Abstract
Aim
We examined the impact of COVID‐19 regarding organizational and management issues at Israeli long‐term care facilities.
Background
Residents in facilities were very vulnerable to significant disease and mortality during COVID‐19.
Methods
A survey of 52 facilities in Israel was conducted in 2020, consisting of closed‐ and open‐ended questions. Mixed methods were used to analyze data both quantitatively and qualitatively.
Results
Three main effects emerged: worsened financial status of long‐term‐care facilities resulting from high expenditures for preventive measures and reduced revenue due to deaths and fewer resident admissions, increased workload due to decreased workforce and additional duties, and negative mental health effects on staff because of increased workload and the conflict between maintaining good clinical practice and following COVID‐19 regulations.
Conclusion
The development of government directives needs to take into account potential conflicts between the directives and quality care principles and to provide a balanced approach that assures humane care. Facilities and their staff lacked adequate pandemic‐related guidance and support.
Implications for Nursing Management
The results highlight the need to address staff shortages and training, to provide more support and clearer guidance to facilities and their staff, and to devise a framework and strategies for future health crises.
Keywords: COVID‐19, nursing homes, pandemic, personal protective equipment, quality care, staff burnout
1. BACKGROUND
Long‐term‐care facilities [hereinafter, ‘facilities’] for older persons in Israel consist of three main types: nursing homes, which are the most controlled institutions on the autonomy‐control continuum, for older persons with functional and/or mental impairments; facilities for functionally independent and semi‐dependent frail older persons; and continuing care retirement communities (CCRCs) mostly for functionally independent older persons, which represent the other end of the autonomy‐continuum in terms of freedom of choice and self‐determination (Lev & Ayalon, 2018). Prior to the outbreak of coronavirus disease 2019 (COVID‐19), the disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) pandemic, nursing homes experienced high transmission rates of infectious diseases due to overcrowding; sharing of resources, such as bathrooms; and suboptimal infection control practices (Lee et al., 2020; Strausbaugh et al., 2003). Among workers at facilities, one sixth had a second job (which added an average of 20 hours to their work week), and over 60% maintained double‐ or triple‐duty caregiving roles, increasing the risk of spreading COVID‐19 among patients (Van Houtven et al., 2020). Lack of staff trained in infection control, insufficient infection control and general understaffing in facilities were known challenges prior to the pandemic (Kim & Jang, 2018; Matheï et al., 2007). COVID‐19's rapid spread affected health care institutions and their staff. Some nursing home administrators identified lack of supplies and shortages of staff among their greatest and most common concerns (Quigley et al., 2020). The Health Ministry in Israel limited workers' ability to move between units and prohibited staff from working in more than one facility. Such regulations were reported to result in an abrupt decrease in staffing (Duan et al., 2020).
Although residents of facilities comprise a small portion of the general population, as of June 2020, many countries reported that between 40% and 85% of their COVID‐19 fatalities occurred in facilities (over 80% in Canada and Slovenia; between 60% and 80% in New Zealand, Belgium and Ireland; between 40% and 60% in Norway, France, Sweden, Finland, United States of America, Israel, United Kingdom and Portugal) (Comas‐Herrera et al., 2020). Yet few studies have examined the experiences of facility staff during the pandemic. Those studies which did, found emotional exhaustion and burnout among staff (Leskovic et al., 2020; Martínez‐López et al., 2021; White et al., 2021). Whereas administrators struggled with confusing and contradictory guidelines from various health agencies, frontline workers labored under increased workloads, feared becoming infected, and experienced the emotional burden of caring for residents who were subject to isolation, illness and death (White et al., 2021).
This paper aims to expand the body of research which examines COVID‐19's effect on facilities and their staff. Specifically, we investigated both how the pandemic affected facilities and how it impacted the routine and well‐being of facility staff.
2. METHODS
This research is part of a larger comprehensive study on the impact of COVID‐19 on facilities, staff and residents. The analysis of the impact on residents is summarized in a separate paper (Cohen‐Mansfield & Meschiany, 2022a). The study involved a cross‐sectional online survey, and in this paper, we focus on the sections of the survey pertaining to the impact of COVID‐19 on the facilities and their staff. Whereas most of the survey pertained to the time of completing the survey, it also included a retrospective section that queried about experiences during the first month of the pandemic, during the second month and at the time of completing the survey. Data collection took place between mid‐July and mid‐October, 2020.
2.1. Participants
The Israel Ministry of Health website lists 250 facilities that provide older person care. Phone calls were attempted to all 250 facilities. Fifty facilities were never reached, and for nine, closure or invalid contact information prevented contact. Of the 191 facilities reached, 61 (32%) declined to participate in the survey. We sent online questionnaires and follow‐up reminders to the remaining 130 facilities that had agreed to participate. Complete responses were collected from 52 facilities.
We endeavored to elicit responses from facility directors, but some directors authorized other knowledgeable staff to respond on their behalf (including occupational therapists, nurses, a social worker and a gerontologist). Presumably well positioned to respond with expertise and insight, these staff members (some serving in more than one role) added perspectives that likely provided a fuller understanding of COVID‐19's effects on the facilities and their staff. In order to determine whether the 52 long‐term‐care facilities that participated were representative of the larger long‐term‐care facility population in Israel, we entered the data concerning size of facility and its for‐profit or non‐profit status for all the facilities that did not participate. We then compared the 52 participating facilities to two groups: (1) all other facilities on the list and (2) all other facilities that answered the phone (given that those that did not answer the phone may have been closed or in the process of closing). The comparisons of the 52 participating facilities to the two groups and for the two variables (size and profit status) were conducted via chi‐square analyses. These analyses showed that the sample was representative of the larger population.
2.2. Assessment
The questionnaire, developed specifically for this study, included background questions about the responding participant's long‐term‐care facility, about the responding participant, and multiple questions about the impact of COVID‐19. It was developed on the basis of prior research on facilities in Israel and North America (Cohen‐Mansfield, 1995, 1997; Cohen‐Mansfield et al., 2012; Cohen‐Mansfield & Bester, 2006; Cohen‐Mansfield & Meschiany, 2022b), information gleaned from news media at the start of the pandemic, and discussions with a nursing home director, a nursing home social worker, and an activist involved in nursing home issues. This paper reports on the questionnaire results regarding the impact of COVID‐19 on the facilities and their workforce. The topics include the staff turnover rate during COVID‐19 and how employees experienced changes instituted by facilities in response to the pandemic.
The survey included both closed‐ and open‐ended questions. The closed‐ended questions inquired into facility demographic characteristics such as number of residents, number and type of units, and the responder's position at the facility. It included questions like: ‘Facility classification: a. For profit, b. Non‐profit. c. Other, please specify’; ‘Reasons for leaving: Please specify how many employees left for each reason: a. Already working at another facility, b. Fear related to increased risk of illness/death due to old age, c. Having diseases that place them at heightened risk if infected, d. Took unpaid leave, e. Contracted COVID‐19, f. Contracted other illness, g. Other, please specify’; and ‘For the following time periods, please describe how the pandemic and staff turnovers affected the stress levels of the remaining staff, compared to the period before COVID‐19. Please use the following scale: 1—Stress decreased to a large extent; 2—stress decreased to a small extent; 3—stress decreased to a moderate extent; 4—stress level has not changed; 5—stress increased to a small extent; 6—stress increased to a moderate extent; 7—stress increased to a large extent; 9—other, please specify. a. The beginning of the pandemic (first month) ___ b. Second month ___ c. Today (time of interview) ___’.
The open‐ended questions included questions such as, ‘what was the greatest challenge posed by the pandemic?’; ‘Please specify whether and what changes were made in work routines during the COVID‐19 pandemic (shifts, contraction/extension of working hours, changes in work procedures, etc.)’; and ‘In the aftermath of the pandemic, what actions would you suggest for the present and in the future that will benefit the facility/residents?’
2.3. Analysis
2.3.1. Quantitative approach
Responses to closed‐ended questions were analyzed quantitatively, using IBM® SPSS® Statistics 26. Differences between groups were compared via t tests for ordinal and interval data, and through chi‐square for nominal level data. Differences between measurement times of stress level from COVID‐19 were compared via repeated measures ANOVA, with post‐hoc tests using Bonferroni corrections.
2.3.2. Qualitative approach
Responses to open‐ended questions and interviewee comments were analyzed qualitatively, by way of the following steps: (1) acquiring a sense of each open‐ended response, (2) extracting significant statements, (3) formulating meanings, (4) organizing formulated meanings into clusters of themes, (5) exhaustively describing the investigated phenomenon and (6) describing the fundamental structure of the phenomenon. These steps were guided by emergent coding strategy (Stemler, 2000), whereby two research staff members read, coded and categorized responses independently and then revised the codes through discussion until agreement was reached. The proposed coding was reviewed by another staff member, and the main themes were ultimately agreed upon by all research staff involved. Themes are illustrated via quotes. Quotes in this paper are identified by facility number, for‐profit versus not‐for‐profit status and facility size: (small, medium or large). Finally, coded data were used to build a process map reflecting the explanations given by the interviewees and diagrammatically depicting the relationships between the themes that emerged.
2.4. Ethical considerations
During the recruitment telephone calls and at the beginning of the questionnaire, potential participants were informed of the purpose of the research, assured that their participation was voluntary and advised that they could stop answering the questionnaire at any time. Informed consent to participate was obtained verbally on the phone and also inferred by completion of the online questionnaire. Ethical approval was obtained from the Institutional Review Board of Tel Aviv University, Number 0001467‐1.
3. RESULTS
3.1. Characteristics of participants and facilities
The 52 facilities that completed the online questionnaire included 28 nursing homes (54%), 14 assisted living facilities (most having nursing care units) (27%) and 10 long‐term geriatric hospitals (19%). Of the facilities, 34% were small (S) (9–38 residents, M = 25.7, SD = 8.6). The same percentage of facilities were medium (MED) (39–120 residents, M = 75.6, SD = 22.3), and 32% were large (L) (120–450 residents, M = 207.4, SD = 81.5). Most facilities (n = 37, 71%) were for‐profit (P) and 29% (n = 15) not‐for‐profit (NP), of which four were kibbutz (collective community)‐sponsored facilities for community members (K). Most of the responders (80%) were facility directors. Others were occupational therapists (8%), nurses (6%), a social worker (2%) and a gerontologist (2%). Characteristics of the facilities and respondents who completed the questionnaire are presented in Table 1.
TABLE 1.
Facility and respondent characteristics (n = 52), Israel
| n | |
|---|---|
| Type of facilities | |
| For profit | 37/52 (71%) |
| Not for profit | 15/52 (29%) |
| Nursing home | 28/52 (54%) |
| Assisted living facilities | 14/52 (27%) |
| Geriatric long‐term hospital | 10/52 (19%) |
| Facility size | |
| # of beds, range, mean (SD) | |
| Small 9–38, 25.7 (8.6) | 17/50 (34%) |
| Medium 39–120, 75.6 (22.3) | 17/50 (34%) |
| Large 121–450, 207.4 (81.5) | 16/50 (32%) |
| Responder gender (female) | 30/52 (58%) |
| Responder role | |
| Facility manager | 41/51 (80%) |
| Activity worker | 4/51 (8%) |
| Nurse | 3/51 (6%) |
| Doctor | 1/51 (2%) |
| Social worker | 1/51 (2%) |
| Gerontologist | 1/51 (2%) |
| Mean (SD) | Min | Max | |
|---|---|---|---|
| Total departments per facility | 3.0 (2.2) | 1 | 10 |
| Types of units per facility | |||
| Skilled nursing | 1.8 (1.2) | 0 | 5 |
| Nursing | 1.0 (2.5) | 0 | 10 |
| Dementia unit for mobile residents | 0.9 (0.8) | 0 | 3 |
| Assisted living | 0.9 (0.8) | 0 | 2 |
| Independent | 0.5 (0.5) | 0 | 1 |
| Residents | |||
| # in the facility | 100.8 (90.1) | 9 | 450 |
| Beds | |||
| # standard geriatric nursing | 52.6 (39.7) | 14 | 180 |
| # dementia unit for mobile residents | 12.3 (20.5) | 0 | 90 |
3.2. Effects of the pandemic on the economic status of facilities
When facility administrators were asked to describe the effects of the pandemic, 31% answered that it led to significant economic damage: ‘We are unable to cope with the large expenses from COVID‐19, and we did not receive any help from the government’ (#2241, non‐profit [NP], small facility [SM]).
Fiscal difficulties were also raised when respondents were asked about the types of assistance they wished to receive. Whereas 15% of respondents indicated the need for direct financial help: ‘an extra budget to compensate for huge expenses and to recognize the [extra effort provided by] employees’ (#3192, for‐profit [P], large facility [LG]), others indicated more generally that higher funding would have enabled facilities to meet the unusual needs that arose. Requests included a wide range of needs, including personal protective equipment (PPE) (25%), ‘We would appreciate receiving a stock of protective equipment on a regular basis’ (#1961, P, medium‐sized facility [MED]), additional support to hire staff (15%), such as nursing assistants, ‘[we] need nursing assistants, but they need to be trained and allowed to continue working overtime [hours]’ (#2531, P‐LG), non‐professional staff for running leisure activities for residents (13%), ‘assistance of activity personnel, of music providers’ (#1081, P‐MED), external support for assuring adherence to pandemic guidelines (10%), ‘assistance in supervising family visits’ (#2691, P‐SM), psychological support for staff (4%), ‘psychological counseling in coping’ (#1392, P‐MED), and staff transportation (#1611, P‐MED) (2%).
About 27% of facilities reported a significant problem with PPE shortages and PPE costs: ‘In the first stage [of the pandemic], the need to buy protective equipment at excessive prices—up to 20 times greater than pre‐pandemic prices—posed a very significant financial challenge’ (#1641, NP‐LG). Shortages were also reported concerning disposable gloves (64% of respondents) and disinfectant products (53%).
The crisis posed by increased operating expenses was worsened by the drying up of new admissions: ‘The biggest problem today is the lack of residents—besides the deaths, there are almost no admissions of new residents, which makes it very difficult for the home [facility]’ (#3501, P‐LG).
3.3. Effects of the pandemic on facility workforce and workload
A quarter of the facilities reported staff shortages: ‘the facility is run with shortages and lack of permanent nursing staff’ (#3111, NP‐SM). The shortages of staff are shown in Table 2.
TABLE 2.
Turnover characteristics
| Left | Joined | ||||||
|---|---|---|---|---|---|---|---|
| Profession | Mean (SD) | Min | Max | Mean (SD) | Min | Max | T |
| Total | 6.0 (7.9) | 0 | 37 | 4.6 (5.5) | 0 | 24 | 1.33 |
| Nursing assistants | 2.5 (3.9) | 0 | 21 | 2.7 (2.7) | 0 | 10 | 0.41 |
| Nurses | 1.8 (3.6) | 0 | 20 | 1.6 (2.6) | 0 | 15 | 0.33 |
| Activity worker (TA) | 1.1 (1.8) | 0 | 10 | 0.4 (0.8) | 0 | 4 | 2.36* |
| Physiotherapists | 0.5 (0.9) | 0 | 3 | 0.2 (0.4) | 0 | 2 | 2.52* |
| Social worker | 0.3 (0.6) | 0 | 2 | 0.2 (0.6) | 0 | 3 | 1.07 |
| Occupational therapist | 0.4 (0.6) | 0 | 2 | 0.1 (0.3) | 0 | 1 | 2.18* |
| Doctors | 0.2 (0.5) | 0 | 2 | 0.2 (0.5) | 0 | 2 | 0.00 |
| Communication clinician | 0.3 (0.5) | 0 | 1 | 0.1 (0.2) | 0 | 1 | 2.51* |
| Dietitians | 0.2 (0.4) | 0 | 1 | 0.1 (0.3) | 0 | 1 | 1.14 |
| Other | 0.3 (0.8) | 0 | 3 | 0.0 (0.0) | 0 | 0 | 1.67 |
p < .05.
Per facility, an average of 6.0 employees left (SD = 7.9, min = 0, max = 37), of whom 3.4 took unpaid vacation (SD = 4.0, min = 0, max = 15), whereas only 4.6 were newly hired (SD = 5.5, min = 0, max = 24). Therefore, only a portion of the staff that stopped working at these facilities could be replaced at a time of increased workload, and therefore, a time during which higher than normal staff levels were needed.
The main reason for staff departures was a new government regulation prohibiting employment of workers at more than one facility in order to reduce the risk of infection among facilities. On average, 4.5 employees (SD = 3.9, min = 0, max = 20) left facilities because they worked at another facility. Some workers left because they contracted COVID‐19 (M = 1.6, SD = 5.5, min = 0, max = 25), others because of fear of older staff related to their increased health risk (M = 1.5, SD = 1.1, min = 0, max = 4), because of personal health conditions that placed them at heightened risk of serious outcomes if infected (M = 0.9, SD = 0.8, min = 0, max = 2), or due to other illness (M = 0.1, SD = 0.3, min = 0, max = 1).
The departure of the staff described above left remaining staff with a greater workload. Due to staff shortages, facilities reported switching to double or longer shifts: ‘nursing assistants work 12–13 hours a day, with breaks’ (#1261, P‐SM). Workers were compelled to extend the scope of their professional responsibilities: ‘everyone worked in all roles according to tasks, regardless of job title’ (#2371, P, MED), and nursing assistants were asked to step in to the role of missing activity workers: ‘The staff was asked to do double shifts and also to run activities for the residents’ (#2081, P‐SM). Managerial staff also experienced a significant increase in their working hours: ‘the truth is that since the beginning of March, I have been almost living at the facility. Hours upon hours, no days and no nights’ (#1961, P‐MED).
3.4. Psychological effects of the pandemic on staff
COVID‐19 created fear and uncertainty, leading to a significant increase in negative emotions among staff, as reported by 67% of respondents who were asked directly about the impact of the pandemic on staff. For example, ‘the biggest problem is the mental stress and anxiety of the staff from the pandemic …’ (#2621, NP‐SM); ‘staff are in constant anxiety’ (#1522, P‐MED); or ‘dealing with increased anxiety or with employees' misunderstandings’ (#1451, P‐MED). Two thirds (66%) of respondents reported increased feelings of stress, worry and frustration: ‘I have been under stress for half a year. At the end of February, a very great fear and very great uncertainty began’ (#2081, P‐MED), and ‘there is uncertainty and ignorance regarding proper conduct, and guidelines vary’ (#2791, P‐SM).
The negative feelings of staff members were due not only to the uncertainty and direct consequences of COVID‐19 but also to various preventive measures implemented to try to curb the rate of infection. For example, at the beginning of the pandemic, family visits with residents were stopped. When asked about the cessation of visitation, about 25% of respondents reported an increase in their workload due to the need to accommodate residents' emotional difficulties with isolation and loneliness, a role particularly problematic for unskilled staff: ‘It had a big effect, as the residents shared their difficulties with the staff regarding the distance from the families and sometimes also projected their difficulties on them’ (#1392, NP, MED). Due to increased workload, opportunities for employees to carry out activities that contributed to their own well‐being were curtailed, as described by the director of one facility:
Avoiding activities that I would do, and I now feel that they are dangerous—especially exercise in the gym. I would go several times a week, and this is a favorite activity of mine, which contributes a lot to my mental well‐being. Now, I have stopped going to gym classes due to the fear of infection. (#1392, NP‐MED)
Another cause for staff discontent was the contradiction between COVID‐19‐related requirements and staff perceptions of good quality care. ‘One of the regulations is that [when] a resident goes to, or returns from the hospital, he needs to be isolated for two weeks, how can this work for a person with dementia? It's two weeks of abuse …’ (#1501, P‐MED), or ‘The behaviors to prevent … infection conflict with the values and foundations of the therapeutic professions and all those involved in promoting well‐being of the geriatric patient…’ (#2231, NP‐LG).
When asked to rate their stress levels at three time periods (in the first month of the pandemic, second month and as of the interview date) on a scale from 1 (stress decreased to a large degree) to 7 (stress increased to a large degree), in comparison with pre‐pandemic levels, the first month was associated with a sharp increase in the level of stress compared with pre‐pandemic levels (M = 5.7, SD = 0.8). In the second month, the reported increase in stress was lower (M = 5.2, SD = 1.2), and as of the interview date, the lowest increase in stress was reported (M = 4.5, SD = 1.9) (F (2,92) = 12.29, p < .001), though the reported rates still showed increases in comparison to pre‐pandemic levels. Post‐hoc Bonferroni comparisons showed that the increase in stress level was significantly higher in the first month than in the second (p < .05) and that these were higher than the stress levels in the third period (p < .05). However, even the levels of stress in the third period were significantly different from the pre‐pandemic levels, that is, as compared with ‘4’—no difference, (t (46) = 1.83, p < .05, one‐tailed comparison).
4. DISCUSSION
Three main themes emerged from the responses to the study survey concerning the impact of the COVID‐19 pandemic on facilities and their staff: worsened financial status for facilities, increased workload for staff and negative mental health effects on staff. The explanations of these effects and the inter‐relations among them are presented in Figure 1.
FIGURE 1.
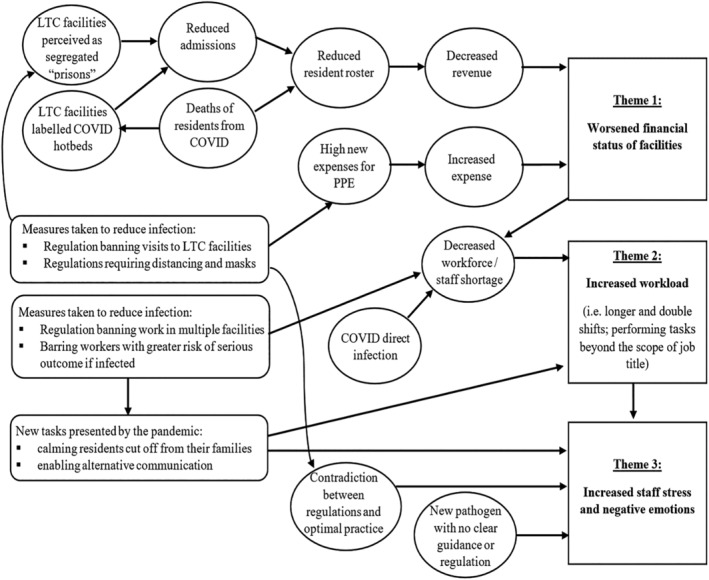
The impact of the COVID‐19 pandemic on long‐term care facilities and their staff
The deterioration in facility finances resulted from increased expenses pertaining to PPE and other supplies and decreased revenue based on diminished resident population due to COVID‐19 deaths and reduced resident admissions. The latter was influenced by the general perception that facilities were hotbeds for COVID‐19 deaths and that they resembled prisons since visitation was prohibited. Reduced admissions to facilities have been reported previously (Barnett et al., 2020).
The second theme, that of increased workload on staff, resulted from a decreased workforce, some of which was directly related to COVID‐19, that is, infection. The more potent influences on the workforce decrease were the measures taken to reduce infections, such as the prohibition on working at more than one facility, or the barring of older workers or those whose medical conditions placed them at greater risk of serious outcomes if infected by COVID‐19. The departure of staff exceeded the number of new hires possibly because the general pool of nursing home workers had shrunk as well, and the facilities' financial strains may have hindered recruitment. Staff shortages resulted in double and longer shifts and required staff to perform tasks beyond the scope of their previous duties or skill set. A study conducted in New York City also reported increased workload and short‐staffing issues that arose after the onset of the pandemic (Fisher et al., 2021).
The third theme, that of increased staff stress, burnout, and negative emotions, may be directly attributed to the increased workload and increased scope of responsibilities at a time of workforce shortage. Additional factors were mentioned by respondents in explaining the impact on mental health. Staff found themselves needing to respond to the escalated emotional needs of residents in the face of the residents' isolation from friends and family, coupled with fear of mortal illness. Staff needed to calm those residents and try to facilitate alternative communication with loved ones (Cohen‐Mansfield & Meschiany, 2022a). Other studies have reported negative emotions such as fatigue, discomfort and helplessness among staff due to heightened concern for residents and families (Sun et al., 2020) and even posttraumatic stress disorder symptoms associated with being a frontline health care worker (Rossi et al., 2020).
Another source of negative emotions was the sense of fear and uncertainty when dealing with a new disease for which clear guidance and standard regulation were lacking. Even when there was no question of clarity, such as the need for PPE, facilities encountered shortages and inflated costs. A related obstacle was the contradiction between regulations and optimal practice. A face mask decreases an older adult's ability to recognize staff members, and banning relatives from facilities detracts from normal social activity, likely the most important types of activities, particularly for those with dementia (Cohen‐Mansfield et al., 2010). Other reasons for the negative impact on staff's mental health included fear and anxiety about the pandemic itself, likely amplified by working in a location with a greater risk of infection, crowded conditions, insufficient testing and limited provision of PPE. Fear of being infected and infecting others were also described by White et al. (2021).
Several papers have reported on the provision of support services for staff. For example, psychological services have been provided, including assistance hotlines and around‐the‐clock online counseling services (Liu et al., 2020) and other services, such as educational training sessions, mental health services, and advocacy for provision of emotional and practical support (e.g., childcare, and access to showers and lodging) (Miotto et al., 2020). In contrast, none of our respondents mentioned receipt of these kinds of staff support, similar to what Fisher et al. (2021) have reported. The lack of these types of staff support in Israel likely contributed to the negative psychological effects of COVID‐19 on staff.
This paper complements that of Lyman et al. (2022). Lyman points to the crucial necessity of an adequate infrastructure in order for organizations to adapt to the changes caused by the pandemic. Our paper exemplifies how the issues of chronic inadequate staffing and the stigma associated with facilities stood in the way of organizational learning. The deficit in infrastructure affected facilities' ability to compensate for missing resources, such as the absence of family members or activity leaders who were not permitted to work at more than one facility. Similarly, whereas some facility directors were able to exercise leadership skills to devise and communicate a strategy for handling some of the new challenges, most did not report creating or executing such plans.
This study is unique in comparison with other reports on the effect of COVID‐19 on facilities and staff in that it studies a diverse and relatively large population of facilities, including for‐profit and not‐for‐profit facilities, as well as those of varying sizes. It is the first study to track changes in staff stress as a function of time after the beginning of the pandemic.
The study's use of a mixed methods design included quantitative and qualitative analyses of closed‐ and open‐ended question data, enabling this study to offer the first comprehensive model of factors involved in explaining COVID‐19's impact on facilities and their workforce.
4.1. Limitations
Our sample responded to the study's online questionnaire between mid‐July and mid‐October 2020, and therefore, early responses may have differed from later ones given changes in regulations and rates of illness. Indeed, when we specifically asked questions relating to different stages of the pandemic, responses varied by timing. Another limitation is our retrospective evaluation of staff stress at different points in time during the pandemic, rather than having studied it by means of repeated testing. The fact that 80% of responses were provided by facility managers may explain respondents' focus on facilities' finances. The high proportion of manager responses may limit a fuller understanding of the phenomenon of COVID‐19‐related staff turnover. Future research should aim to interview a broader range of nursing home employees, especially those who resigned during the pandemic. The study was conducted in only one country, Israel. The sample may be biased in that less than half of those who agreed to participate completed the questionnaire, suggesting that the respondents were more conscientious and perhaps more positive about the potential impact of a survey. On the other hand, our sample was representative of the larger pool of long‐term‐care facilities in Israel in terms of size and for‐profit status. These limitations notwithstanding, the sample size is large compared with others on this topic. Future studies should examine the impact of COVID‐19 on facilities and their staff in a still larger sample that would allow comparisons among different subtypes of facilities, based on size or the level of function of residents.
5. CONCLUSION
Government directives to cope with a pandemic need to take into account potential conflicts between the directives and quality care principles and to provide a balanced approach that assures humane care. Facilities and their staff lacked adequate pandemic‐related guidance and support. Future encounters with pandemics need to include both balanced guidelines and supportive (rather than punitive) guidance. Facility staff and residents will be better served in the future if policy leaders in the government and health care sectors assure the development of an infrastructure that facilitates the formulation of facility strategies to maintain good clinical practice in the face of unique pandemic challenges.
6. IMPLICATIONS FOR NURSING MANAGEMENT
The results highlight the need to (1) address staff shortages and training, (2) provide more support and clearer guidance to facilities and their staff and (3) devise a framework and strategies for future health crises.
CONFLICT OF INTERESTS
The author declares no conflicts of interest.
ETHICS STATEMENT
This study received ethical approval from the Institutional Review Board of Tel Aviv University, Number 0001467‐1.
ACKNOWLEDGEMENT
This work was supported by the Minerva Foundation (3158329500).
Cohen‐Mansfield, J. (2022). The impact of COVID‐19 on long‐term care facilities and their staff in Israel: Results from a mixed methods study. Journal of Nursing Management, 1–9. 10.1111/jonm.13667
DATA AVAILABILITY STATEMENT
Upon reasonable request, numerical data used for this study are available from the author in anonymized form after approval for sharing the data has been obtained from the institutional review board. The open‐ended data are not publicly available due to privacy and ethical concerns.
REFERENCES
- Barnett, M. L. , Hu, L. , Martin, T. , & Grabowski, D. C. (2020). Mortality, admissions, and patient census at SNFs in 3 US cities during the COVID‐19 pandemic. JAMA, 324(5), 507–509. 10.1001/jama.2020.11642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. (1995). Stress in nursing home staff: A review and a theoretical model. Journal of Applied Gerontology, 14(4), 444–466. 10.1177/073346489501400406 [DOI] [Google Scholar]
- Cohen‐Mansfield, J. (1997). Turnover among nursing home staff: A review. Nursing Management, 28(5), 59–62. 10.1097/00006247-199705010-00015 [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , & Bester, A. (2006). Flexibility as a management principle in dementia care: The Adards example. The Gerontologist, 46(4), 540–544. 10.1093/geront/46.4.540 [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , Juravel‐Jaffe, A. , Cohen, A. , Rasooly, I. , & Golander, H. (2012). Physicians' practice and familiarity with treatment for agitation associated with dementia in Israeli nursing homes. International Psychogeriatrics, 25(2), 236–244. 10.1017/S104161021200172X [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , & Meschiany, G. (2022a). Direct and indirect effects of COVID‐19 on long‐term care residents and their family members. Gerontology, 1–9. 10.1159/000521146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , & Meschiany, G. (2022b). Israeli nursing home staff perspectives on challenges to quality care for residents with dementia. Geriatric Nursing, 44, 15–23. 10.1016/j.gerinurse.2021.12.012 [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield, J. , Thein, K. , Dakheel‐Ali, M. , Regier, N. G. , & Marx, M. S. (2010). The value of social attributes of stimuli for promoting engagement in persons with dementia. The Journal of Nervous and Mental Disease, 198(8), 586–592. 10.1097/NMD.0b013e3181e9dc76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas‐Herrera, A. , Zalakaín, J. , Litwin, C. , Hsu, A. , Lemmon, E. , Henderson, D. , & Fernández, J.‐L. (2020). Mortality associated with COVID‐19 outbreaks in care homes: Early international evidence. LTCcovid.org, International Long‐Term Care Policy Network, CPEC‐LSE. https://ltccovid.org/wp-content/uploads/2021/02/LTC_COVID_19_international_report_January-1-February-1-2.pdf
- Duan, Y. , Iaconi, A. , Song, Y. , Norton, P. G. , Squires, J. E. , Keefe, J. , Cummings, G. G. , & Estabrooks, C. A. (2020). Care aides working multiple jobs: Considerations for staffing policies in long‐term care homes during and after the COVID‐19 pandemic. Journal of the American Medical Directors Association, 21(10), 1390–1391. 10.1016/j.jamda.2020.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, E. , Cardenas, L. , Kieffer, E. , & Larson, E. (2021). Reflections from the “forgotten front line”: A qualitative study of factors affecting wellbeing among long‐term care workers in New York City during the COVID‐19 pandemic. Geriatric Nursing, 42(6), 1408–1414. 10.1016/j.gerinurse.2021.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, K. W. , & Jang, S.‐N. (2018). Who comes to the emergency room with an infection from a long‐term care hospital? A retrospective study based on a medical record review. Asian Nursing Research, 12(4), 293–298. 10.1016/j.anr.2018.11.002 [DOI] [PubMed] [Google Scholar]
- Lee, M. H. , Lee, G. A. , Lee, S. H. , & Park, Y.‐H. (2020). A systematic review on the causes of the transmission and control measures of outbreaks in long‐term care facilities: Back to basics of infection control. PLoS ONE, 15(3), e0229911. 10.1371/journal.pone.0229911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leskovic, L. , Erjavec, K. , Leskovar, R. , & Vukovič, G. (2020). Burnout and job satisfaction of healthcare workers in Slovenian nursing homes in rural areas during the COVID‐19 pandemic. Annals of Agricultural and Environmental Medicine: AAEM, 27(4), 664–671. 10.26444/aaem/128236 [DOI] [PubMed] [Google Scholar]
- Lev, S. , & Ayalon, L. (2018). Moral distress among long‐term care social workers: Questionnaire validation. Research on Social Work Practice, 28(5), 628–637. 10.1177/1049731516672070 [DOI] [Google Scholar]
- Liu, S. , Yang, L. , Zhang, C. , Xiang, Y.‐T. , Liu, Z. , Hu, S. , & Zhang, B. (2020). Online mental health services in China during the COVID‐19 outbreak. The Lancet Psychiatry, 7(4), e17–e18. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyman, B. , Horton, M. K. , & Oman, A. (2022). Organizational learning during COVID‐19: A qualitative study of nurses' experiences. Journal of Nursing Management, 30(1), 4–14. 10.1111/jonm.13452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez‐López, J. Á. , Lázaro‐Pérez, C. , & Gómez‐Galán, J. (2021). Burnout among direct‐care workers in nursing homes during the COVID‐19 pandemic in Spain: A preventive and educational focus for sustainable workplaces. Sustainability, 13(5), 2782. 10.3390/su13052782 [DOI] [Google Scholar]
- Matheï, C. , Niclaes, L. , Suetens, C. , Jans, B. , & Buntinx, F. (2007). Infections in residents of nursing homes. Infectious Disease Clinics of North America, 21(3), 761–772. 10.1016/j.idc.2007.07.005 [DOI] [PubMed] [Google Scholar]
- Miotto, K. , Sanford, J. , Brymer, M. J. , Bursch, B. , & Pynoos, R. S. (2020). Implementing an emotional support and mental health response plan for healthcare workers during the COVID‐19 pandemic. Psychological Trauma Theory Research Practice and Policy, 12(S1), S165–S167. 10.1037/tra0000918 [DOI] [PubMed] [Google Scholar]
- Quigley, D. D. , Dick, A. , Agarwal, M. , Jones, K. M. , Mody, L. , & Stone, P. W. (2020). COVID‐19 preparedness in nursing homes in the midst of the pandemic. Journal of the American Geriatrics Society, 68, 1164–1166. 10.1111/jgs.16520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R. , Socci, V. , Pacitti, F. , Di Lorenzo, G. , Di Marco, A. , Siracusano, A. , & Rossi, A. (2020). Mental health outcomes among frontline and second‐line health care workers during the coronavirus disease 2019 (COVID‐19) pandemic in Italy. JAMA Network Open, 3(5), e2010185. 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stemler, S. (2000). An overview of content analysis. Practical Assessment, Research and Evaluation, 7(1), 17. 10.7275/z6fm-2e34 [DOI] [Google Scholar]
- Strausbaugh, L. J. , Sukumar, S. R. , Joseph, C. L. , & High, K. P. (2003). Infectious disease outbreaks in nursing homes: An unappreciated hazard for frail elderly persons. Clinical Infectious Diseases, 36(7), 870–876. 10.1086/368197 [DOI] [PubMed] [Google Scholar]
- Sun, N. , Wei, L. , Shi, S. , Jiao, D. , Song, R. , Ma, L. , Wang, H. , Wang, C. , Wang, Z. , You, Y. , Liu, S. , & Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID‐19 patients. American Journal of Infection Control, 48(6), 592–598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven, C. , Boucher, N. , & Dawson, W. (2020). The impact of COVID‐19 outbreak on long term care in the United States. Country report in LTCcovid org. International Long‐Term Care Policy Network. CPEC‐LSE. https://pdxscholar.library.pdx.edu/aging_pub/54/
- White, E. M. , Wetle, T. F. , Reddy, A. , & Baier, R. R. (2021). Front‐line nursing home staff experiences during the COVID‐19 pandemic. Journal of the American Medical Directors Association, 22(1), 199–203. 10.1016/j.jamda.2020.11.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon reasonable request, numerical data used for this study are available from the author in anonymized form after approval for sharing the data has been obtained from the institutional review board. The open‐ended data are not publicly available due to privacy and ethical concerns.


