Abstract
Objective
To determine the sensitivity of the Interagency Integrated Triage Tool to identify severe and critical illness among adult patients with COVID‐19.
Methods
A retrospective observational study conducted at Port Moresby General Hospital ED during a three‐month Delta surge.
Results
Among 387 eligible patients with COVID‐19, 63 were diagnosed with severe or critical illness. Forty‐seven were allocated a high acuity triage category, equating to a sensitivity of 74.6% (95% CI 62.1–84.7) and a negative predictive value of 92.7% (95% CI 88.4–95.8).
Conclusion
In a resource‐constrained context, the tool demonstrated reasonable sensitivity to detect severe and critical COVID‐19, comparable with its reported performance for other urgent conditions.
Keywords: COVID‐19, emergency care, Papua New Guinea, triage
Introduction
The World Health Organization (WHO) recommends a systematic approach to the management of ED patients with suspected and confirmed COVID‐19, including use of a ‘standardised triage tool’. 1 The only triage instrument specifically named in WHO's guidance is the Interagency Integrated Triage Tool (IITT), a colour‐coded, three‐tier system recently developed by the WHO, International Committee of the Red Cross and Médecins Sans Frontières. 1 , 2
Although the IITT has demonstrated acceptable performance in a pre‐pandemic context, its ability to identify COVID‐19 patients with urgent care needs has not been assessed. 3 , 4 The present study sought to determine the sensitivity of the tool to detect severe and critical COVID‐19 in a resource‐constrained setting.
Methods
This retrospective observational study was a planned sub‐study of a broader project evaluating the IITT. It was conducted in the ED of Port Moresby General Hospital (PMGH) in Papua New Guinea (PNG).
The study was undertaken between September and November 2021, coinciding with the incursion of the Delta variant and the country's third wave (Fig. 1). The period was characterised by overwhelming demands for care, limited bed capacity and severe staff shortages. All patients aged ≥18 years who presented during the study period and were diagnosed with COVID‐19 prior to leaving the ED were eligible. Patients were excluded if their triage category or illness severity was not recorded.
Figure 1.
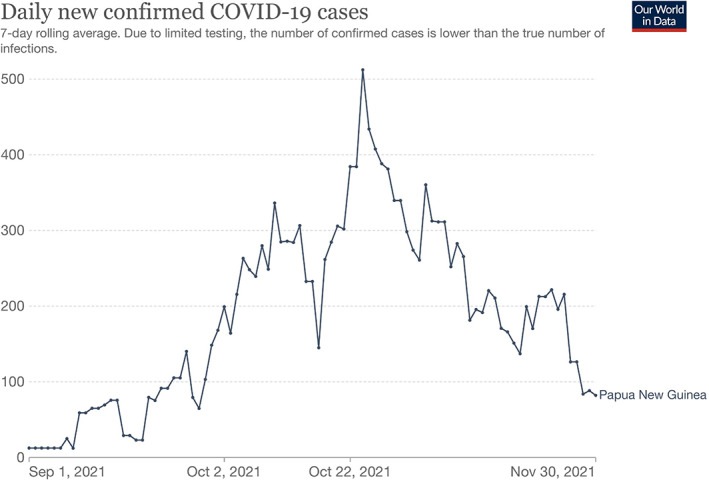
Daily new confirmed COVID‐19 cases in Papua New Guinea, September–November 2021. Source: Our World in Data/Johns Hopkins University Center for Systems Science and Engineering.
The primary outcome was IITT sensitivity to identify COVID‐19 patients with urgent care needs, defined as severe or critical illness based on PNG and WHO criteria (Table 1). 1 By definition, these patients require oxygen therapy and may need other time‐sensitive interventions. 1 Severity assessment was performed by the treating clinician and recorded on a clinical form, usually at the point of ED departure.
TABLE 1.
Summary of Papua New Guinea COVID‐19 severity definitions for adult patients, derived from the World Health Organization criteria 1
| Severity | Clinical syndrome | SpO2 (%) on room air | Respiratory rate (bpm) |
|---|---|---|---|
| Mild | Clinical symptoms of COVID‐19 without evidence of pneumonia | ≥90% | Within normal limits |
| Moderate | Clinical signs of pneumonia (e.g. cough or dyspnoea) without evidence of severe disease | ≥90% | <30 |
| Severe | Clinical signs of pneumonia with hypoxia, tachypnoea or respiratory distress | <90% | ≥30 |
| Critical | Severe disease requiring mechanical ventilation, or severe disease with sepsis or septic shock | N/A | N/A |
The tool's specificity and negative predictive value were calculated as secondary outcomes. Although triage is primarily concerned with sensitivity (i.e. detecting all patients requiring urgent care), in a surge context, the ability of a triage tool to identify low‐risk patients who can safely wait is valuable. This allows for optimal use of resources, ensuring that well patients are not unnecessarily streamed to a high‐acuity area.
To assess these outcomes, a dichotomised triage categorisation was used, with red and yellow ‘positive’ and green ‘negative’. To calculate specificity, patients with mild or moderate illness (i.e. no oxygen requirement, as per Table 1) were considered ‘non‐urgent’. Performance characteristics were expressed as percentages with 95% confidence intervals (CI).
Data were exported from the ED's electronic registry and analysed in Stata v17 (College Station, TX, USA). Ethics approval was provided by Monash University Human Research Ethics Committee (reference 30128), with subsequent endorsement from PMGH executive leadership and the PNG Medical Research Advisory Committee (reference 22.18).
Results
During the study period, 4346 adult patients presented to PMGH ED and 479 (11.0%) were diagnosed with COVID‐19. Of these, 387 (80.8%) had triage and severity data recorded and were included in the analysis. The mean age was 46.5 (SD 14.1) and 161 (41.6%) were female.
Overall, 63 patients (16.3%) were assessed as having severe or critical COVID‐19. Of these, 47 were allocated a red or yellow triage category, equating to a sensitivity of 74.6% (95% CI 62.1–84.7). The corresponding specificity (the proportion of mild and moderate patients allocated a green triage category) was 62.7% (95% CI 57.1–67.9). The negative predictive value was 92.7% (95% CI 88.4–95.8).
Discussion
In this single‐centre study, the IITT demonstrated reasonable sensitivity to identify patients with severe and critical COVID‐19. The tool's specificity was sub‐optimal but reflects that the purpose of triage is to capture all patients with urgent care needs, such that a degree of ‘over‐triage’ is to be expected.
The IITT has shown similar performance for urgent non‐COVID conditions. Previous studies have determined the tool's sensitivity to be 70.8% and 77.8% for identifying patients with time‐sensitive diagnoses such as acute coronary syndrome and ruptured ectopic pregnancy. 3 , 4 Collectively, these figures are within the performance range of other triage systems to detect critical illness. 5 For instance, a recent systematic review reported the sensitivity of established triage tools to identify severe sepsis as between 36% and 74%. 5
The sensitivity observed in the present study may reflect the duration of care at PMGH ED. During the study period, the average ED length of stay for COVID‐19 patients was 37.2 h, so it is probable that some deteriorated between arrival (when a triage category was assigned) and departure (when their severity was documented). The lower specificity likely reflects the presence of ‘red flag’ symptoms (such as chest pain) among some patients with mild and moderate illness.
Study limitations include incomplete data and under‐reporting. Due to resource constraints, not all presentations are likely to have been entered into the registry. Notwithstanding these issues, the findings suggest that the IITT is detecting most COVID‐19 patients who stand to benefit from timely assessment. Staff managing green patients should be aware that, based on the negative predictive value, approximately 7% will require escalation of care for severe illness.
Conclusion
In the resource‐constrained context of PMGH ED, the IITT's sensitivity to identify COVID‐19 patients with severe and critical illness was comparable with the reported performance of triage tools to detect time‐sensitive conditions.
Acknowledgements
The authors would like to acknowledge all ED clinicians at PMGH who have contributed to the care of COVID‐19 patients throughout the pandemic. Implementation of the IITT at PMGH was undertaken as part of the Clinical Support Program (Phase II), facilitated by Johnstaff International Development on behalf of the Australian Government through the PNG‐Australia Partnership. RM is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship and a Monash Graduate Excellence Scholarship; GOR is supported by a NHMRC Early Career Research Fellowship; and PC is supported by a Medical Research Future Fund Practitioner Fellowship. Funders had no role in study design, results analysis or manuscript preparation. Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Author contributions
RM was primarily responsible for registry development, data analysis and manuscript preparation. CK, RT, DS, MK, JP, SK and BJ were essential local collaborators and played important roles in triage operation and care of COVID‐19 patients during the study period. SB, LE, CB and SK supported implementation of new triage, streaming and data processes, while GOR and PC provided advice on planning, analysis and interpretation. All co‐authors reviewed the manuscript.
Competing interests
GOR and PC are section editors for Emergency Medicine Australasia.
Data availability statement
The data that underpin these findings may be released in de‐identified form following reasonable written request to the corresponding author and PMGH.
References
- 1. World Health Organization. Living guidance for clinical management of COVID‐19. [Cited 11 Jan 2022.] Available from URL: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 [PubMed]
- 2. World Health Organization . Clinical care of severe acute respiratory infections – Tool kit. [Cited 1 Oct 2020.] Available from URL: https://www.who.int/publications/i/item/clinical-care-of-severe-acute-respiratory-infections-tool-kit
- 3. Mitchell R, Bue O, Nou G et al. Validation of the interagency integrated triage tool in a resource‐limited, urban emergency department in Papua New Guinea: a pilot study. Lancet Reg. Heal 2021; 13: 100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mitchell R, McKup JJ, Banks C et al. Validity and reliability of the interagency integrated triage tool in a regional emergency department in Papua New Guinea. Emerg. Med. Australas. 2022; 34: 99–107. [DOI] [PubMed] [Google Scholar]
- 5. Hinson JS, Martinez DA, Cabral S et al. Triage performance in emergency medicine: a systematic review. Ann. Emerg. Med. 2019; 74: 140–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that underpin these findings may be released in de‐identified form following reasonable written request to the corresponding author and PMGH.


