Abstract
Background
During the Coronavirus disease 2019 (COVID‐19) pandemic, hospital visits were suspended and video calls were offered to connect patients with their family members, especially toward the end of life (EoL).
Aim
The primary aim was to describe EoL care for COVID‐19 patients dying in an intensive care unit (ICU). The secondary aim was to explore whether making video calls and allowing visits was associated with lower death‐related stress in family members.
Design
Single centre cross‐sectional study. The setting was the ICU of a COVID‐19 center in northern Italy, during the first year of the pandemic. Data on patients who died in the ICU were collected; death‐related stress on their family members was measured using the Impact of Event Scale‐Revised (IES‐R). The statistical association was tested by means of logistic regression.
Results
The study sample included 70 patients and 56 family members. All patients died with mechanical ventilation, hydration, nutrition, analgesia and sedation ongoing. Resuscitation procedures were performed in 5/70 patients (7.1%). Only 6/56 (10.7%) of the family members interviewed had visited their loved ones in the ICU and 28/56 (50%) had made a video call. EoL video calls were judged useful by 53/56 family members (94.6%) but all (56/56, 100%) wished they could have visited the patient. High‐stress levels were found in 38/56 family members (67.9%), regardless of whether they were allowed ICU access or made a video call. Compared with other degrees of kinship, patients' offspring were less likely to show a positive IES‐R score (odds ratio [OR] 0.22, 95% confidence interval [CI] 0.05 to 0.89).
Conclusions
During the first year of the COVID‐19 pandemic, patients died without their family members at the bedside while on life‐sustaining treatment. Stress levels were high in most family members, especially in patients' spouses. Video calls or ICU visits were judged favourably by family members but insufficient to alleviate death‐related stress.
Relevance for Clinical Practice
During a pandemic, ICU access by patients' family members should be considered, particularly as the time of death approaches. Although generally appreciated by family members, EoL video calls should be arranged together with other measures to alleviate death‐related stress, especially for the patient's spouse.
Keywords: COVID‐19, critical care, end‐of‐life care, stress, visitors to patients
What is known about this topic
COVID‐19 was associated with high mortality rates, particularly for critically ill patients early in the pandemic.
ICU hospitalization is a stressful event for family members.
During the COVID‐19 pandemic, video calls were the only means to connect patients with their family members, especially toward the EoL.
What this paper adds
During the first year of the pandemic, most patients with COVID‐19 hospitalized in the ICU died without a family member present.
Death‐related stress levels were high, especially for patients' spouses.
Most family members appreciated the offer of making EoL video calls; however, all interviewees stated that, despite visitation restrictions and fear of infection, they wished they could have been present when the patient died.
1. BACKGROUND
Since its outbreak at the end of 2019, the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS CoV‐2) pandemic has taken a huge toll (410 565 868 people infected and 5 810 880 deaths globally, as of February 15, 2022). 1 Coronavirus disease (COVID‐19) spread from China to Italy, where Lombardy was the hardest hit region 2 : 5.7% of laboratory‐confirmed COVID‐19 cases required intensive care unit (ICU) admission, mainly hospitalization for respiratory support, resulting in high ICU mortality rates. 3
All of a sudden, the long process of opening hospitals to families 4 , 5 was severely restricted and patients remained without the presence of family members during their hospital stay. In this unprecedented scenario, patients died without having their family members at the bedside. The situation was as unbearable for families 6 as it was for health care professionals (HCPs). 7 , 8
ICU stay affects not only the long‐term outcomes of patients but also the mental health, stress, and quality of life of their family members. ICU hospitalization may progress to a full‐blown post‐traumatic stress disorder (PTSD), particularly in family members who receive inadequate or insufficient information 9 or after severe trauma (e.g., death). 10 Such risk factors increase the risk of unsolved mourning, with higher levels of psychological distress and a higher risk of developing PTSD. Before the COVID‐19 outbreak, 48% of family members were reported to experience psychological problems within 90 days after ICU discharge of a family member: depression (13%), anxiety (29%), and PTSD (39%). 11 These worrying data suggest that psychological distress due to the COVID‐19 pandemic is likely to increase.
During the COVID‐19 pandemic, restrictions on ICU visitation placed enormous emotional stress on patients' family members. ICU management attempted to remediate by using technology (i.e., video calls by telephone or tablet). In this way, HCPs could keep patients in touch with their families, 12 , 13 even toward the end of life. 14 , 15 When personal protective equipment (PPE) became available, restrictions were partially relaxed to allow family members to see patients. 16
2. AIMS
The primary aim of this study was to describe the type of end‐of‐life (EoL) care for patients hospitalized for SARS‐CoV‐2 infection and dying in an ICU in a COVID‐19 hub center during the pandemic. Our hypothesis was that the provision of making a video call or ICU visitation might mitigate emotional response to the loss of a family member. We expected that distress caused by grief would be reduced in family members who had the chance to be virtually present at the time of death. The secondary aim was to identify the factors associated with stress as measured with the Impact of Events Scale‐Revised (IES‐R). 17
3. DESIGN AND METHODS
3.1. Design and setting
This cross‐sectional study was performed at the Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico Milano during the COVID‐19 pandemic. Our hospital was designated a COVID‐19 hub center for Lombardy. Our ICU department is composed of six ICUs located in different hospital wings.
To meet the first aim, the study sample included adult patients who died of COVID‐19‐related causes while in the ICU between February 25, 2020 and February 25, 2021. For the second aim, we interviewed patients' family members who willingly participated in the study. Contacts were retrieved from the electronic medical records of our Institution. A family member was defined as the reference person for clinical communication during the patient's ICU stay, even if not directly related to the patient.
The study was approved by the Ethics Committee Milano Area 2 (May 28, 2021; no. 593/2021). Oral and written informed consent was obtained from family members, including permission to publish their statements.
3.2. Communication with family members and visiting policies
Information on the patient's clinical course was provided daily, usually late in the morning, by telephone and by the same consultant in charge, in a quiet room. The consultant would call the family more often as the clinical condition worsened and death was imminent. Following a standardized procedure, 18 the video calls were managed by the physician and/or nurse in charge and took place at the patient's bedside. Before a call was made, the patient and the surrounding area were prepared and the ICU staff was notified of an EoL situation. 15
Hospital visits were arranged in advance by telephone by the consultant and usually preceded by a video call. The physician and/or the nurse in charge informed the family member about infection risk before he/she entered the ICU, helped him/her don and doff PPEs, and were available if needed for the entire duration of the visit. 19 The first video call was made in March 2020; visitors could access the ICU starting in late December 2020.
3.3. Data collection
Patient data were gleaned from clinical electronic records and comprised demographics, clinical characteristics, and treatment delivered. Family members were contacted by telephone in June 2021. The same researcher performed structured interviews according to a case report form that included the family members' demographics. During the interview, the family members were asked if they were allowed to enter the ICU or if they would have liked to do so, if they made a video call or would have liked to, and if they would have made different choices. The family member then completed the IES‐R.
The Italian version of the IES‐R 17 was used to measure the stress level the family member experienced. The IES‐R comprises 22 items in three areas (8 intrusion items, 8 avoidance items, 6 hyperarousal items). 20 The instrument has an adequate internal consistency (Cronbach's α) for each subscale (intrusion, α = 0.78; avoidance, α = 0.72; hyperarousal, α = 0.83). 17 Intrusion is defined as the inability to keep memories of the event from returning. Avoidance is an attempt to avoid stimuli and triggers that may bring back those memories. Hyperarousal is similar to hypervigilance and is a state of increased alertness, which includes insomnia, a tendency to be easily startled, a constant feeling that danger or disaster is nearby, an inability to concentrate and extreme irritability or even violent behaviour. Each item evaluates symptom severity on a 5‐point scale (0 to 4) for the previous 1‐week period. The IES‐R score ranges from 0 to 88, a score ≥ 33 means a probable diagnosis of PTSD, 21 while a score ≥22 but <33 is a subclinical cut‐off for PTSD. 22
3.4. Data analysis
Metrics are reported as mean and standard deviation (SD), median and interquartile range (IQR) or counts and percentage (%). Patient characteristics at the EoL are presented in descriptive tables. To explore the association between IES‐R (positive vs. negative) score and degree of kinship, mortality rate by month, and patient and family member age, we applied a multivariate approach using multiple correspondence analysis (MCA). 23 MCA takes multiple categorical variables and seeks to identify associations between them. Like other multivariate methods, MCA is also a dimension reducing technique, so it represents data as points in a 2‐dimensional space, and the results can be visualized on a biplot. As categories become more similar, they group closer together. Finally, we fitted a logistic model to explore the statistical association between the probability of a positive IES‐R score and selected variables, accounting for the presence of video call/ICU visitation. Results are commented as odds ratio (OR) and 95% confidence intervals (CI). All analyses were performed using R Core Team (version 4.0.3) with the FactoMineR and factoextra packages added for MCA. A p‐value <0.05 was considered statistically significant.
4. RESULTS
During the study period, 297 patients were admitted to the ICUs and 70 (23.6%) died; 18/70 (25.7%) were aged <60 years. The demographic and clinical characteristics of the deceased patients are presented in Table 1.
TABLE 1.
Characteristics of patients who died in the ICU (n = 70)
| Characteristic | No. (%) or mean (SD) |
|---|---|
| Age (years) | 64.7 (10.9) |
| Sex | |
| Male | 56 (80%) |
| Female | 14 (20%) |
| Ethnicity | |
| Caucasian | 63 (90%) |
| Hispanic | 5 (7.1%) |
| Asian | 2 (2.9%) |
| Occupation | |
| Retired | 44 (62.9%) |
| Worker | 26 (37.1%) |
| BMI | 28.8 (4.9) |
| At least one comorbidity | 62 (88.6%) |
| SOFA | 5.7 (2.7) |
| Pressure sores at ICU admission | 12 (17.1%) |
| ICU length of stay (days) | 21.1 (20.7) |
| Ventilation (days) | 21.5 (21) |
| Tracheotomy | 9 (12.9%) |
| Prone position | 57 (81.4%) |
Abbreviations: BMI, body‐mass index (weight in kg divided by height in meters squared); ICU, intensive care unit; SD, standard deviation; SOFA, sequential organ failure assessment.
Most patients were hospitalized during the first COVID‐19 wave (March 18, 2020/70, 25.7%), then April 2020 (14/70, 20%) and October 2020 (second wave, 13/70, 18.6%). The mortality rate peaked in April (15/70, 21.4%), March (14/70, 20%), and November (12/70, 17.1%). Cardiopulmonary resuscitation (CPR) was performed in 5/70 patients (7.1%), 4/46 (8.7%) of which during the first and 1/24 (4.2%) during the second wave. Two out of 70 patients (2.9%) were conscious at the time of ICU admission and none (0/70, 0%) had advance healthcare directives. All patients who died had a medical device for nutrition, hydration, gastric protection, and thrombosis prevention in place. Only 1/70 patient (1.4%) died without an artificial airway and with non‐invasive ventilation ongoing (Table 2).
TABLE 2.
Treatment and medical devices at the end of life (n = 70)
| Treatment | No. (%) |
|---|---|
| Analgesia | 70 (100) |
| Sedation | 70 (100) |
| NMBA | 55 (78.6) |
| Enteral nutrition | 69 (98.6) |
| Prone positioning | 13 (18.6) |
| CRRT | 11 (15.7) |
| ECMO | 5 (7.1) |
| Medical device | |
| Artificial airway | 69 (98.6) |
| Arterial catheter | 70 (100) |
| Central venous catheter | 70 (100) |
| CRRT venous catheter | 15 (21.4) |
| Peripherical venous catheter | 13 (18.6) |
| Swan‐Ganz catheter | 10 (14.3) |
| Urinary catheter | 70 (100) |
| Nasogastric tube | 69 (98.6) |
| Intrarectal faecal collection system | 8 (11.4) |
Abbreviations: CRRT, continuous renal replacement therapy; ECMO, extra corporeal membrane oxygenation; NMBA, neuromuscular blocking agents.
During the last 6 h of life, 5/70 (7.1%) patients underwent a diagnostic (e.g., echography, brain computed tomography, bronchoscopy) or a therapeutic procedure (e.g., blood transfusion) and all received hygienic care (i.e., eye and oral cavity care). The last blood tests and arterial blood gases were performed at 7 (IQR 6; 12) and 5 (IQR 2; 6) hours before death, respectively.
A family member was contacted on the death of the patient (70/70, 100%) by the same consultant who handled the daily communication with families (63/70, 90%). In addition to the daily phone call, a call notifying the family of the worsening of the patient's clinical condition was made in 61/70 (87.1%) cases.
No follow‐up contact could be made with 13/70 (18.6%) family members; 57/70 (81.4%) answered our request and 56/70 (80%) agreed to be interviewed. The family member was most often a son or daughter (25/56, 44.6%) or a spouse (22/56, 39.3%). Characteristics of the family members and their IES‐R scores are presented in Table 3.
TABLE 3.
Characteristics of family members (n = 56)
| Characteristic | No. (%) or mean (SD) |
|---|---|
| Age (years) | 52.8 (14.4) |
| Sex | |
| Female | 48 (85.7%) |
| Male | 8 (14.3%) |
| Relationship with the patient | |
| Offspring | 25 (44.6%) |
| Spouse | 22 (39.3%) |
| Sibling | 5 (8.9%) |
| Friend | 3 (5.4%) |
| Uncle | 1 (1.8%) |
| Video call made | 28 (50%) |
| ICU visit made | 6 (10.7%) |
| IES‐R | |
| Total score | 39.3 (14.7) |
| Avoidance subscore | 11.2 (5.6) |
| Intrusion subscore | 20.6 (6.3) |
| Hyperarousal subscore | 7.5 (5.8) |
| Total score <22 | 7 (12.5%) |
| Total score ≥22 and <33 | 11 (19.6%) |
| Total score ≥33 | 38 (69.7%) |
Abbreviations: ICU, intensive care unit; IES‐R, Impact of Event Scale‐Revised; SD, standard deviation.
All family members (56/56, 100%) stated they wished they had been able to visit the patient; only 6/56 (10.7%) made an ICU visit. Half of the family members (28/56, 50%) made a video call, 17/28 (60.7%) of which when notified that EoL was imminent. Nearly all of those who made a video call would have done it again (27/28 (96.4%), whereas nearly all of those who did not make a call (26/28, 92.9%) wished they had. Most of the video calls were made with the immediate family (spouse and son/daughter). One EoL video call was arranged as a prayer vigil with relatives and friends from Italy and from abroad. An IES‐R score ≥33 was noted for 13/25 (52%) offspring and for 20/22 (90.9%) spouses, respectively.
A religious service was contacted when requested, initially remotely and then present in the ICU. As funeral services were not allowed by law, 25/56 (44.6%) family members could not bury their dead. Hospital or private psychological support was requested by 37.5% (21/56) of family members.
The relationship between IES‐R score and degree of kinship, the death rate by month, and patient and family member age is presented in Figure 1. Family members with a positive IES‐R score are located mostly on the right side of the plot. Spouses, siblings, friends, and uncles are located on the left side of the plot and had a negative IES‐R score. Deaths during the pandemic were associated with a positive IES‐R score for family members aged 55–74 years, except for offspring. Negative IES‐R scores were mostly associated with deaths that occurred outside the wave peaks and with patients older than 65 years.
FIGURE 1.
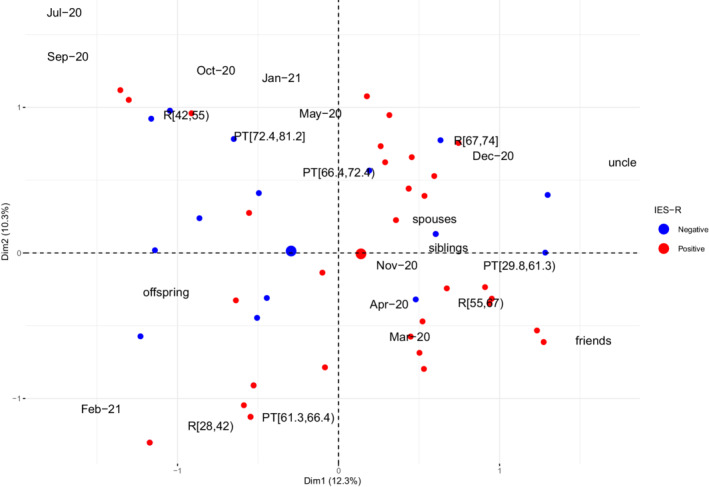
Biplot of individuals and variables in two multiple correspondence analysis (MCA) dimensions. Blue dots denote individuals interviewed with a negative IES‐R score, whereas red dots denote individuals with a positive IES‐R score. MCA refers to the time of death (month‐year: Mar‐20, Apr‐20, May‐20, Jun‐20, Jul‐20, Sep‐20, Oct‐20, Nov‐20, Dec‐20, Jan‐21, Feb‐21), degree of kinship with the patient (friends, spouses, offspring, siblings, uncle), and patient (PT) or interviewed relative's (R) age. Age is reported as quartiles. Age for PT: PT[29.8,61.3), PT[61.3,66.4), PT[66.4,72.4), PT[72.4,81.2]; age for interviewed relatives: R[28,42), R[42,55), R[55,67), R[67,74].“(“or”)” and “[“or”]” denote open and closed intervals. The Dim1 axis (i.e., “degree of kinship”) is the first dimension along which the sample shows the largest variation, whereas the Dim2 axis (i.e., “age”) is the second‐largest dimension and it is orthogonal to Dim1, which explains 12.3% of the variation in the data
The month of death and the degree of kinship were statistically associated with the probability of having a positive IES‐R score among the family members interviewed. Death during the second wave reduced the probability of having an IES‐R score ≥ 33 (OR 0.18, 95% CI 0.04 to 0.8). Compared with other degrees of kinship, offspring were less likely to have a positive IES‐R score (OR 0.22, 95% CI 0.05 to 0.89). The fitted model showed no statistical association between IES‐R score and patient age (OR 0.99, 95% CI 0.42 to 2.33) and making an ICU visit or a video call (OR 0.93, 95% CI 0.24 to 3.65).
5. DISCUSSION
This study initially described EoL care for patients with severe COVID‐19 who died in the ICU during the first year of the pandemic. The patients were seriously ill and received invasive treatment (e.g., renal support and ECMO) despite the limited availability of hospital equipment and human resources, especially during the first pandemic wave. 24 Many of these patients died without having family members present at the bedside, except by video call. 15 Analysis of IES‐R scores revealed high stress in family members, especially in the patient's spouse.
Patients hospitalized in the ICU often require invasive mechanical ventilation in prone positions due to their extremely poor oxygenation status. In the present cohort, prolonged mechanical ventilation for 3 weeks or longer and the high number of medical devices on site at the patient's end of life reflected the severity of the disease. All intubated patients died while receiving anaesthetic and analgesic drugs, which indicates that terminal extubation was not contemplated, not even in extreme situations. When we compared the difference in the number of treatments between pandemic waves, the only clinically relevant difference was the number of CPR procedures performed during the first wave (8.7% vs. 4.2%), suggesting more unexpected deaths. Overall, the EoL treatment burden underscores the difficulty to switch from cure to comfort. 25
During the COVID‐19 pandemic, communication between patients and family was possible only by telephone, video calls, text messages or emails. This remote management contrasts with the policy of an open ICU, which fosters direct contact and the physical presence of family members. 26 The patients' critical condition, the uncertain outcome, and the concern over infection aroused fear and anxiety, accompanied by mental fatigue and frustration. 27 Open ICU visiting policies can reduce the incidence of anxiety, stress, and PTSD. 9 , 28 Involvement of family members in the ICU plays a crucial role in the psychological well‐being of patients and their families alike. 29 Furthermore, open ICU policies also promote better interaction and collaboration between families and HCPs, 30 especially with nurses, who have a key part in the continuum of care between patients and families. This challenging aspect of clinical practice was further complicated by the extraordinary circumstances of the pandemic. 31
Family members of ICU patients face many difficulties; we provided an alternative means of communication and measured death‐related stress with the IES‐R in 56 family members. The IES‐R is the most widely used scale for evaluating traumatic stress symptoms 17 ; it has also been used to measure bereavement stress in COVID‐19 ICUs. 32 In our scenario, the death of a family member may trigger traumatic, and complicated, grief. It is estimated that 10% to 15% of individuals who experience the death of a hospitalized family member are more likely to enter complicated grief rather than elaborate on the loss. 33
Our study shows that spouses had a higher chance of a positive IES‐R score compared with offspring. This finding is shared by previous studies: being in a spousal relationship with a care recipient is a risk factor for developing psychological distress in grief. 34 A plausible explanation is that in the natural course of psychological events in a family it is far more usual, and psychologically tolerated, to experience a parent's rather than a spouse's death.
Furthermore, despite the psychological complexities of ICU management during the COVID‐19 pandemic, our hospital established a procedure that allowed contact between families and end‐stage patients. The IES‐R score was higher and the psychological distress was more severe for family members notified by telephone of their relative's death. This finding is consistent with previous studies; it appears to be a protective factor, especially in the ICU, to communicate as clearly as possible with family members. 35 However, we found no statistically significant association between stress level and the provision of video calls, which suggests that modern communication technologies cannot replace physical contact.
New solutions should be experimented with to facilitate ICU visits by family members. One example is a hug room, which has been adopted by long‐term care facilities, 36 where family members can not only see but also touch their loved ones through transparent plastic barriers. In EoL situations, this option may allow for bidding farewell and facilitating the grieving process. As complicated grief heightens a global (i.e., physical, psychological, economic) risk for bereaved family members, our study is among the first to focus on such a fundamental yet unmet aspect.
5.1. Strengths and limitations
This is the first study in Italy to describe EoL care in COVID‐19 patients in a large ICU. Also, our study compares the stress level of family members in relation to whether they could make an ICU visit or a final video call. Since EoL video calls have not been extensively discussed in the literature, their use by family members needs to be evaluated.
The present study has several limitations. Early during the pandemic nursing notes about EoL comfort care were incomplete, precluding a full picture of the comfort care delivered by the ICU staff. Second, since this is a single‐center study conducted in a geographical area severely hit by the COVID‐19 pandemic, our findings cannot be generalized. A high IES‐R score might also reflect the problematic local social circumstances. The emotional shock associated with the worsening pandemic 37 and the strict lockdown measures enforced in Lombardy might have played a role in driving people's reactions. 38 Third, the family members were interviewed between 6 and 18 months after the patient's death; such a wide time span might have influenced the processing of bereavement. Fourth, the stress levels were measured with a single tool that evaluates the psychological post‐traumatic distress following a single event.
6. CONCLUSION
During the first year of the COVID‐19 pandemic, many ICU patients died while on life‐sustaining treatment and without their family members present. Most family members had elevated stress levels, especially the patients' spouses. The provision of making a video call or ICU visit was judged favourably by family members but was not felt to be sufficient to alleviate death‐related stress. ICU visits by family members should be encouraged, particularly when death is imminent and also in extremeevents.
AUTHOR CONTRIBUTIONS
Filippo Binda and Simone Gambazza contributed equally (co‐second author). All authors made substantial contributions to the conception (Alessandro Galazzi, Maura Lusignani and Dario Laquintana) or design (Alessandro Galazzi, Filippo Binda, Simone Gambazza, Elisa Colombo and Filippo Binda) of the study, to the acquisition (Alessandro Galazzi, Filippo Binda and Filippo Cantù) analysis or interpretation (Alessandro Galazzi, Simone Gambazza, Elisa Colombo and Maura Lusignani) of data, or to the drafting (Alessandro Galazzi, Filippo Binda, Simone Gambazza and Filippo Cantù) and critical revision (Giacomo Grasselli, Dario Laquintana and Laura Rasero) of the manuscript. All authors approved the final version of the manuscript and participated sufficiently in the work to take public responsibility for appropriate portions of the content.
ACKNOWLEDGEMENTS
The authors wish to thank the patients' family members for participating in the study. The authors also thank the ICU staff for their dedication and work.
Galazzi A, Binda F, Gambazza S, et al. The end of life of patients with COVID‐19 in intensive care unit and the stress level on their family members: A cross‐sectional study. Nurs Crit Care. 2022;1‐8. doi: 10.1111/nicc.12783
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1. WHO Coronavirus (COVID‐19) Dashboard, https://covid19.who.int/ (accessed February 15, 2022).
- 2. Foti G, Giannini A, Bottino N, et al. Management of critically ill patients with COVID‐19: suggestions and instructions from the coordination of intensive care units of Lombardy. Minerva Anestesiol. 2020;86(11):1234‐1245. doi: 10.23736/S0375-9393.20.14762-X [DOI] [PubMed] [Google Scholar]
- 3. Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID‐19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345‐1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kleinpell R, Heyland DK, Lipman J, et al. Patient and family engagement in the ICU: report from the task force of the world Federation of Societies of intensive and critical care medicine. J Crit Care. 2018;48:251‐256. [DOI] [PubMed] [Google Scholar]
- 5. Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family‐centered Care in the Neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103‐128. [DOI] [PubMed] [Google Scholar]
- 6. Kentish‐Barnes N, Cohen‐Solal Z, Morin L, Souppart V, Pochard F, Azoulay E. Lived experiences of family members of patients with severe COVID‐19 who died in intensive care units in France. JAMA Netw Open. 2021;4(6):e2113355. doi: 10.1001/JAMANETWORKOPEN.2021.13355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Azoulay E, Cariou A, Bruneel F, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID‐19 a cross‐sectional study. Am J Respir Crit Care Med. 2020;202:1388‐1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bisesti A, Mallardo A, Gambazza S, et al. Facing COVID‐19 pandemic in a tertiary Hospital in Milan: prevalence of burnout in nursing staff working in sub‐intensive care units. Int J Environ Res Public Health. 2021;18:6684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azoulay E, Pochard F, Kentish‐Barnes N, et al. Risk of post‐traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987‐994. [DOI] [PubMed] [Google Scholar]
- 10. Gries CJ, Engelberg RA, Kross EK, et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest. 2010;137:280‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harlan EA, Miller J, Costa DK, et al. Emotional experiences and coping strategies of family members of critically ill patients. Chest. 2020;158:1464‐1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rose L, Cook A, Casey J, Meyer J. Restricted family visiting in intensive care during COVID‐19. Intensive Crit Care Nurs. 2020;60:102896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mistraletti G, Gristina G, Mascarin S, et al. How to communicate with families living in complete isolation. BMJ Support Palliat Care. 2020. doi: 10.1136/bmjspcare-2020-002633 [DOI] [PubMed] [Google Scholar]
- 14. Galazzi A, Brioni M, Mistraletti G, et al. End of life in the time of COVID‐19: the last farewell by video call. Minerva Anestesiol. 2020;86(11):1254‐1255. doi: 10.23736/S0375-9393.20.14906-X [DOI] [PubMed] [Google Scholar]
- 15. Galazzi A, Binda F, Gambazza S, et al. Video calls at end of life are feasible but not enough: a 1‐year intensive care unit experience during the coronavirus disease‐19 pandemic. Nurs Crit Care. 2021;26(6):531–533. doi: 10.1111/nicc.12647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mistraletti G, Giannini A, Gristina G, et al. Why and how to open intensive care units to family visits during the pandemic. Crit Care. 2021;25(1):191. doi: 10.1186/S13054-021-03608-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Craparo G, Faraci P, Rotondo G, Gori A. The impact of event scale ‐ revised: psychometric properties of the Italian version in a sample of flood victims. Neuropsychiatr Dis Treat. 2013;9:1427‐1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Multidisciplinary Working Group “ComuniCovid” . Italian Society of Anesthesia and Intensive Care (SIAARTI), Italian Association of Critical Care Nurses (Aniarti), ItalianSociety of emergency medicine (SIMEU) and IS of PC (SICP). How to communicate with families of patients in complete isolation during SARS‐CoV‐2 pandemic multidisciplinary working group “ComuniCoViD.”. Recenti Prog Med. 2020;111:357‐367. [DOI] [PubMed] [Google Scholar]
- 19. Protti A, Porta V, Severgnini P, et al. Family access to critically ill patients with COVID‐19: a noble but demanding goal. Minerva Anestesiol. 2021;87(8):956‐958. doi: 10.23736/S0375-9393.21.15663-9 [DOI] [PubMed] [Google Scholar]
- 20. Weiss DS, Marmar CR. The Impact of Event Scale – Revised. In: Wilson JP, Keane TM, eds. Assessing psychological trauma and PTSD. Guilford Press; 1997. [Google Scholar]
- 21. Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale ‐ revised. Behav Res Ther. 2003;41:1489‐1496. [DOI] [PubMed] [Google Scholar]
- 22. Rash CJ, Coffey SF, Baschnagel JS, Drobes DJ, Saladin ME. Psychometric properties of the IES‐R in traumatized substance dependent individuals with and without PTSD. Addict Behav. 2008;33:1039‐1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson RA, Wichern DW. Applied Multivariate Statistical Analysis. 6th ed. Pearson Education, Inc.; 2007. [Google Scholar]
- 24. Jackson D, Bradbury‐Jones C, Baptiste D, et al. Life in the pandemic: some reflections on nursing in the context of COVID‐19. J Clin Nurs. 2020;29:2041‐2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Binda F, Clari M, Nicolò G, et al. Quality of dying in hospital general wards: a cross‐sectional study about the end‐of‐life care. BMC Palliat Care. 2021;20(1):153. doi: 10.1186/S12904-021-00862-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Burchardi H. Let's open the door! Intensive Care Med. 2002;28:1371‐1372. [DOI] [PubMed] [Google Scholar]
- 27. Davidson J, Jones C, Bienvenu O. Family response to critical illness: postintensive care syndrome‐family. Crit Care Med. 2012;40:618‐624. [DOI] [PubMed] [Google Scholar]
- 28. McAdam JL, Dracup KA, White DB, et al. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med. 2010;38:1078‐1085. [DOI] [PubMed] [Google Scholar]
- 29. Amendola LM, Galazzi A, Zainaghi I, et al. Validation and analysis of the European quality questionnaire in Italian language. Int J Environ Res Public Health. 2020;17:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bailey JJ, Sabbagh M, Loiselle CG, Boileau J, McVey L. Supporting families in the ICU: a descriptive correlational study of informational support, anxiety, and satisfaction with care. Intensive Crit Care Nurs. 2010;26:114‐122. [DOI] [PubMed] [Google Scholar]
- 31. Bambi S, Iozzo P, Rasero L, Lucchini A. COVID‐19 in critical care units: rethinking the humanization of nursing care. Dimens Crit Care Nurs. 2020;39:239‐241. [DOI] [PubMed] [Google Scholar]
- 32. Cattelan J, Castellano S, Merdji H, et al. Psychological effects of remote‐only communication among reference persons of ICU patients during COVID‐19 pandemic. J Intensive Care. 2021;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mason TM, Tofthagen CS, Buck HG. Complicated grief: risk factors, protective factors, and interventions. J Soc Work End Life Palliat Care. 2020;16:151‐174. [DOI] [PubMed] [Google Scholar]
- 34. Lotterman JH, Bonanno GA, Galatzer‐Levy I. The heterogeneity of long‐term grief reactions. J Affect Disord. 2014;167:12‐19. [DOI] [PubMed] [Google Scholar]
- 35. Probst DR, Gustin JL, Goodman LF, Lorenz A, Wells‐di Gregorio SM. ICU versus non‐ICU hospital death: family member complicated grief, posttraumatic stress, and depressive symptoms. J Palliat Med. 2016;19:387‐393. [DOI] [PubMed] [Google Scholar]
- 36. Harlan C, Pitrelli S. A nursing home hug room softens the isolation of the coronavirus era ‐ The Washington Post. 2020, https://www.washingtonpost.com/world/europe/hug-room-coronavirus-nursing-homes/2020/12/23/973124c6-4187-11eb-b58b-1623f6267960_story.html (accessed September 17, 2021).
- 37. Brivio E, Oliveri S, Guiddi P, Pravettoni G. Incidence of PTSD and generalized anxiety symptoms during the first wave of COVID‐19 outbreak: an exploratory study of a large sample of the Italian population. BMC Public Health. 2021;21:1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nobili RM, Gambazza S, Spada MS, et al. Remote support by multidisciplinary teams: a crucial means to cope with the psychological impact of the SARS‐COV‐2 pandemic on patients with cystic fibrosis and inflammatory bowel disease in Lombardia. Int J Clin Pract. 2021;75(7):e14220. doi: 10.1111/ijcp.14220 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


