Video
EUS demonstration of aneurysmal intrahepatic portosystemic venous shunt.
Abbreviation: PV, portal vein
A 76-year-old woman presented to an outside hospital for evaluation of persistent headache for 2 weeks. On laboratory assessments, she was found to have elevated erythrocyte sedimentation rate. Biopsy from the temporal artery was negative for temporal arteritis. An abdominal CT scan was performed and demonstrated a 25- × 24-mm mass lesion in the left liver lobe with enhancement in the portal venous phase (Fig. 1). Liver enzymes and tumor markers were unremarkable. She was referred for EUS examination at our center for further evaluation of the liver lesion. EUS revealed an aneurysmal communication between the left hepatic vein and the umbilical part of the left portal vein, which supplies blood to segments 2 and 3 of the liver (Fig. 2A and B; Video 1, available online at www.giejournal.org).1 Further interrogation with EUS revealed that ligamentum venosum was present, excluding the presence of patent ductus venosus (Fig. 3). Given the patient’s age, normal liver enzymes, and absence of symptoms, no radiologic or surgical intervention was pursued. The patient underwent expectant management with serial follow-up imaging.
Figure 1.
Abdominal CT scan showing an enhancing mass lesion (white arrow) in the left lobe of the liver.
Figure 2.
EUS images showing hepatic vein (red arrow), the umbilical portion of the left portal vein (yellow arrow), and aneurysmally dilated communicating vessel (white arrow) between the hepatic artery and portal vein. A, Regular EUS image. B, Color Doppler EUS image showing blood flow in the vessels.
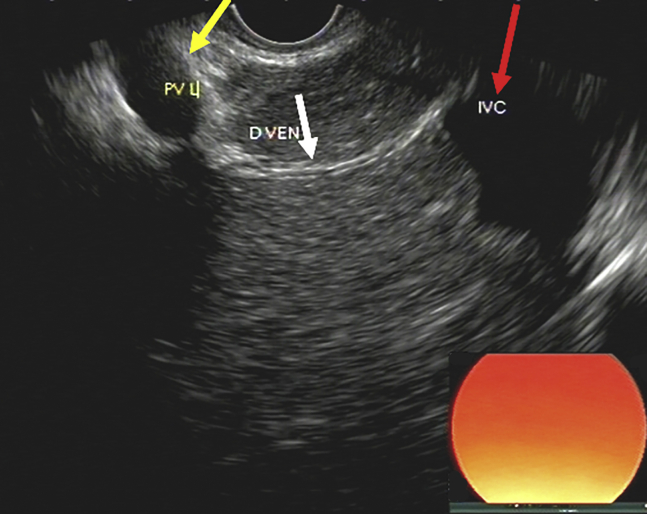
Figure 3.
EUS image showing ligamentum venosum (white arrow) attaching to the umbilical portion of the left portal vein (yellow arrow) and suprahepatic inferior vena cava (red arrow).
Portosystemic venous shunts can be divided into extrahepatic and intrahepatic. Extrahepatic shunts are seen in portal hypertension, with the typical example being esophageal varices communicating the left gastric vein to the azygos vein.2 Intrahepatic shunts are communicating vessels between the portal vein (PV) and a systemic vein within the liver.3 Small intrahepatic shunts between the PV and perihepatic veins may occur secondary to portal hypertension3; however, large intrahepatic shunts are rare congenital anomalies. Intrahepatic portosystemic venous shunts are classified into 4 types according to the Park classification.4 Type 1 is a large vessel communicating the right PV to the inferior vena cava. Type 2 consists of single or multiple vessels communicating branches of the PV to hepatic veins in a liver segment. Type 3 is aneurysmal communication between intrahepatic portal veins and hepatic veins. Type 4 includes multiple communications between peripheral portal and hepatic veins in both liver lobes. Ductus venosus, which connects the left umbilical vein to the inferior vena cava during fetal life, closes after birth and is called a ligamentum venosum. It may remain patent after birth and is considered a fifth type of intrahepatic venous shunt by some experts.5
Patients with intrahepatic shunts may present with a wide variety of adverse events, including hepatic encephalopathy and hepatopulmonary syndrome. However, many intrahepatic shunts may go unnoticed and are found incidentally on imaging studies.3,5
Our case was an aneurysmal communication between the left hepatic vein and the umbilical part of the left portal vein, representing type 3 intrahepatic shunt, and the patient had no sign of liver dysfunction. Aneurysmal portosystemic venous shunt is an exceedingly rare clinical condition. Its diagnosis with transabdominal ultrasound has been reported6; however, to our knowledge, this is the first reported case of type 3 intrahepatic portosystemic shunt diagnosed on EUS.
In conclusion, the reported case represents a benign vascular anomaly of the liver and requires no specific therapeutic intervention. It is important that endosonographers become familiar with the anatomy of the liver and its vascular anatomy to appropriately diagnose liver lesions and avoid unnecessary and potentially harmful diagnostic interventions.
Disclosure
All authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Al-Haddad at moalhadd@iu.edu.
Supplementary data
EUS demonstration of aneurysmal intrahepatic portosystemic venous shunt.
References
- 1.Sharma M., Somani P., Rameshbabu C.S., et al. Stepwise evaluation of liver sectors and liver segments by endoscopic ultrasound. World J Gastrointest Endosc. 2018;10:326–339. doi: 10.4253/wjge.v10.i11.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kiyosue H., Ibukuro K., Maruno M., et al. Multidetector CT anatomy of drainage routes of gastric varices: a pictorial review. Radiographics. 2013;33:87–100. doi: 10.1148/rg.331125037. [DOI] [PubMed] [Google Scholar]
- 3.Remer E.M., Motta-Ramirez G.A., Henderson J.M. Imaging findings in incidental intrahepatic portal venous shunts. AJR Am J Roentgenol. 2007;188:W162–W167. doi: 10.2214/AJR.05.1115. [DOI] [PubMed] [Google Scholar]
- 4.Park J.H., Cha S.H., Han J.K., et al. Intrahepatic portosystemic venous shunt. AJR Am J Roentgenol. 1990;155:527–528. doi: 10.2214/ajr.155.3.2117349. [DOI] [PubMed] [Google Scholar]
- 5.Papamichail M., Pizanias M., Heaton N. Congenital portosystemic venous shunt. Eur J Pediatr. 2018;177:285–294. doi: 10.1007/s00431-017-3058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chagnon S.F., Vallee C.A., Barge J., et al. Aneurysmal portahepatic venous fistula: report of two cases. Radiology. 1986;159:693–695. doi: 10.1148/radiology.159.3.3517953. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
EUS demonstration of aneurysmal intrahepatic portosystemic venous shunt.
EUS demonstration of aneurysmal intrahepatic portosystemic venous shunt.