Abstract
Aim
The aim of this study was to assess the influence of perceived work environment, empowerment and psychological stress on job burnout among nurses working at the time of the COVID‐19 pandemic.
Background
Nurses experienced high levels of job burnout during the pandemic, which impacted their mental health and well‐being. Studies investigating the influence of work environment, empowerment and stress on burnout during the time of COVID‐19 are limited.
Design
The study utilized a cross‐sectional design.
Methods
Data were collected from 351 nurses in Oman between January and March 2021. The Maslach Burnout Inventory, the Practice Environment Scale of the Nursing Work Index, the Conditions of Work Effectiveness Questionnaire and the Perceived Stress Scale were used to assess study variables.
Results
About two‐thirds of the nurses (65.6%) reported high levels of job burnout. Nurse managers' ability, leadership and support; staffing and resources adequacy; and nurses' access to support were significant factors associated with a reduced level of burnout.
Conclusion
Supporting nurses during the crisis, ensuring adequate staffing levels and providing sufficient resources are critical to lower job burnout. Creating a positive and empowered work environment is vital to enhance nurses' retention during the pandemic.
Keywords: COVID‐19, empowerment, job burnout, nursing, stress, work environment
Summary statement
What is already known about this topic?
Nurses' perceived work environment and structural empowerment have been associated with job burnout. However, their impact during the COVID‐19 has not been examined.
As nurses' psychological stress increases, their job burnout increases.
What this paper adds?
Nurses experienced high levels of job burnout during the COVID‐19 pandemic.
Working in a favourable environment and having access to support can reduce nurses' job burnout during the crisis.
The implications of this paper
During pandemics, ensuring adequate staffing levels and providing sufficient resources are critical to lower job burnout and enhance nurse retention.
1. INTRODUCTION
In March 2020, the World Health Organization (WHO) declared coronavirus (COVID‐19) a global pandemic. As of 1 June 2022, the WHO reported more than six million deaths due to COVID‐19 worldwide (WHO, 2022a). Oman, one of the Middle East countries with a 4.5 million population, has reported 389,473 confirmed cases of COVID‐19 and 4260 deaths between 3 January 2020 and 1 June 2022 (WHO, 2022b). In Oman, several health‐related measures have been implemented in response to the vast spread of the virus. Several outpatient clinics, intensive care units and in‐patient wards were converted and restructured into COVID‐19 and non‐COVID units to reduce the transmission of the disease. Management of chronic diseases was suspended at some clinics, home delivery services to transport regular drugs to patients were initiated and patients were instructed to call if they need urgent medical attention (Al Ghafri et al., 2021).
Evidence has shown the negative impact of the pandemic on healthcare providers' mental well‐being (Sun et al., 2020). Findings from a recent systematic review of 13 studies that included 33 062 participants indicated that nurses are the most affected healthcare providers (Pappa et al., 2020). Studies reveal that nurses working during the time of COVID‐19 experience high levels of burnout (Hu et al., 2020; Murat et al., 2021), with an overall prevalence of 34.1% (Galanis et al., 2021).
Job burnout (JB) is defined as a psychological reaction to prolonged emotional and interpersonal stress (Maslach et al., 1996). The nature of nurses' work environment involves several stressors such as high workload, lack of administrative support, exposure to pain and caring for terminally ill patients (Wang et al., 2015; Wilczek‐Rużyczka et al., 2019). During the COVID‐19 pandemic, nurses were exposed to more stressors that increased their risk of developing JB. In Oman, nurses were required to work a 12‐h shift instead of a regular 8‐h shift and some nurses worked continuously for more than 12 h specifically those who worked at the airport clinics. At the beginning of the pandemic, nurses encountered shortages of supplies including facemasks and personal protective equipment (PPE) (Al Ghafri et al., 2021). Al Ghafri et al. (2020) conducted a qualitative study to explore the experience of healthcare workers who were involved in the management of COVID‐19 in Oman. Forty healthcare professionals participated. Participants reported the imbalance between the increasing work responsibilities and limited resources as the main challenge. Nurses' responsibilities were not limited to providing patient care but extended to providing psychological support for their families and dealing with community rumours and the pandemic‐related misleading information. People requested nurses to clarify the accuracy of several misleading information they received from social media platforms and several untrusted sources (Al Sabei, 2022). Other stressors were lack of knowledge of dealing with dead bodies and the fear of spreading the virus to family members (Al Ghafri et al., 2020). These stressors resulted in reducing nurses' motivation to work and increasing their burnout (AlAbri & Bte Siron, 2020).
Burnout has been associated with high turnover rates and poor quality of care (Al Sabei et al., 2020). Therefore, it is critically important to assess the level of burnout among nurses during the pandemic and identify factors that can reduce it.
Psychological stress (SS) is one of several factors associated with nurses' burnout during COVID‐19 (Arnetz et al., 2020). The increasing prevalence of stress among nurses is due to their work in a stressful environment and their fear of being infected or infecting their loved ones (Coşkun Şimşek & Günay, 2021). Evidence has shown that work environment (WE) (Ambani et al., 2020) and structural empowerment (SE) (Zhang et al., 2018) are modifiable factors influencing nurse JB; however, their impact during the COVID‐19 has not been examined. During the pandemic, ensuring a positive nurse WE is vital to sustain nurses' health and assist them in delivering quality care to patients, despite the threat of the virus. Identifying modifiable WE characteristics that can mitigate nurses' burnout can help policymakers implement strategies to ensure healthy working conditions and safe patient care in times of crisis.
The allocation of healthcare human resources was identified as a major factor in the worldwide effort to monitor and respond to the COVID‐19 pandemic (WHO, 2020). The lack of healthcare professionals led to negative outcomes at the organizational and professional levels (Al Sabei et al., 2020; Boamah et al., 2017). However, the relationship of staffing and resource adequacy with nursing JB has not been sufficiently investigated during the pandemic of COVID‐19.
In Oman, COVID‐19 cases were treated only in governmental hospitals (Al Ghafri et al., 2020). The Ministry of Health responded to this situation by changing the working‐hours routine, mobilizing healthcare professionals and modifying the leave days procedure to ensure sufficient healthcare staffing (Al Khalili et al., 2021). These measures were expected to affect the WE and generated new stressors for the nursing workforce. Hence, investigating the influence of such modifications in the WE on nursing JB is essential for future planning and management of similar situations.
1.1. Theoretical framework
The study was based on the Job Demand‐Resources (JD‐R) model (Bakker & Demerouti, 2017). Job demands are defined as cognitive, physical or emotional aspects of a job that must be overcome in order to function effectively (Bakker & Demerouti, 2017). Since the COVID‐19 disease has been prevalent for a long time, health professionals have been exposed to high workloads that have affected their psychological well‐being (Moreno‐Jiménez et al., 2021). In Oman, healthcare workers, including nurses, had to adjust to new demands and stressors such as changes in work routines, wearing protective measures, transitioning to other units, taking care of a high volume of patients and worrying about spreading the virus to their social networks (Al Ghafri et al., 2020). Studies revealed that the frequent exposure to stressors during the COVID‐19 had a negative impact on nurses' mental health (Alshekaili et al., 2020) and psychological well‐being (Al Mahyijari et al., 2021). Therefore, the identification of job resources is critical in reducing the burden of job demands during the pandemic.
According to the JD‐R model, the availability of high levels of job resources results in reducing the job‐related burnout, whereas high levels of job demands can increase JB (Taris & Schaufeli, 2016). Job resources can be defined as aspects of the job that are vital to meeting organizational goals, reducing job demands and encouraging individual growth and development (Zhou et al., 2022). During the COVID‐19, there was a lack of material and human resources in Oman due to increasing number of infected people including healthcare workers. The literature highlighted the importance of WE and SE as organizational supportive resources to cope with stressors during previous pandemics such as the swine flu pandemic (H1N1), the severe acute respiratory syndrome and the Middle East respiratory syndrome (Barello et al., 2020). However, limited evidence assessed the impact of WE and SE on reducing stress during the COVID‐19 situation. Therefore, in the current study, WE and SE components were considered job resources, and SS was considered a reflection of perceived job demand; see Figure 1.
FIGURE 1.
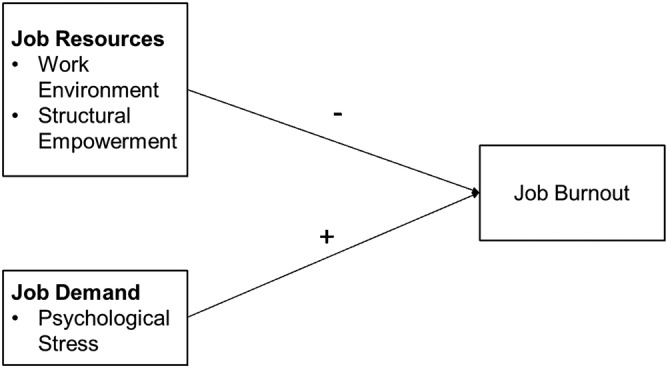
Job‐resources demand model
2. METHODS
2.1. Aim
The aim of the current study was to assess the influence of perceived WE, empowerment and SS on JB among nurses working at the time of COVID‐19 pandemic.
2.2. Design
A descriptive cross‐sectional design was used.
2.3. Participants and settings
The study targeted staff nurses working in five hospitals in Oman. A convenience sampling technique was used to select study hospitals. The sample size was calculated based on the rule of thumb recommendation for multivariate regression analysis suggested by Tabachnick and Fidell (2007). This rule of thumb recommended using 20 cases for each predictor in the regression analysis. In the current study, 19 predictors were used in the final regression analysis. Therefore, the estimated required sample size is 19* 20 = 380 subjects. The inclusion criteria included having at least a diploma in nursing and having spent at least 1 year in their current unit. Participants were not required to have directly cared for patients with COVID‐19, but all worked and completed the survey during the peak COVID‐19 period (January–March 2021).
2.4. Data collection
After securing the hospitals administrators' approval, an initial invitation to participate in the study was posted on the hospitals' websites. Consent was obtained electronically as part of the cover letter of the study. The cover letter included information about the study aims, procedure, the contact information of the study team and a checkbox indicating agreement to participate in order to access the main survey. In addition, participants were informed that their participation is voluntary and no confidential information will be obtained or reported. Finally, the data collected in this study were based on the self‐reported method, which may be associated with response bias. To reduce the possibility of this bias, all data were collected anonymously with no identification data.
The data were collected using an online survey that was distributed to staff nurses in the participating hospitals during January–March 2021. The survey was in English.
2.5. Data collection instruments
The survey assessed five types of variables: demographic variables, SS, SE, WE and JB. Demographic variables included age, gender, marital status, education, nationality, years of experience in the nursing profession and in the current unit and place of work.
Perceptions of the WE were assessed using the Practice Environment Scale of the Nursing Work Index (PES‐NWI) Revised that was developed by Lake (2002). The PES‐NWI is an instrument that measures the quality of the WE, which is defined as ‘the organizational characteristics of a work setting that facilitate or constrain professional nursing practice’ (Lake, 2002, p. 178). The PSE‐NWI is a 31‐item, 4‐point Likert scale, wherein 1 refers to ‘strongly disagree’ and 4 refers to ‘strongly agree,’ with a higher score indicating the positive perception that the feature is present in the WE. Example of the items is ‘staff nurses are involved in the internal governance of the hospital’. The scale consists of five subscales. The first subscale is nursing foundation for quality care that measures to what extent nursing care is based on high standards. The second subscale is nurse participation in hospital affairs that assess nurse's involvement in decision‐making and hospital committees. The third subscale is nurse manager ability, leadership and support of nurses that measures nurses' perception of their direct supervisor's leadership and support. The fourth subscale is staffing and resource adequacy. The fifth subscale is nurse–physician collegial relationship. The mean score was generated for each subscale. Scores below 2.5 on any subscale are indicative of disagreement, while scores above 2.5 demonstrate agreement that the subscale items are present in the WE (Lake & Friese, 2006). The scale has been used internationally and validated in diverse cultures, including in Oman (Al Sabei et al., 2021). The Cronbach's alpha ranged between 0.71 and 0.84 (Lake, 2002). In the current study, the Cronbach's alpha was 0.94 for the composite score and ranged between 0.75 and 0.87 for the subscales.
SE was assessed using the Conditions of Work Effectiveness Questionnaire‐II (CWQ‐II) that was developed by Laschinger et al. (2001). The CWQ‐II is a 12‐item, 5‐point Likert scale, wherein 1 refers to ‘none’ and 5 refers to ‘a lot’. An example of the items is ‘How much access to information regarding the current state of the hospital do you have in your present job’. The CWQ‐11 measures four dimensions of empowerment: access to information, opportunity, support, and resources. Based on Kanter's (2008) theory of workplace empowerment, access to information refers to having important knowledge about organizational policies and technical skills and expertise that are necessary to enhance work effectiveness. Access to opportunity refers to the possibility for growth and development. Access to resources refers to the ability to acquire the required human and physical resources, including staffing, time, materials and supplies necessary to accomplish organizational goals. Access to support involves receiving administrative guidance, directions and timely feedback. Total SE scores are calculated by summing the four subscales. The SE is categorized into three levels: low levels of empowerment (scores between 4 and 9), moderate (scores between 10 and 14) and high (scores between 16 and 20) (Laschinger et al., 2001). The reliability and validity of the scale are well established, with a Cronbach's alpha of 0.82 (Laschinger et al., 2001). In the current study, the Cronbach's alpha was 0.95 for the composite score and ranged between 0.88 and 0.94 for the subscales.
SS was measured using the short version of the Perceived Stress Scale (PSS) that measures ‘the degree to which individuals appraise situations in their lives as stressful’ (Cohen et al., 1983, p. 385). The PSS is a four‐item, 5‐point Likert scale, wherein 0 refers to ‘never’ and 4 refers to ‘very often’. Higher scores indicate higher perceptions of stress. An example of the items is ‘In the last month, how often have you felt that you were unable to control the important things in your life’. The PSS is one of the most widely used psychological instruments. It has demonstrated good validity and reliability, with a Cronbach's alpha of 0.79 (Karam et al., 2012). In the current study, the Cronbach's alpha was 0.56.
JB was measured using the emotional exhaustion subscale of the Maslach Burnout Inventory (Maslach et al., 1996). Emotional exhaustion refers to the feelings of emotionally exhausted by one's work. Emotional exhaustion is a nine‐item, 7‐point Likert scale, wherein 1 refers to ‘never’ and 7 refers to ‘every day’. Higher scores indicate higher levels of emotional exhaustion. Example of the items is ‘I feel emotionally drained by my work’. Emotional exhaustion is described as a mean composite score and is also categorized into three levels: low (scores less than 18), moderate (scores between 19 and 26) and high (scores of 27 or more) (Maslach et al., 1996). The emotional exhaustion scale has been used internationally and validated in diverse cultures, including in Oman (Al Sabei et al., 2022). The internal consistency reliability of the scale has been well demonstrated, with a Cronbach's alpha of 0.92 (Aiken et al., 2008). In the current study, the Cronbach's alpha was 0.73.
2.6. Ethical considerations
Ethical approval was obtained from the Ministry of Health and the university ethics committee prior to data collection. The research assistants explained the study aims and data collection methods to hospitals' representative. Formal administrative approval was obtained from the participating hospitals.
2.7. Data analysis
Sample characteristics were described using descriptive statistics of means, standard deviations, frequencies and percentages. Bivariate associations between JB, nurse demographics and work characteristics were described using analysis of variance (ANOVA), Chi‐square and t‐test. Multivariate regression (enter method) was used to assess the influence of SE, SS and WE on JB. A finding with a p‐value of less than 0.05 was considered statistically significant. No statistical methods were used to replace missing values across all variables. Missing values for each variable were reported in footnotes of the reported tables as appropriate. In the current study, no sensitivity analyses were implemented. Finally, all analyses were conducted using SPSS®‐PC Version 23.
3. RESULTS
Of the 600 nurses who were invited, a total of 351 participated in the study, with a response rate of 58.5%. The age ranged from 22 to 55 years old with an average of 33.7 (SD = 7.22) years. The sample was predominantly female (81.2%) and consisted mostly of Omani nurses (54.7%) with diplomas in nursing (55.6%). On average, the nurses had spent 10 years in the nursing profession and 6 years in their current unit. The majority (61.4%) worked in medical or surgical units; see Table 1.
TABLE 1.
Descriptive and bivariate statistics of job burnout with respect to nurses' sociodemographics and work characteristics (N = 351)
| Entire sample | Job burnout | |||
|---|---|---|---|---|
| Variable | n (%) | Mean | SD | t/F |
| Age | ||||
| 20–30 | 119 (33.9) | 33.680 | 11.026 | 7.913 ** |
| 31–40 | 138 (39.3) | 29.756 | 8.719 | |
| >40 | 59 (16.8) | 28.203 | 9.589 | |
| Gender | ||||
| Female | 285 (81.2) | 31.244 | 10.048 | 0.128 |
| Male | 66 (18.8) | 31.062 | 11.483 | |
| Nationality | ||||
| Local | 192 (54.7) | 33.770 | 10.440 | 5.339 ** |
| Expatriate | 159 (45.3) | 28.057 | 9.258 | |
| Marital status | ||||
| Single | 101 (28.8) | 31.150 | 10.288 | −0.142 |
| Married | 250 (71.2) | 31.233 | 10.345 | |
| Highest education level | ||||
| Diploma | 195 (55.6) | 30.569 | 8.852 | 2.622 |
| Baccalaureate | 144 (41.0) | 31.576 | 12.068 | |
| Master | 12 (3.4) | 37.636 | 6.975 | |
| Years of experience in the profession | ||||
| 7 or less | 109 (31.1) | 34.486 | 10.562 | 13.280 ** |
| 8–15 | 160 (45.7) | 28.819 | 9.829 | |
| 16–36 | 81 (23.1) | 29.012 | 9.047 | |
| Years of experience in the present unit | ||||
| 7 or less | 94 (32.9) | 34.787 | 10.462 | 11.393 ** |
| 8–15 | 115 (40.2) | 29.062 | 9.707 | |
| 16–36 | 77 (26.9) | 28.610 | 9.182 | |
| Type of working unit | ||||
| Medical/surgical | 215 (61.4) | 30.80 | 9.791 | 1.539 |
| Critical care | 68 (19.4) | 31.52 | 10.131 | |
| Oncology | 35 (10) | 34.40 | 11.479 | |
| OBG | 10 (2.9) | 32.10 | 7.622 | |
| Psychiatric | 11 (3.1) | 27.36 | 9.801 | |
| Others a | 11 (3.1) | 26.60 | 12.295 | |
| Hospital teaching status | ||||
| Teaching | 68 (19.4) | 30.88 | 11.786 | −0.291 |
| Nonteaching | 283 (80.6) | 31.30 | 9.946 | |
Note: Missing data were as follows: age = 35, years of experience in nursing = 65.
Include nurses working in multispecialty units, outpatient clinics, paediatric, and operation theatre.
p < 0.05.
p < 0.001.
3.1. JB
About two‐thirds of the nurses (65.6%) reported high levels of JB. A description of burnout in relation to nurses' demographics and work characteristics is shown in Table 1. Bivariate statistics showed that local nurses reported higher levels of burnout than expatriate nurses (p < 0.01). Post hoc comparisons revealed that nurses aged 31–40 and those with 7 years of work experience or less in the profession and in their unit experienced higher levels of burnout than their counterparts.
3.2. WE, empowerment and stress
The mean score for WE was 2.835 (SD = 0.408). All five subscales were scored positively by the study participants. The perception of collegial nurse–physician relationships was rated the highest (M = 2.923, SD = 0.529), followed by foundations for quality care (M = 2.910, SD = 0.417). Staffing and resources adequacy received the lowest rating (M = 2.685, SD = 0.526).
The mean score for SE was 13.096 (SD = 3.438), indicating a moderate level of empowerment. Access to opportunity was rated the highest (M = 3.445, SD = 1.012), followed by access to resources (M = 3.290, SD = 1.003). Access to information was rated the lowest (M = 3.142, SD = 1.080). The mean score for stress was 2.071 (SD = 0.823); see Table 2.
TABLE 2.
Descriptive results of work environment, engagement, stress and job burnout
| Scale/subscales | Mean (SD) |
|---|---|
| Work environment a | 2.835 (0.408) |
| Participation in hospital affairs | 2.769 (0.480) |
| Foundations for quality of care | 2.910 (0.417) |
| Manager ability, leadership and support | 2.861 (0.515) |
| Staffing and resource adequacy | 2.685 (0.526) |
| Collegial nurse–physician relations | 2.923 (0.529) |
| Structural empowerment a | 13.096 (3.438) |
| Access to opportunity | 3.445 (1.012) |
| Access to resources | 3.290 (1.003) |
| Access to information | 3.142 (1.080) |
| Access to support | 3.220 (0.863) |
| Job stress | 2.071(0.823) |
| Job burnout | 31.209 (10.314) |
| n (%) | |
|---|---|
| Job burnout levels | |
| Low | 37 (10.7) |
| Moderate | 82 (23.7) |
| High | 227 (65.6) |
Composite score.
3.3. The influence of WE, empowerment and stress on JB
Results from regression analysis showed that SE, SS and WE were significant predictors of nurses' JB during the time of COVID‐19; see Table 3. The overall model explained 55% of the variance. Controlling for nurse, unit and hospital characteristics, two subscales of the Practice Environment Scale of the Nursing Work Index were significantly and negatively associated with JB: nurse manager ability, leadership and support (β = −0.228, p = 0.041) and staffing and resources adequacy (β = −0.120, p = 0.03). Among the SE subscales, access to support was the only significant predictor of JB (β = −0.140, p = 0.04). Stress was the most significant predictor of JB; each additional point for stress was associated with a 0.533 increase in the level of JB (β = 0.533, p < 0.001).
TABLE 3.
The influence of work environment, structural empowerment and stress on job burnout
| Variable | Job burnout | |||||
|---|---|---|---|---|---|---|
| B | SE | β | t | 95% CI | ||
| Work environment | ||||||
| Participation in hospital affairs | 0.542 | 1.302 | 0.029 | 0.416 | −2.022 | 3.106 |
| Nursing foundations for quality of care | 1.168 | 1.386 | 0.049 | 0.843 | −1.562 | 3.899 |
| Manager ability, leadership and support | −4.268 | 1.172 | −0.228* | −3.643 | −6.575 | −1.960 |
| Staffing and resource adequacy | −2.310 | 1.068 | −0.120* | −2.163 | −4.414 | −0.207 |
| Nurse–physician relations | 0.216 | 0.981 | 0.011 | 0.220 | −1.717 | 2.149 |
| Structural empowerment | ||||||
| Access to opportunity | 0.512 | 0.730 | 0.043 | 0.702 | −0.925 | 1.950 |
| Access to resources | 0.059 | 0.885 | 0.005 | 0.066 | −1.684 | 1.802 |
| Access to information | 1.047 | 0.865 | 0.097 | 1.211 | −0.656 | 2.751 |
| Access to support | −1.711 | 0.851 | −0.140* | −2.011 | −3.388 | −0.035 |
| Stress | 6.801 | 0.603 | 0.533** | 11.272 | 5.612 | 7.989 |
| Constant | 19.354 | 6.124 | 3.160* | 7.290 | 31.417 | |
Note: The model was controlled for nurse, unit and hospital characteristics including age, gender, marital status, level of education, years in nursing, years in present unit, working unit and hospital teaching status.
p < 0.05.
p < 0.01.
4. DISCUSSION
4.1. Study variables score level
The results showed that the majority of nurses (65.5%) experienced high levels of JB. This is consistent with findings from the United States (Arnetz et al., 2020), China (Hu et al., 2020), Italy (Giusti et al., 2020), Turkey (Murat et al., 2021) and Jordan (Algunmeeyn et al., 2020), suggesting that an increasing level of burnout among nurses during the pandemic is a universal psychological concern. This is an expected finding, given that nurses are spending a large amount of time working in a risky and threatening environment.
Although the mean score for the perceived WE in the current study was above the midpoint of 2.5, all subscales were below 3.00, indicating a need to improve nurses' working conditions. Among the five subscales of WE, nurses rated their perceptions of staffing and resources adequacy the lowest. This could be attributed to the global shortages of human and physical resources, including limited beds, ventilators and PPE (Ranney et al., 2020). Nurses rated their collegial relationship with physicians as the most favourable dimension of the WE. Our findings support a previous study conducted in Oman (Al Sabei et al., 2020) and in China (Wu et al., 2018). Nurse–physician relationship has become even more important amid the increasing workplace stressors resulting from the COVID‐19 pandemic (Tannenbaum et al., 2021). It is noteworthy that during the pandemic, interprofessional teams, including nurses and physicians, are often formed temporarily because of the shortages and the extraordinary influx of healthcare providers to supplement hospitals. Therefore, having well‐structured team building strategies is vital to sustain team effectiveness.
The mean score for SE was above the midpoint, indicating a moderately empowering environment. Across the five dimensions of empowerment, access to information was rated the lowest. The literature reveals that nurses feel unprepared to care for COVID‐19 patients because they lack the necessary knowledge and training (Travers et al., 2020). Sun et al. (2020) found that nurses caring for COVID‐19 patients were anxious due to their lack of knowledge about the disease, despite their previous experience of working in the department of infectious diseases. Furthermore, nurses in Oman are being assigned to new units to mitigate the shortages. This result underscores the importance of enhancing nurses' knowledge on how to effectively manage COVID‐19 patients and providing adequate orientation and training for nurses assigned to new units.
4.2. Influence of WE, SE and SS on JB
Findings from the current study advance and support the existing JD‐R model. JB was influenced by the presence of both job demand and job resources. The perceived SS was found to be the most significant predictor. This is in line with findings from international studies conducted prior to COVID‐19 (Guo et al., 2016) and during the pandemic (Giusti et al., 2020; Yıldırım & Solmaz, 2020) which all revealed that as the demands and stress levels among nurses increase, their JB increases. Studies also showed that during the time of COVID‐19, direct care nurses experienced high levels of work distress due to their fear of being infected (Labrague & de los Santos, 2020), infecting others (Pappa et al., 2020) and feeling helpless and concerned about patients' and their families' health and suffering (Sun et al., 2020). Therefore, supporting nurses and providing stress reduction strategies are paramount to reduce their burnout.
At the job resources level, three factors were significantly associated with nurses' JB: staffing and resources adequacy; manager ability, leadership and support; and access to support. The findings showed that adequate access to support and better perceptions of manager ability, leadership and support were associated with lower levels of JB. These findings support the evidence from qualitative research emphasizing that managers and superiors providing leadership support in terms of feedback, guidance, direction and organization of the workplace can create an empowering environment, make nurses feel more competent and appreciated and mitigate the stress and burnout they experience (Arnetz et al., 2020; Travers et al., 2020). Examples of leadership support include addressing nurses' COVID‐19 educational needs, providing flexible work schedules and adequate rest periods and meeting nurses' mental health and safety demands.
Better perceptions of staffing and resource adequacy were associated with lower burnout. This is congruent with studies conducted among nurses before the period of COVID‐19 pandemic (Albashayreh et al., 2019; Boamah et al., 2017). In addition, this result supported studies conducted during the pandemic that linked nurses' burnout to a lack of hospital materials and manpower (Galanis et al., 2021). Despite the importance of adequate staffing in lowering burnout levels among nurses, the nurses in Oman rated staffing and resource adequacy lower than the other WE elements. This result highlights the importance of ensuring reasonable nurse staffing levels and adequate resources (e.g., materials and supplies) to reduce nurses' burnout during the COVID‐19 pandemic. The literature shows that providing nurses with sufficient resources, such as PPE, is essential to reduce their fear (Labrague & de los Santos, 2020; Travers et al., 2020), which can ultimately lower their JB.
4.3. Limitations of the study
As this was a cross‐sectional study, causal links between study variables and burnout could not be established. Moreover, the current study did not report if the nurses were engaged in direct patient care of COVID‐19 cases or not. Having knowledge about this factor could give better insights into the association of caring for COVID‐19 patients and the study variables. Furthermore, the current study included only five hospitals. Caution should be exercised when generalizing the findings as the sample may not be representative to all healthcare sectors in Oman. Although the regression model explained more than half of the variation in JB, there are other important factors that need to be investigated, such as nurses' perceptions of family–work–life balance and whether nurses had a pre‐existing psychological problem. Future studies exploring these factors can contribute to the accuracy of the predictors of burnout among nurses during pandemics.
5. CONCLUSION
Nurses experience high levels of stress and burnout during the COVID‐19 pandemic. The study highlighted five strategies for policymakers to implement to lower nurses' levels of burnout pandemics. First, there is a need to reduce nurses' stress levels by regularly assessing their SS and well‐being and conducting stress reduction mechanisms. Second, nurse managers and policymakers are required to create an empowering environment by providing access to support. Third, ensuring safe staffing levels and adequate resources is critical to enhance the WE. Fourth, nurse leaders should design a plan for updating and increasing nurses' knowledge about infectious diseases. Finally, assigning a mentor to train and socialize nurses who are redeployed during the pandemic is critical.
FUNDING INFORMATION
This work was supported by the The Research Council, Sultanate of Oman (RC/RG‐CON/FACN/18/01), and Sultan Qaboos University (RF/CON/FACN/19/01).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
SA, OA and IAB designed the study. SA collected the data. SA analysed the data. SA, LJL and RA prepared the manuscript. SA, OR, RA, LJL and IAB provide critical revisions for important intellectual content. All authors approved the final version for submission.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Sultan Qaboos University and The Research Council for their support and thank all nurses who contributed to this study.
Al Sabei, S. D. , Al‐Rawajfah, O. , AbuAlRub, R. , Labrague, L. J. , & Burney, I. A. (2022). Nurses' job burnout and its association with work environment, empowerment and psychological stress during COVID‐19 pandemic. International Journal of Nursing Practice, e13077. 10.1111/ijn.13077
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Aiken, L. H. , Clarke, S. P. , Sloane, D. M. , Lake, E. T. , & Cheney, T. (2008). Effects of hospital care environment on patient mortality and nurse outcomes. Journal of Nursing Administration, 38(5), 223–229. 10.1097/01.NNA.0000312773.42352.d7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Ghafri, T. , Al Ajmi, F. , Anwar, H. , Al Balushi, L. , Al Balushi, Z. , Al Fahdi, F. , Al Lawati, A. , Al Hashmi, S. , Al Ghamari, A. , Al Harthi, M. , Kurup, P. , Al Lamki, M. , Al Manji, A. , Al Sharji, A. , Al Harthi, S. , & Gibson, E. (2020). The experiences and perceptions of health‐care workers during the COVID‐19 pandemic in Muscat, Oman: A qualitative tudy. Journal of Primary Care & Community Health, 11, 1–8. 10.1177/2150132720967514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Ghafri, T. , Al Ajmi, F. , Al Balushi, L. , Kurup, P. M. , Al Ghamari, A. , Al Balushi, Z. , Al Fahdi, F. , Al Lawati, H. , Al Hashmi, S. , Al Manji, A. , & Al Sharji, A. (2021). Responses to the pandemic COVID‐19 in primary health care in Oman: Muscat experience. Oman Medical Journal, 36(1), 216–224. 10.5001/omj.2020.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Khalili, S. , Al Maani, A. , Al Wahaibi, A. , Al Yaquobi, F. , Al‐Jardani, A. , Al Harthi, K. , Alqayoudhi, A. , Al Rawahi B., & Al‐Abri, S. (2021). Challenges and opportunities for public health service in Oman from the COVID‐19 pandemic: Learning lessons for a better future. Frontiers in Public Health, 9, 1–10. 10.3389/fpubh.2021.770946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Mahyijari, N. , Badahdah, A. , & Khamis, F. (2021). The psychological impacts of COVID‐19: a study of frontline physicians and nurses in the Arab world. Irish Journal of Psychological Medicine, 38(3), 186–191. 10.1017/IPM.2020.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Sabei, S. D. , Labrague, L. J. , Miner, A. R. , Karkada, S. , Albashayreh, A. , Al Masroori, F. , & Al Hashmi, N. (2020). Nursing work environment, turnover intention, job burnout, and quality of care: The moderating role of job satisfaction. Journal of Nursing Scholarship, 52(1), 95–104. 10.1111/jnu.12528 [DOI] [PubMed] [Google Scholar]
- Al Sabei, S. D. , AbuAlRub, R. , Labrague, L. J. , Burney, I. A. , & Al‐Rawajfah, O. (2021). The impact of perceived nurses' work environment, teamness, and staffing levels on nurse‐reported adverse patient events in Oman. Nursing Forum, 56(4), 897–904. 10.1111/nuf.12639 [DOI] [PubMed] [Google Scholar]
- Al Sabei, S. D. (2022). Information: Too Much or Too Soon? In Al‐Suqri M., Alsalmi J., & Al‐Shaqsi O. (Eds.), Mass Communications and the Influence of Information During Times of Crises (pp. 43–67). IGI Global. 10.4018/978-1-7998-7503-1.ch003 [DOI] [Google Scholar]
- Al Sabei, S. D. , Labrague, L. J. , Al‐Rawajfah, O. , AbuAlRub, R. , Burney, I. A. , & Jayapal, S. K. (2022). Relationship between interprofessional teamwork and nurses' intent to leave work: The mediating role of job satisfaction and burnout. Nursing Forum. 10.1111/NUF.12706 [DOI] [PubMed] [Google Scholar]
- AlAbri, I. , & Bte Siron, R. (2020). Health care professional attitude and motivation during covid‐19: A case of health sector of oman. Systematic Reviews in Pharmacy, 11(9), 1035–1040. 10.31838/srp.2020.9.149 [DOI] [Google Scholar]
- Albashayreh, A. , Al Sabei, S. D. , Al‐Rawajfah, O. M. , & Al‐Awaisi, H. (2019). Healthy work environments are critical for nurse job satisfaction: implications for Oman. International Nursing Review, 66(3), 389–395. 10.1111/inr.12529 [DOI] [PubMed] [Google Scholar]
- Algunmeeyn, A. , El‐Dahiyat, F. , Altakhineh, M. M. , Azab, M. , & Babar, Z. U. D. (2020). Understanding the factors influencing healthcare providers' burnout during the outbreak of COVID‐19 in Jordanian hospitals. Journal of Pharmaceutical Policy and Practice, 13(1), 1–8. 10.1186/s40545-020-00262-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshekaili, M. , Hassan, W. , Al Said, N. , Al Sulaimani, F. , Jayapal, S. K. , Al‐Mawali, A. , Fai Chan, M. , Mahadevan, S. , & Al‐Adawi, S. (2020). Factors associated with mental health outcomes across healthcare settings in Oman during COVID‐19: frontline versus non‐frontline healthcare workers. British Medical Journal Open, 10(10). 10.1136/BMJOPEN-2020-042030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambani, Z. , Kutney‐Lee, A. , & Lake, E. T. (2020). The nursing practice environment and nurse job outcomes: A path analysis of survey data. Journal of Clinical Nursing, 29(13–14), 2602–2614. 10.1111/jocn.15283 [DOI] [PubMed] [Google Scholar]
- Arnetz, J. E. , Goetz, C. M. , Arnetz, B. B. , & Arble, E. (2020). Nurse reports of stressful situations during the COVID‐19 pandemic: Qualitative analysis of survey responses. International Journal of Environmental Research and Public Health, 17(21), 1–12. 10.3390/ijerph17218126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker, A. B. , & Demerouti, E. (2017). Job demands‐resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology, 22(3), 273–285. 10.1037/OCP0000056 [DOI] [PubMed] [Google Scholar]
- Barello, S. , Falcó‐Pegueroles, A. , Rosa, D. , Tolotti, A. , Graffigna, G. , & Bonetti, L. (2020). The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID‐19 emergency: a rapid review. International Journal of Public Health, 65(7), 1205–1216. 10.1007/S00038-020-01463-7/TABLES/2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boamah, S. A. , Read, E. A. , & Spence Laschinger, H. K. (2017). Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: A time‐lagged study. Journal of Advanced Nursing, 73(5), 1182–1195. [DOI] [PubMed] [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Coşkun Şimşek, D. , & Günay, U. (2021). Experiences of nurses who have children when caring for COVID‐19 patients. International Nursing Review, 68(2), 219–227. 10.1111/INR.12651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis, P. , Vraka, I. , Fragkou, D. , Bilali, A. , & Kaitelidou, D. (2021). Nurses' burnout and associated risk factors during the COVID‐19 pandemic: A systematic review and meta‐analysis. Journal of Advanced Nursing, 00, jan.14839. 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusti, E. M. , Pedroli, E. , D'Aniello, G. E. , Stramba Badiale, C. , Pietrabissa, G. , Manna, C. , Badiale, M. S. , Riva, G. , Castelnuovo, G. , & Molinari, E. (2020). The psychological impact of the COVID‐19 outbreak on health professionals: A cross‐sectional study. Frontiers in Psychology, 11(July), 1–9. 10.3389/fpsyg.2020.01684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, J. , Chen, J. , Fu, J. , Ge, X. , Chen, M. , & Liu, Y. (2016). Structural empowerment, job stress and burnout of nurses in China. Applied Nursing Research, 31, 41–45. 10.1016/j.apnr.2015.12.007 [DOI] [PubMed] [Google Scholar]
- Hu, D. , Kong, Y. , Li, W. , Han, Q. , Zhang, X. , Zhu, L. X. , Wan, S. W. , Liu, Z. , Shen, Q. , Yang, J. , He, H.‐G. , & Zhu, J. (2020). Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID‐19 outbreak in Wuhan, China: A large‐scale cross‐sectional study. EClinicalMedicine, 24, 100424. 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter, R. M. (2008). Men and women of the corporation: New edition. Basic Books. [Google Scholar]
- Karam, F. , Bérard, A. , Sheehy, O. , Huneau, M. C. , Briggs, G. , Chambers, C. , Einarson, A. , Johnson, D. , Kao, K. , Koren, G. , Martin, B. , Polifka, J. E. , Riordan, S. H. , Roth, M. , Lavigne, S. V. , Wolfe, L. , & Wisner, K. (2012). Reliability and validity of the 4‐item perceived stress scale among pregnant women: Results from the OTIS antidepressants study. Research in Nursing and Health, 35(4), 363–375. 10.1002/nur.21482 [DOI] [PubMed] [Google Scholar]
- Labrague, L. J. , & de los Santos, J. A. A. (2020). Fear of COVID‐19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 1–9. 10.1111/jonm.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake, E. T. (2002). Development of the practice environment scale of the nursing work index. Research in Nursing and Health, 25(3), 176–188. 10.1002/nur.10032 [DOI] [PubMed] [Google Scholar]
- Lake, E. T. , & Friese, C. R. (2006). Variations in nursing practice environments: Relation to staffing and hospital characteristics. Nursing Research, 55(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Laschinger, H. K. S. , Finegan, J. , Shamian, J. , & Wilk, P. (2001). Impact of structural and psychological empowerment on job strain in nursing work settings: Expanding Kanter's model. Journal of Nursing Administration, 31(5), 260–272. 10.1097/00005110-200105000-00006 [DOI] [PubMed] [Google Scholar]
- Maslach, C. , Jackson, S. , & Leiter, M. (1996). MBI: Maslach Burnout Inventory (3rd ed.). CA: Consulting Psychologists Press Inc. [Google Scholar]
- Moreno‐Jiménez, J. E. , Blanco‐Donoso, L. M. , Chico‐Fernández, M. , Belda Hofheinz, S. , Moreno‐Jiménez, B. , & Garrosa, E. (2021). The job demands and resources related to COVID‐19 in predicting emotional exhaustion and secondary traumatic stress among health professionals in Spain. Frontiers in Psychology, 12, 564036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murat, M. , Köse, S. , & Savaşer, S. (2021). Determination of stress, depression and burnout levels of front‐line nurses during the COVID‐19 pandemic. International Journal of Mental Health Nursing, 30(2), 533–543. 10.1111/inm.12818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranney, M. L. , Griffeth, V. , & Jha, A. K. (2020). Critical supply shortages—The need for ventilators and personal protective equipment during the Covid‐19 pandemic. New England Journal of Medicine, 382(18), e41. 10.1056/nejmp2006141 [DOI] [PubMed] [Google Scholar]
- Sun, N. , Wei, L. , Shi, S. , Jiao, D. , Song, R. , Ma, L. , Wang, H. , Wang, C. , Wang, Z. , You, Y. , Liu, S. , & Wang, H. (2020). A qualitative study on the psychological experience of caregivers of COVID‐19 patients. American Journal of Infection Control, 48(6), 592–598. 10.1016/j.ajic.2020.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick, B. G. , & Fidell, L. S. (2007). Using Multivariate Statistics (7th ed.). Pearson. Retrieved from https://scholar.google.com/scholar?q=using%2Bmultivariate%2Bstatistics%2Btabachnick%2Bpdf&hl=en&as_sdt=0&as_vis=1&oi=scholart [Google Scholar]
- Tannenbaum, S. I. , Traylor, A. M. , Thomas, E. J. , & Salas, E. (2021). Managing teamwork in the face of pandemic: Evidence‐based tips. In BMJ Quality and Safety. BMJ Publishing Group. 10.1136/bmjqs-2020-011447 [DOI] [PubMed] [Google Scholar]
- Taris, T. W. , & Schaufeli, W. B. (2016). The Job Demands‐Resources Model. Retrieved from https://psycnet.apa.org/record/2015‐35805‐008 [Google Scholar]
- Travers, J. L. , Schroeder, K. , Norful, A. A. , & Aliyu, S. (2020). The influence of empowered work environments on the psychological experiences of nursing assistants during COVID‐19: A qualitative study. BMC Nursing, 19(1), 98. 10.1186/s12912-020-00489-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, S. , Liu, Y. , & Wang, L. (2015). Nurse burnout: Personal and environmental factors as predictors. International Journal of Nursing Practice, 21(1), 78–86. 10.1111/IJN.12216 [DOI] [PubMed] [Google Scholar]
- Wilczek‐Rużyczka, E. , Dębska, G. , Pasek, M. , & Zwierzchowska, M. (2019). The mediational effect of coherence on the relationship between mental load and job burnout among oncology nurses. International Journal of Nursing Practice, 25(3), e12736. 10.1111/IJN.12736 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). WHO and Partners Call for Urgent Investment in Nurses. Retrieved March 9, 2021, from https://www.who.int/news/item/07-04-2020-who-and-partners-call-for-urgent-investment-in-nurses [Google Scholar]
- World Health Organization . (2022a). WHO Coronavirus Dashboard. https://covid19.who.int/ [Google Scholar]
- World Health Organization . (2022b). Oman: WHO Coronavirus Disease (COVID‐19) Dashboard With Vaccination Data|WHO Coronavirus (COVID‐19) Dashboard With Vaccination Data. https://covid19.who.int/region/emro/country/om [Google Scholar]
- Wu, Y. , Zheng, J. , Liu, K. , Baggs, J. G. , Liu, J. , Liu, X. , & You, L. (2018). The associations of occupational hazards and injuries with work environments and overtime for nurses in China. Research in Nursing & Health, 41(4), 346–354. 10.1002/NUR.21882 [DOI] [PubMed] [Google Scholar]
- Yıldırım, M. , & Solmaz, F. (2020). COVID‐19 burnout, COVID‐19 stress and resilience: Initial psychometric properties of COVID‐19 burnout scale. Death Studies, 1–9. 10.1080/07481187.2020.1818885 [DOI] [PubMed] [Google Scholar]
- Zhang, X. , Ye, H. , & Li, Y. (2018). Correlates of structural empowerment, psychological empowerment and emotional exhaustion among registered nurses: A meta‐analysis. Applied Nursing Research, 42, 9–16. 10.1016/j.apnr.2018.04.006 [DOI] [PubMed] [Google Scholar]
- Zhou, T. , Xu, C. , Wang, C. , Sha, S. , Wang, Z. , Zhou, Y. , Zhang, X. , Hu, D. , Liu, Y. , Tian, T. , Liang, S. , Zhou, L. , & Wang, Q. (2022). Burnout and well‐being of healthcare workers in the post‐pandemic period of COVID‐19: A perspective from the job demands‐resources model. BMC Health Services Research, 22(1). 10.1186/S12913-022-07608-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


