Video
The case report is presented in the video, with a description of the patient’s clinical course along with a set of endoscopic interventions including the use of per-oral pancreatoscopy with holmium laser therapy for stricturoplasty and stone fragmentation.
Abbreviations: PD, pancreatic duct; POP, peroral pancreatoscopy
Introduction
Pancreatic duct (PD) stones and strictures remain challenging sequelae of chronic calcific pancreatitis and contribute to ductal hypertension, which may manifest as abdominal pain, exocrine pancreatic insufficiency, or biliary obstruction.1,2 Standard ERCP techniques may be insufficient for complex lesions such as severe stricture(s) or extensive stone burden, whereby the degree of obstruction or ductal tortuosity may not permit passage of the wire or catheter.3 Peroral pancreatoscopy (POP) promotes direct ductal visualization and use of additional devices to treat such advanced pathology, which includes laser therapy that can be used for stone fragmentation or tissue dissection as a means of stricturoplasty.4 These techniques have been previously described,3,5, 6, 7 with benefits of potentially reducing or delaying the need for surgery.
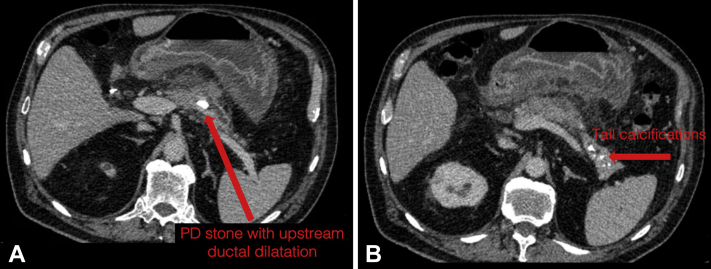
We present a case of a 74-year-old man with alcohol/tobacco-induced chronic calcific pancreatitis, admitted with an acute flare of pancreatitis attributable to a 15-mm stone in the PD body and a severe stricture immediately downstream (Fig. 1), which subsequently required successive POP sessions.
Figure 1.
Index CT scan from referring hospital, demonstrating 15-mm intraductal stone in the body of the main pancreatic duct and upstream ductal dilatation (A). Parenchymal tail calcifications are also noted (B).
Description of technology
Using a standard duodenoscope (Olympus, Center Valley, Pa, USA), we advanced the SpyGlass DS2 (Boston Scientific, Marlborough, Mass, USA for direct pancreatoscopy. A holmium laser (Litho, Quanta System, Italy) was selected in this case for intervention of the large stone burden. The 272-μm, 100-W holmium laser was used for both the initial stricture dissection (lower power soft tissue settings) and later stone fragmentation (lithotripsy settings), with a range of 0.5 to 2.5 J, 5 to 30 W. The first POP session, which primarily involved stricturoplasty and only limited lithotripsy, used a total energy of 2.78 kJ, compared to 26.2 kJ during the second POP session during which stone fragmentation was the primary focus.
Video description
Index ERCP revealed a severe, 3-cm segmental stricture immediately downstream from the intraductal stone, which could not be traversed with the wire or contrast to consider use of traditional dilation via balloon or screw tip drill. A 7F × 10-cm single pigtail stent was placed to the margin of the stone to secure future access to the site for subsequent POP therapy and for possible stone fragmentation. At follow-up ERCP, the initial POP session was pursued as planned. Concise strokes were performed with the holmium laser across the stricture using tissue ablation settings, applied in 3-quadrant fashion. The superior quadrant is difficult to access because of the directionality of the laser fiber exiting from the pancreatoscope in the 6 o’clock position.
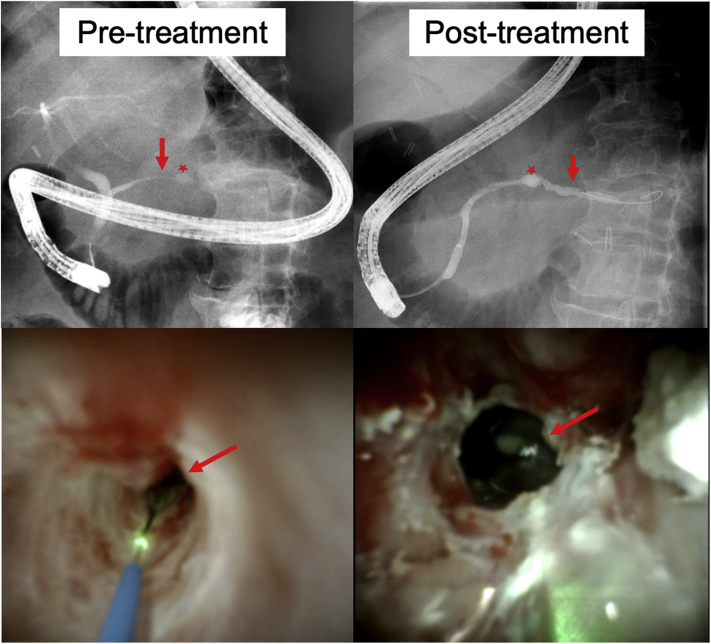
By the end of the first POP session, the wire was able to traverse to the tail, and the proximal margin of the stone was visualized, allowing limited lithotripsy to be performed. At the follow-up POP session, significant obstruction persisted, although there was improved patency of the stricture. Minimal stricturoplasty was required, after which the entire stone could be accessed with the pancreatoscope, and near complete ductal clearance was achieved after lithotripsy (Fig. 2). A 10F × 18-cm wedge stent was placed to the tail. Since this last POP session, the patient has remained clinically stable with improvement of abdominal pain and no further pancreatitis flares or hospitalizations. A 3-month follow-up ERCP is scheduled with anticipated POP if there are residual stone(s) or is a need for further stricturoplasty.
Figure 2.
Fluoroscopic images (top images) and direct visualization of the stricture and stone by pancreatoscopy (bottom images) reveal marked improvement in the caliber of the pancreatic duct and a reduction in the size of the stone after peroral pancreatoscopy therapies. Preintervention images are represented in the left panel, in contrast to postintervention in the right panel.
Take-home message
Complex PD strictures or stones may require advanced techniques owing to limitations of standard devices in accessing the affected area because of the degree of ductal narrowing and stone location. POP overcomes these barriers by targeted laser therapy of both PD strictures and stones simultaneously during the same session, which is a novel application of these combined methods demonstrated in this video (Video 1, available online at www.giejournal.org). Ductal patency was restored to the tail, leading to preservation of a significant portion of a potentially viable pancreas and thereby avoiding the need for surgery.
Disclosure
Dr Shah is an advisory board member for Boston Scientific and a consultant for Boston Scientific, Cook Medical, and Olympus. All other authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Shah at Raj.Shah@cuanschutz.edu.
Supplementary data
The case report is presented in the video, with a description of the patient’s clinical course along with a set of endoscopic interventions including the use of per-oral pancreatoscopy with holmium laser therapy for stricturoplasty and stone fragmentation.
References
- 1.Dumonceau J.M., Delhaye M., Tringali A., et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Updated August 2018. Endoscopy. 2019;51:179–193. doi: 10.1055/a-0822-0832. [DOI] [PubMed] [Google Scholar]
- 2.Kitano M., Gress T.M., Garg P.K., et al. International consensus guidelines on interventional endoscopy in chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancreatology, the American Pancreatic Association, the Japan Pancreas Society, and European Pancreatic Club. Pancreatology. 2020;20:1045–1055. doi: 10.1016/j.pan.2020.05.022. [DOI] [PubMed] [Google Scholar]
- 3.Han S., Shah R.J. Cholangiopancreatoscopy-guided laser dissection and ablation for pancreas and biliary strictures and neoplasia. Endosc Int Open. 2020;8:E1091–E1096. doi: 10.1055/a-1192-4082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaura T., Willingham F.F., Chawla S. Role of pancreatoscopy in management of pancreatic disease: a systematic review. World J Gastrointest Endosc. 2019;11:155–167. doi: 10.4253/wjge.v11.i2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Attwell A.R., Patel S., Kahaleh M., et al. ERCP with per-oral pancreatoscopy-guided laser lithotripsy for calcific chronic pancreatitis: a multicenter U.S. experience. Gastrointest Endosc. 2015;82:311–318. doi: 10.1016/j.gie.2015.01.020. [DOI] [PubMed] [Google Scholar]
- 6.Elmunzer B.J., Forster E., Moran R.A., et al. Advanced techniques for pancreaticobiliary stone extraction. VideoGIE. 2020;5:324–325. doi: 10.1016/j.vgie.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mittal C., Shah R.J. Pancreatoscopy-guided laser dissection and ablation for treatment of benign and neoplastic pancreatic disorders: an initial report (with videos) Gastrointest Endosc. 2019;89:384–389. doi: 10.1016/j.gie.2018.08.045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The case report is presented in the video, with a description of the patient’s clinical course along with a set of endoscopic interventions including the use of per-oral pancreatoscopy with holmium laser therapy for stricturoplasty and stone fragmentation.
The case report is presented in the video, with a description of the patient’s clinical course along with a set of endoscopic interventions including the use of per-oral pancreatoscopy with holmium laser therapy for stricturoplasty and stone fragmentation.