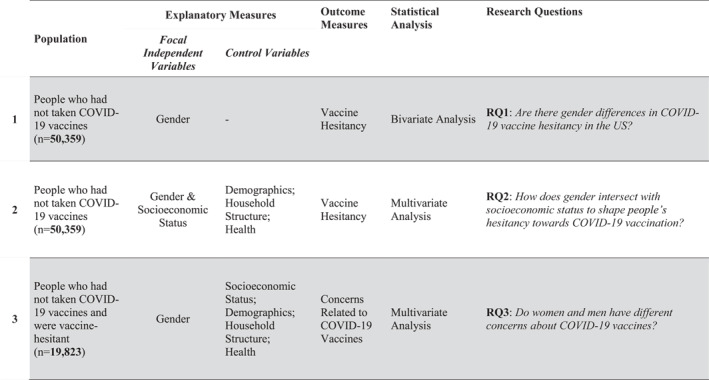
Research design
Generalized estimating equations are appropriate for this study because: first, like generalized linear models, GEEs relax the assumptions of traditional regression models (e.g., normality of variable distribution; Diggle et al., 2002; Liang & Zeger, 1986; Zeger & Liang, 1986; Zorn, 2001); second, GEEs are more suitable than generalized linear models to analyse clustered data (Zorn, 2001). The HPS data has a three‐level clustered structure: the 50,359 respondents were clustered within four census regions (i.e., Northeast, South, Midwest, West) and 50 states and Washington DC. Thus, we used census regions and states to define clusters for the two models. There were 51 clusters in total, and the number of respondents in each cluster ranged between 161 and 1811 people. Since our dependent variables were binary, we selected the binomial distribution with a logit link function under the exchangeable correlation matrix for the six models (Garson, 2012). We also used Variance Inflation Factor (VIF) and tolerance to detect whether the model results were affected by multicollinearity. The statistical software, SPSS 22, International Business Machines Corporation (IBM), was used for the three sets of analyses.
RESULTS
Are there gender differences in COVID‐19 vaccine hesitancy in the US?
We conducted the chi‐square test on gender and the four categories of the vaccine hesitancy variable. As shown in Figure 2, 10% of women (vs. 8% men) reported that they would definitely not get a COVID‐19 vaccine; 13% of women (vs. 10% men) said that they probably would not get a COVID‐19 vaccine; 20% of women (vs. 18% men) reported that they probably would get a COVID‐19 vaccine; while 57% women (vs. 64% men) said that they would definitely get a vaccine. Based on the Chi‐square test result, gender differences across the four categories were statistically significant (p < 0.0001).
FIGURE 2.
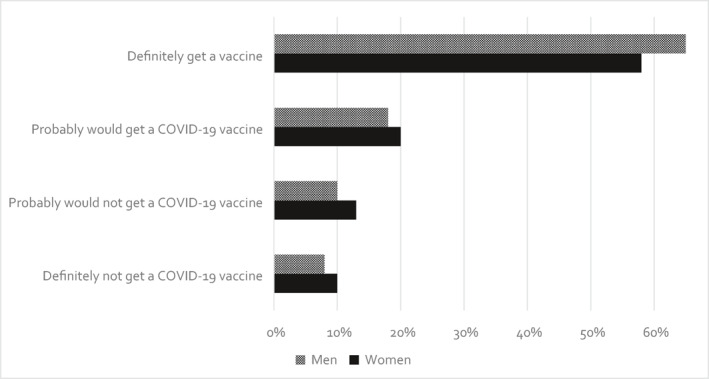
Coronavirus disease 2019 (COVID‐19) vaccine acceptance and hesitancy by gender
How does gender intersect with socioeconomic status to shape people's hesitancy towards COVID‐19 vaccination?
Table 2 reports the results from the two GEE models predicting COVID‐19 vaccine hesitancy among women (Model 1) versus men (Model 2). In terms of the three dimensions of socioeconomic status, if the respondent did not have a college degree, women were 98% (p < 0.0001), and men were 173% (p < 0.0001) more likely to be vaccine‐hesitant than their counterparts who had a college degree. Compared to women living in households above the poverty threshold, women from households below the poverty threshold were 30% more likely to be hesitant to pursue a COVID‐19 vaccine (p < 0.0001); yet, there was no statistically significant association between household income and men's vaccine hesitancy (p = 0.707). As compared to women who were unemployed, women who were retired were 24% less hesitant about COVID‐19 vaccines (p = 0.001), but women who were working were 19% more hesitant (p = 0.003). Employment status was not significantly associated with men's vaccine hesitancy (p > 0.05).
TABLE 2.
Results of the generalized estimating equation models predicting coronavirus disease 2019 (COVID‐19) vaccine hesitancy
| Model 1 (women) (n = 29,880) | Model 2 (men) (n = 20,479) | |||||
|---|---|---|---|---|---|---|
| B | Exp(B) | p | B | Exp(B) | p | |
| Intercept | −1.311*** | 0.270*** | <0.0001 | −2.086*** | 0.124*** | <0.0001 |
| Socioeconomic status variables: | ||||||
| Household income | ||||||
| Above the poverty threshold | Ref | Ref | Ref | Ref | Ref | Ref |
| Below the poverty threshold | 0.261*** | 1.299*** | <0.0001 | 0.040 | 1.040 | 0.707 |
| Education level | ||||||
| Bachelor's or graduate degree | Ref | Ref | Ref | Ref | Ref | Ref |
| Below Bachelor's degree | 0.682*** | 1.977*** | <0.0001 | 1.004*** | 2.728*** | <0.0001 |
| Employment status | ||||||
| Unemployed | Ref | Ref | Ref | Ref | Ref | Ref |
| Employed | 0.177** | 1.193** | 0.003 | 0.355 | 1.427 | 0.234 |
| Retired | −0.279** | 0.757** | 0.001 | −0.273 | 0.761 | 0.110 |
| Demographics: | ||||||
| Age | −0.015*** | 0.985*** | <0.0001 | −0.008** | 0.992** | 0.007 |
| Race/ethnicity | ||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 0.381*** | 1.464*** | <0.0001 | 0.185 | 1.203 | 0.222 |
| Asian | −1.535*** | 0.215*** | <0.0001 | −1.518*** | 0.219*** | <0.0001 |
| Hispanic | −0.488*** | 0.614*** | <0.0001 | −0.644*** | 0.525*** | <0.0001 |
| Other racial/ethnic groups | 0.023 | 1.023 | 0.897 | 0.548*** | 1.730*** | <0.0001 |
| Household structure: | ||||||
| Household size | 0.017 | 1.017 | 0.414 | 0.054 | 1.055 | 0.088 |
| Living with children | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.418*** | 1.518*** | <0.0001 | 0.132 | 1.141 | 0.301 |
| Marital status | ||||||
| Unmarried | Ref | Ref | Ref | Ref | Ref | Ref |
| Married | 0.034 | 1.035 | 0.414 | 0.100 | 1.105 | 0.349 |
| Building type | ||||||
| House | Ref | Ref | Ref | Ref | Ref | Ref |
| Apartment | −0.070 | 0.932 | 0.445 | −0.353** | 0.703** | 0.009 |
| Mobile home | 0.503*** | 1.653*** | <0.0001 | 0.359* | 1.432* | 0.029 |
| RV/van/boat | 1.066* | 2.905* | 0.010 | 1.397*** | 4.042*** | <0.0001 |
| Health‐related variables: | ||||||
| Had COVID‐19 | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.091 | 1.095 | 0.279 | −0.089 | 0.915 | 0.312 |
| Covered by a health insurance | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.129 | 1.138 | 0.212 | 0.511*** | 1.666*** | <0.0001 |
Note: Results presented in Table 2 were weighted based on the HPS recommended sampling weights. Binomial distributions with a logit link function.
Abbreviation: GEE, generalized estimating equation.
***p < 0.0001,**p < 0.01, *p < 0.05.
With regard to demographics, for both women and men, age was negatively related to their vaccine hesitancy for COVID‐19 (p < 0.0001; p = 0.007). As compared to White women, African American women were 46% more likely to be vaccine‐hesitant (p < 0.0001), while Asian women (78%, p < 0.0001) and men (78%, p < 0.0001) and Hispanic women (39%, p < 0.0001) and men (47%, p < 0.0001) were less likely to be vaccine‐hesitant. Men from other racial/ethnic groups were more likely to be hesitant about COVID‐19 vaccination than White men (73%, p < 0.0001).
For household structure, household size and marital status were not significant predictors of vaccine hesitancy for either women or men (p > 0.05). However, having children in the household made women 52% (p < 0.0001) more likely to be vaccine‐hesitant. Further, the type of building where people were living was also related to vaccine hesitancy. For women, living in a mobile home was associated with 65% more vaccine‐hesitancy (p < 0.0001), while living in an RV, van, or boat was associated with 190% more vaccine‐hesitancy (p = 0.010), as compared to living in a house. Similarly, for men, living in a mobile home (43%, p = 0.029) or an RV/van/boat (304%, p < 0.0001) was associated with higher odds of being vaccine‐hesitant. Interestingly, men living in an apartment were 30% less likely to be vaccine‐hesitant than those living in a house (p = 0.009), but this was not a significant predictor of women's vaccine hesitancy (p = 0.445). For health‐related variables, when not covered by health insurance, men were 67% more likely to be vaccine‐hesitant (p < 0.0001).
Do women and men have different concerns about COVID‐19 vaccines?
Tables 3‐a and 3‐b report the results from the four GEE models predicting four vaccine‐related concerns (Models 3–6). Among the 19,823 vaccine‐hesitant respondents, women were 29% more likely than men to report that they were concerned about possible side effects of a COVID‐19 vaccine (p < 0.0001), while men were more likely than women to report that they did not need a vaccine (41%, p < 0.0001) or they did not trust the government (39%, p < 0.0001). There was no significant difference between women and men in terms of their concerns on the cost of vaccines (p = 0.096). Finally, based on VIF and tolerance, the inferences of all GEE models were not affected by multicollinearity.
TABLE 3a.
Results of the generalized estimating equation models predicting coronavirus disease 2019 (COVID‐19) vaccine‐related concerns
| Model 3 “I am concerned about possible side effects of a COVID‐19 vaccine.” (n = 19,823) | Model 4 “I don't believe I need a COVID‐19 vaccine.” (n = 19,823) | |||||
|---|---|---|---|---|---|---|
| B | Exp(B) | p | B | Exp(B) | p | |
| Intercept | 0.500*** | 1.649*** | <0.0001 | 0.016 | 1.016 | 0.960 |
| Female | 0.251*** | 1.286*** | <0.0001 | −0.531*** | 0.588*** | <0.0001 |
| Socioeconomic status variables: | ||||||
| Household income | ||||||
| Above the poverty threshold | Ref | Ref | Ref | Ref | Ref | Ref |
| Below the poverty threshold | −0.082 | 0.921 | 0.300 | −0.338** | 0.713** | 0.001 |
| Education level | ||||||
| Bachelor's or graduate degree | Ref | Ref | Ref | Ref | Ref | Ref |
| Below Bachelor's degree | −0.186*** | 0.830*** | <0.0001 | −0.041 | 0.960 | 0.509 |
| Employment status | ||||||
| Unemployed | Ref | Ref | Ref | Ref | Ref | Ref |
| Employed | 0.094 | 1.098 | 0.305 | 0.130 | 1.139 | 0.174 |
| Retired | 0.142 | 1.153 | 0.313 | 0.249 | 1.282 | 0.117 |
| Demographics: | ||||||
| Age | −0.011*** | 0.989*** | <0.0001 | −0.028*** | 0.972*** | <0.0001 |
| Race/ethnicity | ||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | 0.073 | 1.075 | 0.538 | −0.898*** | 0.407*** | <0.0001 |
| Asian | 0.316 | 1.372 | 0.098 | −0.511 | 0.600 | 0.161 |
| Hispanic | −0.026 | 0.974 | 0.678 | −0.612** | 0.542** | 0.001 |
| Other racial/ethnic groups | −0.051 | 0.950 | 0.754 | 0.224 | 1.250 | 0.328 |
| Household structure: | ||||||
| Household size | 0.024 | 1.024 | 0.314 | 0.045 | 1.046 | 0.173 |
| Living with children | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | −0.015 | 0.986 | 0.809 | −0.086 | 0.918 | 0.380 |
| Marital status | ||||||
| Unmarried | Ref | Ref | Ref | Ref | Ref | Ref |
| Married | −0.036 | 0.965 | 0.562 | 0.023 | 1.024 | 0.824 |
| Building type | ||||||
| House | Ref | Ref | Ref | Ref | Ref | Ref |
| Apartment | 0.048 | 1.050 | 0.680 | −0.307* | 0.735* | 0.048 |
| Mobile home | 0.303* | 1.354* | 0.043 | −0.253 | 0.777 | 0.162 |
| RV/van/boat | −0.634* | 0.530* | 0.020 | 0.001 | 1.001 | 0.998 |
| Health‐related variables: | ||||||
| Had COVID‐19 | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | −0.272** | 0.762** | 0.002 | −0.006 | 0.994 | 0.953 |
| Covered by a health insurance | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | −0.050 | 0.952 | 0.768 | −0.077 | 0.926 | 0.640 |
Note: Results presented in Table 3a were weighted based on the HPS recommended sampling weights. Binomial distributions with a logit link function.
Abbreviation: GEE, generalized estimating equation.
***p < 0.0001,**p < 0.01, *p < 0.05
TABLE 3b.
Results of the generalized estimating equation models predicting coronavirus disease 2019 (COVID‐19) vaccine‐related concerns
| Model 5 “I don't trust the government.” (n = 19,823) | Model 6 “I am concerned about the cost of a COVID‐19 vaccine.” (n = 19,823) | |||||
|---|---|---|---|---|---|---|
| B | Exp(B) | p | B | Exp(B) | p | |
| Intercept | −1.072*** | 0.342*** | <0.0001 | −1.992*** | 0.136*** | <0.0001 |
| Female | −0.499*** | 0.607*** | <0.0001 | −0.229 | 0.796 | 0.096 |
| Socioeconomic status variables: | ||||||
| Household income | ||||||
| Above the poverty threshold | Ref | Ref | Ref | Ref | Ref | Ref |
| Below the poverty threshold | −0.008 | 0.992 | 0.934 | 0.192 | 1.212 | 0.225 |
| Education level | ||||||
| Bachelor's or graduate degree | Ref | Ref | Ref | Ref | Ref | Ref |
| Below Bachelor's degree | 0.135* | 1.145* | 0.023 | 0.352*** | 1.422*** | <0.0001 |
| Employment status | ||||||
| Unemployed | Ref | Ref | Ref | Ref | Ref | Ref |
| Employed | 0.085 | 1.089 | 0.356 | −0.124 | 0.883 | 0.548 |
| Retired | 0.224 | 1.251 | 0.149 | −0.267 | 0.766 | 0.235 |
| Demographics: | ||||||
| Age | −0.006* | 0.994* | 0.028 | −0.025*** | 0.976*** | <0.0001 |
| Race/ethnicity | ||||||
| White | Ref | Ref | Ref | Ref | Ref | Ref |
| Black | −0.140 | 0.869 | 0.376 | −0.595** | 0.551** | 0.008 |
| Asian | −1.213*** | 0.297*** | <0.0001 | −0.412 | 0.662 | 0.278 |
| Hispanic | −0.473** | 0.623** | 0.009 | 0.194 | 1.214 | 0.455 |
| Other racial/ethnic groups | −0.083 | 0.920 | 0.692 | −0.010 | 0.990 | 0.966 |
| Household structure: | ||||||
| Household size | 0.069* | 1.072* | 0.021 | 0.138* | 1.148* | 0.028 |
| Living with children | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.998 | 0.988 | −0.227 | 0.797 | 0.149 | |
| Marital status | ||||||
| Unmarried | Ref | Ref | Ref | Ref | Ref | Ref |
| Married | −0.093 | 0.911 | 0.279 | −0.373 | 0.689 | 0.093 |
| Building type | ||||||
| House | Ref | Ref | Ref | Ref | Ref | Ref |
| Apartment | −0.120 | 0.887 | 0.067 | 0.313 | 1.368 | 0.092 |
| Mobile home | 0.157 | 1.171 | 0.374 | 0.208 | 1.231 | 0.453 |
| RV/van/boat | 0.402 | 1.495 | 0.358 | −0.529 | 0.589 | 0.341 |
| Health‐related variables: | ||||||
| Had COVID‐19 | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | −0.196* | 0.822* | 0.027 | −0.568** | 0.566** | 0.002 |
| Covered by a health insurance | ||||||
| No | Ref | Ref | Ref | Ref | Ref | Ref |
| Yes | 0.063 | 1.065 | 0.705 | 0.838*** | 2.312*** | <0.0001 |
Note: Results presented in Table 3b were weighted based on the HPS recommended sampling weights. Binomial distributions with a logit link function.
Abbreviation: GEE, generalized estimating equation.
***p < 0.0001,**p < 0.01, *p < 0.05.
DISCUSSION
Vaccine hesitancy represents a serious threat to global health. Recent estimates suggest that a range of 60%–75% of the population must have COVID‐19 immunity in order to reach herd immunity (Anderson et al., 2020; Britton et al., 2020). Encouraging trust in COVID‐19 vaccination is critical to achieving such a goal (Harrison & Wu, 2020). Using the HPS data collected by the Census Bureau in early March 2021, we found that among American adults who had not received COVID‐19 vaccines, two in five were hesitant about getting vaccinated against coronavirus. This study contributes to understanding vaccine hesitancy for COVID‐19 in the US by offering a gender perspective. Our results confirmed a higher vaccine hesitancy rate among women than men, which is consistent with previous studies (Callaghan et al., 2021; Fisher et al., 2020; Latkin, Dayton, Yi, Colon, & Kong, 2021; Lazarus et al., 2021; Malik et al., 2020; Sallam, 2021; Troiano & Nardi, 2021).
By employing the theory of intersectionality, we demonstrate that gender, as an axis of significant, interacts with people's social backgrounds to shape their vaccine hesitancy in a complex way, depending on the dimensions of socioeconomic status. For example, income and employment affected women but not men. Women living in poverty or currently working were more vaccine‐hesitant than women from households above the poverty threshold or unemployed. However, the effect of education appears to extend to both genders, as the lack of a college degree contributes to both women and men's COVID‐19 vaccine hesitancy. Those findings first illuminate the importance of applying an intersectionality approach in the study of vaccine hesitancy. If we did not examine women and men separately in our analyses, like most other studies, we might conclude that people with lower socioeconomic status were, in general, more hesitant to accept COVID‐19 vaccines (e.g., Callaghan et al., 2021; Ferdinand et al., 2020; Khubchandani et al., 2021). The intersectional lens helped us detect that poverty and being employed were only associated with women's vaccine hesitancy, while not having a college education was a risk factor for both women and men.
Previous research suggests that the high level of COVID‐19 vaccine hesitancy in lower‐income communities could be explained by preexisting vaccine hesitancy, lower health literacy, lower trust with healthcare professionals, and cost‐based concerns (Callaghan et al., 2021; Ferdinand et al., 2020; Fisher et al., 2020; Malik et al., 2020; Quinn et al., 2020; Shen et al., 2020; Webb et al., 2019). Our findings appear to indicate that those drivers for vaccine hesitancy associated with low income or poverty might affect women more than men. For employment, Khubchandani et al. (2021) offered an explanation that those who were not working but would like to return to employment might be more motivated to take the COVID‐19 vaccine as it can facilitate return to work. Following this line of thinking, our results might suggest that returning to the workforce motivates women (but not men) to be vaccinated.
On the other hand, working women might also be more hesitant to take COVID‐19 vaccines for fear that vaccine side effects could disrupt their multiple responsibilities from work and family. Indeed, our results show that women were more concerned about the vaccine side effects than men. At the same time, women have been facing an increase in familial care and domestic chores during the pandemic (Craig, 2021; Craig & Churchill, 2021; Dunatchik et al., 2021; Hennekam & Shymko, 2020; Power, 2020; Zamarro & Prados, 2021) and have suffered disproportionate job loss and increased unpaid work hours, in comparison to men (Akter, 2021; Collins et al., 2021; Holder et al., 2021; Landivar et al., 2020). We also found that women who had children were more likely to be vaccine‐hesitant, while the same pattern was not found among men. Previous studies documented American parents' opposition to childhood vaccination before the pandemic (e.g., Siddiqui et al., 2013) and their reluctance to be vaccinated during COVID‐19 (e.g., Dror et al., 2020; Khubchandani et al., 2021). Our results suggest that women's vaccine hesitancy might be related to their childcare responsibilities.
We also examined other sociodemographic factors that contribute to COVID‐19 vaccine hesitancy. For demographics, we found that African American women were more likely to be vaccine‐hesitant than Whites women. Low COVID‐19 vaccine confidence among African American communities has been documented (Callaghan et al., 2021) and shown to be linked to racism, negative healthcare experiences, and historical trauma due to biomedical science abuses (Hamel et al., 2020; Holder et al., 2021; Webb et al., 2019). More research is needed to understand the gender difference in vaccine hesitancy within African Americans. Less vaccine hesitancy research has focussed on Asians and Hispanics. Jones et al. (2020) found that Asian respondents had adequate knowledge concerning the facts of the COVID‐19 pandemic. Another study on human papillomavirus (HPV) vaccination suggests that acculturation, knowledge of HPV, knowledge of the HPV vaccine's efficacy attributed to acceptance of the vaccine among Hispanics (Galbraith et al., 2016). It is possible that acculturation and knowledge of COVID‐19 vaccines were related to the high vaccine acceptance among Asians and Hispanics. Consistent with previous research (Sallam, 2021), we found that younger people were less willing to accept COVID‐19 vaccination than older adults.
People living in mobile homes or RVs had a higher COVID‐19 vaccine hesitancy. It might be that mobile home/RV residents feel safe about their living conditions and are less concerned about being infected by the coronavirus. Interestingly, early exploratory research on the RV lifestyle indicates that as compared to other elderly people, RV residents are relatively young and are often in good health (Null & Bailey, 1994). They might feel they did not need a vaccine. In fact, few studies have investigated the relationship between housing type and people's health behaviour (Hotle et al., 2020), and to the best of our knowledge, no prior studies have linked the type of building where people live to their COVID‐19 vaccine hesitancy. For health‐related factors, we found that having health insurance was related to men but not women's vaccine hesitancy, as uninsured men were more vaccine‐hesitant. Callaghan et al. (2021) also found that in the US, men are more likely to oppose COVID‐19 vaccination due to the lack of health insurance than women. However, only a small proportion of people (5%) in our study were not covered by any health insurance. The effect of health insurance on vaccine hesitancy needs to be examined in future research.
Finally, concerns about COVID‐19 vaccines were also gendered. Possible side effects were the major distress for women, which might be related to the fact that women are in general more likely to practice risk‐avoiding behaviours (Yaqub et al., 2014). However, this finding may also be indicative of gendered power relations within medicine. Indeed, the patriarchal foundations of medicine have been shown to generate women's distrust in medicine or hesitancy towards seeking healthcare (Grodzicka, 2021). Conversely, men were more likely than women to believe that they did not need a COVID‐19 vaccine or they did not trust the government. Based on those results, we conclude that women's COVID‐19 vaccine hesitancy seems to be more related to concerns about the safety of the vaccine, while men's hesitancy tends to be driven by lower perceptions of COVID‐19 dangers, higher levels of self‐rated health, and belief in conspiratorial claims surrounding the disease.
LIMITATIONS
Despite the contributions to the literature, the results of the present study might be affected by several limitations. First, we acknowledge that people's reported vaccine hesitance or acceptance might not translate into actual behaviour, mainly because COVID‐19 is a fast‐moving crisis, and there is a time lag between the measurement of vaccine intention and the observation of behaviour. Second, socioeconomic and cultural characteristics in different states might influence whether people reported vaccine hesitancy. In this study, we used GEE models to control state‐level effects statistically; however, GEEs were limited in detecting the individual effect of each state‐level factor. Future research could investigate variations in vaccine hesitancy across states and utilise a mixed‐effects approach to examine how state‐level factors directly influence people's vaccine hesitancy. Third, the HPS did not collect information on whether participants were pregnant, which has been shown to be a contributor to vaccine hesitancy in women (Goncu Ayhan et al., 2021; Skjefte et al., 2021). Fourth, our analyses were based on data collected in early March 2021, when COVID‐19 vaccines were not available to all age groups. People's attitudes might change as more Americans are vaccinated safely. However, gender dynamics in vaccine hesitancy is itself critical, and necessitates further research, in particular qualitative research. Nevertheless, future researchers should continue examining people's intent to accept COVID‐19 vaccination and pay special attention to how it varies between women and men, and how it changes over time.
CONCLUSIONS
The current study reveals a nuanced picture of social inequality surrounding COVID‐19 vaccine hesitancy from a gender perspective. Our analyses contribute to the scholarship on vaccine hesitancy by uncovering the complex intersection of gender and socioeconomic status. The results also provide insights into future directions for improving COVID‐19 vaccine confidence and uptake. Particularly, gender‐based approaches are needed. Concurrent research has documented the disproportionate burden women have endured during the pandemic. Yet, women also had greater vaccine hesitancy and were more concerned about the vaccine side effects. Thus, tailored outreach strategies that directly address the concerns of women, and women living with children, should be developed to encourage trust in vaccination and empower women to vaccinate themselves and their families. At the same time, more resources should be provided to women living in low‐income households and working women.
Culturally competent strategies should also be developed for African American communities, especially African American women (Quinn et al., 2020; Webb et al., 2019). Given the historic medicinal trauma the black community faced in the US (Washington, 2006), local and federal governments ought to assert an aggressive education campaign that emphasises the necessity for the COVID‐19 vaccine, while reconciling this historical trauma. Vaccine developers need to be more transparent with information regarding vaccine trials and emphasize racial/ethnic inclusivity during testing (Painter et al., 2021). In addition, scientific organisations and public health experts should target vaccine efficacy education campaigns to address hesitancy among young adults, especially those who do not have a college education. Finally, as this study demonstrates, we must begin taking an intersectional approach to research and policymaking in order to address systemic issues that have led to institutional mistrust, which puts women and minorities who have been disproportionally affected by the pandemic at greater risk even when a solution is available.
AUTHOR CONTRIBUTION
Danielle Xiaodan Morales: Conceptualizszation; Lead, Formal analysis; Lead, Methodology; Lead, Writing – original draft; Lead, Writing – review & editing; Lead. Tyler Beltran: Formal analysis; Supporting, Methodology; Supporting, Writing – review & editing; Supporting. Stephanie Morales: Formal analysis; Supporting, Methodology; Supporting, Writing – review & editing; Supporting.
Morales, D. X. , Beltran, T. F. , & Morales, S. A. (2022). Gender, socioeconomic status, and COVID‐19 vaccine hesitancy in the US: An intersectionality approach. Sociology of Health & Illness, 44(6), 953–971. 10.1111/1467-9566.13474
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available at https://www.census.gov/programs‐surveys/household‐pulse‐survey/datasets.html.
REFERENCES
- Akter, S. (2021). The gender gap in COVID‐19 mortality in the United States. Feminist Economics, 27(1–2), 30–47. 10.1080/13545701.2020.1829673 [DOI] [Google Scholar]
- Anderson, R. M. , Vegvari, C. , Truscott, J. , & Collyer, B. S. (2020). Challenges in creating herd immunity to SARS‐CoV‐2 infection by mass vaccination. The Lancet, 396(10263), 1614–1616. 10.1016/S0140-6736(20)32318-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton, T. , Ball, F. , & Trapman, P. (2020). A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS‐CoV‐2. Science, 369(6505), 846–849. 10.1126/science.abc6810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brumfiel, G. (2021). Vaccine refusal may put herd immunity at risk, researchers warn. https://www.npr.org/sections/health‐shots/2021/04/07/984697573/vaccine‐refusal‐may‐put‐herd‐immunity‐at‐risk‐researchers‐warn [Google Scholar]
- Callaghan, T. , Moghtaderi, A. , Lueck, J. A. , Hotez, P. , Strych, U. , Dor, A. , Fowler, E. F. , & Motta, M. (2021). Correlates and disparities of intention to vaccinate against COVID‐19. Social Science & Medicine, 272, 113638 10.1016/j.socscimed.2020.113638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . (2021). Data tracker. Accessed 2 June 2021. https://covid.cdc.gov/covid‐data‐tracker/#vaccinations [Google Scholar]
- Collins, C. , Landivar, L. C. , Ruppanner, L. , & Scarborough, W. J. (2021). COVID‐19 and the gender gap in work hours. Gender, Work and Organization, 28(S1), 101–112. 10.1111/gwao.12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, P. H. (1990). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Routledge. [Google Scholar]
- Craig, L. (2021). Coronavirus, domestic labour and care: Gendered roles locked down. Journal of Sociology, 56(4), 684–692. 10.1177/1440783320942413 [DOI] [Google Scholar]
- Craig, L. , & Churchill, B. (2021). Dual‐earner parent couples’ work and care during COVID. Gender, Work and Organization, 28(S1), 66–79. 10.1111/gwao.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw, K. W. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics. University of Chicago Legal Forum, 1989(1), 138–167. http://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8 [Google Scholar]
- Crenshaw, K. W. (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 43, 1241–1299. 10.2307/1229039 [DOI] [Google Scholar]
- Diamond, J. (2021). Biden administration launches $10 million ad campaign, leaders' network to encourage vaccination. Accessed 10 April 2021. https://www.cnn.com/2021/04/01/politics/vaccine‐confidence‐advertising‐biden‐administration/index.html [Google Scholar]
- Diggle, P. J. , Heagerty, P. , Liang, K. , & Zegger, S. L. (2002). Analysis of longitudinal data. Oxford University Press. [Google Scholar]
- Dror, A. A. , Eisenbach, N. , Taiber, S. , Morozov, N. G. , Mizrachi, M. , Zigron, A. , Srouji, S. , & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID‐19. European Journal of Epidemiology, 35(8), 775–779. 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunatchik, A. , Gerson, K. , Glass, J. , Jacobs, J. A. , & Haley, S. (2021). Gender, parenting, and the rise of remote work during the pandemic: Implications for domestic inequality in the United States. Gender & Society, 35(2), 194–205. 10.1177/08912432211001301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand, K. C. , Nedunchezhian, S. , & Reddy, T. K. (2020). The COVID‐19 and influenza “Twindemic”: Barriers to influenza vaccination and potential acceptance of SARS‐CoV2 Vaccination in African‐Americans. Journal of the National Medical Association, 112(6), 681–687. 10.1016/j.jnma.2020.11.001 [DOI] [PubMed] [Google Scholar]
- Fields, J. F. , Hunter‐Childs, J. , Tersine, A. , Sisson, J. , Parker, E. , Velkoff, V. , Logan, C. , & Shin, H. (2020). Design and operation of the 2020 household Pulse survey, 2020. U.S. Census Bureau. [Google Scholar]
- Fisher, K. A. , Bloomstone, S. J. , Walder, J. , Crawford, S. , Fouayzi, H. , & Mazor, K. M. (2020). Attitudes toward a potential SARSCoV‐2 vaccine: A survey of US adults. Annals of Internal Medicine, 173(12), 964–973. 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk, C. , & Tyson, A. (2020). Intent to get a COVID‐19 vaccine rises to 60% as confidence in research and development process increases. Pew Research Center. accessed 10 December 2020. https://heatinformatics.com/sites/default/files/images‐videosFileContent/PS_2020.12.03_covid19‐vaccine‐intent_REPORT.pdf [Google Scholar]
- Galbraith, K. V. , Lechuga, J. , Jenerette, C. M. , Moore, A. D. , Palmer, M. H. , & Hamilton, J. B. (2016). Parental acceptance and uptake of the HPV vaccine among african‐Americans and latinos in the United States: A literature review. Social Science & Medicine, 159, 116–126. 10.1016/j.socscimed.2016.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garson, G. D. (2012). Generalized linear models and generalized estimating equations. Statistical Associates Publishing. [Google Scholar]
- Goncu Ayhan, S. , Oluklu, D. , Atalay, A. , Menekse Beser, D. , Tanacan, A. , Moraloglu Tekin, O. , & Sahin, D. (2021). COVID‐19 vaccine acceptance in pregnant women. International Journal of Gynecology & Obstetrics, 154(2), 291–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grodzicka, E. D. (2021). Taking vaccine regret and hesitancy seriously. The role of truth, conspiracy theories, gender relations and trust in the HPV immunisation programmes in Ireland. Journal for Cultural Research, 25(1), 69–87. [Google Scholar]
- Hamel, L. , Kirzinger, A. , Lopes, L. , Kearney, A. , Sparks, G. , & Brodie, M. (2021). KFF COVID‐19 vaccine monitor: January 2021. Kaiser Family Foundation. Accessed 30 January 2021. https://www.kff.org/coronavirus‐covid‐19/report/kff‐covid‐19‐vaccine‐monitor‐january‐2021/ [Google Scholar]
- Hamel, L. , Lopes, L. , Munana, C. , Artiga, S. , & Brodie, M. (2020). Race, health, and COVID‐19: The views and experiences of black Americans. Kaiser Family Foundation. Accessed 30 January 2021. https://files.kff.org/attachment/Report‐Race‐Health‐and‐COVID‐19‐The‐Views‐and‐Experiences‐of‐Black‐Americans.pdf [Google Scholar]
- Harrison, E. A. , & Wu, J. W. (2020). Vaccine confidence in the time of COVID‐19. European Journal of Epidemiology, 35(4), 325–330. 10.1007/s10654-020-00634-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennekam, S. , & Shymko, Y. (2020). Coping with the COVID‐19 crisis: Force majeure and gender performativity. Gender, Work and Organization, 27(5), 788–803. 10.1111/gwao.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder, M. , Jones, J. , & Masterson, T. (2021). The early impact of Covid‐19 on job losses among black women in the United States. Fem. Economic Times, 27(1–2), 103–116. 10.1080/13545701.2020.1849766 [DOI] [Google Scholar]
- Hotle, S. , Murray‐Tuite, P. , & Singh, K. (2020). Influenza risk perception and travel‐related health protection behavior in the US: Insights for the aftermath of the COVID‐19 outbreak. Transportation Research Interdisciplinary Perspectives, 5, 100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, J. , Sullivan, P. S. , Sanchez, T. H. , Guest, J. L. , Hall, E. W. , Luisi, N. , Zlotorzynska, M. , Wilde, G. , Bradley, H. , Siegler, A. J. 2020. Similarities and differences in COVID‐19 awareness, concern, and symptoms by race and ethnicity in the United States: Cross‐sectional survey. Journal of Medical Internet Research. 22(7), e20001. 10.2196/20001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani, J. , Sharma, S. , Price, J. H. , Wiblishauser, M. J. , Sharma, M. , & Webb, F. J. (2021). COVID‐19 vaccination hesitancy in the United States: A rapid national assessment. Journal of Community Health, 46(2), 270–277. 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosnick, K. (2011). Sexuality and migration studies: The invisible, the Oxymoronic and Heteronormative othering. In Lutz H., Vivar M. H., & Supik L. (Eds.), Framing intersectionality (pp. 121–136). Ashgate. [Google Scholar]
- Landivar, L. C. , Ruppanner, L. , Scarborough, W. J. , & Collins, C. (2020). Early Signs Indicate that COVID‐19 is exacerbating gender inequality in the labor force. Socius: Sociological Research for a Dynamic World, 6, 237802312094799. 10.1177/2378023120947997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin, C. , Dayton, L. A. , Yi, G. , Konstantopoulos, A. , Park, J. , Maulsby, C. , & Kong, X. (2021). COVID‐19 vaccine intentions in the United States, a social‐ecological framework. Vaccine, 39(16), 2288–2294. 10.1016/j.vaccine.2021.02.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin, C. A. , Dayton, L. , Yi, G. , Colon, B. , Kong, X. 2021. Mask usage, social distancing, racial, and gender correlates of COVID‐19 vaccine intentions among adults in the US. PLoS One. 16(2), e0246970. 10.1371/journal.pone.0246970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, J. V. , Ratzan, S. C. , Palayew, A. , Gostin, L. O. , Larson, H. J. , Rabin, K. , Kimball, S. , & El‐Mohandes, A. (2021). A global survey of potential acceptance of a COVID‐19 vaccine. Natura Med, 27, 225–228. 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, K. Y. , & Zeger, S. L. (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. [Google Scholar]
- MacDonald, N. E. & SAGE Working Group on Vaccine Hesitancy. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. 10.1016/j.vaccine.2015.04.036 [DOI] [PubMed] [Google Scholar]
- Malik, A. A. , McFadden, S. M. , Elharake, J. , & Omer, S. B. (2020). Determinants of COVID‐19 vaccine acceptance in the US. EClinicalMedicine, 26, 100495. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata, J. M. , Hernández‐Ramos, I. , Kurup, A. S. , Albrecht, D. , Vivas‐Torrealba, C. , & Franco‐Paredes, C. (2013). Social determinants of health and seasonal influenza vaccination in adults ≥65 years: A systematic review of qualitative and quantitative data. BMC Public Health, 13, 388. 10.1186/1471-2458-13-388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Null, R. , & Bailey, A. (1994). The RV lifestyle: An exploratory research approach. Housing and Society, 21(3), 10–16. [Google Scholar]
- Painter, E. M. , Ussery, E. N. , Patel, A. , Hughes, M. M. , Zell, E. R. , Moulia, D. L. , Scharf, L. G. , Lynch, M. , Ritchey, M. D. , Toblin, R. L. , Murthy, B. P. , Harris, L. Q. , Wasley, A. , Rose, D. A. , Cohn, A. , & Messonnier, N. E. (2021). Demographic characteristics of persons vaccinated during the first month of the COVID‐19 vaccination program—United States, december 14, 2020‐January 14, 2021. Morbidity and Mortality Weekly Report, 70(5), 174–177. 10.15585/mmwr.mm7005e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power, K. (2020). The COVID‐19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy, 16(1), 67–73. 10.1080/15487733.2020.1776561 [DOI] [Google Scholar]
- Quinn, S. C. , Jamison, A. M. , & Freimuth, V. (2020). Communicating effectively about emergency use authorization and vaccines in the COVID‐19 pandemic. Americal Journal of Public Health. 10.2105/AJPH.2020.306036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam, M. (2021). COVID‐19 vaccine hesitancy Worldwide: A concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 160. 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen, A. K. , Hughes, R., IV , DeWald, E. , Rosenbaum, S. , Pisani, A. , & Orenstein, W. (2020). Ensuring equitable access to COVID‐19 vaccines in the US: Current system challenges and opportunities. Health Affairs. 10.1377/hlthaff.2020.01554 [DOI] [PubMed] [Google Scholar]
- Siddiqui, M. , Salmon, D. A. , & Omer, S. B. (2013). Epidemiology of vaccine hesitancy in the United States. Human Vaccines & Immunotherapeutics, 9(12), 2643–2648. 10.4161/hv.27243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skjefte, M. , Ngirbabul, M. , Akeju, O. , Escudero, D. , Hernandez‐Diaz, S. , Wyszynski, D. F. , & Wu, J. W. (2021). COVID‐19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. European Journal of Epidemiology, 36(2), 197–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano, G. , & Nardi, A. (2021). Vaccine hesitancy in the era of COVID‐19. Public Health, 194, 245–251. Advance online publication. 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington, H. A. (2006). Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. Doubleday Books. [Google Scholar]
- Webb, F. J. , Khubchandani, J. , Striley, C. W. , & Cottler, L. B. (2019). Black‐white differences in willingness to participate and perceptions about health research: Results from the population‐based HealthStreet study. Journal of Immigrant and Minority Health, 21(2), 299–305. 10.1007/s10903-018-0729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper, M. , Mitchell, C. , Marshall, V. J. , Cheatham, C. , Austin, K. , Sanders, K. , Krishnamurthi, S. , & Grafton, L. L. (2019). Understanding multilevel factors related to Urban community trust in healthcare and research. International Journal of Environmental Research and Public Health, 16(18), 3280. 10.3390/ijerph16183280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2014). Report of the SAGE working group on vaccine hesitancy. Accessed 21 December 2020. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf [Google Scholar]
- Yaqub, O. , Castle‐Clarke, S. , Sevdalis, N. , & Chataway, J. (2014). Attitudes to vaccination: A critical review. Social Science & Medicine. 112, 1–11. 10.1016/j.socscimed.2014.04.018 [DOI] [PubMed] [Google Scholar]
- Yeung, M. P. , Lam, F. L. , & Coker, R. (2016). Factors associated with the uptake of seasonal influenza vaccination in adults: A systematic review. Journal of Public Health, 38(4), 746–753. 10.1093/pubmed/fdv194 [DOI] [PubMed] [Google Scholar]
- Zamarro, G. , & Prados, M. J. (2021). Gender differences in couples’ division of childcare, work, and mental health during COVID‐19. Review of Economics of the Household, 19(1), 11–40. 10.1007/s11150-020-09534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkov, D. (2011). Exposures and invisibilities: Media, masculinities, and the Narratives of framing intersectionality. In Lutz H., Vivar M. H., & Supik L. (Eds.), Framing intersectionality (pp. 105–120). Ashgate. [Google Scholar]
- Zeger, S. L. , & Liang, K. Y. (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42(1), 121–130. [PubMed] [Google Scholar]
- Zorn, C. J. (2001). Generalized estimating equation models for correlated data: A review with applications. American Journal of Polymer Science, 45(2), 470–490. 10.2307/2669353 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available at https://www.census.gov/programs‐surveys/household‐pulse‐survey/datasets.html.


