Abstract
Objective
This study aimed to assess the impact of the COVID‐19 pandemic on the efficacy of an intensive treatment based on enhanced cognitive behavioral therapy (CBT‐E) in patients with anorexia nervosa.
Methods
This cohort study analyzed 57 patients with anorexia nervosa who experienced the COVID‐19 pandemic during intensive CBT‐E, comparing their outcomes (body mass index [BMI], eating‐disorder and general psychopathology, and clinical impairment) with those of patients with anorexia nervosa matched by gender, age, and BMI given the same treatment before the COVID‐19 outbreak as controls. Patients were assessed at baseline, at the end of treatment and after 20 weeks of follow‐up.
Results
More than 75% of patients during the pandemic versus 85% of controls completed the treatment, a difference that was not significant. BMI, eating disorder and general psychopathology and clinical impairment scores improved significantly from baseline to 20‐week follow‐up in both groups. However, the improvement was more marked in controls than in those treated during the COVID‐19 pandemic.
Conclusion
Patients with anorexia nervosa given intensive CBT‐E during the COVID‐19 pandemic had significantly improved psychopathology, albeit to a lesser extent than patients given the same treatment before the COVID‐19 pandemic.
Public significance statement
In this study, the outcome of 57 patients with anorexia treated with intensive enhanced cognitive behavior therapy during the COVID‐19 pandemic was compared with a matched group treated before the pandemic hit. The rate of remission from anorexia nervosa was similar between the two groups. However, patients exposed to the COVID‐19 pandemic showed lesser improvement than those not exposed.
Keywords: anorexia nervosa; cognitive behavioral therapy; COVID‐19, pandemic; isolation; lockdown; treatment outcomes
1. INTRODUCTION
The coronavirus disease (COVID‐19) pandemic that swept across the world after the initial outbreak in 2019 caused most governments to adopt several measures to counter its spread. These included periods of “lockdown,” with people being required to stay at home, as well as travel restrictions, closure of schools, shops, restaurants, bars and gyms, and other related practices such as social distancing, mask wearing, quarantine periods and “shielding.” However, the social and physical distancing measures introduced due to concerns about the potentially severe complications of COVID‐19 infection have exposed people to several stressors. Some of these (increase in social isolation, life disruption and restrictions on movement and daily activities, not to mention compromised relationships with family and friends, and greater exposure to weight‐related social media messaging) have been proposed as potential factors explaining both the worsening of eating‐disorder and general psychopathology observed in people with eating disorders (Dalle Grave, 2020; Devoe et al., 2022; Monteleone et al., 2021; Rodgers et al., 2020) and the increased incidence of eating disorders recorded during the COVID‐19 pandemic (Taquet et al., 2021). Indeed, since the outbreak began, records show that there has been a noticeable increase in acute and routine referrals (Richardson et al., 2020) and inpatient admissions for eating disorders, particularly in adolescents (Haripersad et al., 2021; Lin et al., 2021; Solmi et al., 2021).
Unfortunately, due to the same restrictions, psychological and psychiatric treatment services have also been under pressure, often being provided remotely (Murphy et al., 2020). Furthermore, even when in‐person delivery was possible, the quality could have been negatively influenced by the fear of infection, the use of personal protection equipment, and the mandatory social distancing and disinfection procedures (Colleluori et al., 2021).
Although these modifications to treatment implementation, alongside the other stressors associated with the observed worsening in eating‐disorder and general psychopathology scores in patients with eating disorders, are likely to have negatively influenced treatment outcomes, only very few studies have investigated this issue to date. One longitudinal study, based on an online survey, assessed the short‐term effects of COVID‐19 lockdown in a cohort of patients who started treatment for an eating disorder between January and September 2019 (Castellini et al., 2020), that is, before precautionary measures were introduced. The study showed that the ensuing lockdown negatively interfered with the recovery process, with patients with bulimia nervosa exhibiting exacerbated binge eating and compensatory physical exercise, and an interruption in the diminishing trend of eating‐disorder psychopathology expected in patients undergoing treatment. In contrast, patients with anorexia nervosa did show improvements in eating‐disorder psychopathology and weight gain.
Another study assessed a transdiagnostic sample of patients being treated for eating disorders in‐person before February 2020 versus virtually between April 2020 and May 2021 (Steiger et al., 2021) using a combination of procedures (weekly group therapy, bimonthly individual therapy and, when indicated, adjunctive nutritional, and pharmacological consultations). Patients in both groups showed similar improvements in eating‐disorder symptoms, as well as weight gain (if indicated) and satisfaction with services. However, the two samples were not matched, and the lack of follow‐up data prevents us understanding whether the clinical improvement achieved by virtual treatment is maintained in the long‐term.
Since the COVID‐19 pandemic is not yet over, more data on the effect of this global emergency on the treatment of patients with eating disorders is needed, with a view to determining whether it is necessary to design specific strategies and procedures to help patients during such difficult periods. With this in mind, this study was designed to assess the impact of the COVID‐19 pandemic on treatment outcomes in patients with severe anorexia nervosa treated with intensive enhanced cognitive behavioral therapy for eating disorders (CBT‐E), involving a phase of treatment in an inpatient setting followed by day hospital, during the COVID‐19 pandemic. For this purpose, end‐of‐treatment and 20‐week follow‐up outcomes of patients with anorexia nervosa exposed to the COVID‐19 pandemic were compared with those recorded for a group of patients with anorexia nervosa matched by gender, age and body mass index (BMI) who had completed the same treatment at least 6 months before pandemic restrictions were introduced.
2. MATERIALS AND METHODS
2.1. Study design and participants
This cohort study was conducted on a sample of consecutively admitted patients with anorexia nervosa treated at the Villa Garda Hospital Department of Eating and Weight Disorders, Italy (Figure 1). All participants were aged between 16 and 60 years, were deemed to meet the Diagnostic and Statistical Manual of Mental Disorders, edition 5 (American Psychiatric Association, 2013), diagnostic criteria for anorexia nervosa by an eating disorder specialist, and had had at least one previous outpatient treatment for anorexia nervosa that failed due to either weight loss or insufficient weight gain after at least 8 weeks of treatment. Unfortunately, no data on these previous treatments are available, but most were multidisciplinary and CBT‐based. Acute psychotic disorder or concomitant substance use disorder were grounds for exclusion.
FIGURE 1.
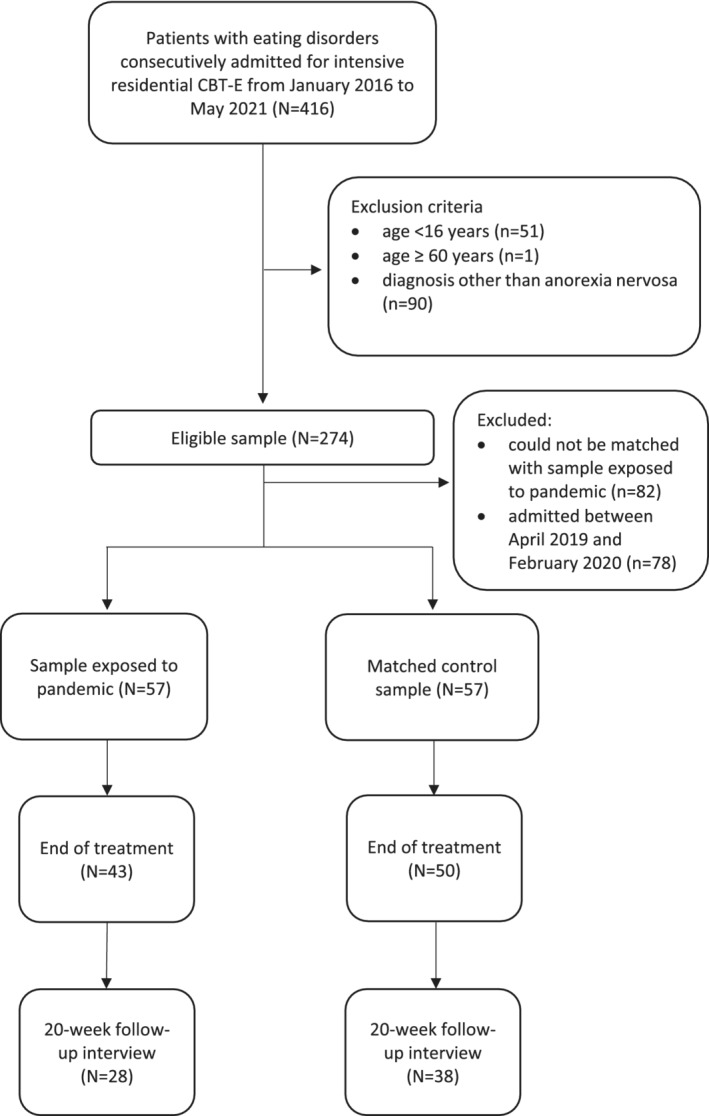
Flow‐chart
The treatment offered to eligible participants was an intensive stepped‐care CBT‐E program that involves 13 weeks of treatment in an inpatient setting followed by 7 weeks in day hospital. Outcome measures were assessed at baseline, at the end of the 20‐week treatment period, and again at 20‐week follow‐up.
The study group, that is, those treated during the COVID‐19 pandemic, were admitted from March 9, 2020 to April 2021, spanning the national lockdown and continuing restrictions in Italy. These were matched by gender, age (±2 years) and BMI (±2 kg/m2) to a control group, retrospectively recruited from patients treated between January 2016 and April 2019, before the pandemic hit. All study and control group participants (and the parent(s) and/or legal guardian(s) of those under 18 years of age) provided informed written consent for the collection and anonymous processing of their clinical data in a service‐level research setting. As all treatment and assessment procedures were performed as part of routine clinical practice rather than purely for the purposes of research, no ethical clearance was sought for the study, in accordance with Italian National Health System ethics guidelines.
2.2. Intensive CBT‐E
The treatment program, derived from outpatient CBT‐E, has been described in previous publications (Dalle Grave, 2012; Dalle Grave et al., 2013; Dalle Grave et al., 2020). Patients are admitted voluntarily after attending 3–4 introduction and preparation sessions. During the inpatient phase, patients attend individual and group sessions in which a psychologist delivers CBT‐E strategies and procedures (including those designed to promote weight gain), and are assisted with eating by a CBT‐E‐trained dietician until their BMI reaches ≥18.5. Throughout the program, the patients' physical health is overseen and managed by CBT‐E‐trained physicians and nurses, respectively, and individual and group sessions are continued into the day‐hospital phase, when the focus shifts to averting and managing potential setbacks.
Even during the inpatient phase, the patients are free to come and go, so that they can learn under expert supervision how to handle the environmental stimuli likely to exacerbate their eating‐disorder psychopathology. The treatment is the same for adults and adolescents, except that adolescents receive lessons from accredited teachers so as not to interrupt their schooling, and the involvement of significant others is greater. Near the end of the treatment, patients are asked to grant permission for their parents (or spouse etc., if adult) to be invited to attend several joint sessions. The primary aim of these sessions is to train the significant others to be “treatment facilitators,” and to help the family unit create a positive, stress‐free home in readiness for their return.
CBT‐E involves the above strategies with a view to reducing the high rate of relapse that is typically seen after hospital discharge. However, once the national lockdown was introduced on March 9, 2020, although no variation in recruitment occurred, patients were no longer able to leave the unit, including going in the unit garden during the inpatient phase, and relatives were no longer allowed to visit. Furthermore, all individual and group sessions in the day‐hospital phase had to be delivered remotely. Even core strategies of CBT‐E such as collaborative weighing and assisted eating had to be delivered online, a practice that continued until May 3, 2020, in the day‐hospital phase, when the national lockdown was lifted. However, some restrictions in the inpatient phase persisted after May 3, 2020 (e.g., being allowed to stay in the unit garden but not leave the hospital and receive visits by relatives).
Thus, the test and control groups received a form of treatment that was theoretically the same, but differed greatly in its delivery.
After the 20‐week program, completers were offered 20 sessions of post‐inpatient outpatient CBT‐E sessions during follow up, as is routine in our unit, in which every treatment “step,” from inpatient to outpatient, is delivered by a unified team of healthcare workers all officially trained in CBT‐E. The focus of the postinpatient outpatient step is developing relapse‐prevention skills and addressing residual eating‐disorder features using CBT‐E strategies and procedures. Whereas the control group attended these sessions in‐person, the study group received them online.
2.3. Assessment
The following validated outcome measures were assessed in both groups at admission (baseline), the end of the 20 weeks of treatment (EOT), and during a follow‐up session after 20 weeks:
Body weight and BMI: To calculate the BMI, the body weight, measured on a beam‐balance scale, was divided by the square of the height, measured on a wall‐mounted stadiometer.
Eating‐disorder psychopathology: Patients were scored on the Eating Disorder Examination Questionnaire (EDE‐Q, 6th edition, Italian version) (Calugi et al., 2017). The internal consistency in our sample was 0.95.
General psychopathology: The Italian version of the Brief Symptom Inventory (BSI) was used (de Leo et al., 1993). The internal consistency in our sample was 0.97.
Clinical Impairment: Patients were scored on the Italian version of the Clinical Impairment Assessment (CIA) (Calugi et al., 2018). The internal consistency in our sample was 0.93.
2.4. Outcome categories
Patients who reached a BMI ≥ 18.5 kg/m2 (Cole et al., 2007), considered the lowest threshold in a healthy BMI range (World Health Organization, 2000), at EOT and/or follow‐up, were classed as having a “good BMI outcome,” and those who also had a global EDE‐Q score of <1 SD above the community mean (i.e., <2.77) (Mond et al., 2006) were described as having a “full response”; this simple and replicable method indicates an excellent outcome (Bardone‐Cone et al. (2010).
2.5. Statistical analysis
All statistical analyses were carried out using SPSS software (IBM SPSS Statistics, version 27.0). Descriptive statistics are reported as either mean and SD (continuous variables) or percentage (categorical variables). After testing for normality, the independent samples t‐test or Mann–Whitney U test, as appropriate, were applied to continuous variables, and the chi‐squared test to dichotomous variables; in this way the clinical and demographic variables describing patients whose treatment and recovery was subject to interference by COVID‐19 prevention measures (study group) were compared with those of controls, whose treatment and follow‐up was completed before the pandemic.
Repeated‐measures analysis of variance (RMANOVA) was applied to the changes in BMI, eating‐disorder and general psychopathology, and clinical impairment scores from baseline to EOT and 20‐week follow‐up for both completers and intention‐to‐treat in both groups. For intention‐to‐treat analysis, EOT and follow‐up data was processed using a multiple‐imputation procedure with the fully conditional specification method. The homogeneity of variance assumption was tested using Mauchly's sphericity test. The percentage of missing data was 21.1% at the end of treatment and 42.1% at the 20‐week follow‐up for BMI and EDE‐Q, BSI, CIA global scores. The missing data were completely at random (Little's MCAR test: chi‐square = 43.9, df = 36, p = .172). Finally, we have used the propensity score as a confounding variable in RMANOVA. The variables included in the propensity score were age, gender, and baseline BMI, EDE‐Q, BSI, CIA global scores.
p value was set to .05.
3. RESULTS
The demographic and clinical features of both groups are presented in Table 1. The great majority of test and control patients were females, with a BMI of around 15 kg/m2, and the mean age of both groups was roughly 26 years. Comparison of the two groups indicated that they had similar mean age and BMI, and identical gender distribution, and that there were no significant differences in baseline eating‐disorder psychopathology or behavior scores. However, patients admitted during the pandemic had lower baseline general psychopathology scores on average than those recorded in control patients.
TABLE 1.
Demographic and clinical characteristics of 57 patients with anorexia nervosa and 57 gender‐, age‐ and body mass index‐matched controls treated during and before the COVID‐19 pandemic, respectively
| Patients exposed to pandemic (n = 57) | Controls (n = 57) | t‐test, Mann–Whitney test or chi‐squared test | p value | |
|---|---|---|---|---|
| Gender, % females | 53 (93.0%) | 53 (93.0%) | — | — |
| Age, years | 26.4 (10.3) | 25.6 (10.1) | Z = 0.64 | .525 |
| Body Mass Index, kg/m2 | 15.0 (2.1) | 14.8 (2.0) | t = 0.69 | .492 |
| EDE‐Q global score | 4.0 (1.2) | 4.1 (1.3) | Z = 0.69 | .488 |
| EDE‐Q objective binge‐eating episodes, mean (SD), if present | 16.9 (16.7) | 15.7 (22.6) | Z = 0.83 | .407 |
| EDE‐Q self‐induced vomiting, mean (SD), if present | 19.2 (18.7) | 27.6 (33.3) | Z = 0.30 | .761 |
| EDE‐Q laxative misuse, mean (SD), if present | 4.9 (4.5) | 15.6 (18.5) | Z = 1.36 | .174 |
| EDE‐Q excessive exercise, mean (SD), if present | 21.2 (21.4) | 20.1 (10.4) | Z = 0.98 | .327 |
| CIA global score | 34.6 (11.8) | 37.8 (8.5) | Z = 1.09 | .277 |
| BSI global score | 1.89 (0.8) | 2.25 (0.7) | t = 2.44 | .016 |
Note: Data are presented as mean (SD) or as number (%).
Abbreviations: BSI, brief symptom inventory; EDE‐Q, Eating Disorder Examination Questionnaire; CIA, clinical impairment assessment.
3.1. Follow‐up completion
Forty‐three study participants (75.4%) and 50 controls (87.7%) completed the intensive CBT‐E program (chi squared = 2.86, df = 1, p = .091). There were no significantly different baseline characteristics between completers and non‐completers in either group. Among completers, 28 (65.1%) from the study group and 38 (76.0%) from the control group attended the follow‐up interview and assessment session at 20 weeks (chi squared = 1.32, df = 1, p = .249).
About 94% of participants (study group, n = 27, 96.4%; controls, n = 34, 89.5%) received some form of treatment following the program (chi squared = 0.61, df = 1, p = .345). In 92.6% of study group patients and 89.6% of controls, this was a 20‐week CBT‐E‐based treatment delivered by trained therapists living close to their place of residence (chi squared = 0.01, df = 1, p = .913).
3.2. Response to treatment
Table 2 shows BMI, eating‐disorder and general psychopathology and clinical impairment at each time point, using completer and intention‐to‐treat analysis. Among completers, RMANOVA controlled for the propensity score, indicated a significant change over time in all measured variables, and a significant difference between groups in all except for BMI (Figure 2). Moreover, a significant TimeXGroup interaction was found in EDE‐Q, BSI and CIA global scores. Contrast analysis indicated that all variables improved significantly from baseline to EOT (all ps < 0.001) but remained stable from EOT to 20‐week follow‐up. Moreover, the two groups showed different trends from baseline to EOT in BSI and CIA global scores (ps <0.01).
TABLE 2.
Body mass index (BMI) in kg/m2, eating disorder examination questionnaire (EDE‐Q), clinical impairment assessment (CIA), and brief symptom inventory (BSI) in patients with anorexia nervosa treated during and before (controls) the COVID‐19 pandemic
| Completer analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | End of treatment | 20‐week follow‐up | |||||||
| Mean and SD | Patients exposed to pandemic (n = 43) | Controls (n = 50) | Patients exposed to pandemic (n = 43) | Controls (n = 50) | Patients exposed to pandemic (n = 28) | Controls (n = 38) | Repeated measures ANOVA | ||
| Time; partial eta squared | Time X group; partial eta squared | Group; partial eta squared | |||||||
| BMI | 15.0 (1.9) | 14.8 (2.0) | 19.9 (1.1) | 19.8 (1.3) | 18.8 (2.5) | 19.4 (1.8) | 40.35b; 0.390 | 1.53; 0.024 | 0.22; 0.004 |
| EDE‐Q global score | 3.9 (1.2) | 4.1 (1.3) | 2.2 (1.1) | 1.9 (1.3) | 2.3 (1.4) | 1.2 (1.1) | 8.18b; 0.118 | 3.76a; 0.058 | 8.39a; 0.121 |
| CIA global score | 33.9 (11.7) | 37.3 (8.7) | 18.9 (10.8) | 15.6 (12.3) | 21.9 (13.2) | 10.9 (10.6) | 23.54b; 0.278 | 7.44b; 0.109 | 14.57b; 0.193 |
| BSI global score | 1.9 (0.8) | 2.3 (0.7) | 1.1 (0.8) | 1.1 (0.7) | 1.3 (0.8) | 0.8 (0.7) | 51.71b; 0.459 | 5.98b; 0.089 | 10.09b; 0.142 |
| N (%) | Chi‐squared test; p value end of treatment | Chi‐squared test; p value 20‐week follow‐up | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI ≥ 18.5 | — | — | 40 (93.0%) | 46 (92.0%) | 17 (60.7%) | 26 (68.4%) | 0.03; .852 | 0.42; .516 |
| BMI ≥ 18.5 and EDE‐Q global score <2.77 | — | — | 23 (53.5%) | 35 (70.0%) | 15 (53.6%) | 25 (65.8%) | 1.51; .218 | 1.01; .315 |
| Intention‐to‐treat analysis–multiple imputation procedure | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | End of treatment | 20‐week follow‐up | Repeated‐measures ANOVA | ||||||
| Mean and SE | Patients exposed to pandemic (n = 57) | Control patients (n = 57) | Patients exposed to pandemic (n = 57) | Control patients (n = 57) | Patients exposed to pandemic (n = 57) | Control patients (n = 57) | Time; partial eta squared | Time X Group; partial eta squared | Group; partial eta squared |
| BMI | 15.0 (0.3) | 14.8 (0.2) | 19.8 (0.2) | 19.7 (0.2) | 18.5 (0.5) | 19.5 (0.5) | 146.3b; 0.191 | 9.29b; 0.015 | 2.87; 0.005 |
| EDE‐Q global score | 4.0 (0.2) | 4.1 (0.1) | 2.1 (0.1) | 1.9 (0.2) | 2.1 (0.2) | 1.4 (0.2) | 82.49b; 0.118 | 23.56b; 0.037 | 34.48b; 0.053 |
| CIA global score | 34.6 (1.6) | 37.8 (1.1) | 18.3 (1.5) | 16.2 (1.8) | 18.8 (2.2) | 13.2 (2.0) | 152.33b; 0.199 | 26.10b | 38.21b; 0.058 |
| BSI global score | 1.89 (0.1) | 2.25 (0.1) | 1.1 (0.1) | 1.1 (0.1) | 1.1 (0.1) | 0.8 (0.1) | 309.87b; 0.335 | 21.61b; 0.034 | 27.33b; 0.042 |
| N (%) | Chi‐squared test; p value end of treatment | Chi‐squared test; p value 20‐week follow‐up | ||||||
|---|---|---|---|---|---|---|---|---|
| BMI ≥18.5, | — | — | 52 (91.2%) | 52 (91.2%) | 38 (66.7%) | 31 (54.4%) | 1.00; — | 1.80; .180 |
| BMI ≥18.5 and EDE‐Q global score <2.77 | — | — | 35 (61.4%) | 39 (68.4%) | 29 (50.9%) | 37 (64.9%) | 0.62; .432 | 2.30; .129 |
Note: Data from completer and intention‐to‐treat analysis. The propensity score was used as a confounding variable. a p < .01 and b p < .001.
FIGURE 2.
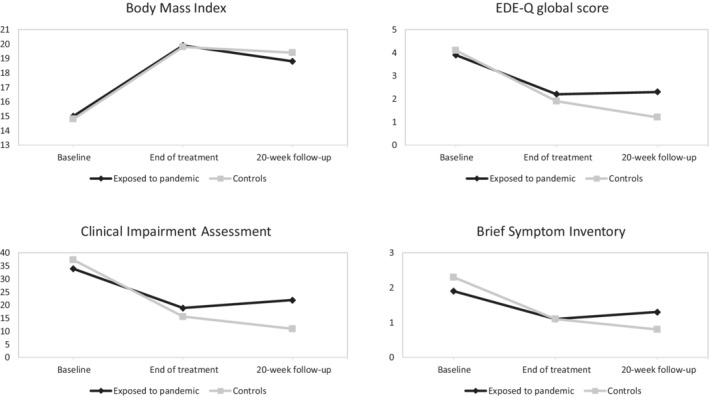
Observed mean percentage change from baseline to end of treatment and 20‐week follow‐up in body mass index (BMI), eating disorder examination questionnaire (EDE‐Q), clinical impairment assessment (CIA) and brief symptom inventory (BSI) scores in completers patients with anorexia nervosa treated during versus before the COVID‐19 pandemic.
Intention‐to‐treat analysis results displayed a similar pattern, with Time, TimeXGroup and Group (except for BMI), all being significant, indicating that there were significant differences between changes in the two groups' eating‐disorder and general psychopathology and clinical impairment scores over time (see Table 2). However, the two groups showed similar “good BMI outcome” and “full response” rates at both EOT and follow‐up.
4. DISCUSSION
This study, which aimed to evaluate the potential impact of COVID‐19 restrictions on the effectiveness of intensive CBT‐E in patients with anorexia nervosa, as measured at EOT and 20‐week follow‐up, yielded three main findings. The first concerns the data collected at admission. At baseline, patients admitted during the COVID‐19 pandemic and controls treated before had comparable BMI, eating‐disorder psychopathology and behaviors and clinical impairment. However, baseline general psychopathology scores were lower, that is, better, in patients exposed to the COVID‐19 pandemic. A recent systemic review, of 13 studies with a total of 7848 participants, on changes in eating‐disorder symptoms and associated psychological health issues during the COVID‐19 pandemic, indicated that the pandemic itself and the related social restrictions detrimentally impacted the mental health of the majority of individuals with eating disorders (Haghshomar et al., 2022). In our case, the difference in eating disorder psychopathology was not significant, but this could be due to the patient selection criteria. Indeed, all patients admitted for intensive CBT‐E have severe baseline psychopathology, making it more difficult to observe differences between the two groups.
Our second finding concerns the drop‐out rate. A similar percentage of patients from the two groups completed the intensive treatment, indicating that the COVID‐19 pandemic did not affect the completion rate of the treatment, even though remote workarounds had to be found for delivering fundamental CBT‐E strategies and procedures to test participants.
The third finding is that treatment was largely successful in both groups, although there were significant differences between outcomes. One the one hand, it is encouraging to note that both groups achieved a substantial and healthy increase in body weight, reaching and maintaining a mean BMI equal to or higher than 18.5. Good BMI outcome and full response rates were similar, and both groups showed significant improvements in eating‐disorder psychopathology, clinical impairment, and general psychopathology from baseline to 20‐week follow‐up. However, on the other hand, between‐group comparison indicated that this improvement was significantly lower in patients who underwent treatment during the COVID‐19 pandemic. Considering the similarity in baseline characteristics between the two groups, it is likely that such differences in outcome may be at least partially due to the dramatic changes imposed by the pandemic restrictions on some key treatment procedures. First and foremost, the traditionally “open” inpatient unit was forced to become “closed,” with patients being unable leave the ward or see other people, likely increasing their stress levels and sense of isolation. Secondly, several key CBT‐E procedures involve real‐world practice in order to increase dietary flexibility (i.e., social eating) and improve body image (i.e., body exposition), for example (Dalle Grave et al., 2008), and could not be implemented during the pandemic limiting the effectiveness of treatment. Thirdly, all CBT‐E procedures had to be administered remotely during the day‐hospital phase in the national lockdown period, which could also have interfered with the treatment's efficacy. However, it is also possible that the lesser improvement observed in patients treated during lockdown may be the consequence of the general psychological distress associated with the COVID‐19 pandemic (Lahav, 2020).
The study presents certain limitations. Firstly, we did not assess variables specifically related to the pandemic that could offer more information explaining patients' conditions during this period. Secondly, the two cohorts differed in terms of historical context. However, the same therapists delivered the treatment based on the same theory and used the same strategies and procedures. Thirdly, only 65% of treatment completers in the pandemic cohort and 76% in the prepandemic cohort were interviewed at follow‐up. Finally, the intensive setting makes extending the results to the normal outpatient setting difficult. However, to our knowledge, this is the first study comparing patients with anorexia nervosa exposed to a pandemic with gender‐, age‐ and BMI‐matched patients who received the same treatment. This design is the best source of reliable data on the impact of the COVID‐19 pandemic on treatment for eating‐disorder psychopathology. Moreover, the treatment investigated is evidence‐based, and was delivered in a real‐world setting, including a 20‐week follow‐up period to enable assessment of its longer‐term effects.
Future studies with a robust study design should evaluate the longer‐term impact of the COVID‐19 pandemic not only in patients with anorexia nervosa but also with other eating disorders. It will be also useful to collect patients' qualitative reports of treatment under COVID‐19 conditions to achieve a better insight into the factors that contribute to different outcomes. Meanwhile, the results of this study seem to indicate that intensive CBT‐E, designed to address eating‐disorder psychopathology, yields good outcomes in patients with severe anorexia nervosa, even in the adverse conditions of the COVID‐19 pandemic, although outcomes are better when it is conducted under normal circumstances. More than 75% of patients seen during the pandemic completed the treatment, and most improved substantially, with more than 60% achieving a good BMI outcome and about 55% a full response at 20‐week follow‐up.
AUTHOR CONTRIBUTIONS
Riccardo Dalle Grave: Conceptualization; project administration; supervision; writing – original draft; writing – review and editing. Anna Dalle Grave: Data curation; writing – review and editing. Elena Bani: Data curation; writing – review and editing. Alessandra Oliosi: Data curation; writing – review and editing. Maddalena Conti: Data curation; writing – review and editing. Laura Dametti: Data curation; writing – review and editing. Simona Calugi: Conceptualization; formal analysis; methodology; writing – original draft; writing – review and editing.
FUNDING INFORMATION
The authors have no source funding from any organization or entity with a financial interest in or a financial conflict with the subject matter or materials discussed in the manuscript.
CONFLICT OF INTEREST
The authors declares there is no potential conflicts of interest.
Dalle Grave, R. , Dalle Grave, A. , Bani, E. , Oliosi, A. , Conti, M. , Dametti, L. , & Calugi, S. (2022). The impact of the COVID‐19 pandemic on intensive cognitive behavioral therapy outcomes in patients with anorexia nervosa—A cohort study. International Journal of Eating Disorders, 1–9. 10.1002/eat.23765
Action Editor: Tracey Wade
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
REFERENCES
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders, (DSM‐5). American Psychiatric Publishing. [Google Scholar]
- Bardone‐Cone, A. M. , Harney, M. B. , Maldonado, C. R. , Lawson, M. A. , Robinson, D. P. , Smith, R. , & Tosh, A. (2010). Defining recovery from an eating disorder: Conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behaviour Research and Therapy, 48(3), 194–202. 10.1016/j.brat.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calugi, S. , Milanese, C. , Sartirana, M. , El Ghoch, M. , Sartori, F. , Geccherle, E. , Coppini, A., Franchini, C., & Dalle Grave, R. (2017). The eating disorder examination questionnaire: Reliability and validity of the Italian version. Eating and Weight Disorders, 22(3), 509–514. 10.1007/s40519-016-0276-6 [DOI] [PubMed] [Google Scholar]
- Calugi, S. , Sartirana, M. , Milanese, C. , el Ghoch, M. , Riolfi, F. , & Dalle Grave, R. (2018). The clinical impairment assessment questionnaire: Validation in Italian patients with eating disorders. Eating and Weight Disorders, 23(5), 685–694. 10.1007/s40519-018-0477-2 [DOI] [PubMed] [Google Scholar]
- Castellini, G. , Cassioli, E. , Rossi, E. , Innocenti, M. , Gironi, V. , Sanfilippo, G. , Felciai, F., Monteleone, A. M., & Ricca, V. (2020). The impact of COVID‐19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. International Journal of Eating Disorders, 53(11), 1855–1862. 10.1002/eat.23368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole, T. J. , Flegal, K. M. , Nicholls, D. , & Jackson, A. A. (2007). Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ, 335(7612), 194. 10.1136/bmj.39238.399444.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colleluori, G. , Goria, I. , Zillanti, C. , Marucci, S. , & Dalla Ragione, L. (2021). Eating disorders during COVID‐19 pandemic: The experience of Italian healthcare providers. Eating and Weight Disorders, 26(8), 2787–2793. 10.1007/s40519-021-01116-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalle Grave, R. (2012). Intensive cognitive behavior therapy for eating disorders. Nova. [Google Scholar]
- Dalle Grave, R. (2020). Coronavirus Disease 2019 and Eating Disorders https://www.psychologytoday.com/intl/blog/eating-disorders-the-facts/202003/coronavirus-disease-2019-and-eating-disorders
- Dalle Grave, R. , Bohn, K. , Hawker, D. , & Fairburn, C. G. (2008). Inpatient, day patient and two forms of outpatient CBT‐E. In Fairburn C. G. (Ed.), Cognitive behavior therapy and eating disorders (pp. 231–244). Guilford Press. [Google Scholar]
- Dalle Grave, R. , Calugi, S. , Conti, M. , Doll, H. , & Fairburn, C. G. (2013). Inpatient cognitive behaviour therapy for anorexia nervosa: A randomized controlled trial. Psychotherapy and Psychosomatics, 82(6), 390–398. 10.1159/000350058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalle Grave, R. , Conti, M. , & Calugi, S. (2020). Effectiveness of intensive cognitive behavioral therapy in adolescents and adults with anorexia nervosa. International Journal of Eating Disorders, 53(9), 1428–1438. 10.1002/eat.23337 [DOI] [PubMed] [Google Scholar]
- de Leo, D. , Frisoni, G. B. , Rozzini, R. , & Trabucchi, M. (1993). Italian community norms for the brief symptom inventory in the elderly. British Journal of Clinical Psychology, 32(2), 209–213. 10.1111/j.2044-8260.1993.tb01045.x [DOI] [PubMed] [Google Scholar]
- Devoe, D. J. , Han, A. , Anderson, A. , Katzman, D. K. , Patten, S. B. , Soumbasis, A. , Flanagan, F., Paslakis, G., Vyver, E., Marcoux, G., & Dimitropoulos, G. (2022). The impact of the COVID‐19 pandemic on eating disorders: A systematic review. International Journal of Eating Disorders. 10.1002/eat.23704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haghshomar, M. , Shobeiri, P. , Brand, S. , Rossell, S. L. , Akhavan Malayeri, A. , & Rezaei, N. (2022). Changes of symptoms of eating disorders (ED) and their related psychological health issues during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Eating Disorders, 10(1), 51. 10.1186/s40337-022-00550-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haripersad, Y. V. , Kannegiesser‐Bailey, M. , Morton, K. , Skeldon, S. , Shipton, N. , Edwards, K. , Newton, R., Newell, A., Stevenson, P. G., & Martin, A. C. (2021). Outbreak of anorexia nervosa admissions during the COVID‐19 pandemic. Archives of Disease in Childhood, 106(3), e15. 10.1136/archdischild-2020-319868 [DOI] [PubMed] [Google Scholar]
- Lahav, Y. (2020). Psychological distress related to COVID‐19 ‐ the contribution of continuous traumatic stress. Journal of Affective Disorders, 277, 129–137. 10.1016/j.jad.2020.07.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, J. A. , Hartman‐Munick, S. M. , Kells, M. R. , Milliren, C. E. , Slater, W. A. , Woods, E. R. , Forman, S. F., & Richmond, T. K. (2021). The impact of the COVID‐19 pandemic on the number of adolescents/young adults seeking eating disorder‐related care. Journal of Adolescent Health, 69(4), 660–663. 10.1016/j.jadohealth.2021.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond, J. M. , Hay, P. J. , Rodgers, B. , … Owen, C. (2006). Eating disorder examination questionnaire (EDE‐Q): Norms for young adult women. Behaviour Research and Therapy, 44(1), 53–62. 10.1016/j.brat.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Monteleone, A. M. , Cascino, G. , Marciello, F. , Abbate‐Daga, G. , Baiano, M. , Balestrieri, M. , Barone, E., Bertelli, S., Carpiniello, B., Castellini, G., Corrivetti, G., De Giorgi, S., Favaro, A., Gramaglia, C., Marzolo, E., Meneguzzo, P., Monaco, F., Oriani, M. G., … Monteleone, P. (2021). Risk and resilience factors for specific and general psychopathology worsening in people with eating disorders during COVID‐19 pandemic: A retrospective Italian multicentre study. Eating and Weight Disorders, 26(8), 2443–2452. 10.1007/s40519-020-01097-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, R. , Calugi, S. , Cooper, Z. , & Dalle Grave, R. (2020). Challenges and opportunities for enhanced cognitive behaviour therapy (CBT‐E) in light of COVID‐19. The Cognitive Behaviour Therapist, 13, e14. 10.1017/s1754470x20000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson, C. , Patton, M. , Phillips, S. , & Paslakis, G. (2020). The impact of the COVID‐19 pandemic on help‐seeking behaviors in individuals suffering from eating disorders and their caregivers. General Hospital Psychiatry, 67, 136–140. 10.1016/j.genhosppsych.2020.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers, R. F. , Lombardo, C. , Cerolini, S. , Franko, D. L. , Omori, M. , Fuller‐Tyszkiewicz, M. , Linardon, J., Courtet, P., & Guillaume, S. (2020). The impact of the COVID‐19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi, F. , Downs, J. L. , & Nicholls, D. E. (2021). COVID‐19 and eating disorders in young people. Lancet Child Adolesc Health, 5(5), 316–318. 10.1016/s2352-4642(21)00094-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger, H. , Booij, L. , Crescenzi, O. , Oliverio, S. , Singer, I. , Thaler, L. , St‐Hilaire, A., & Israel, M. (2021). In‐person versus virtual therapy in outpatient eating‐disorder treatment: A COVID‐19 inspired study. International Journal of Eating Disorders., 55, 145–150. 10.1002/eat.23655 [DOI] [PubMed] [Google Scholar]
- Taquet, M. , Geddes, J. R. , Luciano, S. , & Harrison, P. J. (2021). Incidence and outcomes of eating disorders during the COVID‐19 pandemic. The British Journal of Psychiatry, 1‐3, 262–264. 10.1192/bjp.2021.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2000). Obesity: Preventing and managing the global epidemic: Report of a WHO consultation. WHO Technical Report Series, 894, i‐xii, 1–253. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.


