SUMMARY
Insomnia and circadian dysregulation during adolescence represent important risk factors for emotional and psychological problems. Recent studies have shown that the coronavirus disease 2019 (COVID‐19) pandemic has been linked to a high prevalence of behavioural sleep problems in the general population. This study aimed to provide two pictures of two different time points of the pandemic regarding the prevalence of sleep problems in adolescents and their association with psychological health variables. Two different independent large samples of Italian adolescents aged 13–17 years were recruited at two pandemic time points. A total of 1,146 adolescents at Time 1 (T1; April 2020) and 1,406 at Time 2 (T2; April 2021) took part in the study. Measures of insomnia symptoms, sleep hygiene, chronotype, psychological distress and emotion regulation were collected. Prevalence of insomnia was 12.13% at T1 and 23.19% at T2. Furthermore, high levels of poor sleep habits (late bedtime, poor sleep hygiene, use of electronic devices at bedtime) were also detected at both time points. Insomnia symptoms strongly correlated with poor sleep hygiene, higher psychological distress, and emotional suppression at both time points. Results highlighted an alarming picture for two large samples at two different time points of the pandemic that showed a potential negative impact of the COVID‐19 pandemic, in both the first outbreak and in the later phase of the pandemic, on sleep habits, psychological distress and insomnia symptoms in adolescents. This strongly suggests the need for monitoring these variables and their interaction in the post‐pandemic period and to develop and promote interventions for insomnia and circadian disturbances during adolescence.
Keywords: adolescents, COVID‐19, health, insomnia, psychology, sleep
INTRODUCTION
A multitude of variables can affect the quality and quantity of sleep throughout adolescence (e.g., school start times, caffeine, and use of electronic devices; Adolescent Sleep Working Group, 2014; Gradisar et al., 2013). Over recent decades, a decrease in sleep duration has been observed during adolescence worldwide (Gradisar, Gardner, & Dohnt, 2011; Hysing, Pallesen, Stormark, Lundervold, & Sivertsen, 2013). Recently it was estimated that insomnia (accordingly to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition; American Psychiatric Association, 2013) prevalence is ~18.5% in this age range (23.6% in girls and 12.5% in boys; Hysing et al., 2013). Furthermore, adolescence is a particularly vulnerable period for problems in circadian regulation (Hagenauer & Lee, 2012), presenting the most irregular sleep behaviour (Gradisar et al., 2011). Insufficient sleep has been associated with adverse consequences, including mood disturbances (Moore, Slane, Mindell, Burt, & Klump, 2011), other mental and physical health outcomes (Shochat, Cohen‐Zion, & Tzischinsky, 2014), increased risk of injuries (Lam & Yang, 2007), and poor school performance (Wolfson, Spaulding, Dandrow, & Baroni, 2007). Moreover, night‐time sleep affects daytime mood, emotional reactivity, and the capacity to regulate positive and negative emotions (Gruber & Cassoff, 2014). Adolescent insomnia severely impacts future health and functioning (Roberts, Roberts, & Duong, 2009). Today, more than half of adolescents from technologically advanced countries report using electronic media most evenings during the last hour before they go to bed (Gradisar et al., 2013). Cain and Gradisar (2010) propose several mechanisms through which the use of electronic media in the evening may reduce sleep duration and interfere with sleep quality: displacing other possible activities and sleep; increasing mental, emotional, or physiological arousal; and light emission of the screens of electronic media devices. Furthermore, sleep hygiene factors (e.g., appropriate sleep schedule, use of sleep‐disturbing products, and adequate sleep environment) are of utmost importance for healthy sleep in adolescence. Previous literature proposed that the relationship between sleep and psychiatric risk may be embedded in disrupted emotional processes, such as emotion regulation (Baglioni, Spiegelhalder, Lombardo, & Riemann, 2010; Harvey, Murray, Chandler, & Soehner, 2011; Palmer & Alfano, 2017). Previous research suggested that disrupted sleep increases vulnerability to anxiety and depression via emotional processes (Gregory & Sadeh, 2016; Harvey et al., 2011). The limited ability to reduce negative emotions is a transdiagnostic feature of many disorders (Gross & Jazaieri, 2014).
An external situation that could have played a crucial role in impacting adolescent insomnia and wellbeing was the pandemic situation due to coronavirus disease 2019 (COVID‐19; Altena et al., 2020). Italy was one of the first European nations to be exposed to the outbreak. The rapid growth of contagion from the first case identified in January 2020 led to implementation of strict measure in affected zones (February 2020). From March 11 the Italian Government imposed a total lockdown on the whole national territory (Phase 1) that continued until May 3 (end of Phase 2). People were forced into home confinement and movement was allowed only for documented necessities. Phase 3 started on June 11, when measures were lifted, and some activities reopened. Until then, adolescents could not go to school, play sports, have social leisure and, in many cases, meet friends. With the start of the new academic year (September 2020), school reopened, and adolescents regained some freedom to meet friends and participate in social activities. Before the end of the year, the rapid growth of the new wave of contagion forced new restrictive measures. As a consequence, on November 6, 2020, the Government implemented a system of restrictions based on the risk of transmission of the disease and the pressure on local healthcare systems. Particularly, the Italian regions were classified across three risk levels (yellow, orange, and red, ordered in terms of the severity of the restrictions). In a territory not at high risk, schools reopened and were mandated to ensure that at least 50% (for a maximum of 75%) of students had the possibility of attending lessons, while the remainder were connected via online platforms. In medium‐ and high‐risk zones, schools were closed, and learning was possible only by online lessons. These limitations had important effects on adolescents, with significant lifestyle changes and a widespread reporting of negative feelings associated with COVID‐19 (Esposito et al., 2021).
Due to this severe situation, several studies focused on the negative psychological effect of COVID‐19 in the Italian general population (e.g., Rossi et al., 2020), highlighting high rates of perceived stress, depression and anxiety symptoms, and insomnia complaints. Another large study evaluated the Italian general population, focusing on the impact of the COVID‐19 pandemic and related consequences on sleep quality and circadian rhythms (Salfi et al., 2021; Bacaro et al., 2021). These previous studies observed a high prevalence of sleep disturbances and heightened rates of delayed sleep phase. Participants rated home confinement as a factor that negatively influenced their sleep quality and habits. Furthermore, the evening chronotype was underlined as a vulnerability factor, while the morning chronotype was a protective factor for sleep quality and psychological problems. One study (Amicucci, Salfi, D'Atri, Viselli, & Ferrara, 2021) focused specifically on the Italian adolescents selecting, through the snowball technique, during the first wave of COVID‐19, 670 late adolescents aged on average 19.38 years. The results showed that during that period adolescents reported high levels of poor sleep quality, long sleep onset latency, and irregular sleep habits. Another recent study (Bruni et al., 2021) evaluated sleep patterns of Italian children and adolescents during the first wave of COVID‐19 in 2020 and the authors found similar results, with all the age groups reporting a delay in bedtime and risetime (with most of the school‐aged children and adolescents reporting going to bed after 11:00 pm). These previous studies highlighted how the pandemic situation and its restriction had a strong impact on both psychological wellbeing and sleep quality of the general population and adolescents in particular. Nevertheless, these studies focused mainly on late adolescents and provided a picture of the situation mostly in the first wave of COVID‐19. For these reasons, it is of utmost importance to understand the impact of the changes in lifestyles on sleep during the different times of the pandemic focusing on all the period of adolescence. The present study aimed at providing two snapshots of two different phases of the pandemic on two independent large samples of the Italian adolescent population at the start of COVID‐19 pandemic and after 1 year. By observing two independent large samples of adolescents in two different pandemic time points, we aimed at providing a more comprehensive picture of variables associations in different pandemic phases.
Secondly, we aimed at analysing the association of insomnia disorder with anxiety and depression symptoms, and at evaluating possible mediating factors in this relationship. Specifically, we aimed at evaluating:
Prevalence of insomnia in a large sample in Phase 1 of the pandemic.
Prevalence of insomnia in a large independent sample in Phase 2 of the pandemic.
Prevalence of all considered variables and their association with insomnia severity in the two time points.
A model evidencing the factors that are strongly associated to insomnia disorders in the two time points.
METHODS
Procedure and participants
The first time point (T1) recruitment started on April 14, 2020, and was completed on May 4, 2020, the period in which the more restrictive measures and a national lockdown was implemented. The second time point (T2) was exactly 1 year after, the recruitment started on April 12, 2021, and was completed on May 3, 2021. During T2 in Italy most of the regions were in medium‐ or high‐risk zones with restrictive measures, social distancing, and home confinement. Two independent large samples were recruited. An online survey was created on the Survey Monkey platform, an anonymous data bank and data repository commonly used in research (Fox, Murray, & Warm, 2003). At least one parent with at least one adolescent child aged 13–17 years were invited to participate. The completion of the study was voluntary and anonymous and required an average compilation time of 10 min. If participants were interested in participating, they were asked to read accurately the information about the study and to read and complete a written and informed consent form before starting the survey. Contacts of researchers were given in the information page and participants could contact them for any doubt or need.
Surveys were systematically distributed in all Italian territories by sending emails to all the regional offices of the Ministry of Education, and consequently to the mailing lists of all the schools in the area available on the Ministry of Education website. In these emails the rationale and the aims of the study were explained, furthermore, we asked for the help of the schools’ head in sending the link of the survey to all the parents of their institution.
Parents were asked to answer the general information about the family composition and then to answer some question targeting habits and eventual changes of their adolescents. After that, parents were asked a consent to let their adolescents answer some questions. Only if both parents read and completed this consent could the adolescent answer the remaining questions. No compensation for participating in the study was provided. All procedures were performed in accordance with the 1964 Helsinki Declaration and its later amendments, and the study was approved by the Ethics Committee of the University of Rome Guglielmo Marconi (Acceptance_Letter_Ethic Committee_Data_10032021).
Instruments
-
General information questionnaire for parents.
An ad hoc questionnaire was created to collect general information. The following information was collected: who was completing the questionnaire (mother, father, other); nationality; region; family composition; current insomnia in the family; past insomnia in the family; worry about the pandemic situation; positivity to the virus; parents’ perception of adolescents’ changes in sleep, eating behaviour, and use of technologies.
-
General information questionnaire for adolescents.
An ad hoc questionnaire was created to collect general information of adolescents. The following information was collected: age; gender; height; weight; attended school; actual use of remote school modality; physical activity before and after the pandemic; use of drugs; habitual sleep pattern; use of technologies before and after the pandemic.
-
Insomnia Severity Index (ISI; Bastien, Vallières, & Morin, 2001).
Participants provided answers on a 5‐point Likert scale and summing up the results of the respective seven items, ranging from zero to 28, a total score of insomnia severity during the preceding 2 weeks could be obtained. The total score is interpreted as follows: clinically irrelevant insomnia (0–7 points); subthreshold insomnia (8–14 points); moderate insomnia (15–21 points); and severe insomnia (22–28 points).
-
Sleep Hygiene Index (SHI; Bacaro, Curati, & Baglioni, 2021b).
The SHI is a 13‐item self‐administered questionnaire that evaluates sleep hygiene behaviour. The items included on the SHI were derived from the diagnostic criteria for inadequate sleep hygiene included in the International Classification of Sleep Disorders (The International Classification of Sleep Disorders: Diagnostic and Coding Manual, 1991). Participants were asked to indicate how frequently they engage in specific behaviours (“always” = 5, “frequently” = 4, “sometimes” = 3, “rarely” = 2, “never” = 1). Higher scores are indicative of poorer sleep hygiene status.
-
Morningness–Eveningness Questionnaire Reduced (MEQr; Natale, Esposito, Martoni, & Fabbri, 2006)
The MEQr included five questions: three items requested preferred time for going to bed, getting up, and the hour of the day when personal efficiency is at a maximum. Moreover, participants also had to assess the degree of tiredness within the first half hour after their awakening and to indicate which circadian type they thought they belonged to. The MEQr score was obtained by summing scores of each question and ranged from 4 to 25 points. Scores >18 identified subjects as morning types and scores <11 as evening types.
-
Emotion Regulation Questionnaire (ERQ; Gross & John, 2003).
The ERQ is a 10‐item self‐report scale assessing two individual strategies that people adopt in order to regulate their emotions: cognitive reappraisal and expressive suppression. Participants rate the how much they agree with self‐descriptive statements reflecting cognitive reappraisal or expressive suppression on a 7‐point Likert‐type scale.
-
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983).
The HADS consists of seven items rating anxiety and seven items rating depression. Each item is scored from zero to three. Anxiety and depression values are the sums of the corresponding item scores. Patients can be subsequently allocated to one of the three following categories for anxiety and depression, based on the individual sum scores: non‐case (0–7 points), borderline case (8–10 points) and definite case (≥11 points).
Statistical analysis
Collected data were analysed using Statistical Analysis System (SAS) Software 9.4 version with SAS/STAT version 14.1 (SAS Institute Inc., Cary, NC, USA) by a professional biostatistician (S.C.). Descriptive statistics were performed on demographic data and sleep parameters. Results for descriptive statistics were expressed in means ± standard deviations (SDs) for continuous variables and in absolute and relative frequencies for categorical variables. Pearson's correlations analyses were performed on the analysed variables at T1 and T2. The internal consistency of the instruments used were evaluated calculating Cronbach's α coefficient (good internal consistency was considered 0.70 > α <0.90) (Cronbach, 1951). Linear multivariable regression model was used to determine the association between several independent variables considered as predictors and severity of insomnia as outcome at both T1 and T2.
RESULTS
Cross‐sectional characteristics of the two samples
Two samples were analysed: T1 and T2 samples. In Supplemental Material Document S1 the flow chart of the two time‐points samples are documented. In Table 1 descriptive data for the two samples are summarised. Respectively T1 and T2 samples were composed of 1,146 and 1,406 participants (mean [SD] age for T1: 14.95 [1.38] years and for T2 15.68 [1.11] years).
TABLE 1.
Demographic characteristics
| Socio‐demographic variable | ||||
|---|---|---|---|---|
| Time 1 | Time 2 | |||
| Age, years | N | % | N | % |
| 13 | 214 | 18.7 | 21 | 1.49 |
| 14 | 264 | 23 | 229 | 16.29 |
| 15 | 247 | 21.6 | 357 | 25.39 |
| 16 | 203 | 17.7 | 373 | 26.53 |
| 17 | 218 | 19 | 426 | 30.3 |
| Mean (SD) | 14.95 (1.38) | 15.68 (1.11) | ||
| Gender | ||||
| Female | 637 | 55.6 | 782 | 55.62 |
| Male | 509 | 44.4 | 624 | 44.38 |
| Region | ||||
| North | 60 | 5.24 | 267 | 18.99 |
| Centre | 43 | 3.75 | 87 | 6.19 |
| South | 906 | 79.06 | 927 | 65.93 |
| Islands | 137 | 11.95 | 125 | 8.89 |
| Total, N | 1,146 | 1,406 | ||
North was composed of Lombardia, Piemonte, Veneto, Liguria, Emilia Romagna, Valle D'Aosta, Trentino Alto Adige, Friuli Venezia Giulia; Centre was composed of Lazio, Toscana, Marche, Umbria; South was composed of Abruzzo, Molise, Campania, Basilicata, Puglia, Calabria; Islands: Sicily, Sardinia.
In Table 2, the main results for psychological and sleep variables are reported for both samples. The results showed that at both time points there was a high presence of insomnia symptoms, poor sleep hygiene, and presence of evening type adolescents (categorised as explained in the instruments section) and anxiety symptoms were detected. The number of participants that went to bed late (after 11:00 p.m.) was very high at both time points and this difference was more qualitatively evident during the weekend (T1: weekdays, 54%; weekend, 78.6%; T2: weekdays, 56.54%; weekend, 82.21%). Moreover, in Supplemental Material Document S2 mean scores for the questionnaires for both time points are reported.
TABLE 2.
Psychological and sleep variables
| Categories | Time 1 | Time 2 | ||
|---|---|---|---|---|
| Circadian typology (MEQ) | N | % | N | % |
| Evening type | 134 | 11.69 | 298 | 21.19 |
| Intermediate type | 422 | 36.82 | 938 | 66.71 |
| Morning type | 152 | 13.26 | 170 | 12.09 |
| NA | 125 | 10.9 | 187 | 12.09 |
| Depression symptoms (HADS_D) | ||||
| Normal | 234 | 20.42 | 440 | 31.29 |
| Borderline | 477 | 41.62 | 546 | 38.83 |
| Clinic | 435 | 37.96 | 420 | 29.87 |
| Anxiety symptoms (HADS_A) | ||||
| Normal | 773 | 67.45 | 734 | 52.2 |
| Border | 214 | 18.67 | 245 | 17.43 |
| Clinic | 159 | 13.87 | 427 | 30.37 |
| Insomnia symptoms (ISI) | ||||
| Absence of insomnia | 690 | 60.21 | 640 | 45.52 |
| Subthreshold insomnia | 317 | 27.66 | 440 | 31.29 |
| Moderate insomnia | 117 | 10.21 | 265 | 18.85 |
| Severe insomnia | 22 | 1.92 | 61 | 4.34 |
| Bedtime week | ||||
| Before 9:00 p.m. | 4 | 0.35 | 6 | 0.43 |
| Between 9:00 and 10:00 p.m. | 150 | 13.09 | 159 | 11.31 |
| Between 10:00 and 11:00 p.m. | 373 | 32.55 | 446 | 31.72 |
| Between 11:00 and 12:00 p.m. | 393 | 34.29 | 492 | 34.99 |
| After 12:00 a.m. | 226 | 19.72 | 303 | 21.55 |
| Wake time week | ||||
| Before 7:00 a.m. | 160 | 13.96 | 499 | 35.49 |
| Between 7:00 and 8:00 a.m. | 437 | 38.13 | 766 | 54.48 |
| Between 8:00 and 9:00 a.m. | 412 | 35.95 | 113 | 8.04 |
| Between 9:00 and 10:00 a.m. | 100 | 8.73 | 24 | 1.71 |
| Between 10:00 and 11:00 a.m. | 19 | 1.66 | 1 | 0.07 |
| Between 11:00 a.m. and 12:00 p.m. | 8 | 0.7 | ||
| After 12:00 p.m. | 10 | 0.87 | 3 | 0.21 |
| Bedtime weekend | ||||
| Before 9:00 p.m. | 1 | 0.09 | 1 | 0.07 |
| Between 9:00 and 10:00 p.m. | 31 | 2.71 | 36 | 2.56 |
| Between 10:00 and 11:00 pm | 213 | 18.59 | 213 | 15.15 |
| Between 11:00 p.m. and 12:00 a.m. | 486 | 42.41 | 497 | 35.35 |
| After 12:00 a.m. | 415 | 36.21 | 659 | 46.87 |
| Wake time weekend | ||||
| Before 7:00 a.m. | 15 | 1.31 | 20 | 1.42 |
| Between 7:00 and 8:00 a.m. | 63 | 5.5 | 115 | 8.18 |
| Between 8:00 and 9:00 a.m. | 210 | 18.32 | 270 | 19.2 |
| Between 9:00 and 10:00 a.m. | 350 | 30.54 | 418 | 29.73 |
| Between 10:00 and 11:00 a.m. | 292 | 25.48 | 277 | 19.7 |
| Between 11:00 a.m. and 12:00 p.m. | 162 | 14.14 | 209 | 14.86 |
| After 12:00 p.m. | 54 | 4.71 | 97 | 6.9 |
HADS_A, Hospital Anxiety and Depression Scale – anxiety subscale; HADS_D, Hospital Anxiety and Depression Scale – depression subscale; ISI, Insomnia Severity Index; MEQ, Morningness–Eveningness Questionnaire; NA, not available.
In Document S3 are summarised the descriptive statistics (number and percentage) about the use of electronic devices. The results showed high levels of use of phones and tablets of >6 h and at bedtime. The same situation was highlighted for the personal computer and social media use but not for the television.
Correlations analyses between predictors and insomnia
The results of the correlation analyses at T1 and T2 are given in Document S4. At T1 insomnia severity was significantly and positively correlated with poor sleep hygiene, high anxiety and depression symptoms, and with emotion regulation strategy of emotional suppression. At T2 insomnia severity was associated with the same variables and also with lower total MEQ scores and higher emotion regulation strategy of cognitive reappraisal.
Factors associated with insomnia
Figure 1 shows the Forest plot for the linear multivariable regression model at T1 and T2. At T1 larger effects were detected for poor sleep hygiene (β = 0.15513, 95% confidence interval [CI] 0.11–0.20, p < 0.0001) and anxiety symptoms (β = 0.73341, 95% CI 0.64–0.83, p < 0.0001). Furthermore, at T2 the results showed that sleep hygiene behaviours (β = 0.14857, 95% CI 0.11–0.19, p < 0.0001), anxiety (β = 0.70146, 95% CI 0.62–0.78, p < 0.0001) and depression (β = 0.17867, 95% CI 0.05–0.31, p < 0.01) symptoms were associated with insomnia severity.
FIGURE 1.
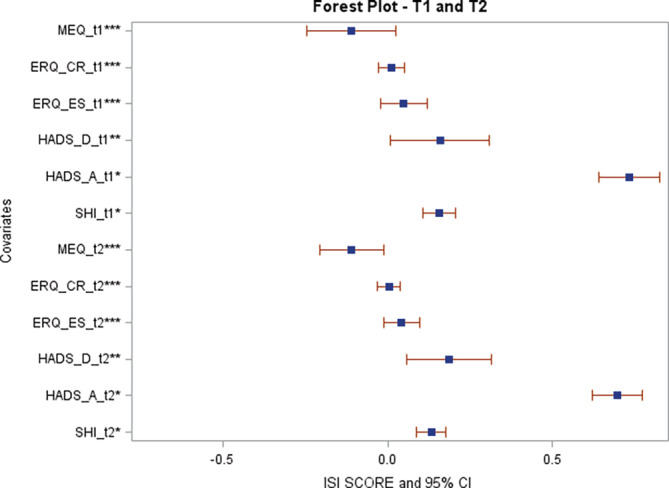
Forest plot for Time 1 and Time 2 linear multivariable regression model. ERQ_CR, Emotion Regulation Questionnaire – cognitive reappraisal subscale; ERQ_ES, Emotion Regulation Questionnaire – expressive suppression subscale; HADS_A, Hospital Anxiety and Depression Scale – anxiety subscale; HADS_D, Hospital Anxiety and Depression Scale – depression subscale; SHI, Sleep Hygiene Index; ISI, Insomnia Severity Index; MEQ, Morningness–Eveningness Questionnaire. *Significant at p ≤ 0.0001; **Significant at p < 0.01; ***Significant at p < 0.05
DISCUSSION
This was a large repeated cross‐sectional study that aimed at evaluating the different impact of the COVID‐19 pandemic on adolescents’ sleep at two different pandemic time points on two distinct large samples. We therefore assessed insomnia prevalence, sleep patterns, and psychological factors in Italian adolescents at the start of the pandemic and after 1 year. As a primary result, we found a high presence of clinical insomnia in adolescents aged 13–17 years at both time points analysed, at the start of the pandemic (T1) and after 1 year (T2) from the COVID‐19 outbreak. The same result was found for the use of electronics, particularly at bedtime.
The results confirmed a trend that was previously observed in the literature for which Italian adolescents’ sleep duration is short (~8 h), and bedtime and waketime patterns are strongly discrepant between weekdays and weekends (Bacaro, Gavriloff, Lombardo, & Baglioni, 2021c). Furthermore, previous work also revealed the role of the COVID‐19 pandemic in increasing sleep disturbances percentages and in delaying sleep–wake patterns (Bruni et al., 2021). This is particularly important considering that previous studies highlighted the potential role of later weeknight bedtime, shorter weeknight sleep duration, greater weekend bedtime delay, and both short and long periods of weekend oversleep for increasing the odds of mood, anxiety, substance use, and behavioural disorders, as well as risk of suicide, tobacco smoking, and poor perceived mental and physical health (Zhang et al., 2017). The use of electronic devices could intensify sleep problems because it has been shown that greater use of electronic devices at bedtime increases the risk of short sleep duration, long sleep onset latency, and increased sleep deficiency (Hysing et al., 2013).
Furthermore, changes in sleep during the COVID‐19 pandemic contribute to the increase in psychopathology symptoms. A particularly clinically relevant result from this study is the high presence of anxiety symptoms at both time points and their potential role in predicting insomnia symptoms. It was previously highlighted the role of lockdowns, physical distancing, school suspension and quarantining in worsening fears, stress, and anxiety symptoms in individuals worldwide (Ahorsu et al., 2020; King, Burke, Halson, & Hawley, 2020). The factors that could be involved in this association are cognitive processes such as worry and rumination. They were found to be significantly correlated with anxiety and depression symptoms in adolescents (Verstraeten, Bijttebier, Vasey, & Raes, 2011). As theorised by Harvey (2002) the tendency to worry and ruminate during the day may extend to the pre‐sleep period, resulting in biased attention to threat, unpleasant intrusive thoughts, and excessive and uncontrollable worry about getting enough sleep. These processes could exacerbate worry, anxiety, and low mood that, in turn, could culminate in a real sleep deficit as well as counter‐productive behaviours such as avoiding bed or getting out of bed. Moreover, results of this study also highlighted the role of the circadian preference in predicting insomnia symptoms and this is consistent with the pre‐pandemic literature (Adan et al., 2012) and confirmed previous results on the impact of circadian preference also on psychopathology and emotional dysregulation in adolescents.
During the pandemic, remote teaching gave adolescents more opportunities to wake up later. In our study, we collected data at two time points with different restrictions concerning school attendance: at T1 (April 14–May 4, 2020) remote teaching was mandatory in all the Italian territory; at T2 (April 12–May 3, 2021) different patterns of remote and in presence teaching were disseminated across regions based on the risk of contagion. With full school reopening, we could expect that T2 was linked with a worse situation of the mismatch between the adolescent's rhythm, with a marked propensity for delayed sleep and rise time, and social demands (e.g., school start time, Alfonsi et al., 2020).
The correlations found at T2 between insomnia symptoms and emotion regulation are also consistent with pre‐pandemic reports (Palmer, Oosterhoff, Bower, Kaplow, & Alfano, 2018). Enhancing adaptive emotion regulation skills in adolescents may help them in dealing with difficult emotions and stress sources, resulting in less engagement with daily worries and deactivation of sleep‐related arousal. This could be particularly important for the implementation of preventing and promoting intervention targeting insomnia symptoms in the post‐pandemic scenario.
This study presents some limitations. First, it was not possible to perform a longitudinal study with the same sample of adolescents. Despite that, we were able to recruit a sample that was comparable both in terms of size and characteristics that was representative of the adolescent population and at the same time ensuring privacy for the participants. Furthermore, the systematic recruitment and the accessibility was a strength of this study, but the telematic format made the use of objectives measures and sleep diaries unfeasible. Future studies should evaluate longitudinally the effects of this pandemic using also objective measures. Another limitation of the study was the fact that the distribution of the sample of the study was not balanced in all the Italian territories. Despite the survey being systematically distributed in the Italian territories through an official mailing list, the participation in the study was voluntary and participants from the North and the Centre were less involved in the study compared to participants from the South of Italy that were more likely to participate. Finally, the follow‐up assessment took place during a period of lighter restraining measures. Despite that, the results pointed to a detrimental effect of the pandemic period itself, regardless of the restrictions in force. Furthermore, another strength of this study was the selective age range of the participants that allowed a specific picture of Italian adolescents.
The results of this study confirm recent literature on the negative effect of the COVID‐19 pandemic in worsening sleep quality and sleep schedules of adolescents (e.g., Bruni et al., 2021). Furthermore, a longitudinal study (Salfi, D'Atri, Tempesta, & Ferrara, 2021), focusing on adult Italian population during two different time points of the first wave of COVID‐19 (2020) found several crucial predictors of poor sleep and insomnia symptoms: female gender, low education, evening chronotype and evening smartphone overuse. This study confirms the trend due to the COVID‐19 pandemic and its restrictions for adolescence in worsening poor sleep quality and delaying bedtime. This is particularly important for clinical implications of this specific population allowing the identification of specific risk factors for the development of sleep disturbance that could also impact psychological wellbeing. Indeed, while this age range was particularly negatively impacted by the pandemic, post‐pandemic health politics should focus on young teenagers and adults. Future health‐promoting interventions are needed in this specific population targeting sleep patterns, insomnia symptoms, and emotion‐regulation strategies. These interventions could be based on the first‐line treatment for insomnia and could be integrated with emotion regulation, implementing a new clinical approach focusing on sleep and emotion‐regulation strategies; offering different preventive and interventional programmes both face‐to‐face and online; and increasing collaboration between clinical psychologist experts of sleep and schools.
AUTHOR CONTRIBUTIONS
Conceptualisation: Chiara Baglioni, Valeria Bacaro and Monica Martoni; methodology: Chiara Baglioni, Valeria Bacaro, Sara Curati; software: Sara Curati; validation: Sara Curati; formal analysis: Sara Curati; investigation: Chiara Baglioni, Valeria Bacaro, Sara Curati, Debora Meneo, Paola De Bartolo, Carlo Buonanno, Francesco Mancini; data curation: Sara Curati, Valeria Bacaro and Chiara Baglioni; writing – original draft preparation: Valeria Bacaro, Paola De Bartolo, Sara Curati; writing – review and editing: Valeria Bacaro, Debora Meneo, Dieter Riemann, Francesco Mancini, Carlo Buonanno, Monica Martoni and Chiara Baglioni. All authors have read and agreed to the published version of the manuscript.
FUNDING INFORMATION
The author(s) received no financial support for this research.
CONFLICT OF INTEREST
All authors declare no conflict of interest.
Supporting information
Appendix S1 Supporting Information
Bacaro, V. , Meneo, D. , Curati, S. , Buonanno, C. , De Bartolo, P. , Riemann, D. , Mancini, F. , Martoni, M. , & Baglioni, C. (2022). The impact of COVID‐19 on Italian adolescents’ sleep and its association with psychological factors. Journal of Sleep Research, 1–8. 10.1111/jsr.13689
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Adan, A. , Archer, S. N. , Hidalgo, M. P. , Di Milia, L. , Natale, V. , & Randler, C. (2012). Circadian typology: A comprehensive review. Chronobiology International, 29(9), 1153–1175. 10.3109/07420528.2012.719971 [DOI] [PubMed] [Google Scholar]
- Adolescent Sleep Working Group . (2014). School start times for adolescents. Pediatrics, 134(3), 642–649. 10.1542/peds.2014-1697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu, D. K. , Lin, C.‐Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The fear of COVID‐19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 20(3), 1537–1545. 10.1007/s11469-020-00270-8 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfonsi, V. , Palmizio, R. , Rubino, A. , Scarpelli, S. , Gorgoni, M. , D'Atri, A. , Pazzaglia, M. , Ferrara, M. , Giuliano, S. , & de Gennaro, L. (2020). The association between school start time and sleep duration, sustained attention, and academic performance. Nature and Science of Sleep, 12, 1161–1172. 10.2147/nss.s273875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altena, E. , Baglioni, C. , Espie, C. A. , Ellis, J. , Gavriloff, D. , Holzinger, B. , Schlarb, A. , Frase, L. , Jernelöv, S. , & Riemann, D. (2020). Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I academy. Journal of Sleep Research, 29(4), e13052. 10.1111/jsr.13052 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM‐5®). American Psychiatric Pub.
- Amicucci, G. , Salfi, F. , D'Atri, A. , Viselli, L. , & Ferrara, M. (2021). The differential impact of COVID‐19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy. Brain Sciences, 11(10), 1336. 10.3390/brainsci11101336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacaro, V. , Chiabudini, M. , Buonanno, C. , De Bartolo, P. , Riemann, D. , Mancini, F. , & Baglioni, C. (2021a). Sleep characteristics in Italian children during home confinement due to Covid‐19 outbreak. Clinical Neuropsychiatry, 18(1), 13–27. 10.36131/cnfioritieditore20210102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacaro, V. , Curati, S. , & Baglioni, C. (2021b). Validation study of the Italian version of the sleep hygiene index. Journal of Sleep Research., 31, e13445. 10.1111/jsr.13445 [DOI] [PubMed] [Google Scholar]
- Bacaro, V. , Gavriloff, D. , Lombardo, C. , & Baglioni, C. (2021c). Sleep characteristics in the Italian pediatric population: A systematic review. Clinical Neuropsychiatry, 18(3), 119–136. 10.36131/cnfioritieditore20210302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglioni, C. , Spiegelhalder, K., Lombardo, C., & Riemann, D. (2010). Sleep and emotions: A focus on insomnia. Sleep Medicine Reviews, 14(4), 227–238. 10.1016/j.smrv.2009.10.007 [DOI] [PubMed] [Google Scholar]
- Bastien, C. H. , Vallières, A. , & Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. 10.1016/s1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Bruni, O. , Malorgio, E. , Doria, M. , Finotti, E. , Spruyt, K. , Melegari, M. G. , … Ferri, R. (2021). Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid‐19 outbreak. Sleep Medicine., 91, 166–174. 10.1016/j.sleep.2021.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain, N. , & Gradisar, M. (2010). Electronic media use and sleep in school‐aged children and adolescents: A review. Sleep Medicine, 11(8), 735–742. doi: 10.1016/j.sleep.2010.02.006 [DOI] [PubMed] [Google Scholar]
- Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. [Google Scholar]
- Esposito, S. , Giannitto, N. , Squarcia, A. , Neglia, C. , Argentiero, A. , Minichetti, P. , Cotugno, N. , & Principi, N. (2021). Development of psychological problems among adolescents during school closures because of the COVID‐19 lockdown phase in Italy: A cross‐sectional survey. Frontiers in Pediatrics, 8, 628072. 10.3389/fped.2020.628072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox, J. , Murray, C. , & Warm, A. (2003). Conducting research using web‐based questionnaires: Practical, methodological, and ethical considerations. International Journal of Social Research Methodology, 6, 167–180. 10.1080/13645570210142883 [DOI] [Google Scholar]
- Gradisar, M. , Gardner, G. , & Dohnt, H. (2011). Recent worldwide sleep patterns and problems during adolescence: A review and meta‐analysis of age, region, and sleep. Sleep Medicine, 12(2), 110–118. 10.1016/j.sleep.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Gradisar, M. , Wolfson, A. R. , Harvey, A. G. , Hale, L. , Rosenberg, R. , & Czeisler, C. A. (2013). The sleep and technology use of Americans: Findings from the National Sleep Foundation's 2011 sleep in America poll. Journal of Clinical Sleep Medicine, 9(12), 1291–1299. 10.5664/jcsm.3272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregory, A. M. , & Sadeh, A. (2016). Annual research review: Sleep problems in childhood psychiatric disorders–A review of the latest science. Journal of Child Psychology and Psychiatry, 57(3), 296–317. 10.1111/jcpp.12469 [DOI] [PubMed] [Google Scholar]
- Gross, J. J. , & Jazaieri, H. (2014). Emotion, emotion regulation, and psychopathology: An affective science perspective. Clinical Psychological Science, 2(4), 387–401. doi: 10.1177/2167702614536164 [DOI] [Google Scholar]
- Gross, J. J. , & John, O. P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relation‐ ships, and well‐being. Journal of Personality and Social Psychology, 85, 348–362. 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Gruber, R. , & Cassoff, J. (2014). The interplay between sleep and emotion regulation: Conceptual framework empirical evidence and future directions. Current Psychiatry Reports, 16(11), 500. 10.1007/s11920-014-0500-x [DOI] [PubMed] [Google Scholar]
- Hagenauer, M. H. , & Lee, T. M. (2012). The neuroendocrine control of the circadian system: Adolescent chronotype. Frontiers in Neuroendocrinology, 33(3), 211–229. 10.1016/j.yfrne.2012.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey, A. (2002). A cognitive model of insomnia. Behaviour Research and Therapy, 40(8), 869–893. 10.1016/s0005-7967(01)00061-4 [DOI] [PubMed] [Google Scholar]
- Harvey, A. G. , Murray, G. , Chandler, R. A. , & Soehner, A. (2011). Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review, 31(2), 225–235. 10.1016/j.cpr.2010.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hysing, M. , Pallesen, S. , Stormark, K. M. , Lundervold, A. J. , & Sivertsen, B. (2013). Sleep patterns and insomnia among adolescents: A population‐based study. Journal of Sleep Research, 22(5), 549–556. 10.1111/jsr.12055 [DOI] [PubMed] [Google Scholar]
- King, A. J. , Burke, L. M. , Halson, S. L. , & Hawley, J. A. (2020). The challenge of maintaining metabolic health during a global pandemic. Sports Medicine, 50, 1233–1241. 10.1007/s40279-020-01295-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam, L. T. , & Yang, L. (2007). Short duration of sleep and unintentional injuries among adolescents in China. American Journal of Epidemiology, 166(9), 1053–1058. doi: 10.1093/aje/kwm175 [DOI] [PubMed] [Google Scholar]
- Moore, M. , Slane, J. , Mindell, J. A. , Burt, S. A. , & Klump, K. L. (2011). Sleep problems and temperament in adolescents. Child: Care, Health and Development, 37(4), 559–562. 10.1111/j.1365-2214.2010.01157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natale, V. , Esposito, M. J. , Martoni, M. , & Fabbri, M. (2006). Validity of the reduced version of the morningness‐eveningness questionnaire. Sleep and Biological Rhythms, 4(1), 72–74. 10.1111/j.1479-8425.2006.00192.x [DOI] [Google Scholar]
- Palmer, C. A. , & Alfano, C. A. (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. 10.1016/j.smrv.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Palmer, C. A. , Oosterhoff, B. , Bower, J. L. , Kaplow, J. B. , & Alfano, C. A. (2018). Associations among adolescent sleep problems, emotion regulation, and affective disorders: Findings from a nationally representative sample. Journal of Psychiatric Research, 96, 1–8. 10.1016/j.jpsychires.2017.09.015 [DOI] [PubMed] [Google Scholar]
- Roberts, R. E. , Roberts, C. R. , & Duong, H. T. (2009). Chronic insomnia and its negative consequences for health and functioning of adolescents: A 12‐month prospective study. Journal of Adolescent Health, 42(3), 294–302. doi: 10.1016/j.jadohealth.2007.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, R. , Socci, V. , Talevi, D. , Mensi, S. , Niolu, C. , Pacitti, F. , di Marco, A. , Rossi, A. , Siracusano, A. , & di Lorenzo, G. (2020). COVID‐19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry, 11. doi: 10.3389/fpsyt.2020.00790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi, F. , Lauriola, M. , D'Atri, A. , Amicucci, G. , Viselli, L. , Tempesta, D. , & Ferrara, M. (2021a). Demographic, psychological, chronobiological, and work‐related predictors of sleep disturbances during the COVID‐19 lockdown in Italy. Scientific Reports, 11(1), 11416. doi: 10.1038/s41598-021-90993-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salfi, F. , D'Atri, A. , Tempesta, D. , & Ferrara, M. (2021b). Sleeping under the waves: A longitudinal study across the contagion peaks of the COVID‐19 pandemic in Italy. Journal of Sleep Research, 30(5), e13313. 10.1111/jsr.13313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shochat, T. , Cohen‐Zion, M. , & Tzischinsky, O. (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. 10.1016/j.smrv.2013.03.005 [DOI] [PubMed] [Google Scholar]
- The International Classification of Sleep Disorders: Diagnostic and Coding Manual . (1991). Annals of Internal Medicine, 115(5), 413. 10.7326/0003-4819-115-5-413_1 [DOI] [Google Scholar]
- Verstraeten, K. , Bijttebier, P. , Vasey, M. W. , & Raes, F. (2011). Specificity of worry and rumination in the development of anxiety and depressive symptoms in children. British Journal of Clinical Psychology, 50(4), 364–378. 10.1348/014466510x532715 [DOI] [PubMed] [Google Scholar]
- Wolfson, A. R. , Spaulding, N. L. , Dandrow, C. , & Baroni, E. M. (2007). Middle school start times: The importance of a good night's sleep for young adolescents. Behavioral Sleep Medicine, 5(3), 194–209. 10.1080/15402000701263809 [DOI] [PubMed] [Google Scholar]
- Zhang, J. , Paksarian, D. , Lamers, F. , Hickie, I. B. , He, J. , & Merikangas, K. R. (2017). Sleep patterns and mental health correlates in US adolescents. The Journal of Pediatrics, 182, 137–143. 10.1016/j.jpeds.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Zigmond, A. S. , & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Supporting Information
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


