Abstract
Purpose
Mandatory COVID‐19 shelter‐in‐place (SIP) orders have been imposed to fight the pandemic. They may also have led to unintended consequences of increased use of controlled substances especially among rural communities due to increased social isolation. Using the data from the American Association of Poison Control Centers, this study tests the hypothesis that the poison control centers received higher rates of calls related to exposures to controlled substances from rural counties than they did from urban counties during the SIP period.
Methods
Call counts received by the poison control centers between October 19, 2019 and July 6, 2020 due to exposure to controlled substance (methamphetamine, opioids, cocaine, benzodiazepines, and other narcotics) were aggregated to per‐county‐per‐month‐per‐10,000 population exposure rates. A falsification test was conducted to reduce the possibility of spurious correlations.
Findings
During the study period, 2,649 counties in the United States had mandatory SIP orders. The rate of calls reporting exposure to any of the aforementioned controlled substances among the rural counties was higher (14%; P = .047) relative to the urban counties. This overall increase was due to increases in the rates of calls reporting exposure to opioids (26%; P = .017) and methamphetamine (39%; P = .077). Moreover, the rate of calls reporting exposures at home was also higher among the rural counties (14%; P = .069).
Conclusion
The mandatory SIP orders may have had an unintended consequence of exacerbating the use of controlled substances at home in rural communities relative to urban communities.
Keywords: drug abuse, health law, mental health, observational data, policy
INTRODUCTION
The COVID‐19 pandemic has caused marked human suffering and societal burden, with many countries around the world continuing to struggle with the rapidly spreading virus. One of the most commonly adopted methods by governments to prevent the spread of the virus during early periods of the pandemic has been mandatory shelter‐in‐place (SIP) orders, which seeks to limit physical interactions in the population by requiring individuals to remain in their homes. 1 , 2 , 3 , 4 One criticism of mandatory SIP orders has been that it may lead to unintended adverse behavioral health outcomes. 5 , 6 Specifically, concerns have been expressed about the possibility that SIP may increase the likelihood that individuals are exposed to, and thus become habitual users of, controlled substances 7 , 8 due to increased social isolation or a lack of usual social and community structure (eg, going to work or school) that resulted in inactivity at home.
This concern may be especially relevant among rural communities because of their greater vulnerability to social isolation and higher prevalence of some substance use disorders. 9 “Death of Despair” is a term recently made popular by Case and Deaton, 10 who documented the increasingly higher rates of premature death among non‐Hispanic Whites residing in rural communities due to “self‐destructive behaviors,” 11 such as accidental poisoning from controlled substances, suicide, and liver diseases. 12 Such pre‐existing vulnerability among rural communities is likely to have contributed to exacerbation of substance use disorders among those communities after the implementation of SIP orders.
Therefore, this study tests the hypothesis that the unintended consequences of increased use of controlled substances among rural communities due to SIP orders were greater than those among urban communities. The current study seeks to test this hypothesis in the context of United States using a national dataset obtained from the American Association of Poison Control Centers (AAPCC). 13 Specifically, this study examines whether the poison control centers, which are located throughout the United States and serve all localities, received higher rates of calls from rural counties than they did from urban counties over a 3‐month period since the mandatory SIP orders became effective, taking into account the pre‐SIP baseline differences between the rural and urban counties via a difference‐in‐difference (DD) method. 14 The DD method used in this study exploits the cross‐sectional variation between urban and rural counties as well as the longitudinal variation between the pre‐ and post‐SIP periods within the urban and rural counties, respectively, to isolate the SIP impact, as explained below.
In theory, the mechanism that drives the association between poison control center call rates and the mandatory SIP orders is not obvious: higher rates of call may be driven by higher prevalence of substance use disorders due to SIP orders as hypothesized above or, alternatively, may reflect the impact of the SIP‐mandated closures of nearby health care facilities, which may have induced individuals to call the poison control centers as an alternative source of care. In other words, the former implies changes in individual behaviors due to SIP orders, whereas the latter does not. To determine which mechanism is more likely, therefore, a secondary hypothesis is also tested: rural communities that implemented SIP orders were more likely to report exposure to controlled substances taking place at home than their urban counterparts due to greater social isolation. Findings consistent with this secondary hypothesis will provide indirect evidence of changes in individual behaviors conducive to substance use disorders directly attributable to SIP orders.
METHODS
Data and variables
This study was approved by the University of Rochester's Institutional Review Board. The study team obtained all the relevant, deidentified data from 3 sources: AAPCC for the national data collected across all the poison control centers in the United States; a database recently compiled by Goolsbee and colleagues on COVID‐19 lockdown policies implemented at the state and local level as of May 16, 2020; 15 and Area Health Resources File (AHRF) to obtain 2019 county‐level population estimates and rural‐urban categorization. 16 The lockdown policy database and the AHRF data were available at state and county levels, and the study team merged them together by the Federal Information Processing Standard state and county codes to create a single county‐level data file. The lockdown policy data indicated that there were 493 US counties that had not yet implemented SIP orders by May 16, 2020 and that among the remaining 2,649 counties that did implement SIP orders, approximately 79% (2,083 out of 2,649) had ended SIP orders by June 15, 2020. This implied that among the 2,083 counties that had ended SIP orders by June 15, 2020, the average duration of SIP order was 45.2 days with standard deviation of 16.3 (range: 17‐80 days; interquartile range: 28‐58 days).
The poison center data were obtained from AAPCC's National Poison Data System, which has been collecting and maintaining all case data from the poison control centers across the United States for the purposes of epidemiological studies related to poison exposures since 1983. 13 , 17 The poison control centers provide free telephonic toxicology consultation services throughout the United States, and previous studies have shown correlations between changes in the poison control center call rates and corresponding changes in the rates of poisoning‐related hospitalization and Emergency Department (ED) visits, 18 , 19 which imply that the patterns of poisoning exposures captured by the poison control center data are likely to be reflective of true patterns of poisoning exposure observed in the community.
In the dataset obtained specifically for this study, the data represented all the calls made to the poison control centers in the United States between October 19, 2019 (ie, 150 days prior to the date of first SIP order issued among the counties, which was March 17, 2020) and July 6, 2020 (ie, 90 days after the date of last SIP order issued prior to May 16, 2020 among the counties, which was April 7, 2020). The study team chose to focus on a 150‐day pre‐SIP period and the subsequent 90‐day post‐SIP period because of the poison control center data availability (ie, the earliest available to the study team was October 1, 2019) and the fact that, as indicated above, about 79% of the counties that had implemented SIP orders had ended them within 90 days (max duration of 80 days). Therefore, the 90‐day post‐SIP period captured not only the entire duration of the SIP orders but also the subsequent several months after the end of the orders for the vast majority of the US counties that had issued SIP orders.
For the purposes of this study, opioids were of the primary interest due to extensive literature documenting the disproportionately high prevalence of opioid use disorder in rural communities. 20 However, because the literature also indicated that the use of opioids is often accompanied by the use of other controlled substances, 21 the calls that were associated with exposures to the following controlled substances were also considered: methamphetamine, cocaine, benzodiazepines, and “other narcotics,” which refers to all unknown narcotics as defined by AAPCC. The poison control center data contained detailed patient‐level information on the specific controlled substances to which the patients were exposed, site of exposure (ie, whether the exposure took place at the patients’ homes or other places), treatments rendered, as well as patient demographic information, including age and gender, along with the states and counties of patients’ residence.
Using the state and county information available in the poison control center data, the study team merged the county‐level data file created from the AHRF and the COVID‐19 lockdown policy database into the poison control center data, generating a single analytic data file. The prepost SIP period was defined by the dates on which either the state or the local governments imposed mandatory SIP orders; in cases where local governments had issued SIP orders earlier than the state governments or vice versa, only the earliest SIP order dates were considered for the purposes of this analysis.
Rural counties were defined based on the 2013 Rural‐Urban Continuum Codes (RUCC; available in the AHRF database) developed by the US Department of Agriculture's Economic Research Service. 22 Specifically, a county was defined as rural if it was classified either as completely rural or less than 2,500 urban population (code 8 or 9) or as nonmetropolitan urban not adjacent to a metropolitan area (code 5 or 7). This particular definition of rural counties was different from the standard definitions used by the US federal government 23 because the study team chose to consider a subset of nonmetro counties that are nonadjacent to metro counties or are adjacent but have no population center of even 2,500 people. This particular definition was chosen because the standard definitions reflect population sizes rather than degrees of social isolation experienced by communities. A sensitivity analysis was performed using an alternative definition of rural counties (ie, code 4 or greater) to determine whether the results and the overall conclusions would be different under this alternative definition.
Statistical analysis
To test the hypothesis that rural counties experienced higher rates of calls regarding exposure to controlled substances after the mandatory COVID SIP orders were issued, a DD method was used. 14 To do so, the patient‐level poison control center data were aggregated to capture county‐level counts of calls due to exposure to the aforementioned list of controlled substances. Among these calls, separate counts of calls by exposure site (ie, exposure at home vs not home) were also obtained to test the hypothesis that patients in rural counties were more likely to make calls related to the exposure to controlled substances at home after the COVID SIP orders were issued. For the purposes of testing these hypotheses, therefore, those states and counties that had not issued mandatory COVID SIP orders prior to May 16, 2020 were excluded from the sample, as their data do not contribute any variation relevant to these hypotheses.
For each county in the data, the study team considered 5 months (ie, 150 days) prior to and 3 months (ie, 90 days) after the SIP order date. Then, per‐county‐per‐month counts of calls were calculated for each 30‐day period before and after the SIP order date. Because variation in the per‐month counts of calls related to exposure differed by county population size, the per‐month counts of calls were further divided by the 2019 county population estimates to obtain per‐county‐per‐month‐per‐10,000 rates. These rates were then compared between the rural and urban counties in the data over the 3‐month period since the SIP order dates.
Because the post‐SIP 3‐month comparisons between the urban and rural counties were potentially confounded by pre‐SIP differences between them, the analysis took such differences into account by calculating the average differences between the rural and urban counties during the 5‐month pre‐SIP period and subtracting them from the post‐SIP 3‐month rural versus urban comparisons, which is consistent with the DD approach. 14 Moreover, because the DD method relies on the assumption of parallel trends, this assumption was tested using the 5‐month pre‐SIP data, and the results indicated that the assumption is likely to be valid in this context (the results are shown in online Table A1). The data were analyzed by fitting a Poisson model with the exposure parameter set to 2019 county population size in 10,000s. In addition, because the same counties were observed repeatedly over time, clustered standard errors were estimated to reflect the fact that standard errors are correlated across the same counties over time. 24 The statistical analyses were performed using Stata (version 15.1, College Station, TX).
The SIP order impact on the rates of calls to poison control centers related to control substance use was conceptualized as the difference between “Observed” and “Expected” rates. “Observed” referred to the rates calculated among the rural counties as directly observed from the data. “Expected” referred to the rates among the same rural counties that would be expected if they had followed the same trends as the urban counties in the data over the 3‐month post‐SIP period. Thus, the differences between the observed and expected rates represent the impact of the SIP order on the respective rates. For example, if the observed rates for rural counties were higher (or lower) than the expected rates after the SIP order, it would indicate that the SIP order was associated with increased (or decreased) rates of calls and thus increased (or decreased) exposure to controlled substances among the rural counties relative to the urban counties during the same period. Because the pre‐SIP period served as the reference category against which the subsequent post‐SIP periods were compared in the regression model, the expected rates among the rural counties during the pre‐SIP period were identical to the observed rates (ie, the pre‐SIP differences between the rural and the urban counties had been subtracted from all periods of comparison according to the DD approach).
A falsification test was conducted to reduce the possibility of a spurious correlation. As mentioned above, as of May 16, 2020, there was a relatively small number of counties that had not yet implemented any mandatory SIP order, either at the local or the state level. Although these counties were excluded from the main analysis, they served as a non‐SIP comparison group that could inform whether the associations observed in the main analysis might be spurious. Specifically, if significant differences between urban and rural counties were to be observed even among the counties that did not impose any mandatory SIP order, it would imply that the urban versus rural differences among the counties that had imposed the SIP orders––as estimated with the methods described above and in total or partially––were attributable to uncontrolled confounders rather than to the SIP orders.
Therefore, using a subsample consisted of only the non‐SIP counties (n = 493), the non‐SIP rural counties (n = 314) were compared against the non‐SIP urban counties (n = 179) in terms of the rate of exposure to all controlled substances considered in the main analysis using the identical Poisson regression model (see online Table A3 for the baseline comparison between the non‐SIP rural vs urban counties). For these non‐SIP counties, their post‐SIP index date was arbitrarily defined as March 19, 2020, which was the date of first state‐level mandatory SIP order issued in the United States due to COVID (California).
RESULTS
Table 1 summarizes the baseline differences between the rural and urban counts of calls related to exposure to controlled substances during the 5‐month period prior to the mandatory SIP orders being imposed. Excluding 493 counties that had not imposed mandatory SIP orders, there are 855 counties that were considered rural and 1,794 counties considered urban in the sample. The urban counties have population sizes that were on average 10 times larger than those of the rural counties. After adjusting for population size, the data suggest that the urban and rural counties were mostly comparable in call volume per capita at the baseline, albeit some differences that were statistically significant but relatively small in magnitude.
TABLE 1.
County characteristics during pre‐SIP 5‐month period
| Variable | Urban (n = 1,794) | Rural (n = 855) | P value |
|---|---|---|---|
| County population estimate in 2019 (in 10,000s; mean, SD) | 16.78 (42.94) | 1.68 (1.81) | <.001 |
| Poison control center call count: per‐county‐per‐month (mean, SD): | |||
| All narcotics | 4.305 (12.024) | 0.46 (1.006) | <.001 |
| Methamphetamine | 0.34 (1.979) | 0.065 (0.304) | <.001 |
| Opioid | 1.796 (6.399) | 0.182 (0.518) | <.001 |
| Cocaine | 0.237 (0.983) | 0.01 (0.103) | <.001 |
| Benzodiazepines | 2.223 (5.44) | 0.241 (0.643) | <.001 |
| Other narcotics | 0.14 (1.377) | 0.006 (0.088) | <.001 |
| Exposure at home | 3.71 (9.867) | 0.396 (0.883) | <.001 |
| Poison control center call rate: per‐county‐per‐month/10,000 population (mean, SD) | |||
| All narcotics | 0.249 (0.357) | 0.223 (0.58) | .007 |
| Methamphetamine | 0.027 (0.126) | 0.029 (0.172) | .568 |
| Opioid | 0.099 (0.205) | 0.094 (0.401) | .389 |
| Cocaine | 0.01 (0.049) | 0.005 (0.076) | <.001 |
| Benzodiazepines | 0.131 (0.224) | 0.113 (0.389) | .006 |
| Other narcotics | 0.005 (0.035) | 0.002 (0.03) | <.001 |
| Exposure at home | 0.219 (0.325) | 0.195 (0.552) | .009 |
Note: Excluded 493 counties that did not have SIP. P values were obtained via 2‐sample t‐tests.
Abbreviation: SD, standard deviation.
Table 2 shows the Poisson regression model estimates. The key coefficients are the interaction effects between the rural indicator variable and the post‐SID period indicator variables, which represent the DD estimates capturing the differential impacts of SID order among rural counties relative to the urban counties. The positive and statistically significant interaction effects indicate that since the SIP order implementation, the rural counties were associated with higher rates of calls to the poison control centers for cases involving the controlled substances considered in this study. Additionally, the results of a sensitivity analysis that used a different definition of rural counties (RUCC 4 or greater) are shown in online Table A2, suggesting that although some of the individual coefficients are no longer statistically significant, the overall conclusion remains unchanged.
TABLE 2.
Full Poisson regression model output including falsification test
| Covariate | Call count: all narcotic | Call count: methamphetamine | Call count: opioid | Call count: cocaine | ||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Is rural | 0.065 | .225 | 0.641 | .000 | 0.013 | .856 | −0.834 | .000 |
| Post‐SIP: month 1 | −0.157 | .000 | −0.231 | .013 | −0.172 | .000 | −0.168 | .009 |
| Post‐SIP: month 2 | −0.089 | .000 | −0.129 | .130 | −0.096 | .002 | −0.132 | .083 |
| Post‐SIP: month 3 | −0.067 | .002 | −0.315 | .001 | −0.042 | .191 | −0.124 | .042 |
| Rural × SIP month 1 | 0.032 | .591 | 0.394 | .016 | −0.024 | .811 | 0.073 | .845 |
| Rural × SIP month 2 | 0.133 | .041 | 0.161 | .344 | 0.135 | .171 | 0.355 | .304 |
| Rural × SIP month 3 | 0.133 | .047 | 0.329 | .077 | 0.230 | .017 | 0.252 | .485 |
| Constant | −1.360 | .000 | −3.899 | .000 | −2.234 | .000 | −4.261 | .000 |
| Covariate | Call count: benzodiazepines | Call count: other narcotic | Call count: exposure at home | Call count: all narcotic non‐SIP (n = 493) | ||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | P value | Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| Is rural | 0.082 | .120 | −0.796 | .016 | 0.063 | .196 | −0.025 | .785 |
| Post‐SIP: month 1 | −0.135 | .000 | −0.216 | .006 | −0.131 | .000 | −0.109 | .124 |
| Post‐SIP: month 2 | −0.078 | .000 | −0.007 | .930 | −0.063 | .002 | −0.145 | .027 |
| Post‐SIP: month 3 | −0.058 | .004 | 0.121 | .112 | −0.052 | .009 | −0.031 | .583 |
| Rural × SIP month 1 | −0.030 | .725 | 0.476 | .235 | 0.028 | .655 | −0.117 | .431 |
| Rural × SIP month 2 | 0.119 | .177 | 0.518 | .115 | 0.120 | .070 | 0.056 | .654 |
| Rural × SIP month 3 | 0.006 | .952 | 1.189 | .000 | 0.133 | .069 | −0.049 | .676 |
| Constant | −2.021 | .000 | −4.787 | .000 | −1.509 | .000 | −1.104 | .000 |
Figures 1 through 3 graphically summarize the DD estimates shown in Table 2 in terms of “observed” and “expected” call rates, as described above. Figure 1 suggests that across all controlled substances included in the analysis, rural counties were associated with higher call rates to poison control centers, particularly during the second and third months since the SIP order date, by approximately 14% (P < .05). Figure 1 also suggests that there is some evidence of rural communities having been more likely to report exposures at home than the urban counties, as indicated by approximately 13% higher call rates reporting exposures at home during the second and third months since the SIP order (P < .1). Moreover, the falsification test result as shown in Figure 1 indicates that there was no significant difference between the non‐SIP rural counties and the non‐SIP urban counties.
FIGURE 1.
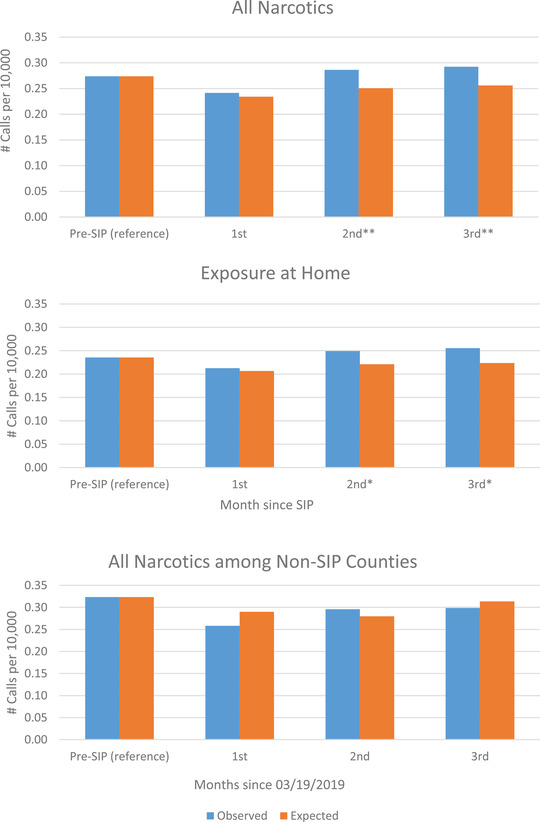
Rates of exposure to controlled substances among rural counties by month since SIP and exposure site. Data Source: AAPCC; estimated via Poisson regression model; *P < .1; **P < .05.
FIGURE 3.
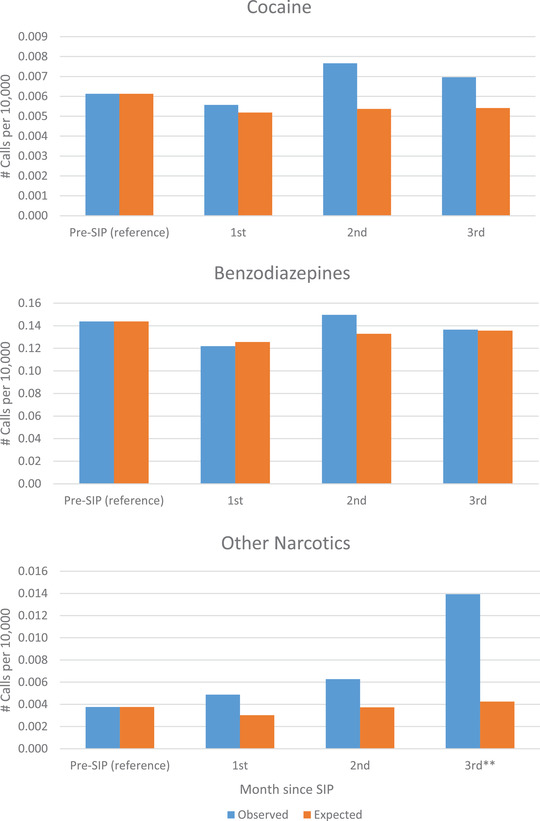
Rates of exposure to cocaine, benzodiazepines, and other narcotics among rural counties by month since SIP. Data Source: AAPCC; estimated via Poisson regression model; *P < .1; **P < .0.
Figure 2 suggests the rates of calls to poison control centers related to opioids and methamphetamine increased more among the rural counties relative to the urban counties during the post‐SIP period, particularly a couple of months after the SIP order started. For methamphetamine, the first month since the SIP order dates was associated with the largest increase, and the increases in the subsequent months remained significant at 10% level during the third month. Figure 3 indicates that there was no statistically significant difference between the rural and urban counties in calls related to benzodiazepine exposures in the 3 months following the SIP. However, a statistically significant difference in calls related to other narcotics was observed in the third month following the SIP for rural counties compared to urban counties. As well, calls related to cocaine exposure appeared to increase in the second month following the SIP for rural counties compared to urban counties, although this comparison did not reach statistical significance.
FIGURE 2.
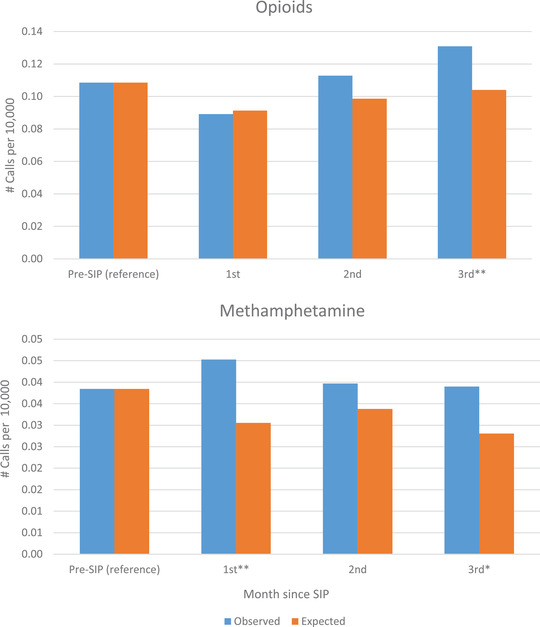
Rates of exposure to opioids and methamphetamine among rural counties by month since SIP. Data Source: AAPCC; estimated via Poisson regression model;*P < .1; **P < .05.
DISCUSSION
The results of this study provide empirical evidence in support of the hypothesis that individuals residing in rural communities were more likely to be exposed to controlled substances than those residing in urban communities, particularly to opioids and methamphetamine, after COVID‐19 SIP orders. This evidence is further supported by the finding that the SIP orders may have induced changes in individual behaviors that were conducive to greater prevalence of substance use disorders in the rural communities––that is, individuals in rural counties became more likely to stay home due to the SIP orders, as indicated by greater call rates reporting exposures at home. Therefore, the association between the higher poison control center call rates and the SIP orders cannot be entirely explained by the alternative hypothesis that the SIP orders may have induced individuals to substitute poison control centers for local health care providers due to SIP‐mandated closures without changing behavior. Furthermore, the falsification test results that showed no rural versus urban difference among the counties that did not impose SIP orders provide additional evidence that the SIP orders led to rural‐urban disparity in the rate of exposure to controlled substances.
As noted previously, however, the precise causal mechanism of how the SIP orders have led to the higher poison control center call rates among rural counties cannot be determined from the available data and, therefore, remains a subject of future research. During the SIP phase, for instance, emerging evidence suggests that telemedicine visits had replaced in‐person outpatient visits. 25 , 26 To the extent that rural communities face systematic barriers to telemedicine due to limited availability of technology and reliable internet access, 27 , 28 the higher call rates may, therefore, reflect disparities in access to telemedicine rather than increased use of controlled substances. At the same time, the fact that no such changes in access to care were imposed among the non‐SIP communities potentially explains the lack of rural versus urban disparity in the poison control center call rates among the non‐SIP counties as demonstrated in the falsification test.
Nevertheless, to the extent that the mandatory SIP orders might indeed have contributed to the increased rural versus urban disparity in substance use disorder as suggested by this study, 2 possible explanations are discussed below: increased risk of exposure at home due to job losses associated with the SIP orders, and spatial and geographical factors that uniquely impact rural communities relative to urban communities. Due to the SIP orders, which have resulted in involuntary job losses and workplace closures, more people have been forced to remain at home, leading to a scenario that may lead to greater illicit drug use due to boredom and inactivity, social isolation, among other factors. Because unemployment is more prevalent and chronic in rural communities, 29 , 30 loss of even just a handful jobs in those communities may imply a more amplified risk of exposure in rural areas.
Another possible explanation is the spatial and geographical factors in rural communities that uniquely impact their social interactions relative to urban communities. Showalter et al 31 have examined the patterns of individual mobility based on the geo‐positioning data obtained from mobile devices and have found that during the period of SIP orders, rural communities were associated with a higher degree of mobility than nonrural communities. The authors of this study cite the usual need for long travels among the residents of rural communities to obtain basic necessities, such as food and other essential items, which was exacerbated during the mandatory SIP orders because of closures of nearby businesses. As a result, residents of rural communities may have been forced to travel even longer distances to obtain such basic necessities. This implies that for those who remained at home, there was more time to spend in isolation at home without family supervision, resulting in greater loneliness and thus a greater risk of exposure to illicit substances at home. Future studies are needed to identify and confirm the exact underlying mechanisms that explain the reported patterns shown in the data.
This study is limited by its observational nature and a lack of more granular individual and household‐level data that would allow a more detailed examination of why such rural versus urban disparity exists. Furthermore, the poison control center data do not represent all incidences of substance use disorder cases in the community, as the data include only those cases for which phone calls were made to poison control centers. The data, therefore, represent only a subset of all the substance use disorder cases in the community. Nevertheless, to the extent that the goal of study is not to capture all cases of substance use disorder but rather to describe the changes in patterns of substance use disorder cases over time, the results of this study are still valid.
Moreover, this study does not address a broader question about whether mandatory SIP orders contribute to overall increases in exposure to controlled substances in the general population, regardless of the rural or urban status, which is an area of future study. To answer this broader question using the available data is challenging because of the relatively small number of counties that never implemented SIP orders––which would serve as the logical comparison group in such an analysis––and the inherent difficulty of accounting for unobserved heterogeneity that would confound any differences between the counties that had implemented SIP orders and those that never did, such as cultural attitudes and ideological proclivities toward government‐enforced mandatory policies. Lastly, although the patterns by substance type and month since the SIP order dates are suggestive of potentially interesting insights, it is difficult to interpret and explain them fully given the available data. As such, future studies are needed to address them in greater details.
CONCLUSION
The mandatory SIP orders that were designed to prevent the spread of COVID‐19 may have had an unintended consequence of exacerbating the use of controlled substances at home in rural communities, which had been vulnerable to high prevalence of substance use disorders even before the COVID pandemic. Policymakers and public health stakeholders should take into consideration such disparity in implementing future SIP orders.
DISCLOSURE
This study was funded by the Rural Communities Opioid Response Program (RCORP) Rural Centers of Excellence (RCOE) on Substance Use Disorder, which is supported by the Health Resources and Services Administration (HRSA) of the United States Department of Health and Human Services (HHS) as part of an award totaling $12.3M with 0% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by HRSA, HHS, or the US Government.
Supporting information
Appendix
Maeng D, Li Y, Lawrence M, et al. Impact of mandatory COVID‐19 shelter‐in‐place order on controlled substance use among rural versus urban communities in the United States. J Rural Health. 2022;1–9. 10.1111/jrh.12688
REFERENCES
- 1. Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID‐19 growth rate. Health Aff (Millwood). 2020;39(7):1237‐1246. [DOI] [PubMed] [Google Scholar]
- 2. Gupta S, Georgiou A, Sen S, Simon K, Karaca‐Mandic P. US trends in COVID‐19–associated hospitalization and mortality rates before and after reopening economies. JAMA Health Forum. 2021;2(6):e211262‐e211262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hsiang S, Allen D, Annan‐Phan S, et al. The effect of large‐scale anti‐contagion policies on the COVID‐19 pandemic. Nature. 2020;584(7820):262‐267. [DOI] [PubMed] [Google Scholar]
- 4. Lyu W, Wehby GL. Shelter‐in‐place orders reduced COVID‐19 mortality and reduced the rate of growth in hospitalizations. Health Aff (Millwood). 2020;39(9):1615‐1623. [DOI] [PubMed] [Google Scholar]
- 5. Kotwal AA, Holt‐Lunstad J, Newmark RL, et al. Social isolation and loneliness among San Francisco bay area older adults during the COVID‐19 shelter‐in‐place orders. J Am Geriatr Soc. 2021;69(1):20‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McGinty EE, Presskreischer R, Anderson KE, Han H, Barry CL. Psychological distress and COVID‐19‐related stressors reported in a longitudinal cohort of US adults in April and July 2020. JAMA. 2020;324(24):2555‐2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Panchal N, Kamal R, Cox C, Garlfield R. The Implications of COVID‐19 for Mental Health and Substance Use. 2021.
- 8. Rosenbaum J, Lucas N, Zandrow G, et al. Impact of a shelter‐in‐place order during the COVID‐19 pandemic on the incidence of opioid overdoses. Am J Emerg Med. 2021;41:51‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rural Mental Health: Issues, Policies, and Best Practices. Springer Publishing Company; 2012. [Google Scholar]
- 10. Case A, Deaton A. Rising morbidity and mortality in midlife among white non‐Hispanic Americans in the 21st century. Proc Natl Acad Sci USA. 2015;112(49):15078‐15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stein EM, Gennuso KP, Ugboaja DC, Remington PL. The epidemic of despair among white Americans: trends in the leading causes of premature death, 1999–2015. Am J Public Health. 2017;107(10):1541‐1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Erwin PC. Despair in the American Heartland? A focus on rural health. Am J Public Health. 2017;107(10):1533‐1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gummin DD, Mowry JB, Beuhler MC, et al. Annual report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 37th annual report. Clin Toxicol (Phila). 2020;58(12):1360‐1541. [DOI] [PubMed] [Google Scholar]
- 14. Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference‐in‐differences approach. JAMA. 2014;312(22):2401‐2402. [DOI] [PubMed] [Google Scholar]
- 15. Austan G, Nicole Bei L, Roxanne N, Chad S. COVID‐19 Lockdown Policies at the State and Local Level. Becker Friedman Institute for Research in Economics; 2020. [Google Scholar]
- 16. Area Health Resources Files . Health Resources and Services Administration. https://data.hrsa.gov/topics/health‐workforce/ahrf. 2020. Accessed August 24, 2021.
- 17. Litovitz T, Veltri JC. 1984 Annual report of the American Association of Poison Control Centers National Data Collection System. Am J Emerg Med. 1985;3(5):423‐450. [DOI] [PubMed] [Google Scholar]
- 18. Zaloshnja E, Miller T, Jones P, et al. The potential impact of poison control centers on rural hospitalization rates for poisoning. Pediatrics. 2006;118(5):2094‐2100. [DOI] [PubMed] [Google Scholar]
- 19. Zaloshnja E, Miller T, Jones P, et al. The impact of poison control centers on poisoning‐related visits to EDs–United States, 2003. Am J Emerg Med. 2008;26(3):310‐315. [DOI] [PubMed] [Google Scholar]
- 20. Rigg KK, Monnat SM, Chavez MN. Opioid‐related mortality in rural America: geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018;57:119‐129. [DOI] [PubMed] [Google Scholar]
- 21. Compton WM, Valentino RJ, DuPont RL. Polysubstance use in the U.S. opioid crisis. Mol Psychiatry. 2021;26(1):41‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. USDA . Rural‐Urban Continuum Codes. 2020.
- 23. Svynarenko R, Lindley LC. Defining rurality in hospice research: evaluation of common measures. J Health Care Poor Underserved. 2021;32(4):2167‐2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Austin N, Mark ES. Clustered Standard Errors in Stata. Stata Users Group; 2007. [Google Scholar]
- 25. Weiner JP, Bandeian S, Hatef E, Lans D, Liu A, Lemke KW. In‐person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the COVID‐19 pandemic. JAMA Netw Open. 2021;4(3):e212618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Patel SY, Mehrotra A, Huskamp HA, Uscher‐Pines L, Ganguli I, Barnett ML. Trends in outpatient care delivery and telemedicine during the COVID‐19 pandemic in the US. JAMA Intern Med. 2021;181(3):388‐391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Annaswamy TM, Verduzco‐Gutierrez M, Frieden L. Telemedicine barriers and challenges for persons with disabilities: COVID‐19 and beyond. Disabil Health J. 2020;13(4):100973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lopez AM, Lam K, Thota R. Barriers and facilitators to telemedicine: can you hear me now? Am Soc Clin Oncol Educ Book. 2021;41(41):25‐36. [DOI] [PubMed] [Google Scholar]
- 29. Pickering K, Harvey MH, Summers GF, Mushinski D. Welfare Reform in Persistent Rural Poverty: Dreams, Disenchantments, and Diversity. Penn State University Press; 2021. [Google Scholar]
- 30. Henkel D. Unemployment and substance use: a review of the literature (1990–2010). Curr Drug Abuse Rev. 2011;4(1):4‐27. [DOI] [PubMed] [Google Scholar]
- 31. Showalter E, Vigil‐Hayes M, Zegura E, Sutton R, Belding E. Tribal mobility and COVID‐19. Proceedings of the 22nd International Workshop on Mobile Computing Systems and Applications. 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix


