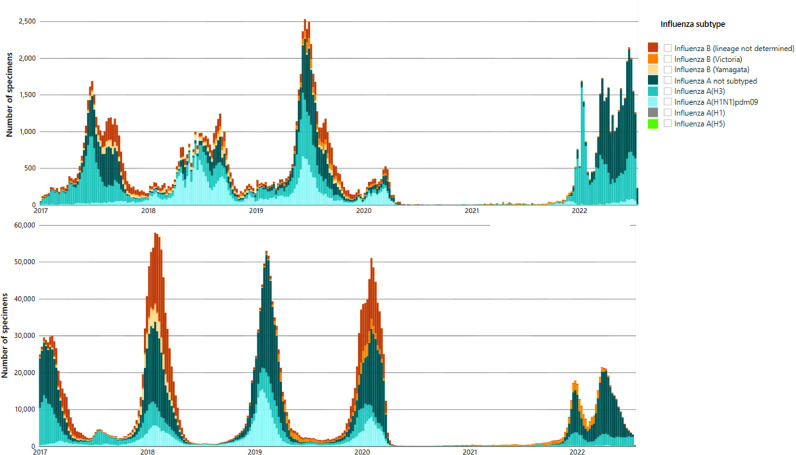
The COVID-19 pandemic has generated global perturbations in our daily lives that are unprecedented in scale. Since early 2020, changes in contact patterns and mobility have affected the regular seasonal cycles of many infectious diseases globally, including influenza (Figure 1 ). A better understanding of the effect of these perturbations can shed light on key epidemiological mechanisms that remain unclear despite decades of research. These include the strength and mechanisms that drive seasonality in transmission, the persistence of immunity from natural infection, the evolutionary bottlenecks operating during low transmission seasons, and the impact of non-pharmaceutical interventions (NPI) that could be used in future influenza pandemics.
Figure 1.
Patterns of weekly influenza virus circulation in the Northern (top) and Southern (bottom) Hemispheres, Jan 2017 to present. Different colors represent different influenza (sub)types. Data are based on laboratory confirmed influenza activity reported to WHO flunet (https://www.who.int/tools/flunet).
On a global scale, influenza circulation was particularly low in 2020 as lockdown and travel-related quarantines were imposed in many countries. Influenza started to resurge in late 2021, marked by out-of-season activity in the Southern Hemisphere. In the first half of 2022, seasonal patterns had not returned to normal, with unusually late and protracted influenza seasons in the Northern Hemisphere, and early season activity in the Southern Hemisphere. In June 2022, a peak in weekly influenza cases was reported in Australia, dominated by the A/H3N2 subtype (Department of Health and Aged Care. Australian Government, 2022), far exceeding their 5-year average and earlier than is typical. The upsurge of influenza occurred after the Omicron (B.1.1.529) wave peaked in January 2022, with reported co-circulation of SARS-CoV-2 and influenza A since that time. In South America, seasonal influenza arrived in Brazil in the odd summer months of November and December 2021 (Faico-Filho et al., 2022), between the Delta (B.1.617.2) and Omicron waves (Nott et al., 2022). As reported in the latest World Health Organization (WHO)’s update in July 2022 (WHO, 2022), influenza activity was decreasing in Argentina and Paraguay and increasing in Chile and Uruguay. South Africa experienced an unusually late influenza season in 2021, followed by a return to normal timing of activity in 2022, with both seasons dominated by A/H1N1. Overall, recent influenza activity in the temperate Southern Hemisphere is not occurring synchronously between countries nor with climatic drivers. What is to be expected of influenza activity patterns in the Northern Hemisphere in the coming months?
Seasonality is a hallmark of influenza epidemiology in the inter-pandemic period, a complex phenomenon shaped by the interplay of population contact patterns, virus survival and host immunity (Tamerius et al., 2011). Environmental and climatic influences have been shown to play a role in influenza seasonality but do not fully explain spatio-temporal variability in the occurrence of seasonal outbreaks (Shaman et al. 2010; Tamerius et al., 2013). During the interpandemic period, influenza seasons are well-synchronized in temperate climate zones of Northern and Southern Hemispheres and organized around their respective winters (Wenger et al., 2010; Lam et al., 2019; Morris et al., 2018). Yet, peak timing can vary by up to 3-4 months depending on the season (Price et al., 2019; Pica et al., 2012). In influenza pandemic seasons, which mark the emergence and dissemination of antigenically novel strains, large departures from regular seasonal cycles can occur. Out-of-season waves have been reported during the 1918 and 2009 influenza pandemics (Andreasen et al., 2008; He et al. 2015). These perturbations are typically limited to the first year of pandemic virus circulation. Of note, the evolutionary process generating new pandemic strains is unpredictable, involving cross-species transmission (for instance for swine to humans), a process which can theoretically occur in any season (Zimmer and Burke, 2009).
COVID-19 has generated more perturbation in influenza activity than prior influenza pandemics. When COVID-19 first emerged in 2020, little or no influenza activity was recorded in both the Northern (Chan et al., 2020) and Southern Hemispheres (Kim et al., 2021). The absence or abrupt subsidence of influenza circulation is likely the result of reduction of human mobility and contacts in response to COVID-19. While 2020 was a mostly silent year for influenza, the situation in 2021-2022 has been more difficult to interpret. The heterogeneity in magnitude and timing of influenza activity globally can be partly attributed to the diversity of COVID-19 control strategies. The roll-out of COVID-19 vaccines in 2021, with varied coverage between countries, age groups and time periods, resulted in decreased uptake for other vaccines (Maltezou et al., 2022), though the global impact on influenza coverage has yet been fully evaluated. In the US for instance, COVID-19 vaccination has increased disparities in influenza vaccine coverage between states (Leuchter et al., 2022). Further, NPI to mitigate COVID19 have been highly heterogeneous between countries, ranging from containment to achieve elimination on one end, to mitigation with strategic relaxation on the other. This would have likely increased heterogeneity in contacts between locations and in turn in permissiveness for influenza transmission (Oliu-Barton et al., 2022). With the ever-changing COVID-19 crisis as the backdrop, waning population immunity against influenza and reduced genetic diversity of circulating influenza viruses add to the unpredictability of future outbreaks, creating challenges in the development of control strategies (Dhanasekaran et al., 2022).
Experimental data indicate that co-infection between influenza and SARS-CoV-2 viruses is a condition of concern, with co-infected mice progressing to severe disease (Achdout et al., 2021). The relentless occurrence of COVID-19 outbreaks fuelled by new variants, along with a return of influenza, could potentially increase the likelihood of influenza/SARS-CoV-2 infection. However, epidemiological studies in England and the USA have shown that influenza infection was associated with a lower risk of SARS-CoV-2 infection (Stowe et al., 2021; Nowak et al., 2020) though co-infection, when it occurred, led to risk of severe disease and death (Stowe et al., 2021). There may be antagonistic competition between these two viruses limiting the risk of co-infection, perhaps modulated by the innate immune response. A similar phenomenon has been demonstrated for influenza and common cold rhinoviruses, or COVID-19 and rhinovirus (Nickbakhsh et al., 2019), and even if co-infections remain rare, the combined impact of a COVID-19 and influenza outbreak could wreak havoc on a country's health system. Vaccination and NPIs could be important tools for the prevention of influenza in this context. But when and how should we implement these interventions given the heterogeneous and dynamic nature of influenza circulation post COVID-19?
Over the past decades, the synchronicity of influenza circulation at the hemispheric level has enabled a global control strategy to be developed (Saha et al., 2014), centered on semi-annual vaccine recommendations based on a country's Hemispheric location. The disorderly return of influenza activity in 2021-2022 brings up new questions for control: will influenza seasonal patterns return to normal after the COVID-19 pandemic? Should the timing of influenza vaccination be altered and should influenza campaigns be synchronized with COVID-19 immunization? Should the current scheme for designing the composition of the annual vaccine be revised? Do NPIs have differential impacts on SARS-CoV-2 and influenza transmission? And what about other respiratory infections? This is a critically opportune period to launch well-designed research studies and understand the interplay between seasonal forcing, immunity, contacts and infection. These studies include statistical and model-based analyses of real-world surveillance data, analyses of the transmission of different influenza lineages, clinical research on influenza/SARS-CoV-2 co-infections, and monitoring of changes in population immunity through sero-epidemiology. There may be a small silver lining in the COVID-19 crisis we face globally, which is to offer new insights on the epidemiology of other pathogens and new opportunities for control.
REFERENCES
- Achdout H, Vitner EB, Politi B, Melamed S, Yahalom-Ronen Y, Tamir H, et al. Increased lethality in influenza and SARS-CoV-2 coinfection is prevented by influenza immunity but not SARS-CoV-2 immunity. Nat Commun. 2021;12(1):5819. doi: 10.1038/s41467-021-26113-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen V, Viboud C, Simonsen L. Epidemiologic characterization of the 1918 influenza pandemic summer wave in Copenhagen: implications for pandemic control strategies. J Infect Dis. 2008;197(2):270–278. doi: 10.1086/524065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan CP, Wong NS, Leung CC, Lee SS. Positive impact of measures against COVID-19 on reducing influenza in the Northern Hemisphere. J Travel Med. 2020 doi: 10.1093/jtm/taaa087. [ePub 28 May 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Aged Care. Australian Government. Australian Influenza Surveillance Report and Activity Updates. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-ozflu-flucurr.htm (Accessed 30 July 2022).
- Dhanasekaran V, Sullivan S, Edwards KM, Xie R, Khvorov A, Valkenburg SA, et al. Human seasonal influenza under COVID-19 and the potential consequences of influenza lineage elimination. Nat Commun. 2022;13(1):1721. doi: 10.1038/s41467-022-29402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faico-Filho KS, Barbosa GR, Bellei N. Peculiar H3N2 outbreak in São Paulo during summer and emergence of the Omicron variant. J Infect. 2022;85(1):90–122. doi: 10.1016/j.jinf.2022.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He D, Lui R, Wang L, Tse CK, Yang L, Stone L. Global Spatio-temporal Patterns of Influenza in the Post-pandemic Era. Sci Rep. 2015;5:11013. doi: 10.1038/srep11013. https://doi.orfg/10.1038/srep11013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Gómez Gómez RE, Hong K, Yum S, Jang J, Chun BC. Changing influenza activity in the Southern Hemisphere countries during the COVID-19 pandemic. Int J Infect Dis. 2021;108:109–111. doi: 10.1016/j.ijid.2021.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam TT, Tang JW, Lai FY, Zaraket H, Dbaibo G, Bialasiewicz S, et al. Comparative global epidemiology of influenza, respiratory syncytial and parainfluenza viruses, 2010-2015. J Infect. 2019;79(4):373–382. doi: 10.1016/j.jinf.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leuchter RK, Jackson NJ, Mafi JN, Sarkisian CA. Association between Covid-19 Vaccination and Influenza Vaccination Rates. N Engl J Med. 2022;386(26):2531–2532. doi: 10.1056/NEJMc2204560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maltezou HC, Medic S, Cassimos DC, Effraimidou E, Poland GA. Decreasing routine vaccination rates in children in the COVID-19 era. Vaccine. 2022;40(18):2525–2527. doi: 10.1016/j.vaccine.2022.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SE, Freiesleben de Blasio B, Viboud C, Wesolowski A, Bjørnstad ON, et al. Analysis of multi-level spatial data reveals strong synchrony in seasonal influenza epidemics across Norway, Sweden, and Denmark. PLoS One. 2018;13(5) doi: 10.1371/journal.pone.0197519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickbakhsh S, Mair C, Matthews L, Reeve R, Johnson PCD, Thorburn F, et al. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc Natl Acad Sci USA. 2019;116(52):27142–27150. doi: 10.1073/pnas.1911083116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nott R, Fuller TL, Brasil P, Nielsen-Saines K. Out-of-season influenza during a COVID-19 void in the State of Rio de Janeiro, Brazil: temperature matters. Vaccines (Basel) 2022;10(5):821. doi: 10.3390/vaccines10050821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak MD, Sordillo EM, Gitman MR, Paniz Mondolfi AE. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J Med Virol. 2020;92(10):1699–1700. doi: 10.1002/jmv.25953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliu-Barton M, Pradelski BSR, Algan Y, Baker MG, Binagwaho A, Dore GJ, et al. Elimination versus mitigation of SARS-CoV-2 in the presence of effective vaccines. Lancet Glob Health. 2022;10(1):e142–e147. doi: 10.1016/S2214-109X(21)00494-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pica N, Bouvier NM. Environmental factors affecting the transmission of respiratory viruses. Curr Opin Virol. 2012;2(1):90–95. doi: 10.1016/j.coviro.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RHM, Graham C, Ramalingam S. Association between viral seasonality and meteorological factors. Sci Rep. 2019;9(1):929. doi: 10.1038/s41598-018-37481-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Chadha M, Al Mamun A, Rahman M, Sturm-Ramirez K, Chittaganpitch M, et al. Influenza seasonality and vaccination timing in tropical and subtropical areas of southern and south-eastern. Asia. Bull World Health Organ. 2014;92(5):318–330. doi: 10.2471/BLT.13.124412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol. 2010;8(2) doi: 10.1371/journal.pbio.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowe J, Tessier E, Zhao H, Guy R, Muller-Pebody B, Zambon M, et al. Interactions between SARS-CoV-2 and influenza, and the impact of coinfection on disease severity: a test-negative design. Int J Epidemiol. 2021;50(4):1124–1133. doi: 10.1093/ije/dyab081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius J, Nelson MI, Zhou SZ, Viboud C, Miller MA, Alonso WJ. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect. 2011;119(4):439–445. doi: 10.1289/ehp.1002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius JD, Shaman J, Alonso WJ, Bloom-Feshbach K, Uejio CK, Comrie A, et al. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9(3) doi: 10.1371/journal.ppat.1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger JB, Naumova EN. Seasonal synchronization of influenza in the United States older adult population. PLoS One. 2010;5(4):e10187. doi: 10.1371/journal.pone.0010187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva: 2022. Influenza Update no. 421.https://www.who.int/publications/m/item/influenza-update-n-421 accessed on 26 June 2022. [Google Scholar]
- Zimmer SM, Burke DS. Historical perspective–Emergence of influenza A (H1N1) viruses. N Engl J Med. 2009;361(3):279–285. doi: 10.1056/NEJMra0904322. [DOI] [PubMed] [Google Scholar]