Abstract
This study aimed to examine changes in depression and anxiety symptoms from before to during the first 6 months of the COVID‐19 pandemic in a sample of 1,339 adolescents (9–18 years old, 59% female) from three countries. We also examined if age, race/ethnicity, disease burden, or strictness of government restrictions moderated change in symptoms. Data from 12 longitudinal studies (10 U.S., 1 Netherlands, 1 Peru) were combined. Linear mixed effect models showed that depression, but not anxiety, symptoms increased significantly (median increase = 28%). The most negative mental health impacts were reported by multiracial adolescents and those under ‘lockdown’ restrictions. Policy makers need to consider these impacts by investing in ways to support adolescents’ mental health during the pandemic.
Keywords: COVID‐19, depression and anxiety, collaborative
There is widespread concern that child and adolescent mental health has worsened during the COVID‐19 pandemic (Branje & Morris, 2021; Golberstein et al., 2020; Guessoum et al., 2020; Holmes et al., 2020; Lee, 2020; Racine et al., 2020). Adolescence is a period of vulnerability to mental health disorders in general and internalizing (i.e., depression and anxiety) disorders in particular (Costello et al., 2011), with these disorders impacting health and functioning in other domains of life into adulthood (Ormel et al., 2017). The pandemic caused many large changes in factors that are known to be relevant to mental health, such as routines, family finances, and opportunities to socialize (Branje & Morris, 2021). Exploration of the social environment outside of the family and forming more adult‐like social relationships are key to healthy adolescent development (Nelson et al., 2016; Orben et al., 2020) and were complicated by pandemic‐related restrictions.
In the context of the COVID‐19 pandemic, several cross‐sectional studies from China showed higher anxiety and depression symptoms than expected based on statistics from prepandemic studies in Chinese children and/or adolescents (Duan et al., 2020; Xie et al., 2020; Zhou et al., 2020), and one longitudinal study showed increases in depression and anxiety symptoms in 13‐ to 16‐year‐old Australian adolescents (Magson et al., 2020). A British study reported longitudinal increases in depressive symptoms but not anxiety symptoms in late childhood (age 7–11 years; Bignardi et al., 2020). However, other papers reported no change in internalizing symptoms (Achterberg et al., 2021 or a reduction in risk for anxiety in early adolescents (Widnall et al., 2020). There is still limited evidence of longitudinal changes in mental health from before the pandemic to during the COVID‐19 pandemic in a large, diverse sample spanning all of adolescence (age 9–18).
Therefore, we aimed to examine to what extent depression and anxiety symptoms of adolescents have changed from before the pandemic to during the first six months of the COVID‐19 pandemic within a collaborative sample of over 1,300 adolescents from three countries.
Changes in youth mental health from before the pandemic to during the pandemic might differ by individual‐level factors, such as age and race/ethnicity. Testing these factors as moderators can help elucidate who is mostly at risk and requires support. Cross‐sectional studies have reported higher anxiety/depression symptom levels in older adolescents than in younger adolescents early in the pandemic (Duan et al., 2020; Zhou et al., 2020), but older adolescents are also at increased risk of depression and several anxiety disorders (e.g., generalized anxiety and panic disorder) outside of the context of the pandemic (Kessler et al., 2012). Therefore, previously‐reported results do not necessarily mean older adolescents show a greater change in mental health symptoms during the pandemic than younger adolescents. However, there might still be a reason to think different age groups have experienced the pandemic differently. For example, although the perceived importance of friend social support remains the same from earlier to later adolescence (Demaray & Malecki, 2003), older adolescents spend more time with peers than younger adolescents (Richards et al., 1998), which may be complicated by pandemic‐related restrictions. In addition, older adolescents might have higher needs for autonomy and independence (Wray‐Lake et al., 2010).
Similarly, racial disparities in the mental health of U.S. adolescents have been reported (Anderson & Mayes, 2010; McLaughlin et al., 2007), although there are inconsistent findings about which group is at highest risk (Bitsko et al., 2022). Surveys on mental health in U.S. adults show continued racial disparities during the COVID‐19 pandemic, with the “other race or multiple races” group having the highest levels of depression and anxiety symptoms (Centers for Disease Control and Prevention, 2021). However, it is unknown if Black, Indigenous, and People of Color (BIPOC) adolescents disproportionately display a difference in mental health during the pandemic relative to before the pandemic. If this is the case, it might reflect discrepancies in the exposure to stressors, such as family financial stress, having a family with (severe) COVID‐19 and discrimination, which may be associated with adolescents' well‐being. To elucidate these potential moderators, the second research question was:
Is any change in anxiety and depression symptoms moderated by the current age of the adolescent or by their race/ethnicity?
Disease burden and government regulations may also be associated with youth mental health. Thus, given the potential implications for policy decisions, it is important to test the extent to which disease burden and government regulation moderate any extant association between change in youth mental health from before to during the pandemic. For example, if government regulations are a significant moderator, mental health symptoms are more likely related to increased physical distancing; if disease burden is a moderator, stress about one's own or loved one's health is a potential mechanism. Cross‐sectional studies on Chinese youth reported that those from the hardest hit region, Hubei, had elevated mental health symptoms compared with the rest of the sample (Duan et al., 2020; Xie et al., 2020; Zhou et al., 2020). On the other hand, one of the few studies with multiple time points of mental health data during the pandemic included adolescents and adults from China and found no change in anxiety or depression symptoms from early February to March, when cases dramatically increased (although, only 19% of 1,738 participants had longitudinal data and no longitudinal analysis was done; Wang et al., 2020). Further, social support has been found to buffer against adolescents' internalizing symptoms during the pandemic (Bernasco et al., 2021; Magson et al., 2020). Social support is a general protective factor against mental illness (Taylor, 2011). Since adolescents are developmentally primed to explore the social environment outside of their family (Nelson et al., 2016; Orben et al., 2020), increased governmental restrictions that limit the opportunity for explorative behavior and social contact might be particularly impactful for adolescents. Therefore, the final research question was:
Is any change in anxiety and depression symptoms from before the pandemic to during the first six months of the pandemic moderated by the disease burden or strictness of government restrictions in the adolescents' county of residence?
To answer these questions, we combine data from 12 research groups across three countries (17 states and D.C. in the U.S., and the Netherlands and Peru), which measured anxiety and depression symptoms of 1,339 adolescents longitudinally before and during the first 6 months of the COVID‐19 pandemic.
METHODS
Samples and Participants
We used data from 12 ongoing longitudinal studies on adolescent development. Studies were required to primarily or solely include adolescent participants, have conducted at least one assessment prior to the pandemic and at least one assessment during the pandemic that inquired about anxiety or depression symptoms, and be willing and able to share data in the collaboration by summer 2020. All anxiety and depression measures were adolescent self‐reports, except when this was not available (Table 1). Participants aged 9.0–18.0 as of March 2020 were included. We chose this age range because we were interested in adolescence, which is generally considered to start at the onset of puberty and end when adult rights and responsibilities are obtained (Dahl et al., 2018). The final total sample included 3,948 data points (65% prepandemic) from 1,339 participants (59% female). The mean age at participants' earliest time point was 13.5 years (SD = 2.0; range 8.2–17.6), and the mean age at participants' most recent time point was 15.4 years (SD = 1.8; range 9.4–19.0). Race/ethnicity in the total sample was distributed as follows: 42.7% White, 15.9% Latino/Hispanic, 9.2% Biracial/Multiracial, 7.7% Black/African American, 2.5% Asian, 1.4% other race/ethnicity (including American Indian or Alaskan Native), 20.5% missing. See Measures for information on the categorization of race/ethnicity. Within the Biracial/Multiracial group, 54% did not have full details of the racial categories, but for the subgroup that had this information, all racial categories were represented (77% had White as one of their categories, 31% Latino/Hispanic, 38% Black/African American, 24% Asian, 33% other). The studies from Peru and the Netherlands (N = 180) did not collect race/ethnicity information; considering that and the context‐dependent meaning of racial/ethnic group differences, participants from non‐U.S. studies are in the “missing” category and were not included in race/ethnicity moderation analyses. For information on race/ethnicity (and socioeconomic status) by study, see Table S1.
TABLE 1.
Sample Characteristics for each of the Studies Included in the Collaborative Analysis
| Study | Main Location(s) | N | No. of Time Points a | Dates of Collection | % Female Sex | Age Range Across All Time Points | Community or Clinical Sample | Measure of Depressive Symptoms | Measure of Anxiety Symptoms |
|---|---|---|---|---|---|---|---|---|---|
| ARC | Lima, Peru | 109 | 2 | Oct 2019–May 2020 | 57 | 11.3–17.6 | Community | PROMIS Depression Scale | PROMIS Anxiety Scale |
| BLP | The Netherlands | 71 | 8 | July 2018–April 2020 | 62 | 10.6–18.0 | Community | None | POMS Tension |
| CAT | Maryland, US | 66 | 4 | June 2015–Sept 2020 | 53 | 8.4–17.8 | Autism spectrum disorder and controls | CBCL withdrawn/depressed (parent report) | SCARED |
| EFC | Texas, US | 108 | 2 | Nov 2016–July 2020 | 48 | 8.2–18.2 | Community (but oversampled those with mental illness) | None | MASC (pre)/CASPE‐negative emotion (mid) |
| KLG | California, US | 38 | 2 | March 2018–August 2020 | 100 | 8.3–13.2 | Community, Latina‐identifying | CDI‐II | SCARED |
| LIS |
Kentucky, US; Ohio, US; Virginia, US |
237 | 2 | August 2018–June 2020 | 44 | 14.9–18.0 | ADHD and controls | RCADS Depressed Mood Scale | RCADS Anxiety Scale |
| MFS | Missouri, US; Florida, US | 140 | 2 | Feb 2016–July 2020 | 51 | 10.0–18.0 | Community | CES‐DC | RCMAS |
| NT/TTP | North Carolina, US | 207 | 8 (n = 68) or 5 (n = 139) | Nov 2016–August 2020 | 53 | 11.2–17.4 | Community | Short MFQ | None |
| SDS | Texas, US | 63 | 2 | Jan 2019–July 2020 | 38 | 13.7–18.0 | Incarcerated youth, youth on probation, and nonarrested youth | None | RCADS Generalized Anxiety Scale |
| TAB | New York, US | 76 | 2 | March 2018–August 2020 | 55 | 12.0–16.4 | High risk for anxiety disorders | CDI (pre) | SCARED |
| TAG | Oregon, US | 174 | 4 | Jan 2016–April 2020 | 100 | 10.1–17.1 | Community | CES‐DC | SCARED‐R (pre)/GAD‐7 (mid) |
| TGR | California, US | 50 | 10 | Oct 2017–August 2020 | 60 | 13.6–18.2 | Depression and controls | PHQ‐9 | MASC‐2 (pre)/GAD‐7 (mid) |
Note. CASPE = COVID‐19 Adolescent Symptom & Psychological Experience; CDI = Child Depression Inventory; CES‐DC = Center for Epidemiological Studies—Depression scale for Children; GAD‐7 = General Anxiety Disorder‐7; MASC = Multidimensional Anxiety Scale for Children; MFQ = Mood and Feelings Questionnaire; PHQ‐9 = Patient Health Questionnaire‐9; POMS Tension = Tension Subscale of the Profile of Mood States; PROMIS = Patient‐Reported Outcomes Measurement Information System; RCADS = Revised Children's Anxiety and Depression Scale; RCMAS = Revised Children's Manifest Anxiety Scale; SCARED=Screen for Child Anxiety‐Related Emotional Disorders.
This is the number of assessment time points or waves, some participants might not have completed all of the time points. Also, how many of the time points were prepandemic and midpandemic could vary by participant within each study.
Since this paper describes a post hoc collaborative analysis, studies unsurprisingly varied in their sample characteristics such as the age range and the number of time points. Table 1 summarizes the sample characteristics for each study. For more detailed information on the study design, inclusion, and exclusion criteria of each study, see Table S2. All studies were approved by their local ethics review committees and data sharing for combined analyses was done in compliance with Health Insurance Portability and Accountability Act guidelines. Participants provided assent to participate and a parent/guardian provided informed consent, except for participants who were 18 years old, and provided informed consent.
Measures
Anxiety and depression measures varied between samples (Table 1); therefore, we made the a priori decision to convert scores into the proportion of maximum score (POMS), which can range from 0 to 1. The POMS is calculated as follows: (participant's score − minimum of scale)/(maximum of scale − minimum of scale). We chose POMS because it avoids problems inherent in creating z‐scores for longitudinal data, which depending on how standardization is done, can for example include obfuscation or removal of mean level differences, mean changes, or relative rank information (Moeller, 2015).
Any assessments completed prior to March 11, 2020, the day the World Health Organization declared a pandemic, were considered prepandemic symptoms. Age in all analyses was defined as the age of the adolescent in March 2020 in years with one decimal. Race/ethnicity information was available for samples from the U.S. only. If race and ethnicity were collected as separate variables, adolescents identifying as white Latino/Hispanic or Mexican/South‐American Latino/Hispanic were categorized as Latino/Hispanic, whereas Latino/Hispanic with another racial identity was categorized as multiracial.
Disease burden was measured as the number of daily cases and deaths per 1 M people in the participant's county (U.S.) or city/province (outside the U.S.) averaged over the 7 days up to the date of assessment. This information was pulled from the database of the Johns Hopkins University for U.S. data (Dong et al., 2020) and based on national government reporting for studies outside the U.S. (OpenInfo, n.d.; Peru Ministerio de Salud, n.d.). If participants had multiple mid‐pandemic time points, case rates, and death rates were averaged across those. The final case rate and death rate variables were square‐root transformed to reach an approximate Gaussian distribution.
The strictness of government restrictions on the date of assessment was measured at the state and county level for each participant using a scale from 1 to 5. Both state‐ and county‐level restrictions were coded to account for restrictions at both levels (e.g., a state‐wide stay‐at‐home order plus a county‐wide mask mandate). The most stringent restrictions in the participant's location were coded, such that, if county restrictions were more stringent than state restrictions, county restrictions were coded. If participants had multiple mid‐pandemic time points, the median was calculated across those. Level 1 indicated “no restrictions,” 2 “a few closures of businesses or public facilities, limited restrictions,” 3 “some business closures, restrictions in the size of gatherings,” 4 “more extensive business closures, gathering restrictions, social distancing, and masks,” and 5 “a stay‐at‐home order, non‐essential businesses closed, enforced masks, and social distancing.” Ratings were conducted by one of the lead authors of the paper (CC). A doctoral graduate assistant was asked to blind code a random sample of 150 of the data points, and the intraclass correlation coefficient (single measures) was .776.
Analyses
Analyses were conducted with lmerTest in R version 3.6.3 (Bates et al., 2015). Scripts are available on https://github.com/dsnlab/CAPE. We modeled the change in symptom levels (i.e., POMS) with the following linear mixed‐effects model: symptoms ~ Before_vs_DuringPandemic + timespan + Before_vs_DuringPandemic*timespan + sex + age + (1 | Study/ID) and comparing this to a baseline model without Before_vs_DuringPandemic and its interaction with timespan. Anxiety and depression symptoms were modeled separately. The Before_vs_DuringPandemic factor specifies if an observation was made before or during the pandemic and (1 | Study/ID) reflects the random intercept by the participant within the study, since the model has three levels (time points within participants within studies). The covariate timespan represents the time passed between a participant's earliest and latest assessment in years, and its main effect plus interaction with Before_vs_DuringPandemic allow us to test whether changes in symptoms occur independently of how much older a participant has gotten. We examined moderating effects of race/ethnicity by adding that variable and its interaction with Before_vs_DuringPandemic, using White as the reference racial category. We examined moderating effects of age by adding the interaction between age and Before_vs_DuringPandemic. Moderating effects of case rate, death rate, and government restrictions were tested by adding that (scaled) individual‐level variable and its interaction with Before_vs_DuringPandemic. Model fit of each of these interaction models was compared with the main model, laid out in the equation above, with likelihood ratio tests. This is to examine whether model fit significantly improves with the addition of the new predictors; if not, then we prefer the simpler model. Fit statistics of the best fitting model are reported. Since we used two measures to examine the construct disease burden, a Bonferroni correction was applied across the models for case rate and death rate, adjusting the significance threshold to .025.
We additionally ran exploratory analyses to better understand if the observed changes in internalizing symptoms are distinguishable from general developmental increases in symptom levels. We calculated the slope of general developmental change in depression and anxiety symptoms by predicting symptom levels from age in prepandemic data only, controlling for sex. We then compared this with the Before_vs_DuringPandemic change from the main change model described above.
Finally, we ran post hoc “leave one out” (LOO) analyses and a meta‐analysis of the main change in depression and anxiety. We did this to examine whether any of the samples unduly impacted the findings or whether they are robust to variations between studies in sample composition, study design, and measures. For the LOO analyses, we repeated each of the analyses while leaving out one of the study samples at a time and reported whether the findings remained consistent with the analysis that includes all samples with data for that analysis. For the meta‐analysis, models of main change in depression and anxiety were run for every study sample separately, controlling for sex, age, and a random intercept by the participant. Next, pooled estimates were calculated using the metagen command in the meta package in R v3.6.3, applying restricted maximum likelihood to estimate between‐study variance. Considering the variation in study designs and the substantial between‐study variance, we focused on the random‐effects model.
RESULTS
Descriptive Information
The number of time points per participant ranged from 1 to 10 (median = 2). See Table 1 for information by study. Data were collected between January 2016 and September 2020. The median date of collection (DOC) for prepandemic data was 2 December 2018, and the median DOC of timepoints during the pandemic was 28 May 2020.
Daily case rates per 1 M (averaged over the week before assessment) ranged from 0 to 438.7 and daily death rates per 1 M ranged from 0 to 60.4. Case and death rates correlated moderately (ρ = .51). Government restriction levels ranged from 2 to 5 (i.e., all adolescents faced at least some restrictions). The restriction levels were negatively correlated with case rates (ρ = −.22) and not correlated with death rates (ρ = .00).
Main Change and Interaction with Age
The results demonstrated that depression, but not anxiety, symptoms significantly increased from before to during the pandemic (Tables 2 and 3, and Figures 1 and 2). The median POMS of depression symptoms, adjusted for repeated measures, increased from 0.195 to 0.250 (a 28% increase). The median POMS of anxiety symptoms was 0.234 prepandemic and 0.250 during the pandemic. The current age of the adolescent did not moderate the change in depression or anxiety symptoms. There was a significant interaction with timespan for anxiety symptoms: adolescents who were followed for a shorter time showed a decrease in anxiety symptoms from before to during the pandemic (Tables 2 and 3, and Figure 3). However, after removing the three samples that used a different anxiety symptom questionnaire prepandemic versus during the pandemic, this interaction disappeared and the baseline model was the best fitting model.
TABLE 2.
Model Fit Comparisons
| Model | AIC | BIC | Log Likelihood | p (vs. Model One Row Up) |
|---|---|---|---|---|
| Depression symptoms | ||||
| Baseline | −1556.1 | −1513.8 | 785.1 | NA |
| Main effect Before_vs_DuringPandemic | −1602.3 | −1547.9 | 810.1 | <.001 |
| Age interaction | −1600.4 | −1539.9 | 810.2 | .77 |
| Main effect Before_vs_DuringPandemic(full race data) | −1482.3 | −1429.0 | 750.2 | NA |
| Race interaction | −1487.5 | −1374.8 | 762.8 | .005 |
| Main effect Before_vs_DuringPandemic (full case rate data) | −1392.6 | −1339.1 | 705.3 | NA |
| Case rate interaction | −1410.5 | −1345.1 | 716.2 | <.001 |
| Main effect Before_vs_DuringPandemic (full death rate data) | −1392.6 | −1339.1 | 705.3 | NA |
| Death rate interaction | −1394.5 | −1329.1 | 708.2 | .05 |
| Main effect Before_vs_DuringPandemic (full restrictions data) | −1359.5 | −1306.0 | 688.7 | NA |
| Government restrictions interaction | −1364.3 | −1299.0 | 693.2 | .01 |
| Anxiety symptoms | ||||
| Baseline | −1993.2 | −1951.7 | 1003.6 | NA |
| Main effect Before_vs_DuringPandemic | −2038.4 | −1985.1 | 1028.2 | <.001 |
| Age interaction | −2039.2 | −1979.9 | 1029.6 | .10 |
| Main effect Before_vs_DuringPandemic (full race data) | −1746.1 | −1695.4 | 882.1 | NA |
| Race interaction | −1757.2 | −1650.1 | 897.6 | <.001 |
| Main effect Before_vs_DuringPandemic (full case rate data) | −1744.7 | −1692.8 | 881.3 | NA |
| Case rate interaction | −1745.1 | −1681.7 | 883.5 | .11 |
| Main effect Before_vs_DuringPandemic (full death rate data) | −1744.7 | −1692.8 | 881.3 | NA |
| Death rate interaction | −1742.4 | −1679.1 | 882.2 | .41 |
| Main effect Before_vs_DuringPandemic (full restrictions data) | −1730.0 | −1678.2 | 874.0 | NA |
| Government restrictions interaction | −1755.5 | −1692.2 | 888.7 | <.001 |
Note. AIC = Akaike information criterion; BIC = Bayesian information criterion.
P‐values bolded when meeting significance threshold.
TABLE 3.
Summaries of Fixed Effects of Best‐fitting Models of Main Time Effect and Age Interaction
| Model | Parameter | b | SE | t | p |
|---|---|---|---|---|---|
| Depression symptoms (level 3 ICC = 0.43) | Intercept | −0.005 | 0.07 | −0.07 | .95 |
| Before vs. during the pandemic | 0.04 | 0.01 | 2.70 | .01 | |
| Timespan | −0.01 | 0.007 | −1.55 | .12 | |
| Timespan interaction | 0.005 | 0.005 | 1.00 | .32 | |
| Sex (male) | −0.09 | 0.01 | −7.76 | <.001 | |
| Age | 0.02 | 0.004 | 4.20 | <.001 | |
| Anxiety symptoms (level 3 ICC = 0.56) | Intercept | 0.17 | 0.06 | 3.11 | .002 |
| Before vs. during the pandemic | −0.05 | 0.01 | −5.09 | <.001 | |
| Timespan | −0.03 | 0.006 | −4.24 | <.001 | |
| Timespan interaction | 0.03 | 0.005 | 7.00 | <.001 | |
| Sex (male) | −0.08 | 0.01 | −7.47 | <.001 | |
| Age | 0.01 | 0.003 | 3.66 | <.001 |
Note. ICC = intraclass correlation coefficient.
P‐values bolded when meeting significance threshold.
FIGURE 1.
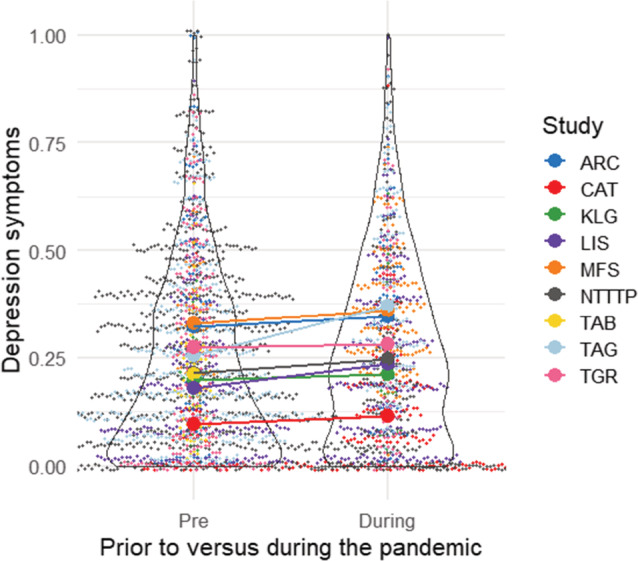
Depression symptoms prior to and during the pandemic in proportion of maximum score. Colors indicate which study the individual data points belonged to and the bigger dots depict means of each study at each time point, connected by a line. Note that jitter was added to visualize overlapping data points.
FIGURE 2.
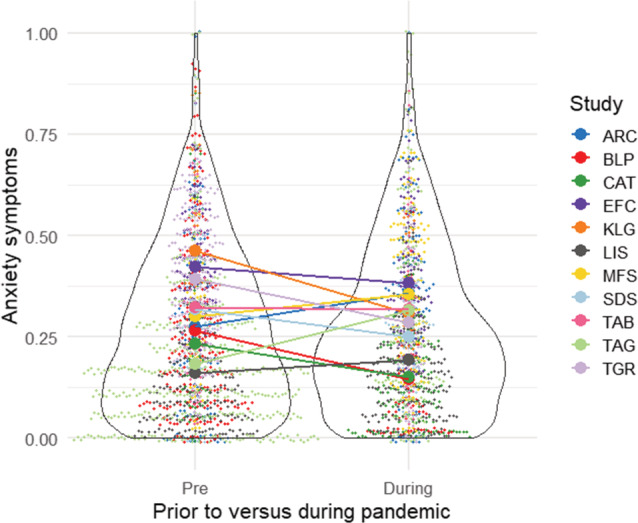
Anxiety symptoms prior to and during the pandemic in proportion of maximum score. Colors indicate which study the individual data points belonged to and the bigger dots depict means of each study at each time point, connected by a line. Note that jitter was added to visualize overlapping data points.
FIGURE 3.
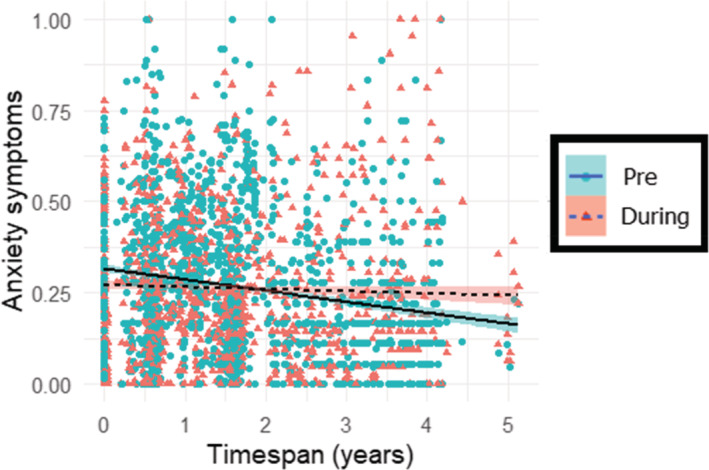
The change in anxiety symptoms from prior to (“Pre”) to during (“During”) the pandemic in relation to the timespan between earliest and latest assessment.
Race/Ethnicity
There was a significant interaction with race/ethnicity for both depression and anxiety symptoms. Biracial/multiracial adolescents were more likely to show increases in depression and anxiety symptoms, but Latino/Hispanic adolescents were less likely to increase in depression symptoms and more likely to decrease in anxiety symptoms. See Tables 2 and 4 and Figure 4 for details. Note that the models to test a race/ethnicity interaction were fit on a smaller dataset with only samples from the U.S. We reran the analysis without the three samples that used a different questionnaire prepandemic versus during the pandemic for anxiety symptoms, and the interaction model remained significant.
TABLE 4.
Summary of Fixed Effects of the Model with Race/Ethnicity Moderating the Time Effect on Depression and Anxiety Symptoms
| Outcome | Parameter | b | SE | t | p |
|---|---|---|---|---|---|
| Depression symptoms (level 3 ICC = 0.41) | Intercept | −0.02 | 0.08 | −0.25 | 0.80 |
| Before vs. during the pandemic | 0.04 | 0.02 | 2.60 | .01 | |
| Timespan | −0.01 | 0.01 | −1.71 | .09 | |
| Timespan interaction | 0.01 | 0.01 | 1.17 | .24 | |
| Sex (male) | −0.08 | 0.01 | −6.84 | <.001 | |
| Age | 0.02 | 0.01 | 3.61 | <.001 | |
| Asian | −0.03 | 0.03 | −0.93 | .36 | |
| Biracial/multiracial | 0.01 | 0.02 | 0.54 | .59 | |
| Black/African American | 0.00 | 0.02 | 0.17 | .87 | |
| Latino/Hispanic | 0.01 | 0.02 | 0.61 | .55 | |
| Other race | 0.01 | 0.04 | 0.22 | .83 | |
| Interaction of Asian and “before vs. during the pandemic” | 0.01 | 0.03 | 0.24 | .81 | |
| Interaction of biracial/multiracial and “before vs. during the pandemic” | 0.05 | 0.02 | 2.31 | .02 | |
| Interaction of Black/African American and “before vs. during the pandemic” | −0.06 | 0.02 | −2.57 | .01 | |
| Interaction of Latino/Hispanic and “before vs. during the pandemic” | −0.04 | 0.02 | −2.13 | .03 | |
| Interaction of other race and “before vs. during the pandemic” | −0.07 | 0.05 | −1.39 | .17 | |
| Anxiety symptoms (level 3 ICC = 0.58) | Intercept | 0.24 | 0.07 | 3.61 | <.001 |
| Before vs. during the pandemic | −0.05 | 0.01 | −3.91 | <.001 | |
| Timespan | −0.02 | 0.01 | −3.21 | <.001 | |
| Timespan interaction | 0.04 | 0.01 | 7.35 | <.001 | |
| Sex (male) | −0.08 | 0.01 | −7.08 | <.001 | |
| Age | 0.01 | 0.00 | 1.91 | .06 | |
| Asian | 0.02 | 0.03 | 0.79 | .43 | |
| Biracial/multiracial | 0.03 | 0.02 | 2.07 | .04 | |
| Black/African American | 0.01 | 0.03 | 0.30 | .76 | |
| Latino/Hispanic | 0.03 | 0.02 | 1.56 | .12 | |
| Other race | 0.05 | 0.04 | 1.23 | .22 | |
| Interaction of Asian and “before vs. during the pandemic” | −0.05 | 0.03 | −2.07 | .04 | |
| Interaction of biracial/multiracial and “before vs. during the pandemic” | 0.04 | 0.02 | 2.20 | .03 | |
| Interaction of Black/African American and “before vs. during the pandemic” | −0.03 | 0.03 | −1.04 | .30 | |
| Interaction of Latino/Hispanic and “before vs. during the pandemic” | −0.05 | 0.02 | −2.70 | .01 | |
| Interaction of other race and “before vs. during the pandemic” | −0.04 | 0.04 | −0.88 | .38 |
Note. “White” was used as the reference category; no. of observations = 2782 for depression model and 2068 for anxiety model.
ICC = intraclass correlation coefficient.
P‐values bolded when meeting significance threshold.
FIGURE 4.
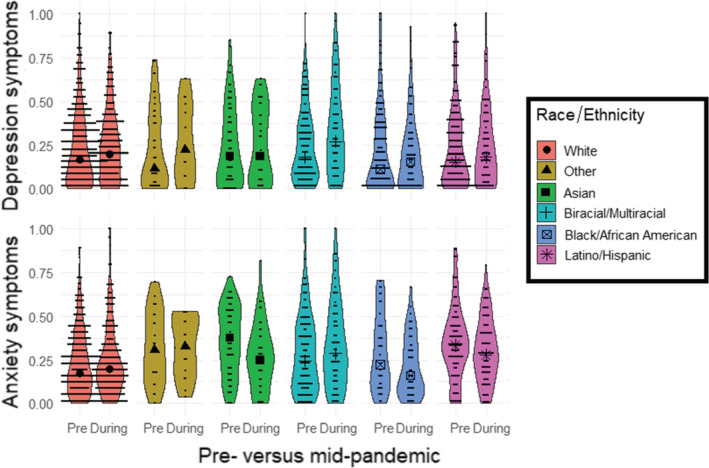
The change in symptoms from prior to (“Pre”) to during (“During”) the pandemic by race/ethnicity of the adolescent. The larger black symbol is the median for that racial/ethnic category and time point.
Disease Burden
We examined interactions between time and local case rates and death rates, which both reflect average daily rates across the week before assessment. For depression symptoms, there was a significant interaction with case rates, but not death rates: symptoms increased more for participants in areas with lower case rates (Tables 2 and 5 and Figure 5). The average within‐person increase in depression symptoms was 0.07 (on a scale from 0 to 1) for those in regions with <100 cases per 1 M people in the week before assessment, but 0.01 for those in regions with >200 cases per 1 M. For anxiety symptoms, there was no significant interaction with case rates or death rates. The analysis for death rates was repeated without participants from the TAB study (from New York), since they were outliers, but this did not change the significance of the results.
TABLE 5.
Summaries of Fixed Effects of the Significant Models Including the Interaction with Case Rate
| Outcome | Predictor | Parameter | b | SE | t | p |
|---|---|---|---|---|---|---|
| Depression symptoms (level 3 ICC = 0.44) | Case rate | Intercept | −0.02 | 0.08 | −0.29 | .77 |
| Before vs. during the pandemic | 0.03 | 0.01 | 2.42 | .02 | ||
| Timespan | −0.01 | 0.009 | −1.40 | .16 | ||
| Timespan interaction | 0.005 | 0.005 | 0.86 | .39 | ||
| Sex (male) | −0.09 | 0.01 | −7.19 | <.001 | ||
| Age | 0.02 | 0.005 | 4.00 | <.001 | ||
| Case rate | 0.01 | 0.01 | 1.12 | .26 | ||
| Case rate interaction | −0.03 | 0.007 | −4.69 | <.001 |
Note. ICC = intraclass correlation coefficient.
P‐values bolded when meeting significance threshold.
FIGURE 5.
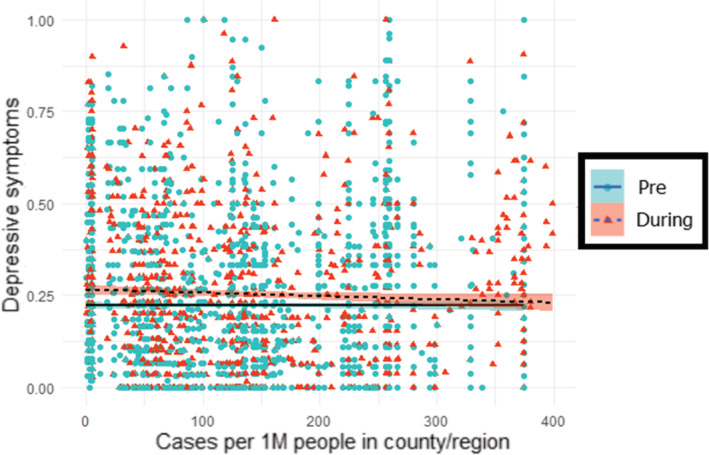
Changes in symptom levels in relation to case rates in the participant's county or region. Note that data from TAB were removed from this plot, since they formed an extreme outlier.
Government Restrictions
Change in both anxiety and depression symptoms was moderated by the strictness of government restrictions in the participant's county/region (Tables 2 and 6 and Figure 6). Depression symptoms increased more and anxiety symptoms decreased less for participants in regions with higher levels of government restrictions.
TABLE 6.
Summaries of Fixed Effects of the Significant Models Including the Interaction with Government Restriction Level
| Outcome | Parameter | b | SE | t | p |
|---|---|---|---|---|---|
| Depression symptoms (level 3 ICC = 0.44) | Intercept | −0.02 | 0.08 | −0.28 | .78 |
| Before vs. during the pandemic | 0.04 | 0.01 | 2.76 | .01 | |
| Timespan | −0.01 | 0.01 | −1.49 | .14 | |
| Timespan interaction | 0.00 | 0.01 | 0.51 | .61 | |
| Sex (male) | −0.09 | 0.01 | −7.52 | <.001 | |
| Age | 0.02 | 0.01 | 4.05 | <.001 | |
| Government restriction level | −0.01 | 0.01 | −0.66 | .51 | |
| Government restriction level interaction | 0.02 | 0.01 | 2.97 | <.001 | |
| Anxiety symptoms (level 3 ICC = 0.57) | Intercept | 0.15 | 0.06 | 2.53 | .01 |
| Before vs. during the pandemic | −0.04 | 0.01 | −4.32 | <.001 | |
| Timespan | −0.03 | 0.01 | −3.74 | <.001 | |
| Timespan interaction | 0.03 | 0.01 | 5.79 | <.001 | |
| Sex (male) | −0.08 | 0.01 | −7.16 | <.001 | |
| Age | 0.01 | 0.00 | 3.95 | <.001 | |
| Government restriction level | −0.01 | 0.01 | −1.28 | .20 | |
| Government restriction level interaction | 0.03 | 0.01 | 5.45 | <.001 |
Note. ICC = intraclass correlation coefficient.
P‐values bolded when meeting significance threshold.
FIGURE 6.
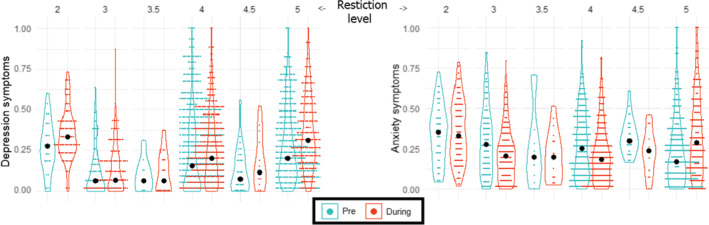
Changes in depression (left) or anxiety (right) symptoms in relation to government restriction levels in the participant's county or region. The larger black dots represent the median for that restriction level and time point.
Developmental Trends
For the depression model, the regression coefficient for Before_vs_DuringPandemic was 0.04, meaning that symptoms were 0.04 higher (on a scale from 0 to 1) during the pandemic compared with before. However, the time passed between the average prepandemic DOC (28th of September 2018) and the average DOC during the pandemic (31st of May 2020) was longer than a year (1.68 years), so the adjusted slope was 0.04/1.68 = 0.024. The regression coefficient of the model predicting prepandemic depression symptoms from age was 0.001, showing that the increase per year from before to during the pandemic was greater compared with the increase per year in prepandemic data. For the anxiety model, the adjusted slope for Before_vs_DuringPandemic was −0.05/1.68 = −0.03, whereas the age slope in prepandemic data was 0.01.
Post Hoc “Leave One Out” Analyses and Meta‐Analysis
Table 7 reports the findings of the “leave one out” (LOO) analyses. These analyses suggest that the reported findings are largely stable for depression, but less stable for main change, age interaction, and case rate interaction in relation to anxiety. Results of meta‐analytic tests of the main change in depression and anxiety symptoms confirmed that there was a significant increase in depression, but not in anxiety (Table S3).
TABLE 7.
Findings of “Leave One Out” Analyses, Indicating the Number of Times Findings Remained Consistent with the Original Analysis
| Analysis | Depression | Anxiety | ||
|---|---|---|---|---|
| # | Influential Samples | # | Influential Samples | |
| Main change | 9/9 | none | 4/11 | ARC, EFC, KLG, LIS, MFS, SDS, TAB |
| Age | 9/9 | none | 5/11 | ARC, BLP, MFS, SDS, TAG, TGR |
| Race/ethnicity | 7/8 | TAG | 9/9 | none |
| Case rate | 8/9 | TAG | 6/11 | ARC, BLP, MFS, SDS, TAG, TGR |
| Death rate | 5/9 | MFS, LIS, NTTTP, TGR | 9/11 | TAB, TAG |
| Government restrictions | 8/9 | TAG | 10/11 | TAG |
DISCUSSION
In the current study, we examined to what extent adolescents' depression and anxiety symptoms changed from before to during the first 6 months of the COVID‐19 pandemic. We also investigated to what extent any change in anxiety or depression symptoms was moderated by the current age or race/ethnicity of the adolescent, by the disease burden or by the strictness of government restrictions in the adolescents' county of residence. Depression symptoms increased significantly, with a median increase of 28%. Although we cannot be certain that the pandemic caused this increase in depression symptoms, and these symptoms also tend to rise with age outside of the context of the pandemic, the reported increase was independent of age at the start of the pandemic, it was independent of how much (or little) time had passed between the earliest and latest assessment, and it was greater in absolute terms than the age slope in prepandemic data. Importantly, this is one of the first studies to report a longitudinal change in mental health symptoms from before relative to during the COVID‐19 pandemic in a large sample of adolescents, spanning three continents and the full developmental span of adolescence.
Longitudinal assessment is crucial to understanding change in youth mental health over time. For example, Pan et al. (2020) reported that, cross‐sectionally, adults with a prior diagnosis of anxiety and/or depressive disorders had the greatest self‐perceived impact of the COVID‐19 pandemic on their well‐being. However, a longitudinal assessment of their symptoms showed that depression, anxiety, loneliness, and worry decreased or did not change, whereas each of these domains increased in adults without a history of mental illness. Although our sample differed from Pan and colleagues' (e.g., participants were primarily drawn from community samples; we did not distinguish based on the history of mental illness; our findings reflect an increase in subthreshold depression symptoms), our results were similar: youth depression symptoms, but not anxiety symptoms, increased on the aggregate.
Our results indicate anxiety symptoms decreased during the early months of the COVID‐19 pandemic, at least for those where the time between earliest and latest assessment was relatively short. However, this result was unstable in the LOO analyses and showed high variability between studies. This finding contrasts with previous cross‐sectional studies (Duan et al., 2020; Xie et al., 2020; Zhou et al., 2020) and a longitudinal study (Magson et al., 2020), which used a variety of anxiety scales (e.g., Spence Children's Anxiety Scale; Screen for Child Anxiety Related Emotional Disorders; Generalized Anxiety Disorder scale) among adolescents. There are several explanations for this discrepancy. First, anxiety is multifaceted: it is possible that some types of anxiety increased during the pandemic, whereas other types might have declined. For example, social anxiety may have temporarily subsided with fewer opportunities for social interactions and reduced social pressures, whereas generalized anxiety may have increased with the global pandemic, and several other local, national, and global events that took place during this time, especially in the U.S. The use of broad screening questionnaires in the majority of the included studies limited our opportunity to look at changes in specific forms of anxiety. Second, anxiety may have fluctuated during the course of the pandemic based on the contexts to which adolescents were exposed. For example, several standardized measures of anxiety include items that are difficult to endorse under local restrictions (e.g., “I get stomach aches at school”) and therefore may underreport experienced anxiety or may mask anxiety that has no behavioral expression when youth are largely at home. At the same time, returning to school and social activities might come with an increase in anxiety symptoms because of missed opportunities for exposure (Frenkel et al., 2015).
For both anxiety and depression, increases were strongest in multiracial adolescents, whereas Hispanic/Latino adolescents reported decreases/weaker increases than White adolescents, Black/African American adolescents showed smaller increases in depressive symptoms and Asian American adolescents decreased in anxiety. Although studies varied in their racial distribution (Table S1), these findings remained largely stable under the LOO analyses. These findings align with representative surveys in adults, which report the highest levels of depression and anxiety symptoms in the “other race or multiple races” group (Centers for Disease Control and Prevention, 2021). However, they do not align with the idea of a disproportionate increase in symptoms in all BIPOC adolescents. Further research is needed to examine the risk and resilience factors that could explain this mixed picture of stronger increases in symptoms for multiracial adolescents, but weaker increases or decreases for Black/African American and Hispanic/Latino adolescents.
The change in depression symptoms was moderated by the case rate, such that adolescents in areas with lower disease burden experienced a greater symptom increase. Although speculative, these results may be due to a mismatch between policies of restriction and actual case level. Restriction levels and case rates were negatively correlated in the current study, and stricter government restrictions were associated with more depression symptom increase. High local case rates across the last week thus did not appear to increase worries or distress across the last one to 2 weeks. This could be because adolescents are not focused on them, adolescents might not be exposed as much to these numbers or because they do not inform adolescents' mental state. Humans—particularly young people—often have difficulty intuitively understanding big numbers (Tretter et al., 2006), so case rates going from high to higher might not have a significant mental impact. Also, the risk of becoming physically ill from COVID‐19 (or to see that happening to loved ones) may not be a major factor affecting mental well‐being, as also shown by a study comparing older and younger adults' emotional well‐being (Carstensen et al., 2020): emotional well‐being during the pandemic was better in older adults than in young adults, despite older adults perceiving a higher risk of complications from COVID‐19.
Moderation by restriction levels on the other hand showed the opposite pattern: adolescents in areas with stricter government restrictions reported greater depression and anxiety symptom increase. This suggests that higher levels of government restrictions, and the social isolation and cancellations of in‐person activities (including regular schooling) that are the result of such restrictions, might be burdensome on adolescents' mental health. This is supported by a study that reported that changes in depression and anxiety symptoms were stronger in adolescents who felt socially disconnected (Magson et al., 2020) and aligns with findings in the UK from March 2020 to March 2021 showing an association between rates of mental health difficulties and pandemic‐related restrictions (Shum et al., 2021). It is also not surprising in light of the knowledge that adolescents are developmentally primed to explore their social environment and build connections outside their household (Nelson et al., 2016; Orben et al., 2020). A higher level of government restrictions, which captures, for example, limits on gathering sizes and social distancing (see Methods), directly limits the opportunities for this exploration and building of new connections. Future longitudinal research should examine whether adolescents with lower levels of social connectedness or support before the pandemic are more negatively affected during the pandemic.
These findings highlight the importance of considering adolescents' emotional well‐being in policy decisions for the remainder of the COVID‐19 pandemic and potentially future pandemics. Public health policymakers need to explicitly consider mental health impacts of their policies. For example, the American Academy of Pediatrics recommends the return to in‐person schooling and states that “School policies should be guided by supporting the overall health and well‐being of all children [and] adolescents” (https://bit.ly/2BMPtW5). Although the present study was not equipped to test the impact of school closures on adolescents' mental health specifically, Lee (2020) found that school closures exacerbated existing mental health issues among youth. Taken together with the results of the present study, disruptions to structure and opportunities for social interaction may be detrimental to youth mental health. Further, investing in sources of support to buffer negative mental health impacts, especially under “lockdown” or “stay‐at‐home” mandates, is warranted. For example, a predictable, stable home environment was protective of mental health during the COVID‐19 pandemic (Rosen et al., 2021). Overall, evidence is mounting that policy should focus on preserving normalcy and preventing disruptions in youth social structures, resources, and support to the extent that it is possible to do so in emergency situations.
Limitations
The findings of this study should be considered within the context of several limitations. Importantly, causality cannot be assumed from longitudinal studies like this one. Although depressive symptoms increased regardless of how much (or little) time had passed between the earliest and latest assessment, and the increase was greater in absolute terms than the slope in prepandemic data, we cannot be certain that these increases are caused by the pandemic. Further, the current dataset was a post hoc collaboration of studies with varying inclusion criteria, age ranges, and measures of anxiety and depression symptoms. We took several steps to correct for this site‐level variability as much as possible: converting symptom levels into the proportion of maximum score, including a random intercept by study, correcting for sex and current age in all analyses, and conducting a LOO sensitivity analysis. The proportion of maximum score has several advantages over z‐scores as described in the Methods, but we acknowledge that this approach also has limitations: maximum scores can have different meanings for different questionnaires. Also, unlike some studies in single samples, we applied mixed‐effects modeling, which reduces bias resulting from selective dropout or incomplete data compared with complete case analysis. Finally, the overall change in depression symptoms was also significant when tested with a meta‐analytic approach, suggesting it might be robust to the various sources of site‐level variability.
Also, some factors might have reduced the generalizability of the current findings. Most studies included a community sample, but four studies specifically recruited participants with or at‐risk for mental illness. Although these studies did not emerge as particularly influential in the LOO analyses, it does indicate that the prior mental illness burden in our sample might be higher than in the general population of adolescents. Second, two studies specifically recruited girls, leading to 59% female participants in the total sample. However, we control for sex in all analyses and the sample still has 549 males. Third, participants were mostly from middle‐class families (see Table S1 for the socioeconomic status [SES] information by study; we did not provide this information for the total sample because of the variation in measures and categories). Since the economic impact of the pandemic has been mostly felt by lower SES families, the mental health effects of families' financial problems might not have been well‐captured by the current study. Fourth, our racial distribution was close to that of the U.S. population of adolescents based on Census data of 10–17‐year‐olds (United States Census Bureau, 2019), with somewhat higher percentages of White and multiracial adolescents in the current sample. This may be partly due to classifying non‐White Latino/Hispanic adolescents as multiracial (7% of the multiracial group). We chose not to subdivide the group who identified as Latino/Hispanic, partly because not all studies had this data and partly because the number of racial categories was already large, limiting our power to detect differences. However, this means that the differences found are unlikely to be trivial. For 2 out of the 10 studies with race/ethnicity data, racial diversity was somewhat lower among participants who completed the surveys sent out during the pandemic compared with the original sample (Table 8), but there was no selective dropout for the majority of studies.
TABLE 8.
Response Rates and COVID‐sample Retention Rates per Study
| Study | Recruitment % | COVID Retention % | Difference by Age | Difference by Sex | Difference by Race |
|---|---|---|---|---|---|
| ARC | Unknown | 20.6 | NS | NS | N/A a |
| BLP | 82 | 37 | NS | Fewer males* b | NS b |
| EFC | Unknown | 60 | NS | NS | NS |
| KLG | Unknown | 100 | N/A | N/A | N/A |
| LIS | 82.1 | 90.8 | NS | NS | NS |
| MFS | Unknown | 37.3/42 | Lower age/NS* c | NS | */*More White, fewer Black |
| NT/TTP | 76.2/61 | 82/80.4 | NS/NS | NS/* d (more males) | NS/NS |
| SDS | 31.4 | 35.2 | NS | NS | NS |
| TAB | 22.0 | 56.3 | NS | NS | NS |
| TAG | 65 | 73 | NS | NS | NS |
| TGR | MDD: 57.7, control: 73 | 53.2* e | NS | NS | NS |
| CAT | 81 | 52 | NS | NS | Fewer Latinx/Hispanic* f |
Note. Percent recruitment rate is the percentage of people that indicated they were interested in the study out of the number of people originally contacted for the study at wave 1. For some studies that had exclusion criteria (e.g. MDD), the percent of people eligible to participate was smaller than total interest. Percent of COVID retention is the percentage of people who completed at least one COVID‐related measurement, compared out of the number of people contacted to participate in the COVID data collection. Age, sex, and race differences were calculated based on who participated in COVID‐related measurement vs. those contacted for COVID‐related measurement. NS = no significant difference between groups. N/A = not applicable; 100% contacted for COVID study, participated. Unknown = this information was not available based on recruitment methods (e.g. flyers in the community and entire school districts).
*Significant differences between people who participated in at least one COVID survey vs. who were contacted but did not participate in COVID surveys. For any group that had significant differences, the directions of those differences are shown below.
ARC did not collect information on race.
In BLP, females were more likely to respond to COVID study than males (no/yes: females 48/42; males 41/11). The test of differences by race (NS) was based on country of birth.
The MFS study contains two subsamples. University of Missouri sample: age (significantly lower age; COVID study M = 12.36, SD = 1.62; not in COVID‐study M = 12.92, SD = 1.65). Race: only difference was with Black/African American group: t(242) = −2.94, p = .004 (yes 8.8%, no 23.5%). University of South Florida Sample did not have significant age differences. Race: Higher percentage of White (yes 75%; no 54%) and lower percentage of Black/African American adolescents participated in COVID study (yes 23%; no 47%).
NT/TTP contains two subsamples. In TTP, males were more likely to complete COVID survey than females (no/yes: females: 40/47; males: 24/65).
TIGER COVID retention rate is reported as total. By sample, it was 43.64% MDD sample, 75% control. No significant differences in demographics, but the MDD group had significantly lower retention than the control group.
For CAT, Latino/Hispanic participants were less likely to complete COVID surveys (0% vs. not in COVID sample 10%).
Further, we only used data collected up to September 2020, so the current study only covers the early phase of the pandemic. Finally, it is important to note that the changes reported here might be temporary. It is beyond the scope of the present study to determine the long‐term impacts of the pandemic on adolescents' mental health; however, this is an important area for future research.
CONCLUSION
The current study is one of the first studies to report the longitudinal change in mental health symptoms from before to during the COVID‐19 pandemic in a large, international sample spanning the full age range of adolescence. The COVID‐19 pandemic appears to have impacted adolescent depression symptoms, and the impacts on depression and anxiety were felt most strongly by multiracial adolescents and those under “lockdown” restrictions. Future research should examine the long‐term impacts of the pandemic on adolescents' mental health and look for ways to boost adolescents' well‐being under physical distancing conditions. Public health policymakers need to explicitly consider the mental health impacts of their policies and invest in sources of support to buffer expected negative impacts.
Supporting information
Table S1. SES and race/ethnicity information by study.
Table S2. Descriptions of the individual studies.
Table S3. Results of the meta‐analysis of change in depression and anxiety symptoms (random effects model).
Table S4. Summaries of fixed effects of the models including the interaction between restrictions and Before_vs_DuringPandemic, as well as the interaction between case/death rate and Before_vs_DuringPandemic.
Study ARC was funded by an anonymous private donor and by the Bezos Family Foundation (PIs Magis‐Weinberg and Dahl). Study BLP was funded by the European Research Council (PI Crone; grant no. ERC CoG PROSOCIAL 681632). Study CAT was funded by the National Institute of Mental Health (PI Redcay; grant no. R01MH107441). Study EFC was funded by the Brain & Behavior Research Foundation and University of Texas start‐up funds (PI Church). Study KLG was supported by grants from the Hellman Fellows Fund and the National Institute of Mental Health/UCR Center for Health Disparities Research (PI Michalska; grant no. NIMH/UCR HDR U54MD013368). Study LIS was funded by the Institution of Education Sciences (PIs: Langberg & Becker; grant no. R305A160126), a Cincinnati Children's Research Foundation Research Innovation/Pilot (RIP) Award and a grant from the Virginia Tech COVID‐19 Rapid Response Seed Fund (PIs and CoIs: Becker, Langberg, Dvorsky, Breaux, & Sciberras). Study MFS was funded by the National Science Foundation (PI Campione‐Barr, grant no. 00047447), University of South‐Florida SP Internal Research Award (PI Rote) and University of Missouri Research Council (PI Killoren). Study NT/TTP was funded by the NIH (grant no. R01DA039923 for NT/TTP), National Science Foundation (grant no. SES 1459719 for NT), and Jacobs Foundation (grant no. 2018‐1288‐13 for TTP); PIs Telzer and Prinstein. Study SDS was funded by the National Science Foundation (PIs Thomas and Cavanagh; grant no. NSF‐2018‐1,826,773), American Psychological Foundation (PI Thomas), UTEP Center for Law and Border Studies (PI Thomas), and University of Texas at El Paso Internal Research Funding (PI Thomas). Study TAB was funded by the National Institute of Mental Health (PI Dennis‐Tiwary; grant no. R56MH111700). Study TAG was funded by the National Institute of Mental Health (PI Pfeifer; grant no. R01MH107418). Study TGR was supported by the National Institutes of Health (K01MH117442 to Ho, R37MH101495 to Gotlib), Klingenstein Third Generation Foundation (Child and Adolescent Depression Fellow Award to Ho), Stanford Maternal and Child Health Research Institute (Early Career Award and K Support Award to Ho), Stanford Center for Cognitive and Neurobiological Imaging (Seed Grant to Ho), and Ray and Dagmar Dolby Family Fund (to Ho). The funding agencies had no role in the design of the study or the collection, analysis, and interpretation of data or in writing the manuscript, apart from their financial contribution; the content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agencies. We would like to thank Claire Chie for her assistance in reliability coding and all participants and their families for their involvement in the study.
The authors declare no competing interests.
REFERENCES
- Achterberg, M. , Dobbelaar, S. , Boer, O. D. , & Crone, E. A. (2021). Perceived stress as mediator for longitudinal effects of the COVID‐19 lockdown on wellbeing of parents and children. Scientific Reports, 11(1), 2971. 10.1038/s41598-021-81720-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, E. R. , & Mayes, L. C. (2010). Race/ethnicity and internalizing disorders in youth: A review. Clinical Psychology Review, 30(3), 338–348. 10.1016/j.cpr.2009.12.008 [DOI] [PubMed] [Google Scholar]
- Bates, D. , Mächler, M. , Bolker, B. , & Walker, S. (2015). Fitting linear mixed‐effects models using lme4. Journal of Statistical Software, 67(1), 1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Bernasco, E. L. , Nelemans, S. A. , van der Graaff, J. , & Branje, S. (2021). Friend support and internalizing symptoms in early adolescence during COVID‐19. Journal of Research on Adolescence, 31(3), 692–702. 10.1111/jora.12662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bignardi, G. , Dalmaijer, E. S. , Anwyl‐Irvine, A. L. , Smith, T. A. , Siugzdaite, R. , Uh, S. , & Astle, D. E. (2020). Longitudinal increases in childhood depression symptoms during the COVID‐19 lockdown. Archives of Disease in Childhood, 106, 791–797. 10.1136/archdischild-2020-320372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsko, R. H. , Claussen, A. , Lichstein, J. , Black, L. , Everett Jones, S. , Danielson, M. , Hoenig, J. , & Ghandour, R. M. (2022). Mental health surveillance among children—United States, 2013–2019. MMWR Supplements, 71, 1–42. 10.15585/mmwr.su7102a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branje, S. , & Morris, A. S. (2021). The impact of the COVID‐19 pandemic on adolescent emotional, social, and academic adjustment. Journal of Research on Adolescence, 31(3), 486–499. 10.1111/jora.12668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen, L. L. , Shavit, Y. Z. , & Barnes, J. T. (2020). Age advantages in emotional experience persist even under threat from the COVID‐19 pandemic. Psychological Science, 31(11), 1374–1385. 10.1177/0956797620967261 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2021, January 26). Mental health—household pulse survey—COVID‐19. https://www.cdc.gov/nchs/covid19/pulse/mental‐health.htm
- Costello, E. J. , Copeland, W. , & Angold, A. (2011). Trends in psychopathology across the adolescent years: What changes when children become adolescents, and when adolescents become adults? Journal of Child Psychology and Psychiatry, and Allied Disciplines, 52(10), 1015–1025. 10.1111/j.1469-7610.2011.02446.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl, R. E. , Allen, N. B. , Wilbrecht, L. , & Suleiman, A. B. (2018). Importance of investing in adolescence from a developmental science perspective. Nature, 554(7693), 441–450. 10.1038/nature25770 [DOI] [PubMed] [Google Scholar]
- Demaray, M. K. , & Malecki, C. K. (2003). Importance ratings of socially supportive behaviors by children and adolescents. School Psychology Review, 32(1), 108–131. 10.1080/02796015.2003.12086186 [DOI] [Google Scholar]
- Dong, E. , Du, H. , & Gardner, L. (2020). An interactive web‐based dashboard to track COVID‐19 in real time. The Lancet Infectious Diseases, 20(5), 533–534. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, L. , Shao, X. , Wang, Y. , Huang, Y. , Miao, J. , Yang, X. , & Zhu, G. (2020). An investigation of mental health status of children and adolescents in China during the outbreak of COVID‐19. Journal of Affective Disorders, 275, 112–118. 10.1016/j.jad.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenkel, T. I. , Fox, N. A. , Pine, D. S. , Walker, O. L. , Degnan, K. A. , & Chronis‐Tuscano, A. (2015). Early childhood behavioral inhibition, adult psychopathology and the buffering effects of adolescent social networks: A twenty‐year prospective study. Journal of Child Psychology and Psychiatry, 56(10), 1065–1073. 10.1111/jcpp.12390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein, E. , Wen, H. , & Miller, B. F. (2020). Coronavirus disease 2019 (COVID‐19) and mental health for children and adolescents. JAMA Pediatrics, 174, 819–820. 10.1001/jamapediatrics.2020.1456 [DOI] [PubMed] [Google Scholar]
- Guessoum, S. B. , Lachal, J. , Radjack, R. , Carretier, E. , Minassian, S. , Benoit, L. , & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID‐19 pandemic and lockdown. Psychiatry Research, 291, 113264. 10.1016/j.psychres.2020.113264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, H. , Cohen Silver, R. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Petukhova, M. , Sampson, N. A. , Zaslavsky, A. M. , & Wittchen, H.‐U. (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. (2020). Mental health effects of school closures during COVID‐19. The Lancet Child & Adolescent Health, 4(6), 421. 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2020). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50, 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, K. A. , Hilt, L. M. , & Nolen‐Hoeksema, S. (2007). Racial/ethnic differences in internalizing and externalizing symptoms in adolescents. Journal of Abnormal Child Psychology, 35(5), 801–816. 10.1007/s10802-007-9128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller, J. (2015). A word on standardization in longitudinal studies: Don't. Frontiers in Psychology, 6, 1–4. 10.3389/fpsyg.2015.01389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, E. E. , Jarcho, J. M. , & Guyer, A. E. (2016). Social re‐orientation and brain development: An expanded and updated view. Developmental Cognitive Neuroscience, 17, 118–127. 10.1016/j.dcn.2015.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OpenInfo (n.d.). Corona cijfers per dag op gemeente, provincie en landelijk niveau . https://service.openinfo.nl/downloads/corona‐cijfers‐per‐dag‐op‐gemeente‐provincie‐en‐landelijk‐niveau/
- Orben, A. , Tomova, L. , & Blakemore, S.‐J. (2020). The effects of social deprivation on adolescent development and mental health. The Lancet Child & Adolescent Health, 4(8), 634–640. 10.1016/S2352-4642(20)30186-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel, J. , Oerlemans, A. M. , Raven, D. , Laceulle, O. M. , Hartman, C. A. , Veenstra, R. , Verhulst, F. C. , Vollebergh, W. , Rosmalen, J. G. M. , Reijneveld, S. A. , & Oldehinkel, A. J. (2017). Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychological Medicine, 47(7), 1271–1282. 10.1017/S0033291716003445 [DOI] [PubMed] [Google Scholar]
- Pan, K.‐Y. , Kok, A. A. L. , Eikelenboom, M. , Horsfall, M. , Jörg, F. , Luteijn, R. A. , Rhebergen, D. , Oppen, P. , van Giltay, E. J. , & Penninx, B. W. J. H. (2020). The mental health impact of the COVID‐19 pandemic on people with and without depressive, anxiety, or obsessive‐compulsive disorders: A longitudinal study of three Dutch case‐control cohorts. The Lancet Psychiatry, 8(2), 121–129. 10.1016/S2215-0366(20)30491-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peru Ministerio de Salud (n.d.). MINSA | Datos Abiertos Minsa y Gestión del Conocimiento en Covid‐19. https://www.minsa.gob.pe/datosabiertos/?op=22
- Racine, N. , Cooke, J. E. , Eirich, R. , Korczak, D. J. , McArthur, B. , & Madigan, S. (2020). Child and adolescent mental illness during COVID‐19: A rapid review. Psychiatry Research, 292, 113307. 10.1016/j.psychres.2020.113307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, M. H. , Crowe, P. A. , Larson, R. , & Swarr, A. (1998). Developmental patterns and gender differences in the experience of peer companionship during adolescence. Child Development, 69(1), 154–163. 10.1111/j.1467-8624.1998.tb06140.x [DOI] [PubMed] [Google Scholar]
- Rosen, M. L. , Rodman, A. M. , Kasparek, S. W. , Mayes, M. , Freeman, M. M. , Lengua, L. J. , Meltzoff, A. N. , & McLaughlin, K. A. (2021). Promoting youth mental health during the COVID‐19 pandemic: A longitudinal study. PLoS One, 16(8), e0255294. 10.1371/journal.pone.0255294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shum, A. , Skripkauskaite, S. , Pearcey, S. , Waite, P. , & Creswell, C. (2021). Children and adolescents’ mental health: One year in the pandemic (No. 10). https://cospaceoxford.org/wp‐content/uploads/2021/04/Co‐SPACE‐report‐10_06‐09‐21.pdf
- Taylor, S. E. (2011). Social support: A review. In Friedman H. S. (Ed.), The Oxford handbook of health psychology (pp. 189–214). Oxford University Press. [Google Scholar]
- Tretter, T. R. , Jones, M. G. , & Minogue, J. (2006). Accuracy of scale conceptions in science: Mental maneuverings across many orders of spatial magnitude. Journal of Research in Science Teaching, 43(10), 1061–1085. [Google Scholar]
- United States Census Bureau (2019). American community survey tables B01001A‐I . https://data.census.gov/cedsci/table?q=B01001&t=Age%20and%20Sex&tid=ACSDT1Y2019.B01001A&hidePreview=false
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , McIntyre, R. S. , Choo, F. N. , Tran, B. , Ho, R. , Sharma, V. K. , & Ho, C. (2020). A longitudinal study on the mental health of general population during the COVID‐19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widnall, E. , Winstone, L. , Mars, B. , Haworth, C. M. A. , & Kidger, J. (2020). Young people’s mental health during the COVID‐19 pandemic: Initial findings from a secondary school survey study in South West England. NIHR School for Public Health Research. https://sphr.nihr.ac.uk/wp‐content/uploads/2020/08/Young‐Peoples‐Mental‐Health‐during‐the‐COVID‐19‐Pandemic‐Report.pdf [Google Scholar]
- Wray‐Lake, L. , Crouter, A. C. , & McHale, S. M. (2010). Developmental patterns in decision‐making autonomy across middle childhood and adolescence: European American Parents' perspectives. Child Development, 81(2), 636–651. 10.1111/j.1467-8624.2009.01420.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie, X. , Xue, Q. , Zhou, Y. , Zhu, K. , Liu, Q. , Zhang, J. , & Song, R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174(9), 898. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, S.‐J. , Zhang, L.‐G. , Wang, L.‐L. , Guo, Z.‐C. , Wang, J.‐Q. , Chen, J.‐C. , Liu, M. , Chen, X. , & Chen, J.‐X. (2020). Prevalence and socio‐demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID‐19. European Child & Adolescent Psychiatry, 29, 749–758. 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. SES and race/ethnicity information by study.
Table S2. Descriptions of the individual studies.
Table S3. Results of the meta‐analysis of change in depression and anxiety symptoms (random effects model).
Table S4. Summaries of fixed effects of the models including the interaction between restrictions and Before_vs_DuringPandemic, as well as the interaction between case/death rate and Before_vs_DuringPandemic.


